Abstract
Background:
To estimate the magnitude and determinants of diabetic retinopathy (DR) among persons with diabetes registered at the employee health department of King Khaled Eye Specialist Hospital (KKESH).
Methods:
A retrospective review of medical records was conducted in 2013–14 at KKESH. The case record review extracted demographic, profile of diabetes, diabetic complications, and different blood indices to determine the status of potential risk factors. Ocular profile, especially DR was also noted.
Results:
Our cohort had 94 staff with diabetes. Eye examination was carried out in 51 (54.8%) of them. The rate of DR was 52% (95% confidence interval (CI) 28–66). Sight-threatening diabetic retinopathy (STDR) (proliferative DR and/or diabetic macular edema) was present in 40% of those examined. Good glycemic control was noted in 42% of participants. Duration of diabetes was associated with DR (P = 0.04). Good glycemic control was negatively associated to DR (odds ratio = 0.2 [95% CI 0.04–0.6]). The coverage of eye screening was 55% only. Laser treatment was given to 80% of STDR cases. The lens opacity and glaucoma rate was 15% and 8.3%, respectively.
Conclusions:
Low coverage for eye screening and laser treatment to diabetics among the staff of an eye hospital is a matter of concern. The underlying causes of low coverage of screening, digital fundus photography as a screening tool and management should be addressed.
Keywords: Diabetes, diabetic nephropathy, diabetic retinopathy, glycemic control, hyperlipidemia
Introduction
The prevalence of diabetes in Saudi Arabia is estimated to be 27.7% (95% CI 25.7–29.7) among 18 years and older Saudi population.[1] There could be 32,27,006 persons with diabetes in Saudi Arabia in 2010.[2] The prevalence of diabetic retinopathy (DR) ranged from 37% to 47% among 40+-year-old population of three administrative areas of Saudi Arabia. The rate of diabetic maculopathy ranged from 14.8% to 20.3% among diabetics in 40 years and older population.[3]
Duration of diabetes, type of diabetes, presence of renal complications of diabetes, older age, poor glycemic control, high lipid levels, hypertension are the known risk factors of DR and its progression.[4,5,6,7,8] In spite of blinding eye complications and ways to prevent/delay the progression, risk factors are less attended, and compliance of annual eye screening is often low and, therefore, all efforts for improving their compliance are suggested.[9]
The status of diabetic complications and their risk factors among eye health staff to the best of our knowledge is not yet studied. Eye health staff is more likely to be aware of complications of diabetes. Therefore, they are likely to take care of their diabetes and address the risk factors of DR more judiciously in comparison with diabetic patients in the community. We, therefore, conducted a study to estimate the magnitude and determinants of DR among persons with diabetes that were registered at Employee Health Department (EHD) of King Khaled Eye Specialist Hospital (KKESH).
Methods
The Institutional Research Board of KKESH approved of the research proposal. The study was conducted between July 2013 and March 2014. This was a retrospective review of case files of patients with diabetes that were registered at EHD of KKESH. Nearly 4,000 persons are employed in this institute. The majority of them are young professionals aged between 25 and 40 years. However, the dependents of staff (parents and children) also get health care at EHD. The identity of the person with diabetes was kept confidential.
Two research coordinators were the field staff of the study. A list of case files of employees that had undergone HbA1c blood test in last 1-year at KKESH was compiled from laboratory records. In addition, records of fasting blood sugar levels noted at the time of mandatory health check for renewal of employment contract were also referred. Their files were extracted and reviewed. Variables such as age, sex, area of residence, type of work at KKESH, date of first time registered at KKESH, date of first time diabetes detected, date of last follow-up, readings of the fasting blood sugar, lipid levels and serum cholesterol, blood pressure and history of taking medications for hypertension, other medical conditions such as diabetic nephropathy, diabetic neuropathy, diabetic foot, depression, erectile dysfunction, diabetic cardiomyopathy, and frequent infections in the body were extracted from the case records. The details of ocular comorbidities, refraction, presence, and stage of DR were based on their latest ophthalmic assessment.
To verify the history, values of laboratory tests and physical measurements were reviewed. Standard international definitions to define hyperglycemia, hyperlipidemia, hypercholesterolemia, and hypertension were applied while determining the status of diabetes and diabetic complications among participants.[10]
The data were compiled using Microsoft XL spreadsheet (Microsoft XL®) and then exported to the Statistical Package for Social Studies (SPSS 22, IBM, Chicago, USA). The number, percentage proportions, 95% confidence intervals of DR rate by gender and age group were calculated. Association of different factors to the DR was carried out using univariate and then multivariate analysis. Odd's ratio with 95% confidence intervals and P value were used to validate the association.
Results
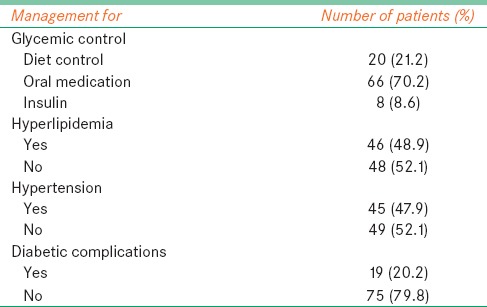
We evaluated the case records of 94 diabetic patients registered with EHD of KKESH. Males were 52 and mean age of participants was 50.2 ± 11.1 years (range 24–89 years). The mean duration of diabetes was 3.6 ± 4.2 years (range 1-month–30 years). Eighty-six persons had Type II diabetes; three had Type I and five women had gestational diabetes. The management mode for diabetes and its complications are given in Table 1. Nearly 70% of patients were prescribed oral anti-diabetic medications.
Table 1.
Management mode of diabetes and its complication among diabetic staff registered at a tertiary eye hospital
Among study participants, complications such as cardiac (two cases), renal (one), retinopathy (two), and depression (one) were documented at the time of registration.
During the last 1-year, 78 (83%) patients had visited the clinic for follow-up. Another 12 participants had visited diabetes clinic between last 1-year and 2 years. The reports of blood investigations that were carried out during last follow-up visit are presented in Table 2 and Figure 1. The hba1c level of more than 6.5% was found in 42.5% of participants.
Table 2.
Blood levels of diabetic patients at the time of their last follow-up
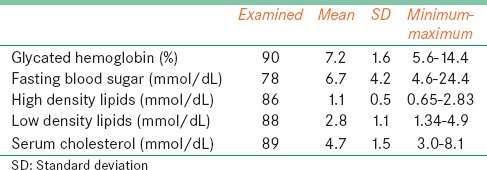
Figure 1.
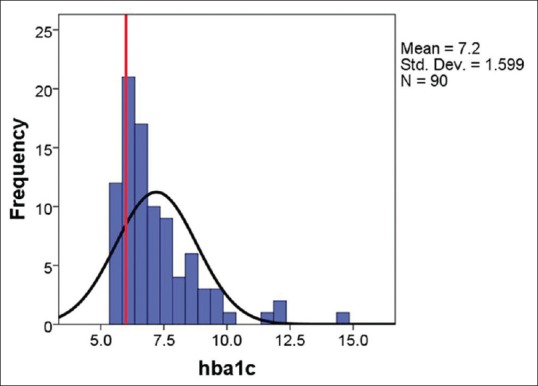
Glycemic control of persons with diabetes
Of 94 participants, eye examination was carried out of 51 (54.8%) diabetics. Visual acuity, as presented in the better eye, was 20/20–20/40 in 30 (65.2%) persons, <20/40–20/200 (moderate visual impairment) in 9 (19.6%) participants, <20/200–20/400 (severe visual impairment [SVI]) in 3 (6.5%) and <20/400 (blind) in 4 (8.7%) of 46 participants who had documented visual acuity.
Refractive status was documented of 27 participants. Myopia, hypermetropia, astigmatism, and anisometropia were in 14, three, one and two participants respectively. Presbyopia was present in 26 (54.2%) participants. Among 48 diabetics, two had lens opacities, and five had pseudophakia. Four patients were suffering from glaucoma.
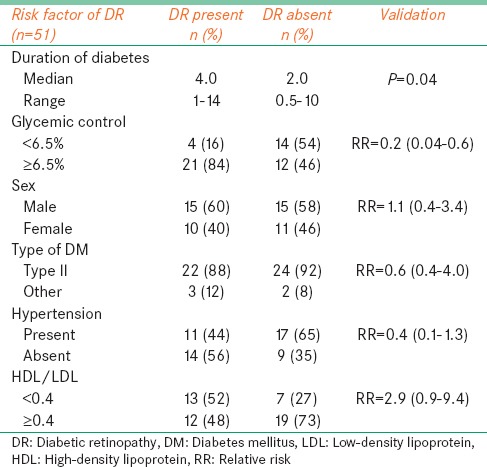
Different risk factors were associated with DR using univariate analysis [Table 3]. Duration of diabetes (relative risk [RR] =2.2) and glycemic control (RR = 0.3) were associated with the DR.
Table 3.
Risk factors of DR among diabetics that had eye check up
The coverage of DR screening was 48 (51.1%). Only one patient had undergone digital photography. Twenty-five diabetics had DR. The rate of DR was 52% (95% CI 28–66). In 20 patients, at least one eye had nonproliferative diabetic retinopathy. The rate of sight-threatening diabetic retinopathy (STDR) was 40%. In 5 (10%) patients and 4 (8.3%) patients, proliferative diabetic retinopathy (PDR), and diabetic macular edema (DME) were noted. DR was absent in either eye of 23 participants. Four patients had undergone laser treatment (one pan-retinal photocoagulation and three focal lasers) in the past. Two patients of DME were treated by intravitreal injections. None of the participants had vitreoretinal surgery in the past.
Discussion
The study covered a special category of diabetic patients that had easy and free of cost access to both diabetes and eye care. The coverage of annual screening among them was 80%, eye screening was 51% and laser treatment was 80%. The prevalence of DR and STDR was 52% and 40% respectively. Duration of diabetes and glycemic control were risk factors for DR. Nine percentage of diabetic had vision <20/400 (legal blind).
The prevalence of DR of all grades in our study was high. In a study with a large sample based on the national diabetes registry, Al Rubeaan et al. had reported 16.2% prevalence of DR.[11] In Taif province of Saudi Arabia, the prevalence of DR was 36.8%.[3] In Madinah province, a study reported that 36.1% of persons with diabetes had DR.[12] In Eastern province of Saudi Arabia, this rate was 30%.[13] DR rate in another study in Riyadh was 16.7%.[14] Different age groups, sample size and location of recruitment could be the reasons for such wide variation of prevalence rates of DR.
The high proportion of cases with STDR (40% out of 52%) in our study suggests advanced stages of blinding complications of diabetes. Of the 36.1% DR rate, 6.4% was due to PDR in Madinah and 17.5% in Taif study.[3,12] Reporting positive feedback of advanced stages in the case record of the employee in the present study and those not having DR record could be without or in early stages of DR in our study.
The long duration of diabetes was a risk factor for DR in our study. This is an established risk factor in the literature.[15,16] Tight glycemic control is also a protective factor for both development and progression of DR as was found in our study.[17] Glycemic control, lipid control, and hypertension control are the main primary prevention strategies for DR and its progression.[18]
The coverage of DR screening in our study in an eye hospital was 51%. While coverage of laser treatment among STDR cases was 80%. This was better than diabetic cases in the population (27% and 71%).[19] Overcoming the barrier of distance, lack of awareness and high cost in our study population could be one of the reasons for better coverage. Individual counseling to explain the risk of SVI and need for laser treatment in cases with STDR are recommended to improve compliance for laser treatment.[20]
Glaucoma and cataract were noted in 8.3% and 15% of a diabetic in our study. Primary open angle glaucoma and neovascular glaucoma are associated to diabetes mellitus and DR.[21,22] The risk of lens opacity also is higher among persons with diabetes.[23] Control of risk factors reduces progression of both DR as well as lens opacities in diabetics.[24] Comprehensive eye assessment and not just DR screening is therefore recommended to all persons with diabetes.
The inherent limitation of a retrospective review is a loss of data.[25] The data of eye care in our study was based on the records of 51% of a diabetic who had undergone eye screening in last 1-year. If we assume that all the absentees had no DR, the prevalence could be as low as 27%. If all absentees are assumed to have DR, the prevalence could be as high as 76%. In view of the special population that was studied, care should be taken while extrapolating the study results to Saudi diabetic population.
The visual impairment and blindness rate in our study was 15% and 9% in our study. A study in Jordan it was 11% and 7%, respectively.[26] It was 9.8% and 0.7% among adult diabetics in Oman.[27] Noncompliance of spectacle ware among Saudi student was as high as 68%. This behavior issue even in person with diabetes could be the underlying cause of high rate of visual disabilities that was measured using presented vision instead of best corrected vision in our study.
High prevalence of DR, low coverage of eye screening and care is a matter of concern, and we recommend prompt corrective actions. The family physicians must encourage diabetic patients for annual eye screening and should include DR screening within the protocol of diabetes care. Adoption of DR screening using the nonmydriatic camera and digital image interpretation using software could further improve the annual screening rate.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We thank Ches Sorou, Nouf Al Saara for assisting in retrieving the case files and information. The staff of EHD was cooperative and instrumental in expediting data collection.
References
- 1.Al-Daghri NM, Al-Attas OS, Alokail MS, Alkharfy KM, Yousef M, Sabico SL, et al. Diabetes mellitus type 2 and other chronic non-communicable diseases in the central region, Saudi Arabia (Riyadh cohort 2): A decade of an epidemic. BMC Med. 2011;9:76. doi: 10.1186/1741-7015-9-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khandekar R. Screening and public health strategies for diabetic retinopathy in the Eastern Mediterranean region. Middle East Afr J Ophthalmol. 2012;19:178–84. doi: 10.4103/0974-9233.95245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Al Ghamdi AH, Rabiu M, Hajar S, Yorston D, Kuper H, Polack S. Rapid assessment of avoidable blindness and diabetic retinopathy in Taif, Saudi Arabia. Br J Ophthalmol. 2012;96:1168–72. doi: 10.1136/bjophthalmol-2012-301874. [DOI] [PubMed] [Google Scholar]
- 4.Cakir Gundogan F, Tas A, Faruk Sahin O. Risk factors and diabetic retinopathy. Med Glas (Zenica) 2013;10:197. [PubMed] [Google Scholar]
- 5.Cho NH, Kim TH, Woo SJ, Park KH, Lim S, Cho YM, et al. Optimal HbA1c cutoff for detecting diabetic retinopathy. Acta Diabetol. 2013;50:837–42. doi: 10.1007/s00592-013-0452-3. [DOI] [PubMed] [Google Scholar]
- 6.Grunwald JE, Alexander J, Ying GS, Maguire M, Daniel E, Whittock-Martin R, et al. Retinopathy and chronic kidney disease in the Chronic Renal Insufficiency Cohort (CRIC) study. Arch Ophthalmol. 2012;130:1136–44. doi: 10.1001/archophthalmol.2012.1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Popescu T, Mota M. Dyslipidemia and hypertension in patients with type 2 diabetes and retinopathy. Rom J Intern Med. 2009;47:235–41. [PubMed] [Google Scholar]
- 8.Cheng YJ, Gregg EW, Geiss LS, Imperatore G, Williams DE, Zhang X, et al. Association of A1C and fasting plasma glucose levels with diabetic retinopathy prevalence in the U.S. population: Implications for diabetes diagnostic thresholds. Diabetes Care. 2009;32:2027, 32. doi: 10.2337/dc09-0440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khandekar R, Al Lawati J, Barakat N. A retrieval system for patients with avoidable blindness due to diabetic retinopathy who do not present for ophthalmic assessment in Oman. Middle East Afr J Ophthalmol. 2011;18:93–7. doi: 10.4103/0974-9233.80694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Preferred Practice Pattern Guidelines. [Last accessed on 2013 Jun 17]. Available from: http://www.one.aao.org/CE/PracticeGuidelines/PPP_Content.aspx?cid = d0c853d3-219f-487b-a524-326ab3cecd9a .
- 11.Al-Rubeaan K, Youssef AM, Subhani SN, Ahmad NA, Al-Sharqawi AH, Al-Mutlaq HM, et al. Diabetic nephropathy and its risk factors in a society with a type 2 diabetes epidemic: A Saudi national diabetes registry-based study. PLoS One. 2014;9:e88956. doi: 10.1371/journal.pone.0088956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.El-Bab MF, Shawky N, Al-Sisi A, Akhtar M. Retinopathy and risk factors in diabetic patients from Al-Madinah Al-Munawarah in the Kingdom of Saudi Arabia. Clin Ophthalmol. 2012;6:269–76. doi: 10.2147/OPTH.S27363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khan AR, Wiseberg JA, Lateef ZA, Khan SA. Prevalence and determinants of diabetic retinopathy in Al Hasa region of Saudi Arabia: Primary health care centre based cross-sectional survey, 2007-2009. Middle East Afr J Ophthalmol. 2010;17:257–63. doi: 10.4103/0974-9233.65502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alwakeel JS, Sulimani R, Al-Asaad H, Al-Harbi A, Tarif N, Al-Suwaida A, et al. Diabetes complications in 1952 type 2 diabetes mellitus patients managed in a single institution in Saudi Arabia. Ann Saudi Med. 2008;28:260–6. doi: 10.5144/0256-4947.2008.260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Du ZD, Hu LT, Zhao GQ, Ma Y, Zhou ZY, Jiang T. Epidemiological characteristics and risk factors of diabetic retinopathy in type 2 diabetes mellitus in Shandong Peninsula of China. Int J Ophthalmol. 2011;4:202–6. doi: 10.3980/j.issn.2222-3959.2011.02.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li X, Wang Z. Prevalence and incidence of retinopathy in elderly diabetic patients receiving early diagnosis and treatment. Exp Ther Med. 2013;5:1393–6. doi: 10.3892/etm.2013.1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Health Organization. Prevention of Blindness from Diabetes Mellitus Report of a WHO Consultation Geneva, Switzerland. 2006. [Last accessed on 2014 Apr 21]. Available from: http://www.who.int/blindness/Prevention%20of%20Blindness%20from%20Diabetes%20Mellitus-with-cover-small.pdf .
- 18.Yau JW, Rogers SL, Kawasaki R, Lamoureux EL, Kowalski JW, Bek T, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35:556–64. doi: 10.2337/dc11-1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Al-Rubeaan KA, Youssef AM, Subhani SN, Ahmad NA, Al-Sharqawi AH, Ibrahim HM. A web-based interactive diabetes registry for health care management and planning in Saudi Arabia. J Med Internet Res. 2013;15:e202. doi: 10.2196/jmir.2722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hua W, Cao S, Cui J, Maberley D, Matsubara J. Analysis of reasons for noncompliance with laser treatment in patients of diabetic retinopathy. Can J Ophthalmol. 2013;48:88–92. doi: 10.1016/j.jcjo.2012.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Klemm M, Gesser C. The relevance of diabetes for patients with glaucoma. Klin Monbl Augenheilkd. 2014;231:116–20. doi: 10.1055/s-0033-1360143. [DOI] [PubMed] [Google Scholar]
- 22.Shakya-Vaidya S, Aryal UR, Upadhyay M, Krettek A. Do non-communicable diseases such as hypertension and diabetes associate with primary open-angle glaucoma? Insights from a case-control study in Nepal. Glob Health Action. 2013;6:22636. doi: 10.3402/gha.v6i0.22636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pollreisz A, Schmidt-Erfurth U. Diabetic cataract-pathogenesis, epidemiology and treatment. J Ophthalmol. 2010;2010:608751. doi: 10.1155/2010/608751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen SJ, Liu JH, Shih HC, Chou P, Tsai CY, Tung TH. Prevalence and associated factors of lens opacities among Chinese type 2 diabetics in Kinmen, Taiwan. Acta Diabetol. 2008;45:7–13. doi: 10.1007/s00592-007-0012-9. [DOI] [PubMed] [Google Scholar]
- 25.Hennekens CH, Buring JE, Mayrent SL. Boston, USA: Little Brown and Company; 1987. Cohort Studies in Epidemiology in Medicine; pp. 153–74. [Google Scholar]
- 26.Al-Till MI, Al-Bdour MD, Ajlouni KM. Prevalence of blindness and visual impairment among Jordanian diabetics. Eur J Ophthalmol. 2005;15:62–8. doi: 10.1177/112067210501500110. [DOI] [PubMed] [Google Scholar]
- 27.Khandekar R, Mohammed AJ. Visual disabilities among diabetics in Oman. Saudi Med J. 2005;26:836–41. [PubMed] [Google Scholar]


