Abstract
Annular elastolytic giant cell granuloma initially described by O’Brien in 1975 is a disorder of uncertain etiopathogenesis presenting with annular erythematous plaques predominantly on the sun-exposed areas. Hisptopathologically, it is characterized by elastin degenration, multinucleate giant cells, and elastophagocytosis. The authors came across 10 such cases, which were managed with hydroxychloroquine resulting in complete resolution in 4–6 months.
Keywords: Annular elastolytic giant cell granuloma, elastophagocytosis, elastosis, granulomatous disorder
INTRODUCTION
Annular and arciform lesions in dermatology practice are encountered in a varied etiology. Often histopathology correlation is relied upon to arrive at a final diagnosis in doubtful presentations of conditions, which include Hansen's disease, sarcoidosis, leishmaniasis, secondary syphilis, granuloma annulare, granuloma multiforme, and rarely annular elastolytic giant cell granuloma (AEGCG). Granulomatous infiltrate and overlapping histopathology have resulted in forme fruste of well-defined entities, such as granuloma annulare, granuloma multiforme, sarcoidal reaction in Hansen's disease, necrobiosis lipoidica, and even annular elastolytic granuloma.[1,2,3]
Management of these patients has been reported to be variable from difficult and unsatisfactory to a good response.[4]
The authors came across 10 cases of an otherwise rare entity of AEGCG, all presenting with similar clinical and histopathological features.
CASE REPORT
The authors encountered 10 similar cases presenting with annular lesions over the exposed areas of the body at the dermatology outpatient department [Table 1]. Three males (cases 2, 3, and 4) were farmers by occupation with a history of working outdoors for a number of years, whereas case 6 and females gave history of routine outdoor exposure to sunlight.
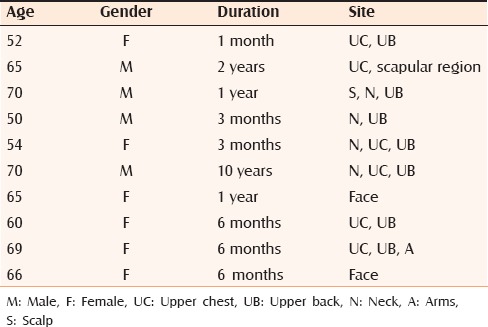
Table 1.
Summary of cases
The patients presented with asymptomatic “ring”-shaped skin lesions. The appearance in all was sudden onset, progressive, and varying in duration from 1 month to 10 years before presentation to us. There was no history of itching, loss of or altered sensations, prolonged drug intake for any chronic disease, or any comorbidity such as diabetes mellitus except in case 9 who was a known hypothyroid on treatment with levothyroxine. None had been treated for their complaint before their presentation to us.
Examination revealed well-defined skin colored to erythematous annnular and arciform lesions over the exposed areas of the neck, anterior chest wall, back, and arms in the two female patients and males had involvement of the scalp, face, neck, anterior chest wall, as well as the scapular regions [Figures 1 and 2]. Sensations were preserved. Mucosae, palms, soles, scalp, and hair and nails revealed no abnormality.
Figure 1.

Cases 1–5
Figure 2.

Cases 6, 8, and 9
Hematological (hemoglobin, complete blood count), biochemical (liver function tests, renal function tests, lipid profile, blood sugar) parameters, serum angiotensin-converting enzyme levels were normal and antinuclear antibody test was negative. Chest radiograph in all revealed no abnormality. Skin biopsy revealed similar changes in all patients with a keratinized thinned out epidermis, and superficial and middermis revealed presence of epithelioid cells with many multinucleated giant cells of Langhans and foreign body type with a presence of mild perivascular lymphoid infiltrate. Elastin stain revealed elastin degeneration specially adjacent to the giant cells [Figure 3]. There was no palisading granuloma, eosinophils, or obvious mucin. Ziehl–Neelsen and fungal stains were negative.
Figure 3.
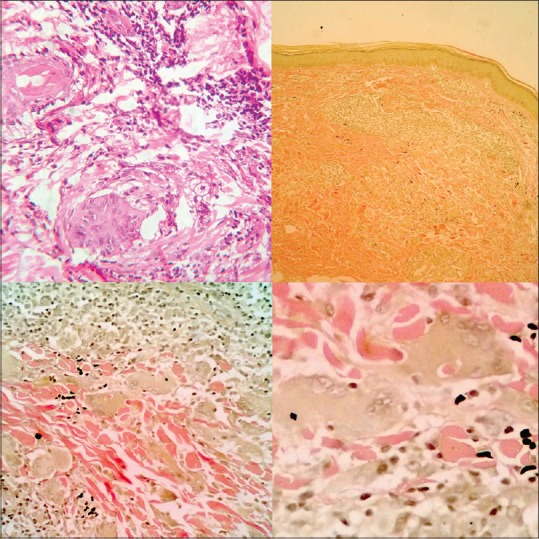
Upper left: photomicrograph showing mixed cell granulomatous infiltrate with giant cells, H and E, ×40; upper right: photomicrograph showing mixed cell granulomatous infiltrate with giant cells, Verhoeff–Van Gieson stain, ×10; lower left: photomicrograph showing elastin fiber degeneration and giant cells, Verhoeff–Van Gieson stain, ×40 and elastophagocytosis lower right Verhoeff–Van Gieson stain, ×100
All were placed on hydroxychloroquine 200 mg twice a day after a pre-treament ophthalmologic examination, baseline hemogram, liver function tests, and kidney function tests, which were normal in all cases. None developed fresh lesions after therapy, with complete resolution in 4–6 months. Ophthalmic review was repeated along with above tests at the completion of treatment.
DISCUSSION
Annular elastolytic giant cell granuloma is considered a distinct entity characterized by appearance of annular erythematous to skin-colored lesions preferentially on sun-exposed areas and histopathologically with a granulomatous reaction with elastolysis, phagocytosis of the elastic fibers, and multinucleate giant cells with absence or reduction of elastin fibers. Histopathological hallmarks also include absence of collagen necrobiosis or mucin deposition.
Hanke et al. initially proposed this term in a series of five cases in 1979.[5] Their clinical similarity to granuloma multiforme, necrobiosis lipoidica, and granuloma annulare has led to its debate as a separate entity.[6,7] However since their initial report in literature, few other cases have been reported, albeit with distinct histopathologial changes of granulomatous changes with lymphocytic infilterate, elastin degeneration, and multinucleate giant cells and rarely with overlapping features.[8] Pathogenesis of AEGCG is poorly understood. Initially described as actinic granuloma, atypical necrobiosis lipoidica, and Miescher's granuloma of the face it is proposed that ultraviolet radiation–induced cellular immunological reaction wherein the elastin fiber's immunopathogenicity plays a central role resulting in the formation of the elastocytic granuloma with ultimate destruction of elastin fibers.[9,10] Clinically, AEGCG presents on the sun-exposed areas of the face, neck, arms, and the upper back with skin colored to erythematous annular plaques and sometimes papules[11] with a raised erythematous border. It ususally manifests in the fourth to the seventh decade with a male preponderance to equal gender occurrence in different series.[12,13] There is no yellow discoloration or telangiectasia as in nerobiosis lipoidica diabeticorum. The lesions may persist for months to years resolving with either mottled pigmentation or normal appearing skin. O’Brien described four histopathological variants: the giant cell variant, the necrobiotic variant, the histiocytic variant, and the sarcoid variant.[9] Gutierrez-Gonzalez et al. reported the giant cell variant as the commonest variant in their review of 20 such cases.[12]
Management of these cases is controversial with variable treatement outcomes to topical measures with corticosteroids, tacrolimus, retinoids, and systemic agents in the form of methotrexate, isotretinoin, clofazimine, corticosteroids, acitretin, and hydroxychloroquine.[4]
Our patients presented in the sixth to the seventh decade. The females to male ratio was 1.2:1. They presented with lesions commonly on the upper chest and upper back, whereas one had involvement of the scalp and two of only the face. Three of our patients were farmers and reported intense sun exposure, whereas the rest had routine exposure. Sun exposure, specifically ultraviolet A radiation has been reported as the main etiologic factor. Hence the predominance of the exposed areas of involvement, with reports of covered areas being rarer,[14] although the classical actinic granuloma in contrast only involved the exposed areas.[10] Only one patient had an associated comorbidity in the form of hypothyroidism. A higher incidence of diabetes mellitus has been reported with AEGCG.[12,13] None of our patients had coexistent diabetes mellitus. Histopathologically all our patients manifested with granulomatous infilterates in the upper and middermis with multinucleate giant cells with fragmentation and reduced density of elastic fibers with elastophagocytosis. There was no evidence of necrobiosis or mucin deposition.
All our patients were managed with general sun protective measures and hydroxychloroquine 200 mg twice a day over a period of 4–6 months. Complete resolution was seen in six cases in 4 months, whereas four demonstrated partial remission with fading of the lesions with residual pigmentation over a period of 6 months. None developed fresh lesions while on treatment. All patients had been followed up for a minimum period of 6 months after their treatment.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Thomas M, Khopkar US. Necrobiosis lipoidica: A clinicopathological study in the Indian scenario. Indian Dermatol Online J. 2013;4:288–91. doi: 10.4103/2229-5178.120639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berliner JG, Haemel A, LeBoit PE, Pincus LB. The sarcoidal variant of annular elastolytic granuloma. J Cutan Pathol. 2013;40:918–20. doi: 10.1111/cup.12237. [DOI] [PubMed] [Google Scholar]
- 3.Shanmuga SC, Rai R, Laila A, Shanthakumari S, Sandhya V. Generalized granuloma annulare with tuberculoid granulomas: A rare histopathological variant. Indian J Dermatol Venereol Leprol. 2010;76:73–5. doi: 10.4103/0378-6323.58691. [DOI] [PubMed] [Google Scholar]
- 4.Babuna G, Buyukbabani N, Yazganoglu KD, Baykal C. Effective treatment with hydroxychloroquine in a case of annular elastolytic giant cell granuloma. Indian J Dermatol Venereol Leprol. 2011;77:110–1. doi: 10.4103/0378-6323.74988. [DOI] [PubMed] [Google Scholar]
- 5.Hanke CW, Bailin PL, Roenigk HH., Jr Annular elastolytic giant cell granuloma. A clinicopathologic study of five cases and a review of similar entities. J Am Acad Dermatol. 1979;1:413–21. [PubMed] [Google Scholar]
- 6.MacGrae JD., Jr Actinic granuloma. A clinical, histopathologic, and immunocytochemical study. Arch Dermatol. 1986;122:43–7. doi: 10.1001/archderm.122.1.43. [DOI] [PubMed] [Google Scholar]
- 7.Ragaz A, Ackerman AB. Is actinic granuloma a specific condition? Am J Dermatopathol. 1979;1:43–50. [PubMed] [Google Scholar]
- 8.de Oliveira FL, de Barros Silveira LK, Machado Ade M, Nery JA. Hybrid clinical and histopathological pattern in annular lesions: An overlap between annular elastolytic giant cell granuloma and granuloma annulare? Case Rep Dermatol Med 2012. 2012 doi: 10.1155/2012/102915. 102915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.O’Brien JP. Actinic granuloma: An annular connective tissue disorder affecting sun- and heat-damaged (elastotic) skin. Arch Dermatol. 1975;111:460–6. doi: 10.1001/archderm.111.4.460. [DOI] [PubMed] [Google Scholar]
- 10.Goldminz AM, Gottlieb AB. Noninfectious granulomatous dermatitides: A review of 8 disorders (Part 2 of 3) Semin Cutan Med Surg. 2013;32:e1–6. doi: 10.12788/j.sder.0028. [DOI] [PubMed] [Google Scholar]
- 11.Marmon S, O’Reilly KE, Fischer M, Meehan S, Machler B. Papular variant of annular elastolytic giant-cell granuloma. Dermatol Online J. 2012;18:23. [PubMed] [Google Scholar]
- 12.Gutierrez-Gonzalez E, Gomez-Bernal S, Alvarez-Perez A, Sanchez-Aguilar D, Toribio J. Elastolytic giant cell granuloma: Clinic-pathologic review of twenty cases. Dermatol Online J. 2013;19:20019. [PubMed] [Google Scholar]
- 13.Limas C. The spectrum of primary cutaneous elastolytic granulomas and their distinction from granuloma annulare: A clinicopathological analysis. Histopathology. 2004;44:277–82. doi: 10.1111/j.0309-0167.2004.01755.x. [DOI] [PubMed] [Google Scholar]
- 14.Pock L, Blazková J, Caloudová H, Varjassyová I, Konkolová R, Hercogová J. Annular elastolytic giant cell granuloma causes an irreversible disappearance of the elastic fibres. J Eur Acad Dermatol Venereol. 2004;18:365–8. doi: 10.1111/j.1468-3083.2004.00912.x. [DOI] [PubMed] [Google Scholar]


