Abstract
Background
An emergency department is typically a place of high activity where practitioners care for unanticipated presentations, which yields a flow culture so that actions that secure available beds are prioritised by the practitioners.
Objectives
How does the flow culture in an emergency department influence nurses’ use of a research‐based clinical guideline and a nutrition screening routine.
Methods
Ethnographic fieldwork was carried out over three months. The first author followed nurses, medical secretaries and doctors in the emergency department. Data were also collected by means of semi‐structured interviews. An activity system analysis, as described in the Cultural Historical Activity Theory, was conducted to identify various contradictions that could exist between different parts of the activity system.
Results
The main contradiction identified was that guidelines and screening routines provided a flow stop. Four associated contradictions were identified: insufficient time to implement guidelines; guilty conscience due to perceived nonadherence to evidence‐based practices; newcomers having different priorities; and conflicting views of what constituted being a professional.
Conclusion
We found that research‐supported guidelines and screening routines were not used if they were perceived to stop the patient flow, suggesting that the practice was not fully evidence based.
Keywords: acute care, advanced practice, clinical guidelines, emergency care, emergency department, evidence‐based practice
What does this paper contribute to the wider global clinical community?
Understanding the local culture is necessary to realise ambitions for a more evidence‐based health care.
The concepts of flow culture and flow stoppers can be used by other researchers and practitioners in their analysis and understanding of the culture in other departments and specialties.
A strong focus on patient flow can have benefits such as reduced cycle times and shorter throughput intervals, but it may also create a culture that inhibits a more evidence‐based clinical practice in this setting. It is critically important to analyse the culture in which implementation occurs to address challenges involved in the implementation of evidence‐based practices.
Background
Hospital emergency departments play a vital role in the acute health care system, offering care for patients with acute illnesses and injuries and providing access to the health care system. Many countries have experienced an increase in the number of patients seeking emergency care. Combined with a reduction in bed capacity, this development has led to overcrowding in many emergency departments (Anneveld et al. 2013, O'Connor et al. 2014). Emergency departments in Denmark have undergone structural changes following health care reforms instigated in 2007 (Andersen & Jensen 2010). Many emergency departments in Denmark have merged, resulting in increased congestion in the remaining emergency departments due to the high demand for care, particularly among older people.
The emergency department is typically a place of high activity where emergency practitioners care for a wide range of unanticipated presentations, often dealing with life and death situations (Duffield et al. 2010). Like other health care practitioners, emergency department practitioners are expected to keep pace with the latest research advances and ascertain that their practice is evidence based. However, research has shown that the challenges of overcrowding and poor patient flow in emergency department settings can lead to decreased adherence to guidelines, inappropriate decision making and an increased numbers of adverse events, thus hampering ambitions to achieve an evidence‐based practice (Bigham et al. 2010, Person et al. 2013).
Barriers to the implementation of evidence‐based interventions, services and programs in health care are often identified at the individual practitioner level, e.g. in terms of health care practitioners’ knowledge, skills, self‐efficacy, attitudes and beliefs concerning the use of research in clinical practice (Estabrooks et al. 2003). However, there is increasing recognition of the relevance of the organisational culture for implementation of evidence‐based practices; the shared assumptions, beliefs, values and norms among members of an organisation can exert a strong influence on how individual practitioners think, feel and behave in relation to the use of research in clinical practice (Nilsen 2010). A previous study by the authors of this study showed that the maintenance of continuous patient flow in a Danish emergency department generated an organisational culture where actions that secured available beds were collectively prioritised by the emergency department practitioners; this culture was termed a flow culture (Kirk & Nilsen 2015).
Research is still limited regarding the impact of culture on the implementation of evidence‐based practices although researchers (Aarons et al. 2012, Rabin & Brownson 2012) have called for more studies to improve our understanding of cultural influences on implementation processes and health care practitioners’ use of research in their daily practice. By cultural influence we mean ways of learning and acting mediated by artefacts in local practice (Hasse 2011). In recognition of the potential importance of organisational culture for developing an evidence‐based practice, the aim of this study was to explore how the flow culture in a Danish emergency department influenced nurses’ use of an evidence‐based clinical guideline concerning management of vital parameters and an evidence‐based nutrition screening routine. We conducted an ethnographic study and subsequently performed an activity system analysis, as described in the Cultural Historical Activity Theory (CHAT; Engeström 1987, 2001) to obtain a deeper understanding of how a flow culture influenced the use of evidence‐based practices in this environment.
Methods
Study setting
The study was conducted in Denmark, where the public health care system funded by tax payers provides free treatment for primary medical care, hospitals and homecare services for all citizens. All hospitals are obligated to pass a national accreditation program, the Danish Healthcare Quality Programme. Hospitals are paid to deliver information about their admissions to the National Patient Registry, which enables information to be gathered about all admissions to Danish hospitals.
The study was carried out in the emergency department of a 750‐bed Danish urban university hospital. The emergency department had 70 employees, primarily registered nurses and medical secretaries. Each morning, doctors came from their specialty departments to participate in rounds for the patients who were admitted to the department (the doctors were not employed in the emergency department). On average, 60% of the patients in the emergency department were discharged within 24 hours.
Theoretical framework
We applied the CHAT (Vygotsky 1978), which posits that learning is collective, social and situated and is achieved through participation in practice. The theory attempts to overcome dichotomies between the individual and the collective, proposing that a so‐called activity system is the most appropriate unit of analysis (Engeström 1987).
Cultural Historical Activity Theory originated from the Russian psychologists, Vygotsky (1978) and Leont'ev (1978), and has been applied to other situations (Virkkunen & Kuutti 2000), including health care environments (Engeström 2001). Activity systems analysis is based on Vygotsky's work on mediating action and Leont'jev's work on mediated collective activity (Leont'ev 1978, Engeström 1987). According to Engeström (1987), the elements of activity systems include components such as subject, tool, object (goal), rules, community, division of labour and outcomes (Fig. 1).
Figure 1.
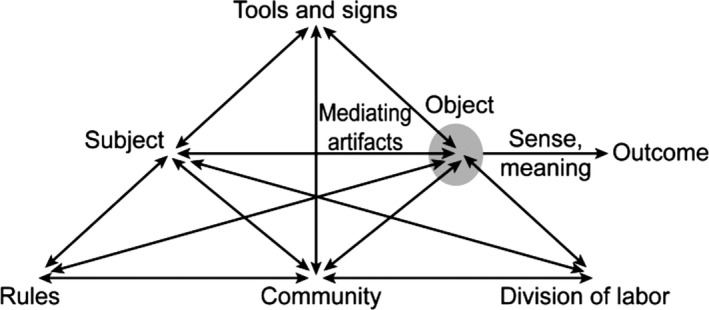
A complex model of an activity system (Engeström 1987).
Cultural Historical Activity Theory assumes that cultural tools or artefacts, physical or intellectual, mediate the experience of reality. This means that a person is never in direct, uninterpreted contact with the surrounding world. Activity system analysis was applied to this study of the emergency department with tools such as whiteboards, tables and language (Table 1).
Table 1.
The emergency department as an activity system
| Components of the activity system (Engeström 1987, 2001) | Explanation of the components | Applied to the emergency department |
|---|---|---|
| Activity | Defined as an object and targeted activity; activity represents dynamic interactions between individual and collective actions mediated by artefacts and context | All actions that were aimed at securing a free bed for the next patient, e.g. taking blood tests so the doctors can get feedback and decide what to do with the patients |
| Motive | The direction of an activity is determined by a motive towards its object, an individual psychological driving force in achieving the object | To secure flow, the nurses, doctors and medical secretaries appeared professional in the leaders’ and in each other's eyes |
| Outcome | The outcome is the consequences that the subject faces because of his/her actions driven by the object. These outcomes can encourage or hinder the subject's participation in future activities | The outcome in a flow culture was to secure a continuous flow of patients |
| The subject | The acting individuals who, through mediating artefacts, are included in the various object‐related activities, which are directed towards the common object | The nurses |
| The object | The object connects the individual actions within the collective activity. Objects can be material things, plans, common ideas – everything that can be shared and transformed by the participants in the activity and that motivates participants’ actions | Securing free beds |
| Mediation of human activity through tools, signs, artefacts | Artefacts such as objects, signs, language or symbols are understood as cultural tools that groups of people have developed over time to reflect the users’ values, ideas, principles and practices | The electronic boards, the leaders, the other professionals and the language |
| Rules | The implicit and explicit regulations, norms and conventions that influence and affect the efficacy of actions and interactions within the individual activity system | Screening for nutrition and using clinical guidelines |
| Community | A group of individuals, all acting in relation to the same object and simultaneously constructing themselves differently from other groups and other social contexts | Nurses, medical secretaries and doctors |
| Division of labour | Incorporates both the vertical division of power and status and the horizontal distribution of tasks and functions | Leaders, the other professions and the experienced nurses |
In CHAT, the term contradiction is used to describe tension or mismatches between different parts of the activity system or between different activity systems. Contradictions should be seen as opportunities for development rather than as obstacles (Engeström 2001). They are, however, often manifested as problems, disturbances or breakdowns in the activity system (Virkkunen & Kuutti 2000).
Study objects
The study focused on identifying contradictions in the emergency department activity system that might influence the implementation of two evidence‐based practices in this setting: screening for nutrition and a clinical guideline concerning measurement of vital parameters.
Nurses in the emergency department performed screening for nutrition risk to identify patients who require nutritional support. Screening was carried out by all the nursing staff. All emergency departments in Demark use a general nutrition screening that focuses on current and adapted weight loss, body mass index and severity of disease (Volkert et al. 2006). Nutrition risk screening must be performed within 24 hours of admission according to the Danish Healthcare Quality Programme.
Emergency department health care practitioners throughout Denmark use many different evidence‐based guidelines. We specifically studied a guideline that recommends systematic measurement of vital parameters. The (Modified) Early Warning Score (MEWS) is a systematic observation and risk assessment tool for patients who are admitted (Subbe et al. 2001). MEWS is bedside evaluation tool based on five physiologic parameters: systolic blood pressure, pulse rate, respiratory rate, temperature and AVPU (alert, voice, pain, unresponsive) score, a system by which health care practitioners can record a patient's responsiveness, indicating their level of consciousness. Adherence to this guideline is required by the International Joint Commission Programme and the Danish Healthcare Quality Programme.
Collection of data
Ethnographic fieldwork was carried out by the first author for three months between September and December 2011. Ethnographic methods are based on participation in everyday practice, which is considered a credible way to study cultural practices (Hasse 2011). Previous research on patient flow (Nugus et al. 2014) suggests that ethnographic methods can provide rich information for improved understanding of the practical challenges involved in the implementation of evidence based practices in emergency departments.
The first author followed nurses, medical secretaries and doctors, the three professions represented in the emergency department. The health care practitioners were followed up for an average of 8 hours/day between the hours of 8 am and 8 pm. The researcher followed 34 health care practitioners (27 nurses, four medical secretaries, three doctors) and made 420 hours of observations. Their median clinical experience was five years (medical secretaries), 7·5 years (nurses) and eight years (doctors). Field notes were taken throughout. Continuous cross‐checking of information was accomplished by checking verbal assertions with observations (Davies 2008).
Medical records were also checked for data on nutrition screening in case the screening was performed when the researcher was not in the emergency department. The number of nutrition screenings in the emergency department decreased more during 2009–2011 than in the other departments in the hospital, according to information in the medical records.
After the fieldwork, 14 interviews were conducted in June 2012. The interviews were semi‐structured, based on a conventional thematic analysis of data from the observational studies. Of the 34 health care practitioners, eight nurses, two medical secretaries and 1 doctor were interviewed. Three nurses who were not followed in the fieldwork were also interviewed. After the interviews, another conventional thematic analysis was conducted with data from the interviews (Hsieh & Shannon 2005). One of the themes was clinical guidelines and screenings, which belong to the rules component of the activity system. Rules refer to implicit and explicit norms, conventions and social relations in the community. Some clinical guidelines and screenings seem to create contradictions in the flow culture.
Analysis of data: contradiction analysis
We conducted a contradiction analysis to identify the various contradictions that may exist between different parts of the activity systems (Yagamata‐Lynch 2010). We organised quotations and field notes into groups consisting of statements on specific issues. Each group was analysed to clarify the meaning of the quotations and to identify contradictions and consensus expressed in these quotations and seen in the field notes (Table 2).
Table 2.
Contradictions analysis
| Illustrative quotations and notes from the field study and the interviews | Interpretive remarks | Contradiction analysis |
|---|---|---|
| How often do you receive new guidelines? What do you think about that? | ||
|
‘Every day. I think we receive 2–3 new or updated guidelines per day. I don't have any chance in daily practice to update my knowledge.’ (nurse 12) ‘Every day. If guidelines are made to beat the staff over the head, then don't send them. They become a tool to increase the poor conscience.’ (nurse 3) ‘I am not sure … maybe every day. It is difficult to find the time to look at all these guidelines. I now that I'm not up to date with a lot of guidelines.’ (doctor 2) ‘Every day. I think it is a problem that we only receive an email as the only reminder that there are new guidelines. Nobody in this department can check emails during the day.’ (medical secretaries 2) All guidelines were sent from the hospital's central quality department to a secretary in the department. She made sure that the guidelines were available in the central web portal and she also sent a message via email to all professions (field notes from researcher) |
There appears to be a consensus across professional borders that everyone knows that they receive new or updated guidelines every day They also agree that time is a limiting factor for the opportunity to look at these new guidelines. And the method used is not deemed appropriate When the staff do not manage to look at the guidelines or perform actions similar to those in the guidelines, it is experienced as a tool that preys on the conscience |
The amount of guidelines sent daily to the health professionals creates contradictions between community and rules. Lack of time and the methods used create contradictions between the subject and rules, which increase bad conscience. Simultaneously, the methodological approach is seen as a sign of a top‐down thinking thereby creating contradictions between different activity systems and their embedded cultural thinking about the use of guidelines and standards |
| Are there clinical guidelines you rarely use? And why? | ||
|
‘If you call nutrition and pressure ulcer screenings standards, those screening tools I don't use. They don't fit within an emergency department’ (nurse 17) ‘Nutrition screening is in contrast with acute treatment’ (nurse 1) ‘If the guidelines are not FAM (emergency department) specified, then I do not use them. It is a waste of my time’ (nurse 22) ‘I don't know, but I know that many of the nurses in the department do not prioritise screening for nutrition and pressure ulcers. They find that these screenings do not fit in. They (the screenings) don't support patients moving on in the hospital and that is very important in this department’ (doctor 3) The researcher did not see many nurses do nutrition or pressure ulcer screenings. When some of the new nurses started to screen, they were asked to prioritise differently by their more experienced colleagues (field notes from researcher) When some nurses did the nutrition screening, they felt tied to the patient. They began to sweat and became abrupt with the patients (field notes from the researcher) |
There appears to be a consensus across all professions that screening for nutrition and pressure ulcers is not performed in the department The explanations were that the screenings do not fit within the emergency department – they are not FAM specified. They also do not help the staff to move patients on in the system and this is why the guidelines were not deemed useful Newcomers learned over time which actions were right in the department |
Screening for nutrition and pressure ulcers creates contradictions between the nurses and the rules. At the same time, it is common knowledge in the community that these screenings do not fit into the department, which is represented by the activity system flow culture Instead, the screenings become a mediating sign of an embedded understanding of a professional identity that belongs in a medical department and not in a flow culture When newcomers began to screen, it created contradictions between the subject and the community |
| In what situations do you use clinical guidelines? | ||
|
‘I use guidelines especially in unknown and acute situations.’ (doctor 1) ‘I use guidelines when it helps my colleagues move on with their work and if the actions connected to the guidelines ensure that the patients move on into the hospital or home.’ (nurse 8) ‘What is it that causes death in the first 24 hours? Not hunger but fluid! That is why I always give the highest priority to treatment with intravenous fluids. When a stable patient is transferred, then the medical department can do the nutrition screening. I think it is part of their job.’ (nurse 9) The researcher often experienced that guidelines that secured patient transfer were prioritised (field notes from the researcher) |
Guidelines are used particularly in the case of acute care situations, but were also given priority if the guidelines supported moving the patient on to another department or home If the use of guidelines helped the professional to finish in the emergency department and go back to their specialised department (doctors), then the guidelines were prioritised Screenings for nutrition and pressure ulcers were perceived as not belonging to an emergency department but in a medical department. The health professionals found that only specific types of guidelines belong in the emergency department |
Guidelines and screenings that do not support the creation of a continuous patient flow or do not ensure that the doctors can get back to their specialised department creates contradictions between rules, subject and community Another contradiction created between rules and community was that nutrition and pressure ulcer screening challenged the embedded common knowledge and understanding about being a professional, an understanding created in the flow culture |
Ethical review
Before beginning the study, the first author participated in four weekly meetings with the emergency department staff, which gave them the opportunity to ask questions about the study. All participants gave their written, voluntary and informed consent before participation. All names were replaced by code names in the researcher's notes. Ethical approval was not required for the study. According to Danish law, formal ethical approval is not mandatory for studies that do not involve biomedical issues.
Results
The contradiction analysis yielded five contradictions that were observed in the emergency department. The main contradiction was that the evidence‐based screening routine and clinical guidelines provided flow stops. This contradiction was associated with four other contradictions in the flow culture: (1) insufficient time to implement a large number of guidelines; (2) guilty conscience due to perceived nonadherence to evidence‐based practices; (3) newcomers had different priorities in the emergency department; and (4) conflicting views of what constituted being a professional in the emergency department.
Guidelines and screenings created flow stops
Nutrition screening created contradictions between rules and object. When the object in the flow culture was to free up beds to create a constant flow of patients, it was important that guidelines and standards supported the achievement of this object. The nurses believed nutrition screening hindered patient flow and obstructed the progression of patients in the system:
When I prioritise nutrition screening it has the consequence that the patients can't move on in the system. (nurse 8, field notes)
The nurses experienced that nutrition screening occupied their time, which made it difficult for them to stay ahead of freeing up beds, which was necessary to ensure a constant flow of patients. Hence, nutrition screening was seen as a flow stopper in the flow culture and the screening was not widely used. However, data from the medical records on the MEWS guidelines showed that checking blood pressure, pulse rate and respiratory rate were prioritised by the professions in the emergency department:
One of the things I do first is to measure the vital parameters. It gives me a picture of the patient. However, these parameters are also the ones the doctor is using to find out where the patient belongs in the system … if the patient is acutely ill, then we have to find a bed in the hospital or perhaps the patient can be discharged soon. (nurse 11, interview)
Modified Early Warning Score provided the doctors and nurses with a professional impression of the patients, which helped in planning the flow of patients. Thus, the MEWS guidelines were not perceived as a flow stopper and were prioritised in the emergency department.
Insufficient time to implement a large number of guidelines
Insufficient time to implement a large number of clinical guidelines created contradictions between different activity systems. The medical secretaries in the emergency department received guidelines almost daily. Guidelines were delivered from the top down from health authorities and the hospital's quality department. The staff knew that they were expected to read, understand and implement the recommendations described in these guidelines in their everyday practice. However, they had difficulties finding the time to gain access to a computer and check for emails concerning these guidelines:
I find the large number of guidelines totally stressing and it is completely unrealistic … especially because many of them (the guidelines) are not relevant for the staff in the emergency department. I wonder what the capital thinks we are spending our time doing. (doctor 3, field notes)
Many practitioners believed that it was simply unrealistic to keep abreast of the continuous flow of guidelines. The practitioners perceived that these expectations created contradictions with daily practices; many of these guidelines were perceived as irrelevant because they did not support patient flow or were flow stoppers, which can be seen as contradictions between different activity systems. The guidelines also created contradictions between rules and community, because the consequence of not prioritising these guidelines was that they were not implemented.
Nonadherence to evidence‐based practices generated a guilty conscience
The lack of adherence to various evidence‐based practices generated a guilty conscience among the nurses in the emergency department. This created contradictions between the nurses and the rules. The nurses knew that the screening for nutrition was of relevance to the patients:
I have learned the importance of well‐nourished patients, but there are other actions I have to prioritise in this department. (nurse 17, interview)
When some nurses did the screening, they were psychologically challenged because they felt tied to these patients. Their discomfort was evident in the form of bodily reactions, such as being abrupt and sweating, which reinforced the impression that nutrition screening was something that enhanced the staff's guilty conscience. Thus, nutrition screening created contradictions between the nurses and the rules because they excluded the screening, despite the fact that it was part of the Danish Healthcare Quality Programme, as a means to achieve more evidence‐based practices and despite the nurses’ knowledge that nutrition was important for the patients.
Newcomers to the emergency department had different priorities
Those who were new to the emergency department often had different priorities from the existing staff. These priorities created contradictions between the subject and division of labour. The screening of patients by nurses who were newcomers showed that they had not yet acquired a thorough understanding of what was considered important to prioritise in the flow culture:
We'll quickly teach the new nurses that nutrition screening doesn't belong in this department (in the emergency department). (medical secretary 1, interview)
The more experienced health care practitioners had bodily and verbal reactions when the newcomers started screening the patients. For instance, the medical secretaries sharpened their tone when they talked to the newcomers and other nurses yelled at the newcomers and gossiped about them. Screening of patients by newcomers also caused conflicts among the experienced health care practitioners. Doctors were frustrated with the experienced nurses because they expected them to teach the newcomers that nutrition screening should not be a priority because time spent on the screening might mean that the doctors could not get their job done in the emergency department in a timely manner, delaying their return to their specialty department. Over time (most of) the newcomers learned through the other practitioners’ bodily reactions what was perceived as culturally relevant in the emergency department. Most of the newcomers stopped screening the patients, which created a guilty conscience and low adherence to various evidence‐based practices.
Conflicting views of what constituted being a professional in the emergency department
There were conflicting views about what it meant to be a professional in the emergency department, which created contradictions between the rules and the different activity systems. Acting professionally in the emergency department meant contributing to the flow culture, i.e. not prioritising screening for nutrition, as recommended in the guidelines. When nurses were able to maintain a flow of patients in the emergency department, they were perceived as professionals by the other emergency department professionals and managers. Thus, being considered a professional in the emergency department meant that one had to learn to prioritise correctly. However, this view of a professional nurse contradicted the nurses’ traditional view of professionalism because nutrition screening was seen to be part of holistic care and treatment of the patients:
It must be a pressure for the nurses to be educated to be able to account for “the whole patient” while practice requires that you have to have an overview to maintain the flow of patients. (doctor 2, interview)
These conflicting views about what it means to be a professional in the emergency department were very significant for some nurses in the department:
I have to stop in the department … there are too many basic nursing actions that are not a priority in this department. I need to go somewhere else where basic nursing actions are considered important. (nurse 26, field notes)
To ensure patient flow and the flow culture created by this pressure, some nurses experienced a loss of professional identity, which caused them to leave the department.
Discussion
This study explored how nurses’ use of clinical guidelines and a screening routine was influenced by the flow culture in an emergency department in Denmark. We applied the CHAT (Engeström 1987) and conducted a contradiction analysis to identify various tensions or mismatches (i.e. contradictions), between different parts of the activity system or between different activity systems, that might affect the implementation of two types of evidence‐based practices. The main contradiction was that guidelines and screenings that did not facilitate the object (goal), i.e. securing beds for patients arriving in the emergency department, and were therefore perceived as flow stops, were not implemented as intended. A flow stop is an action that, despite execution, has no influence on how quickly the patients move through the department. This contradiction was associated with four other contradictions in the flow culture: insufficient time to implement a large number of guidelines, guilty conscience due to perceived nonadherence to evidence‐based practices, newcomers had different priorities in the emergency department and conflicting views of what constituted being a professional in the emergency department.
Patient flow has often been described in linear terms (Lane & Huseman 2008). Generating patient flow by means of mathematical models appears to have benefits, such as reduced cycle times and shorter throughput intervals (Baker et al. 2013), potentially yielding better patient outcomes and improved patient satisfaction with health services. However, a strong focus on achieving patient flow might also contribute to a culture that hampers ambitions to attain an evidence‐based clinical practice. Achieving an evidence‐based practice is not merely about getting research into practice; it is also about creating a culture where health care practitioners think in an evidence‐based way so that it becomes natural to seek out research and base treatment decisions on that evidence. This requires an appreciation of the context in which practitioners are a part.
Explanations for the research–practice gap have largely focused on the characteristics of the individual health care practitioner, such as poor confidence in identifying and critically appraising evidence and perceived lack of time to integrate research into clinical practice (Estabrooks et al. 2003, Rycroft‐Malone 2008). However, our findings suggest that difficulties in achieving a more evidence‐based health care practice may not be due primarily to individual barriers related to practitioners’ knowledge, skills, self‐efficacy, attitudes or beliefs. Despite the fact that barriers and facilitators in achieving an evidence‐based practice are likely to be present at multiple levels, Yano (2008) believes that implementation research has ‘failed to fully recognise or adequately address the influence and importance of health care organisational factors’. There is growing recognition among implementation researchers of the role of organisational factors in the successful implementation of evidence‐based practices (Fixsen et al. 2005).
Our findings underscore the relevance of accounting for the context in which individuals are a part. Context has been described as ‘an important but poorly understood mediator of change and innovation’ in health care organisations. The influence of context is often unrecognised or underappreciated, despite the fact that implementation researchers have called for more research to gain a better understanding of this complex concept (Kent & McCormack 2010, Nilsen 2010).
The context is often depicted as a passive backdrop to implementation of new practices (McCormack et al. 2002) but our study suggests a more active notion of the context. From the CHAT perspective, the emergency department context consists of practitioners who interact with each other and with managers, guidelines, artefacts, physical spaces and other institutional and societal structures.
This study provides a somewhat different perspective of time as a barrier to implementation of evidence‐based practices in health care. Lack of time is frequently cited as a barrier in implementation research due to the time it takes to identify and critically assess relevant research and apply it in clinical practice or adapt and implement evidence‐based practices, for instance guidelines and screening routines (Ellen et al. 2013, Harrison et al. 2013). The health care practitioners in our study did not consider screenings or guidelines as contradictions due to a lack of clock time. Their perceptions of the two practices can be understood in relation to their underlying motives. Ensuring a flow of patients made the health care practitioners appear professional in each other's eyes, which was very important for the security of their role (Kirk & Nilsen 2015). Verbal expressions and bodily reactions created a collective understanding of what activities should be prioritised and determined what the clock time was going to be used for.
We used an ethnographic approach for the study because we believed it would enable a deeper understanding of how health care practitioners engage with evidence‐based practices in their everyday work. Previous research on patient flow has suggested that ethnography is a beneficial approach (Nugus & Forero 2011), but implementation research has predominantly used questionnaires and interviews to investigate how and the extent to which practitioners use research. However, we believe that some of our observations would not have been possible using other data collection methods or approaches. For instance, the importance of securing the flow of patients was not something that was addressed or discussed in official meetings in the emergency department. It was something that could be observed through reactions from other practitioners in the emergency department and by following the practitioners in different physical spaces. Ethnography has been described ‘the art and science of describing a group or a culture’ (Fetterman 1998, p. 1) where one is trying to understand their way of life from their point of view. The purpose of our approach was to understand what was really going on when health care practitioners use or refrain from using evidence‐based practices. Ethnography involves no interference or experimentation or any fixed pattern of gathering data. The aim is to use whatever means one can to build up a ‘thick description’ (Geertz 1973) of the actions and events one is observing to get below the surface and interpret the subtleties and meanings that the actors themselves might not attribute to them.
Limitations
The study has some limitations that must be considered when interpreting the findings. The potential for the researchers’ background and theoretical assumptions to bias the findings is a central problem in ethnography. The researcher is always a ‘cultural human being’ (Davies 2008) who brings his or her own values, attitudes and opinions into the field, which can be both a strength and a weakness in relation to data collection and analysis of the ethnography. The first author of the study is a registered nurse with many years’ experience working in health care. This means that the researcher knew the field as an insider, which can increase the researcher's access to the study arena, facilitating collection and analysis of the data. Conversely, too much familiarity can make it difficult to recognise and see things that we do not normally notice or have come to take for granted, i.e. leading to a certain blindness as to what is really going on, which could reduce the contextual and cultural understanding (Hastrup et al. 2011). The second author of the study has no previous health care experience but is an experienced implementation researcher who has studied health care and community‐based health services from many perspectives using a broad range of study approaches. Discussions between the two authors provided an opportunity to bring assumptions that were taken for granted to the surface and articulate, explain and critically appraise observations made in the emergency department. This process of reflection strengthened the trustworthiness of the analysis.
Another limitation of the study is the focus on only one department. This may affect the reliability and generalisability of the findings, at least from a natural science perspective (Davies 2008). Reliability in ethnographic studies can be strengthened by cross‐checking information by returning to the same topic under varying circumstances and comparing verbal assertions with observations. Although the practitioners in the emergency department performed collective activities and had developed a form of collective consciousness, the group will always encompass varying perspectives, something that the researcher must be aware of. Achieving reliability by repeating a study is not possible in ethnography because the participant researcher is an integral part of the study (Hasse 2011). By making the data collection and analysis process as transparent as possible, we have tried to make our reflexive experience visible. Generalisability of the findings in this study was sought in terms of theoretical inference (Hastrup et al. 2011), by being inspired by CHAT and describing the empirical concept of flow stops in the flow culture. These concepts can be transferred to and applied in other emergency departments.
Conclusion
This study found that a research‐supported guideline and screening routine were not used if they were perceived to stop the continuous flow of patients in the emergency department. A flow culture in the emergency department appears to have great impact on the use of evidence‐based practices in this environment. Hence, achieving an evidence‐based practice in an emergency department represents a substantial challenge.
Relevance to clinical practice
A strong focus on patient flow can have benefits such as reduced cycle times and shorter throughput intervals, but it may also create a culture that inhibits a more evidence‐based clinical practice in this setting. It is critically important to analyse the culture in which implementation occurs to address the challenges involved in the implementation of evidence‐based practices. Flow culture and flow stoppers are concepts that other researchers and practitioners will be able to use as possible concepts for their analysis and understanding of the culture of other departments and specialties. Understanding the local culture is necessary to realise ambitions for a more evidence‐based health care.
Contributions
Study design: JK; Data collection and analysis: JK; Manuscript preparation: JK, PN.
Funding
The project was funded by the Capital Region of Denmark.
Conflict of interest
The authors have no conflicts of interest to declare.
Acknowledgements
The authors would like to thank the managers and practitioners in the emergency department in Hvidovre Hospital, Denmark. They would also like to thank the Capital Region of Demark for their financial support for this project. Special thanks to Professor Cathrine Hasse from the Department of Education for communicative assistance.
References
- Aarons GA, Glisson C, Green PD, Hoagwood K, Kelleher KJ & Landsverk J (2012) The organizational social context of mental health services and clinician attitudes toward evidence‐based practice: a United States national study. Implementation Science 7, 56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen PT & Jensen J‐J (2010) Healthcare reform in Denmark. Scandinavian Journal of Public Health 38, 246–252. [DOI] [PubMed] [Google Scholar]
- Anneveld M, Van der Linden C, Grootendorst D & Galli‐Leslie M (2013) Measuring emergency department crowding in an inner city hospital in The Netherlands. International Journal of Emergency Medicine 6, 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker SJ, Shupe R & Smith D (2013) Driving efficient flow: three best‐practice models. Journal of Emergency Nursing 39, 481–484. [DOI] [PubMed] [Google Scholar]
- Bigham BL, Aufderheide TP, Davis DP, Powell J, Donn S, Suffoletto B, Nafziger S, Stouffer J & Morrison LJ (2010) Knowledge translation in emergency medical services: a qualitative survey of barriers to guideline implementation. Resuscitation 81, 836–840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies C (2008) Reflexive Ethnography. A Guide to Researching Selves and Others, 2nd edn Routledge, London, New York. [Google Scholar]
- Duffield CM, Conlon L, Kelly M, Catling‐Paull C & Stasa H (2010) The emergency department nursing workforce: local solutions for local issues. International Emergency Nursing 18, 181–187. [DOI] [PubMed] [Google Scholar]
- Ellen ME, Leon G, Bouchard G, Lavis JN, Ouimet M & Grimshaw JM (2013) What supports do health system organizations have in place to facilitate evidence‐informed decision‐making? A qualitative study. Implementation Science 8, 84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engeström Y (1987) Learning by Expanding: An Activity‐Theoretical Approach to Developmental Research. Orienta‐Konsultit Oy, Helsinki. [Google Scholar]
- Engeström Y (2001) Expansive learning at work: toward an activity theoretical reconceptualization. Journal of Education and Work 14, 133–156. [Google Scholar]
- Estabrooks CA, Floyd JA, Scott‐Findlay S, O'Leary KA & Gushta M (2003) Individual determinants of research utilization: a systematic review. Journal of Advanced Nursing 43, 506–520. [DOI] [PubMed] [Google Scholar]
- Fetterman D (1998) Ethnography: Step‐by‐Step. Applied Social Research Methods. Sage Publications, Stanford University. [Google Scholar]
- Fixsen DL, Naoom SF, Blase KA, Friedman RM & Wallace F (2005) Implementation Research: A Synthesis of the Literature. University of South Florida, Louis de la Parte Florida Mental Health Institute, The National Implementation Research Network, Tampa, FL: (FMHI Publication no. 231). [Google Scholar]
- Geertz C (1973) The Interpretation of Cultures. Basic Books, New York. [Google Scholar]
- Harrison MB, Graham ID, Van Den Hoek J, Dogherty EJ, Carley ME & Angus V (2013) Guideline adaptation and implementation planning: a prospective observational study. Implementation Science 8, 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasse C (2011) Kulturanalyse i organisationer. Begreber, metoder og forbløffende læreprocesser, 1. udgave [Cultural Analysis in Organizations. Concepts, Methods and Amazing Learning Processes, Part 1]. Samfundslitteratur, Frederiksberg. [Google Scholar]
- Hastrup K, Rubow C & Tjørnhøj‐Thomsen T (2011) Kulturanalyse. Kort fortalt [Cultural Analysis. In Brief]. Samfundslitteratur, Frederiksberg. [Google Scholar]
- Hsieh H‐F & Shannon SE (2005) Three approaches to qualitative content analysis. Qualitative Health Research 15, 1277–1288. [DOI] [PubMed] [Google Scholar]
- Kent B & McCormack B (2010) Clinical Context for Evidence‐Based Nursing Practice. Wiley‐Blackwell, Chichester. [Google Scholar]
- Kirk W & Nilsen P (2015) The influence of flow culture on nurses’ research use in emergency care: an ethnographic study. Clinical Nursing (The Danish Clinical Nursing) 29, 16–32. [Google Scholar]
- Lane D & Huseman E (2008) System dynamics mapping of acute patient flows. Journal of the Operational Research Society 59, 213–224. [Google Scholar]
- Leont'ev AN (1978) Activity, Consciousness, and Personality. Prentice‐Hall, Englewood Cliffs, NJ. [Google Scholar]
- McCormack B, Kitson A, Harvey G, Rycroft‐Malone J, Titchen A & Seers K (2002) Getting evidence into practice: the meaning of “context”. Journal of Advanced Nursing 38, 94–104. [DOI] [PubMed] [Google Scholar]
- Nilsen P (2010) Implementering. Teori och tillämping inom hälso‐& sjukvård [Implementation. Theory and Application in Health and Medicine]. Studentlitteratur, Lund. [Google Scholar]
- Nugus P & Forero R (2011) Understanding organizational work in the emergency department: An ethnographic approach. International Emergency Nursing 19, 69–74. [DOI] [PubMed] [Google Scholar]
- Nugus P, Forero R, McCarthy S, Mcdonnell G, Travaglia J, Hilman K & Braithwaite J (2014) The emergency department “carousel”: an ethnographically‐derived model of the dynamics of patient flow. International Emergency Nursing 22, 3–9. [DOI] [PubMed] [Google Scholar]
- O'Connor E, Gatien M, Weir C & Calder L (2014) Evaluating the effect of emergency department crowding on triage destination. International Journal of Emergency Medicine 7, 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Person J, Spiva L & Hart P (2013) The culture of an emergency department: an ethnographic study. International Emergency Nursing 21, 222–227. [DOI] [PubMed] [Google Scholar]
- Rabin BA & Brownson RC (2012) Developing the terminology for dissemination and implementation research In Dissemination and Implementation Research in Health (Brownson RC, Colditz GA. & Proctor EK. eds). Oxford University Press, New York, pp. 23–54. [Google Scholar]
- Rycroft‐Malone J (2008) Evidence‐informed practice: from individual to context. Journal of Nursing Management 16, 404–408. [DOI] [PubMed] [Google Scholar]
- Subbe CP, Kruger M, Rutherford P & Gemmel L (2001) Validation of a modified early warning score in medical admissions. Quarterly Journal of Medicine 94, 521–526. [DOI] [PubMed] [Google Scholar]
- Virkkunen J & Kuutti K (2000) Understanding organizational learning by focusing on “activity systems”. Accounting, Management and Information Technologies 10, 291–319. [Google Scholar]
- Volkert D, Berner Y, Berry E, Cederholm T, Coti B, Milne A, Palmblad J, Schneider S, Sobotka L & Stanga Z; DGEM (German Society for Nutritional Medicine) , Lenzen‐Grossimlinghaus R, Krys U, Pirlich M, Herbst B, Schütz T, Schröer W, Weinrebe W, Ockenga J & Lochs H; ESPEN (European Society for Parenteral and Enteral Nutrition) (2006) ESPEN guidelines on enteral nutrition: geriatrics. Clinical Nutrition 25, 330–360. [DOI] [PubMed] [Google Scholar]
- Vygotsky LS (1978) Mind in Society: The Development of Higher Psychological Processes. Harvard University Press, The United States of America. [Google Scholar]
- Yagamata‐Lynch LC (2010) Activity Systems Analysis Methods: Understanding Complex Learning Environments. Springer, New York, London. [Google Scholar]
- Yano EM (2008) The role of organizational research in implementing evidence‐based practice: QUERI series. Implementation Science 3, 29. [DOI] [PMC free article] [PubMed] [Google Scholar]


