Abstract
Glomus tumors are usually benign hamartomas, which are painful, small, and uncommon. They are usually subungal in location but may occur at other sites. A female patient presented to the outpatient department with painful swelling over the nail matrix of her right index finger. Here, we describe the use of a videodermosope having white light, polarized light, and ultraviolet (UV) light in the localization of glomus tumors that revealed a pinkish glow on UV light examination suggesting the vascular nature of the tumor. Thus, videodermoscopy can be used as an outpatient department procedure to confirm the diagnosis of glomus tumors.
Keywords: Dermoscopy, glomus tumor, pink glow, UV light
INTRODUCTION
Glomus tumor is a rare hamartoma, which arises from glomus body situated at the arterial end. Glomus tumors are usually solitary but can be multiple.[1] This tumor is generally common in young adults (20–40 years of age) and females are more commonly affected.[1] Here, we present videodermoscopic findings in a young female who had glomus tumor over the nail matrix of her right index finger.
CASE REPORT
A 23-year-old unmarried female came with the complaint of painful subungual swelling over the distal end of right index finger since 3 years. The lesion was very painful even to touch and light pressure (Love's sign), which affected her daily activities. The pain was severe, radiating, and increased on exposure to cold.
She had approached various specialists and was extensively investigated including radiography and magnetic resonance imaging (MRI) of the affected finger, which did not reveal any abnormality.
On clinical examination, there was an ill-defined swelling over the nail matrix of her right index finger with a slightly rounded, uniform elevation [Figure 1]. Love's sign was positive.[2] The nail plate was normal without any linear erythematous markings suggestive of vascular abnormality.
Figure 1.
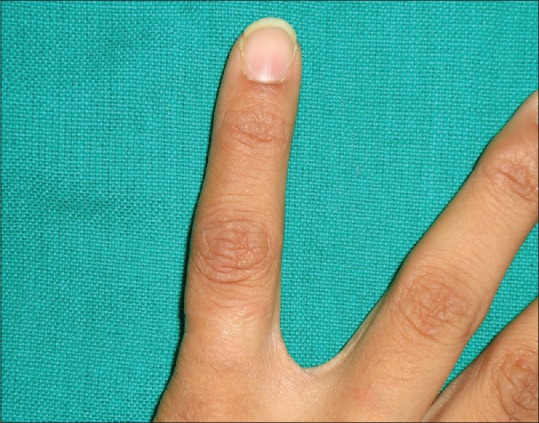
Glomus tumor: Barely perceptible lesion over nail matrix of right index finger
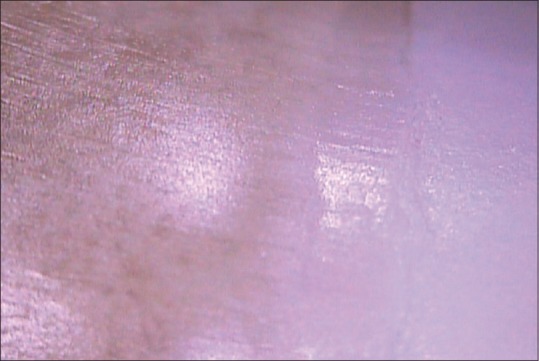
A videodermoscopy of the lesional site was done using white light, polarized light, and ultraviolet (UV) light. On white light, the swelling was well appreciated [Figure 2], whereas on polarized light altered pigmentary network pattern of the overlying skin was revealed [Figure 3]. UV light revealed a pinkish glow, which suggested the vascular nature of the tumor[3] [Figure 4].
Figure 2.
Glomus tumor: Slight elevation on white light dermoscopy
Figure 3.

Glomus tumor: Altered pigmentary network on polarized light dermoscopy
Figure 4.

Glomus tumor: Pink glow on ultraviolet light dermoscopy
Ultrasonography (USG) of local area revealed hypoechoeic nodule with prominent vascularity between distal phalanx and nail body, suggestive of glomus tumor. Surgical excision was done and the sample was sent for histopathological examination.
Histopathology revealed presence of glomus cells arranged around vascular spaces lined by endothelial cells, which confirmed diagnosis of glomus tumor [Figure 5].
Figure 5.
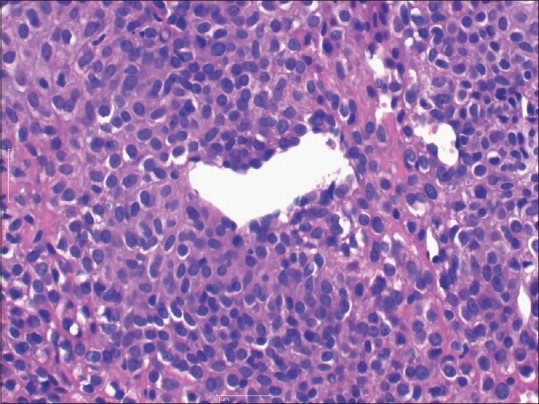
Glomus tumor: Neoplastic glomus cells with monomorphic round or oval nuclei and abundant pink cytoplasm. (H and E ×40)
DISCUSSION
Glomus tumor is an uncommon tumor arising from the glomus cells. They are usually noted in subungal locations. They are extremely painful to pressure, exposure to cold, and even to touch.[4] The pain increases on application of pressure with the tip of a pencil over the precise area (Love's sign[2]).
Treatment of choice for glomus tumor is surgical excision. Recurrences are noted due to local invasion of tumor. Sclerotherapy as well as laser therapy with CO2, KTP, Nd: YAG, and pulsed dye can be employed.[1]
Pre- and intraoperative use of dermoscope in a case of glomus tumor revealed discrete linear vascular structure on nail plate and numerous ramified telangiectasia on nail bed and matrix during surgery.[5]
To the best of our knowledge, the above-mentioned findings on polarized light and use of UV light source for characterising glomus tumors are not reported previously in the literature. USG needs expertise for early diagnosis, whereas cost and low specificity are the disadvantages of MRI. Thus, videodermoscopy with inbuilt white light, polarized light, and UV light can be used as an outpatient procedure to confirm the diagnosis of glomus tumor.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.North PE, Kincannon J. Vascular Neoplasms and Neoplastic. like Proliferations. In: Bolognia JL, Jorizzo JL, Schaffer JV, editors. Dermatology. 2nd ed. Spain: Elsevier Limited; 2008. pp. 1790–92. [Google Scholar]
- 2.Murthy PS, Rajagopal R, Kar PK, Grover S. Two cases of subungal glomus tumor. Indian J Dermatol Venereol Leprol. 2006;72:47–9. doi: 10.4103/0378-6323.19719. [DOI] [PubMed] [Google Scholar]
- 3.Gupta LK, Singhi MK. Wood's lamp. Indian J Dermatol Venereol Leprol. 2004;70:131–5. [PubMed] [Google Scholar]
- 4.Khandpur S, Ramam M. Skin tumors. In: Walia RG, Walia AR, editors. IADVL Textbook of Dermatology. 3rd ed. Mumbai: Bhalani Publishing House; 2008. pp. 1516–7. [Google Scholar]
- 5.MaeharaLde S, Ohe EM, Enokihara MY, Michalany NS, Yamada S, Hirata SH. Diagnosis of glomus tumor by nail bed and nail matrix dermoscopy. An Bras Dermatol. 2010;85:236–8. doi: 10.1590/s0365-05962010000200018. [DOI] [PubMed] [Google Scholar]


