Abstract
Objective
To describe the design and rationale of the Healthy Community Neighborhood Initiative (HCNI), a multi-component study to understand and document health risk and resources in a low-income and minority community.
Design
A community-partnered participatory research project.
Setting
A low-income, biethnic African American and Latino neighborhood in South Los Angeles
Participants
Adult community residents aged >18 years.
Main Outcome Measures
Household survey and clinical data collection; neighborhood characteristics; neighborhood observations; and community resources asset mapping.
Results
We enrolled 206 participants (90% of those eligible), of whom 205 completed the household interview and examination, and 199 provided laboratory samples. Among enrollees, 82 (40%) were aged >50 years and participated in functional status measurement. We completed neighborhood observations on 93 street segments; an average of 2.2 (SD=1.6) study participants resided on each street segment observed. The community asset map identified 290 resources summarized in a Community Resource Guide given to all participants.
Conclusions
The HCNI community-academic partnership has built a framework to assess and document the individual, social, and community factors that may influence clinical and social outcomes in a community at high-risk for preventable chronic disease. Our project suggests that a community collaborative can use culturally and scientifically sound strategies to identify community-centered health and social needs. Additional work is needed to understand strategies for developing and implementing interventions to mitigate these disparities.
Keywords: Design, Rationale, Community-Partnered Research, African American, Latino, Under-resourced Communities, Community Assets, Chronic Disease
Introduction
African Americans, Latinos, and adults from other racial/ethnic minority groups have higher rates and worse control of chronic conditions such as obesity, diabetes, cardiovascular disease and stroke than their White peers and face worse outcomes from these conditions.1-5 Residence in low-income, under-resourced communities is also associated with poorer chronic disease outcomes.1,2,6-10 At the individual and the community levels, many shared mechanisms may contribute to health inequities, among them lower educational attainment and income, higher rates of deleterious health behaviors, poorer access to health care and health-promoting resources, lower quality of care, and chronic stressors.11-14 There is limited understanding, however, of the best strategies for improving individual health outcomes and reducing health disparities in communities where physical and social conditions undermine efforts to prevent and manage chronic conditions.15-19 An emerging literature suggests that interventions developed through community-academic partnerships have the potential to translate evidence into practice to address health disparities in a manner that is both acceptable and sustainable in under-resourced communities.20-24
Community-partnered participatory research (CPPR) refers to partnering with communities to conduct research25,26 that facilitates knowledge-sharing between community and academic partners; incorporates community priorities into all phases of research; and builds community and academic capacity for conducting partnered research.26-28 Although community-engaged approaches show promise for improving population health and reducing disparities, there is only limited evidence on the impact and sustainability of these efforts.20,22,23,29,30
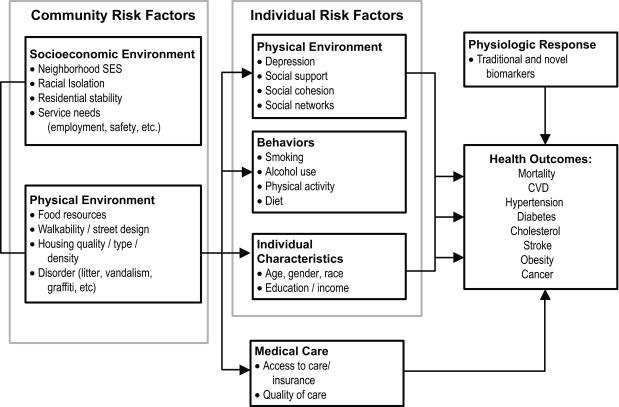
We present the rationale and design of the Healthy Community Neighborhood Initiative (HCNI), a CPPR project designed to address health disparities in a low-income bi-ethnic community in South Los Angeles (LA). The HCNI employs shared community and academic responsibility and authority to guide the selection, design, implementation, evaluation, and dissemination of efforts to intervene on local health inequalities (Figure 1).
Figure 1. Healthy Community Neighborhood Initiative conceptual framework.
Background, Conceptual Framework, and Rationale
In Los Angeles County, African Americans and Latinos are disproportionately affected by high rates of hazardous social conditions, preventable chronic disease, and poor quality of care that contributes to poor health outcomes.31,32 South LA, an area that is >95% Latino and African American, has the highest rates of obesity (37%), hypertension (32%), and diabetes (11%) in LA County.33 In addition to substantial preventable chronic disease, the community also has high rates of behavioral and social risk factors such as poor nutrition,33 smoking,33 sedentary lifestyle,34 low graduation rates,35 and high rates of unemployment,36 home foreclosure,37,38 and crime.39
In response to a series of reports that highlighted social and health inequities among African American and Latino residents of LA County,40 a community-academic partnership was formed to identify and intervene upon health disparities in a high-risk neighborhood in South LA. The collaborative was formed in 2008 between the Los Angeles Urban League (LAUL), Healthy African American Families Phase II (HAAF II), Charles R. Drew University (CDU), and the University of California Los Angeles (UCLA). Two more academic institutions—Cedars-Sinai Medical Center and LA Biomed/Harbor-UCLA Medical Center—joined the partnership when the UCLA Clinical and Translational Science Institute (CTSI) was funded in 2011.
The partners established a memorandum of understanding in 2009 that outlined project governance and procedures; data ownership, sharing and dissemination; and publication and presentation policies. All study protocols, informed consent forms, data collection instruments, and other documents were developed and revised iteratively during weekly or biweekly community-academic team meetings. The Charles Drew University human subjects’ protection committee approved the study.
The co-occurrence of clinical and social disparities highlights the need to address the social environments and physical conditions of the communities in which people live, individual risk factors for disease, and the clinical care they receive in order to influence their health outcomes. (Figure 1)41,42 Guided by this conceptual framework, the HCNI team identified the following three aims: 1) to understand clinical and social factors that might be intervened upon to influence health outcomes in this South LA community; 2) to examine patterns of chronic condition disease prevalence and control, biomarkers of stress and inflammation, and the relationship of biomarker levels to clinical and social outcomes; and 3) to engage community residents, agency representatives, and other stakeholders in collaborative data analysis, interpretation, and dissemination in order to set priorities for future intervention development.
Methods
The systematic data collection included a household survey and clinical assessment, neighborhood observations, and a community asset map. In recognition of prior evidence of earlier health deterioration among African Americans and Latinos,43 we incorporated survey and clinical measurements of geriatric syndromes and functional status among residents aged >50 years.
Recruitment
Eligibility was determined by study interviewers trained to screen participants in a linguistically and culturally appropriate manner and to sensitively and accurately assess their understanding of the research. Eligible participants were aged >18 years or an emancipated minor; English or Spanish speaking; and residents of the community and planned to remain in the community for the next 12 months. Between May 2012 and December 2013, we identified residents using publicly available listings and recruited participants using mailers, flyers, links on community websites, and through word-of-mouth, door-to-door visits, and presentations at community health fairs, churches, telephone town hall meetings, and on radio broadcasts.44
Household Survey
The household survey, conducted either in the participant’s home or at a community partner site, included three components: the adult interview, the health screening, and laboratory data collection.
Adult Interview
This face-to-face interview lasted approximately 60 minutes and included questions on: demographic characteristics; concerns around employment, education, safety, housing, and discrimination; clinical factors including medical conditions, health status, experience of care, health habits, and neighborhood perceptions. Most survey items were obtained from validated instruments. Because the study team was unable to find extant surveys that adequately captured the unmet social needs related to interventions and the expertise of the community partners, the partners developed a set of questions on this topic. Unmet clinical and social needs identified during the interview were flagged, referrals made to the appropriate health and social services, and follow-up of these concerns tracked within the study. We enrolled up to three adult residents from each household. To account for multiple participants within a household, we will include a household-level random effect in multivariable regression models that use these data.
Household Health Screening Physical Examination
The household health screening included measurement of participants’ height, weight, waist circumference,45 blood pressure,46 and heart rate in a standardized manner consistent with prior studies. For participants aged >50 years, we also measured grip strength47 and timed chair stands.48
Household Collection of Laboratory Data
For all participants, a trained nurse or phlebotomist performed a fingerstick to obtain bloodspots for hemoglobin (Hb), hemoglobin A1c (A1c), and C-reactive peptide (CRP). We used a CardioCheck PA machine (Polymer Technology Systems, Inc., 2010) to measure a non-fasting lipid panel.
Selected results from the clinical examination and point of care laboratory tests were recorded on a form for the participant with an explanation of the test and reference values. The participants received brief counseling about their findings at the end of the visit. The other blood spots were sent to an outside laboratory. A letter containing an explanation of the test results and reference values was sent to the participant, with a duplicate copy to share with their health care provider if requested.
Payment for Participation
Participants received a $25 gift card for completing the baseline interview and another $25 gift card for participation in the combined examination and laboratory phases of the study. Each participant also received a gift bag that included a Community Resource Guide and health-related items. Certificates of Completion and a note of thanks were sent to all participants on behalf of the study team.
Neighborhood Observations
To document residential neighborhood physical and social environments, we created a database of the street segments where HCNI participants resided.49,50 Each street segment spanned both sides of the street from one intersection to the next. Each team member completed a half-day training session, led by a graduate student with expertise in urban planning. We modified standardized protocols for the trainings.49,50 Each rating team recorded the characteristics of each street segment. The test-retest reliability statistics (Kappa) for a random 10% sample of street segments, with two selected teams rating the same street segment within an 8-week time period, was calculated.
Teams obtained information on the condition and quality of the following neighborhood characteristics: housing, street, sidewalks, overall aesthetics, traffic conditions, access to recreational facilities, other amenities, and physical disorder.51 A composite physical disorder scale was constructed using seven items: abandoned cars, garbage, drug paraphernalia, beer bottles, cigarettes, graffiti, and painted over graffiti.52 Spatial analyses were conducted using ArcGIS software (ESRI ArcGIS Desktop Redlands, CA Environmental Systems Research Institute) to geocode the residential street segments of HCNI participants and assign neighborhood characteristics.
Community Asset Mapping
The community asset map characterized local resources in order to link residents to needed health care and social services. The study team systematically updated resource lists previously collected by the community partners and determined the appropriateness of services for residents based on their health care and social service needs. The community asset map incorporated information on locally available health care resources, social services, recreational facilities, and the food environment.
Training and Mentoring
The study team placed special emphasis on training of team members and mentoring of students as a means of building both community and academic capacity for partnered research. All study personnel were IRB-certified for human subjects research and study participant confidentiality. Staff received training in the clinical examination, use and care of the equipment, collecting data in a respectful, accurate, and minimally invasive manner; cultural competency; and personal safety when conducting community research. Study team members also mentored nursing, medicine, and social work graduate students and post-doctoral fellows from CDU and UCLA.
Collaborative Data Analysis
University-based programmers and analysts worked with the study team to clean, review, and summarize data and respond to the questions posed at team meetings. To date, we have conducted partnered descriptive analyses of data from the household interviews, clinical data, neighborhood observations, and community assets.
Results
Among the 258 adults screened for eligibility, 29 (11%) were ineligible because they resided outside the study boundaries. Of the 229 eligible participants, 23 (10%) refused participation and 206 (90%) enrolled in the study. All 206 enrolled participants completed the interview; 205 (99%) completed the physical examination; and 199 (97%) completed the laboratory examination. Among enrollees, 82 (40%) were aged > 50 years and thus eligible for the functional status measurement; however, 8 participants (10%) were unable to perform the chair stand and another participant (1%) declined to participate in the chair stand (Table 1).
Table 1. Household survey, interviews and clinical examinations.
| Participants, n (%) | Unique households, n (%) | ||
| Participants/households screened for eligibility | 258 | 193 | |
| Ineligible | 29 (11) | - | |
| Eligible | 229 | ||
| Eligible but refused | 23 (10) | - | |
| Enrolled participantsa | 206 (90) | 144 (75) | |
| Household survey and laboratory data for enrolled participants | 206 | ||
| In-home adult interview | 206 (100) | - | |
| Physical examination | 205 (99) | - | |
| Complete laboratory data (lipids, A1c, CRP, total hemoglobin) b | 189 (92) | - | |
| Partial laboratory data (A1c, CRP, total hemoglobin) b | 10 (5) | - | |
| Functional status tests for participants > 50 years: | 82 | ||
| Grip strength completed | 81 (99) | - | |
| Chair stand completed | 71 (87) | - | |
| Unable to perform chair stand due to physical inability | 8 (10) | - | |
| Unable to perform chair stand due to household conditions | 1 (1) | - | |
| Refused or missing chair stand measurement | 2 (2) | - | |
a. In-home survey is a 60-minutes face-to-face interview, household health screening includes anthropomorphic, blood pressure measurements and laboratory data collection includes lipids, CRP, A1c, total hemoglobin measurements.
b. Refused (n=7), could not complete laboratory data collection for lipids due to mechanical problems (n=6) or insufficient sample (n=4).
Characteristics of the Enrolled Participants Compared with Surrounding Regions
Table 2 compares demographic and limited clinical characteristics of participants in the recruited sample with residents of the surrounding community using data obtained from administrative sources, including 2012 US Census Bureau American Community Survey census tract data; the 2011-2012 California Health Interview Survey (CHIS) health district data; and 2011-2012 CHIS Neighborhood Edition data.
Table 2. Characteristics of HCNI participants.
| HCNI Participants Total, N=206 | Community characteristicsa b d f | |
| %, Mean (SD) | % | |
| Demographic characteristics | ||
| Age, yearsa | ||
| 18-24 | 20 | 19 |
| 25-44 | 40 | 28 |
| 45-64 | 29 | 38 |
| ≥65 | 11 | 15 |
| Sex b | ||
| Female | 71 | 55 |
| Race/Ethnicity b | ||
| African American | 75 | 67 |
| Latino | 25 | 25 |
| Other race/ethnicity | 0 | 8 |
| High school graduateb | 77 | 80 |
| Marital statusa c | ||
| Married/living with partner | 34 | 31 |
| Widowed/divorced/separated | 24 | 23 |
| Never married | 42 | 46 |
| Language spoken at home a | ||
| English | 79 | 62 |
| Spanish | 21 | 31 |
| Other languages | 0 | 7 |
| Household size, persons,d | 3.3 (1.88) | 3.2 |
| Employment statusb | ||
| Full time/part time/self-employed | 37 | 53 |
| Unemployed/other e | 63 | 47 |
| Chronic conditions (self-report)f | ||
| High blood pressure | 39 | 33 |
| Asthma, CLD, emphysema | 14 | 11 |
| Diabetes | 14 | 9 |
| Body mass indexf | ||
| Obese (>30) | 53 | 34 |
a. Source: 2012 Census Bureau American Community Survey Census Tract.
b. Source: 2011-2012 California Health Interview Survey Neighborhood Edition for the zip code.
c. Marital status estimates for community characteristics include residents aged >15 years.
d. Source: 2010 Profile of General Population and Housing Characteristics: 2010 Demographic Profile Data.
e. The other category includes respondents not considered part of the labor force (students, homemakers, disabled adults, and retired workers).
f. Source: 2011-2012 California Health Interview Survey for the health district.
Neighborhood Observations
The observers reviewed 93 street segments, with a mean of 37 street segments per observer. On average, 2.2 (SD=1.6) study participants resided on each street segment reviewed. A reliability test of a random 10% sample of street segments found high inter-rater reliability between the two selected rating teams for the seven physical disorder components (Kappa=.843). Each observer spent an average of 5.6 days (SD=2.7) in the field and day length ranged from four to seven hours (Table 3).
Table 3. Neighborhood characteristics obtained from street segments observed.
| Street segments observed, n | 93 |
| Observers, n | 6 |
| Streets segments observed per observer (range: 11 – 62) | |
| Mean (SD) | 37 (20.2) |
| Median (IQR) | 32 (28, 52) |
| Total person days in fielda | 28 |
| Days in field per observer, mean (SD) | 5.6 (2.7) |
| Residents per street segment (range: 1 – 9) | |
| Mean (SD) | 2.2 (1.6) |
| Median (IQR) | 2 (1,3) |
| Kappa statistic between rating teamsb | .843 |
a. Days in field ranged from 4 to 7 hours.
b. Reliability test of a random sample of 10% (n=10) street segments for components of disorder scale (abandoned cars, garbage, drug paraphernalia, beer bottles, cigarettes, graffiti, and painted over graffiti).
Community Asset Map
The community asset map identified 290 resources in 10 categories that were reviewed and summarized in a Health, Wellness and Community Resource Guide by study team members (Table 4); (https://courtneyrporter.uberflip.com/i/326031).
Table 4. Categories of neighborhood asset mapping.
| Category | Content |
| Los Angeles County general contacts | |
| Elected officials | |
| Los Angeles county hotlines | |
| Los Angeles fire and police departments | |
| Health and wellness resources | |
| Los Angeles Urban League health programs | |
| Health centers/clinics, hospitals | |
| Trauma centers, emergency departments, Urgent care units | |
| Mental health/counseling | |
| Chronic conditions | |
| Kidney disease | |
| Dental | |
| Smoking cessation | |
| Faith-based organizations | |
| African American Churches, Latino/Hispanic Churches | |
| Food and nutrition | |
| Grocery stores | |
| Farmers’ market | |
| Fitness and recreation | |
| Gyms/fitness clubs | |
| Parks and recreation | |
| Senior resources | |
| Senior centers | |
| Youth and parenting assistance | |
| Parenting | |
| Child abuse | |
| Legal aid | |
| Legal aid agencies | |
| Education | |
| Adult school and mentoring/tutoring centers | |
| Employment and financial assistance | |
| Financial aid | |
| Job assistance | |
| Housing | |
| Housing assistance and emergency shelter | |
| Neighborhood hazards | |
| Liquor stores, massage parlors, sex stores/stores that sell pornography, bars | |
Conclusions
The HCNI partnership has built a framework for partnered research to address health disparities in a community with high rates of preventable chronic disease and many social risks. We first developed a baseline assessment that tailored clinical research methods to the needs of this community. The results presented here demonstrate the feasibility of partnering in order to bring both community and academic expertise to bear on the most salient problems affecting these communities. Analyses will be conducted separately for each of the data collection efforts and integrated into a uniform multifaceted description of the community that can be used to design meaningful and acceptable interventions.
This study has some potential limitations. We are focused on a small geographic area that may not be representative of South LA overall, and the study includes a relatively small number of participants. This is an area, however, with historically low rates of participation in clinical research, and our study suggests that it is feasible to identify and recruit study participants for health research in this community. Once enrolled, participants had very high rates of completion of all components of the study.44 We also recognize that some groups within the community were under-represented, notably older Latino men. The study team is working to develop new approaches to outreach and recruitment of older Latino and African American men. An additional concern is that chronic conditions were self-reported and may have been under-, over-, or mis-diagnosed. We did not have resources to compare self-report to medical record data; however, we selected survey items that were shown to have good concordance with the medical record in prior studies.53
Findings from this research will be used to develop community-partnered interventions. With experiential and measurement competence from community and academia, we will identify and develop specific patient-centered and community-feasible strategies for ensuring that residents—those at risk for preventable disease and those with treatable chronic conditions—receive services and care needed to optimize health outcomes.
Acknowledgments
This study was funded, in part, by National Clinical and Translational Science #UL1TR000124 and the USC/UCLA Center of Biodemography #5P30AG017265-13. Dr. Arleen F. Brown certifies that all persons named in the Acknowledgment section have provided permission to be named. We would like to acknowledge the support of Juan Barron, Nancy Hernandez, Blanca Corea, and Linda Thompson.
References
- 1. Haan M, Kaplan GA, Camacho T. Poverty and health. Prospective evidence from the Alameda County Study. Am J Epidemiol. 1987;125(6):989-998. [DOI] [PubMed] [Google Scholar]
- 2. . Kaplan GA. People and places: contrasting perspectives on the association between social class and health. International journal of health services : planning, administration, evaluation. 1996;26(3):507-519. [DOI] [PubMed]
- 3. Kington RS, Smith JP. Socioeconomic status and racial and ethnic differences in functional status associated with chronic diseases. Am J Public Health. 1997;87(5):805-810. 10.2105/AJPH.87.5.805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- 5. Mead H, Cartwright-Smith L, Jones K, Ramos C, Siegel B, Woods K. Racial and Ethnic Disparities in US Health Care: A Chartbook. Washington, DC: Commonwealth Fund; 2008. [Google Scholar]
- 6. Bosma H, van de Mheen HD, Borsboom GJ, Mackenbach JP. Neighborhood socioeconomic status and all-cause mortality. Am J Epidemiol. 2001;153(4):363-371. 10.1093/aje/153.4.363 [DOI] [PubMed] [Google Scholar]
- 7. Diez Roux AV, Merkin SS, Arnett D, et al. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345(2):99-106. 10.1056/NEJM200107123450205 [DOI] [PubMed] [Google Scholar]
- 8. . Marmot MG, Fuhrer R, Ettner SL, Marks NF, Bumpass LL, Ryff CD. Contribution of psychosocial factors to socioeconomic differences in health. The Milbank quarterly. 1998;76(3):403-448, 305. 10.1111/1468-0009.00097 [DOI] [PMC free article] [PubMed]
- 9. Smith GD, Hart C, Watt G, Hole D, Hawthorne V. Individual social class, area-based deprivation, cardiovascular disease risk factors, and mortality: the Renfrew and Paisley Study. J Epidemiol Community Health. 1998;52(6):399-405. 10.1136/jech.52.6.399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Brown AF, Liang LJ, Vassar SD, et al. Neighborhood socioeconomic disadvantage and mortality after stroke. Neurology. 2013;80(6):520-527. 10.1212/WNL.0b013e31828154ae [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. . Lynch JW, Kaplan GA, Salonen JT. Why do poor people behave poorly? Variation in adult health behaviours and psychosocial characteristics by stages of the socioeconomic lifecourse. Social science & medicine (1982). Mar 1997;44(6):809-819. [DOI] [PubMed]
- 12. Lynch JW, Smith GD, Kaplan GA, House JS. Income inequality and mortality: importance to health of individual income, psychosocial environment, or material conditions. BMJ. 2000;320(7243):1200-1204. 10.1136/bmj.320.7243.1200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Williams DR, Jackson PB. Social sources of racial disparities in health. Health Aff (Millwood). 2005;24(2):325-334. 10.1377/hlthaff.24.2.325 [DOI] [PubMed] [Google Scholar]
- 14. Institute of Medicine Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care (full printed version). Washington, DC: The National Academies Press; 2003. [PubMed] [Google Scholar]
- 15. Olshansky SJ, Antonucci T, Berkman L, et al. Differences in life expectancy due to race and educational differences are widening, and many may not catch up. Health Aff (Millwood). 2012;31(8):1803-1813. 10.1377/hlthaff.2011.0746 [DOI] [PubMed] [Google Scholar]
- 16. Harper S, MacLehose RF, Kaufman JS. Trends in the black-white life expectancy gap among US states, 1990-2009. Health Aff (Millwood). 2014;33(8):1375-1382. 10.1377/hlthaff.2013.1273 [DOI] [PubMed] [Google Scholar]
- 17. . Karas Montez J, Hayward MD Cumulative Childhood Adversity, Educational Attainment, and Active Life Expectancy Among U.S. Adults. 10.1007/s13524-013-0261-x. April 1, 2014 2014;51(2):413-435. [DOI] [PMC free article] [PubMed]
- 18. Singh GK, Siahpush M. Widening rural-urban disparities in life expectancy, U.S., 1969-2009. Am J Prev Med. 2014;46(2):e19-e29. 10.1016/j.amepre.2013.10.017 [DOI] [PubMed] [Google Scholar]
- 19. . Elo IT, Beltrán-Sánchez H, Macinko J The Contribution of Health Care and Other Interventions to Black–White Disparities in Life Expectancy, 1980–2007. Population Research and Policy Review. February 1, 2014 2014;33(1):97-126. [DOI] [PMC free article] [PubMed]
- 20. Wallerstein N, Duran B. Community-based participatory research contributions to intervention research: the intersection of science and practice to improve health equity. Am J Public Health. 2010;100(S1)(suppl 1):S40-S46. 10.2105/AJPH.2009.184036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. .Community-Based Participatory Research for Health: From Process to Outcomes. 2nd Edition ed. San Francisco, CA: Jossey-Bass; 2008.
- 22. Miranda J, Ong MK, Jones L, et al. Community-partnered evaluation of depression services for clients of community-based agencies in under-resourced communities in Los Angeles. J Gen Intern Med. 2013;28(10):1279-1287. 10.1007/s11606-013-2480-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wells KB, Jones L, Chung B, et al. Community-partnered cluster-randomized comparative effectiveness trial of community engagement and planning or resources for services to address depression disparities. J Gen Intern Med. 2013;28(10):1268-1278. 10.1007/s11606-013-2484-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. . Wells K, Jones L, Chung B, et al. Erratum to: Community-Partnered Cluster-Randomized Comparative Effectiveness Trial of Community Engagement and Planning or Resources for Services to Address Depression Disparities. Journal of general internal medicine. November 1, 2013 2013;28(11):1534. [DOI] [PMC free article] [PubMed]
- 25. . Ferre CD, Jones L, Norris KC, Rowley DL The Healthy African American Families (HAAF) project: from community-based participatory research to community-partnered participatory research. Ethn Dis. Winter 2010;20(1 Suppl 2):S2-1-8. [PMC free article] [PubMed]
- 26. Jones L, Wells K. Strategies for academic and clinician engagement in community-participatory partnered research. JAMA. 2007;297(4):407-410. 10.1001/jama.297.4.407 [DOI] [PubMed] [Google Scholar]
- 27. Minkler M, Blackwell AG, Thompson M, Tamir H. Community-based participatory research: implications for public health funding. Am J Public Health. 2003;93(8):1210-1213. 10.2105/AJPH.93.8.1210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Norris KC, Brusuelas R, Jones L, Miranda J, Duru OK, Mangione CM. Partnering with community-based organizations: an academic institution’s evolving perspective. Ethn Dis. 2007;17(1)(suppl 1):S27-S32. [PubMed] [Google Scholar]
- 29. Viswanathan M, Ammerman A, Eng E, et al. Community-based participatory research: assessing the evidence. Evid Rep Technol Assess (Summ). 2004;(99):1-8. [PMC free article] [PubMed] [Google Scholar]
- 30. Wells K, Jones L. “Research” in community-partnered, participatory research. JAMA. 2009;302(3):320-321. 10.1001/jama.2009.1033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. . Los Angeles County Department of Public Health - Office of Health Assessment and Epidemiology Mortality in Los Angeles County. Leading Causes of Death and Premature Death with Trends for 2002-2011. Los Angeles, CA: Los Angeles County Department of Public Health, Office of Health Assessment and Epidemiology; August 2014 2014. [Google Scholar]
- 32. Senerfitt J, Long A, Shih M, Teutsch S. How Social and Economic Factors Affect Health. Los Angeles, CA: Los Angeles County Department of Public Health January; 2013. [Google Scholar]
- 33. California Health Interview Survey. CHIS 2011-2012 Adult Public Use File. Los Angeles, CA: UCLA Center for Health Policy Research; 2012. [Google Scholar]
- 34. California Health Interview Survey. CHIS 2009 Adult Public Use File. Los Angeles, CA: UCLA Center for Health Policy Research; 2009. [Google Scholar]
- 35. . Ong P. Neighborhood Assessment of Park Mesa Heights. Los Angeles, CA UCLA School of Public Affairs; May 2010 2010. [Google Scholar]
- 36. United States Census Bureau American Community Survey Employment Status Census Tract. Washington, DC: United States Census Bureau; 2012. [Google Scholar]
- 37. California RAND. Housing Foreclosure Statistics. Los Angeles, CA: RAND California; 2012. [Google Scholar]
- 38. .RealtyTrac®. Los Angeles Real Estate Trends & Market Information. Los Angeles, CA: RealtyTrac® October 2014 2014.
- 39. Advancement Project Community Safety Scorecard City of Los Angeles 2011. Los Angeles, CA: Advancement Project; 2011. [Google Scholar]
- 40. The Los Angeles Urban League, United Way of Greater Los Angeles The State of Black Los Angeles. Los Angeles: CA July; 2005. [Google Scholar]
- 41. Goering J, Feins J. What have we learned from housing mobility and poverty deconcentration. Choosing a better life? Evaluating the Moving to Opportunity social experiment. Washington, DC: Urban Institute Press; 2000:3-36. [Google Scholar]
- 42. Olsen EO. Housing programs for low-income households. In: Moffitt R, ed. Means-tested transfer programs in the United States. Chicago, IL: University of Chicago Press; 2003:365-442. 10.7208/chicago/9780226533575.003.0007 [DOI] [Google Scholar]
- 43. Balfour JL, Kaplan GA. Neighborhood environment and loss of physical function in older adults: evidence from the Alameda County Study. Am J Epidemiol. 2002;155(6):507-515. 10.1093/aje/155.6.507 [DOI] [PubMed] [Google Scholar]
- 44. Sankaré IC, Bross R, Brown AF, et al. Strategies to Build Trust and Recruit African American and Latino Community Residents for Health Research: A Cohort Study. Clin Transl Sci. 2015;8(5):412-420; Epub ahead of print. 10.1111/cts.12273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.International Chair on Cardiometabolic Risk. Waist Circumference Measurement Guidelines - Healthcare Professional. 2011; http://www.myhealthywaist.org/fileadmin/pdf/WCMG-Healthcare_Professional.pdf. Accessed May 1, 2012.
- 46. Charles R. Drew University of Medicine and Science. Clinical and Translational Research Center Standard Operating Procedures for Vital Signs. Los Angeles, CA: Charles R. Drew University; 2012:1-5. [Google Scholar]
- 47. Patterson Medical SP. JAMAR Plus Hand Dynamometer User Guide. Patterson Medical, Sammons Preston; 2014:1-13. [Google Scholar]
- 48. Bennell K, Dobson F, Hinman R. Measures of physical performance assessments: Self-Paced Walk Test (SPWT), Stair Climb Test (SCT), Six-Minute Walk Test (6MWT), Chair Stand Test (CST), Timed Up & Go (TUG), Sock Test, Lift and Carry Test (LCT), and Car Task. Arthritis Care Res (Hoboken). 2011;63(S11)(suppl 11):S350-S370. 10.1002/acr.20538 [DOI] [PubMed] [Google Scholar]
- 49. Sastry N, Pebley AR. Non-Response in the Los Angeles Family and Neighborhood Survey. Santa Monica, CA: RAND; 2003. [Google Scholar]
- 50. Evenson KR, Sotres-Alvarez D, Herring AH, Messer L, Laraia BA, Rodríguez DA. Assessing urban and rural neighborhood characteristics using audit and GIS data: derivation and reliability of constructs. Int J Behav Nutr Phys Act. 2009;6(1):44. 10.1186/1479-5868-6-44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Sampson RJ, Raudenbush SW. Systematic social observation of public spaces: A new look at disorder in urban neighborhoods. Am J Sociol. 1999;105(3):603-651. 10.1086/210356 [DOI] [Google Scholar]
- 52. Jones M, Pebley AR, Sastry N. Eyes on the Block: Measuring Urban Physical Disorder Through In-Person Observation. Soc Sci Res. 2011;40(2):523-537. 10.1016/j.ssresearch.2010.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373-383. 10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]