Abstract
Objective
Our objective was to determine the effectiveness of combining positive affect and self-affirmation strategies with motivational interviewing in achieving blood pressure control among hypertensive African Americans (AA) compared with AA hypertensives in an education-only control group.
Design
Randomized trial.
Setting
Ambulatory practices in the South Bronx and Harlem, New York City.
Participants
African American adults with uncontrolled hypertension.
Interventions
Participants were randomized to a positive affect and self-affirmation intervention or an education control group. The positive affect and self-affirmation intervention involved having participants think about things that made them happy and that reminded them of their core values on a daily basis. These strategies were reinforced every two months through motivational interviewing. The control arm received a workbook of strategies on blood pressure control. All participants were called every two months for one year.
Main Outcomes
Blood pressure control rate.
Results
A total of 238 participants were randomized. The average age was 56 ± 11 years, approximately 70% were female, 80% were not married, and up to 70% had completed high school. There was no difference in control rates between the intervention and the control group. However, at one year, female participants were more likely to be controlled. Participants with high depressive symptoms or high perceived stress at baseline were less likely to be controlled.
Conclusions
While this study did not demonstrate an intervention effect, it does provide important insight into the psychosocial factors that may underlie blood pressure control in African Americans. Implications for future behavioral intervention trials are discussed.
Keywords: African Americans, Blood Pressure, Medication Adherence, Positive Affect, Self-Affirmation, Motivational Interviewing
Introduction
Compared with Caucasians, African Americans are more likely to have uncontrolled blood pressures (BP).1 Medication adherence is one of the most important determinants of blood pressure control, yet one that is often most challenging to achieve.2 Even when access to medication is taken into consideration, medication adherence remains problematic among African Americans.3 This calls for interventions that tackle other putative factors that impact medication adherence. The Counselling African Americans to Control Hypertension study (CAATCH) identified perceived discrimination as a factor associated with poor medication adherence. In that study, stress and depressive symptoms were mediators of the relationship between perceived discrimination and adherence.4 Charlson et al reported associations between perceived stress, depressive symptoms, and low social support with medication adherence.5 Therefore, interventions that are designed to improve blood pressure control rates in African Americans must address these barriers.
The objective of the study, Trial Using Motivational Interviewing and Positive Affect and Self-Affirmation in African Americans with Hypertension (TRIUMPH), was to improve blood pressure control by targeting self-efficacy, a major determinant of medication adherence.6 Rooted in social cognitive theory, self-efficacy describes the confidence in one’s ability to take action to overcome barriers. It is a major cornerstone of health behavior change.7,8 The techniques used in TRIUMPH included motivational interviewing, positive affect induction, and self-affirmation manipulation. The approach to motivational interviewing was based on the work done by Miller and Rollnick.9-12 The approach to positive affect induction was based on positive affect theory, which states that positive affect enables individuals to be more open-minded, motivated, and responsive to health messages thus, fostering their ability to achieve their personal goals.13,14 Positive affect may increase self-efficacy by increasing the desirability of the ultimate health behavior goal, the perceived link between the steps needed to accomplish this goal, and the belief that this effort will ultimately lead to the desired goal.15 Self-affirmation theory describes the importance of focusing on personal strength and core values as a method of counteracting negative responses to stress and maintaining psychological well-being.16,17 Self-affirmation can be achieved by having people focus on their core values or on things that hold importance for them.18,19 By drawing on previous experiences of success, self-affirmation may increase self-efficacy for health behavior change.20 The underlying premise of TRIUMPH is that an intervention based on inducing positive affect and self-affirmation will improve medication adherence and therefore, achieve better blood pressure control.
Methods
The study design and methods of TRIUMPH have been described in greater detail elsewhere.10 Briefly, TRIUMPH was a two-arm randomized controlled trial. Adult patients who received care in federally qualified health centers and community ambulatory practices located in the South Bronx and Harlem, New York City were recruited. These communities were selected because they have higher rates of hypertension compared with other communities in New York City.21 Eligibility was determined via the electronic medical record system at these sites. Eligibility included self-identification as African American or Black, having a diagnosis of hypertension, being on at least one antihypertensive medication and having an elevated blood pressure reading at the time of recruitment.
After providing consent, participants completed baseline assessments that included demographic characteristics, medications, comorbidity using the Charlson Comorbidity Index,22 hypertension history, as well as a battery of psychosocial measures. Psychosocial assessments were administered at baseline and at 12 months. Depressive symptoms were assessed with the Center for Epidemiologic Studies Depression (CES-D) scale, which is a reliable, and well-validated 20-item, self-report depression scale developed to identify depressive symptoms in the general population.23 A 26-item Medication Adherence Self-Efficacy Scale was used to measure self-efficacy.6 Perceived stress was measured with the Perceived Stress Scale (PSS) a 10-item scale that measures the degree to which situations are appraised as stressful.24 Affect was measured with the Positive and Negative Affect Scale (PANAS), which has two 10-item mood scales and was developed to provide brief measures of positive and negative affect, respectively.25 Social support was measured with the Medical Outcomes Study-Social Support Survey (MOS-SS), which measures multiple dimensions of social support.26
Research assistants were trained to deliver the intervention components. Given the interactive nature of the study, neither the participants nor the research assistants could be blinded to the study intervention. Upon completion of baseline assessments, participants were randomized in a 1:1 ratio to either an active intervention group or an education-based control group. Randomization group was not disclosed to the participants’ providers. In an effort to equalize knowledge about hypertension, participants in both arms were given a hypertension workbook. This workbook was developed during a previous study in African Americans with hypertension and provided education about the etiology of hypertension, treatment options, and lifestyle changes that one could take to improve blood pressure control and to support goals setting.27 Participants in both groups were also asked to develop a behavior contract that specified steps that they would take in an effort to improve their ability to take their blood pressure medications as prescribed.
Participants in the intervention arm received the educational workbook plus a positive affect and self-affirmation induction protocol. The positive affect strategy entailed focusing on positive thoughts that made them feel good throughout their day or when they encountered stressful situations. They also received unexpected gift cards on a bimonthly basis as another method of inducing positive affect. Providing small and unexpected gifts is based on the work of Isen.15,28 The self-affirmation intervention was adapted based on the work of Steele and colleagues.29 Participants were instructed to think of core values and things that made them proud whenever they encountered stressful situations that may make it difficult for them to adhere to their medications. Participants in the intervention group also received motivational interviewing based counseling. The motivational interviewing counseling for medication adherence included the following steps: 1) an assessment of the motivation and confidence for medication adherence; 2) eliciting barriers to adherence; 3) eliciting the ‘pros’ and ‘cons’ of any concerns; 4) a menu of options to address any barriers or concerns about improving medication adherence; and 5) a re-assessment of their values and goals and linking their current health behavior pattern to their core values and life goals. These strategies were reinforced during bimonthly telephone calls. Participants in both groups received bimonthly calls during a 12-month follow up period. During these calls, they were asked to describe interim events such as changes in medications, hospital admissions or emergency room visits, and any major stressful life events.
Outcomes
The primary outcome was blood pressure control rate at 12 months. Blood pressure (BP) was assessed with a valid automated digital BP monitor (BPTru),30,31 following the American Heart Association guideline.32 Patients were categorized as having controlled BP if they had an average BP that fulfilled the Seventh Joint National Committee on Detection, Evaluation and Treatment of High Blood Pressure (JNC-7) criteria of SBP < 130 and DBP < 80 mm Hg (for patients with diabetes or chronic kidney disease); or SBP < 140 and DBP < 90 mm Hg (for all other patients).33 JNC-7 was used because the study predates the release of JNC-8.34
The primary outcome was blood pressure control defined as having both systolic and diastolic blood pressure readings in target range. Therefore, a composite outcome variable called “success” was used in our analyses and operationalized as blood pressure <140/90 mm Hg.5
Changes from baseline in psychosocial variables were analyzed. An increase in social support as measured by the MOS or an increase in positive affect as measured by the PANAS positive affect scale was designated as a positive change or improvement in psychosocial status. This was operationalized as an increase greater than the 75th percentile between baseline and follow-up on these scales. A decrease below the 25th percentile for these variables was considered a negative change in psychosocial status. Similarly, a decrease in depressive symptoms as measured by the CESD, in stress as measured by the PSS, or in negative affect as measured by the PANAS negative affect scale was denoted as a positive change in psychosocial status. This was operationalized as a decrease greater than the 25th percentile between baseline and follow-up. An increase in these variables above the 75 percentile was classified as a negative change. All changes were calculated relative to baseline values.
Statistical Analysis
Parameters for sample size calculation included a power of 80% and a standard test level of .05. Based on our pilot data, it was expected that 57% in the intervention group would achieve target blood pressure control compared with 39% in the control. Therefore, 85 patients per group, or 170 overall, were estimated. A conservative loss to follow-up rate of 15% was predicted and the sample size was increased to accommodate for this potential loss. Chi square and student’s t-test were used to evaluate sociodemographic, clinical, and psychological differences between the two groups at baseline for categorical and continuous data, respectively. Univariate logistic regression was conducted to identify sociodemographic and psychological predictors of blood pressure control. Significant predictors were included along with the group allocation in a final multivariate model to evaluate the effect of the active intervention. All results are based on an intent-to-treat analysis. Analyses were performed using the Statistical Package for the Social Sciences (SPSS) windows software version 22.0. The study was approved by Weill Cornell’s institutional review board on ethical conduct of research.
Results
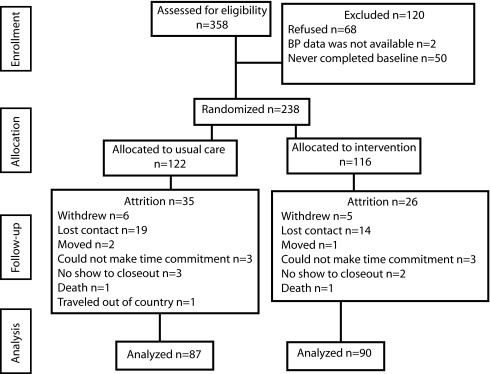
As shown in Figure 1, a total of 238 participants met eligibility criteria and were randomized. There were no statistically significant differences in demographic or clinical variables between the two groups (Table 1). The average age of all patients was 56 ± 11, approximately 70% were female, 80% were not married, and up to 70% completed high school. Both groups reported similar average duration of hypertension of 12 years. There was no difference in the number of comorbid conditions between the control (35.6%) and the experimental group (28.7%). There was no significance difference with regard to recent life events, depressive symptoms, self-efficacy, social support, or affect. The only significant difference emerged in the Perceived Stress Scale, with participants in the intervention group reporting higher levels of stress compared to controls (P<.05) at baseline (Table 1).
Figure 1. Numbers of participants per enrollment, allocation follow-up and analysis.
Table 1. Baseline characteristics and changes in psychosocial variables between baseline and follow up.
| Positive affect, motivational interviewing and self-affirmation group, n=90 | Educational/behavioral contract group (controls), n=87 | t/ χ2 | P | |
| Sociodemographic | ||||
| Age | 55.45 ( ± 9.26) | 58.01 ( ± 10.39) | 1.803 | .073 |
| Sex (female) | 67.4% | 70.3% | 0.190 | .756 |
| Marital status (married) | 19.8% | 20.8% | 0.030 | >.999 |
| Completed high school | 64.3% | 71.9% | 1.244 | .277 |
| Clinical | ||||
| Systolic blood pressure | 138 ( ± 18) | 140 ( ± 17) | .412 | .681 |
| Diastolic blood pressure | 81 ( ± 11) | 80 ( ± 12) | .213 | .832 |
| Charlson Comorbidity Index (CCI>3) | 28.7% | 35.6% | .902 | .408 |
| BMI | 34.87 ( ± 8.61) | 34.12 ( ± 8.27) | .355 | .724 |
| Hypertension duration, years | 11.69 ( ± 11.09) | 13.61 ( ± 11.72) | 1.156 | .249 |
| Family history | 81.9% | 83.3% | .060 | .843 |
| Psychosocial score | ||||
| Life events | 48.8% | 45.2% | .209 | .756 |
| Depression (CES-10) | 9.80 ( ± 6.59) | 8.32 ( ± 5.75) | 1.626 | .106 |
| Self-efficacy scale (MASES) | 37.87 ( ± 9.33) | 38.28 ( ± 7.92) | .330 | .742 |
| Morisky adherence scale | 2.82 ( ± 1.14) | 2.95 ( ± 1.03) | .813 | .417 |
| Social support scale (MOS) | 74.99 ( ± 23.85) | 71.58 ( ± 27.58) | .892 | .373 |
| PANAS – positive affect | 35.93 ( ± 9.38) | 38.10 ( ± 8.86) | 1.543 | .125 |
| PANAS – negative affect | 19.98 ( ± 8.13) | 18.68 ( ± 8.10) | 1.048 | .296 |
| Perceived stress scale (PSS) | 16.14 ( ± 7.75) | 13.23 ( ± 7.54) | 2.549 | .012 |
| Positive changes in psychosocial variables between baseline and 12 months | ||||
| Increased social support | 28.1% | 22.7% | .703 | .449 |
| Decreased depressive symptoms | 25.6% | 21.6% | .392 | .601 |
| Increased positive affect | 27.5% | 21.8% | .721 | .472 |
| Decreased negative affect | 26.1% | 20.8% | .755 | .400 |
| Decreased perceived stress | 25.6% | 19.1% | 1.075 | .370 |
| Negative changes in psychosocial variables between baseline and 12 months | ||||
| Decreased social support | 33.0% | 17.7% | 5.692 | .026 |
| Increased depressive symptoms | 26.7% | 25.8% | .022 | >.999 |
| Decreased positive affect | 27.5% | 23.0% | .451 | .593 |
| Increased negative affect | 29.3% | 22.8% | 1.084 | .327 |
| Increased perceived stress | 23.3% | 22.3% | .021 | >.999 |
Predictors of Blood Pressure Control
On univariate analysis, sex, baseline depressive symptoms and perceived stress scores emerged as predictors of blood pressure control at one year (Table 2). Female participants had a higher odds (OR=2.46, CI=1.14-5.29, P=.021) of blood pressure control. Greater depressive symptoms (OR=.92, CI=.87-.98, P=.005) and greater perceived stress scores (OR=.95, CI=.90-.99, P=.027) were associated with lower odds of blood pressure control at 12-month follow-up. When significant baseline predictors were entered in the final multivariate model, only female gender (P=.01) and depressive symptoms (P=.047) remained significant predictors of blood pressure control at 12 months (Table 3).
Table 2. Univariate predictors of success.
| Characteristics | Unadjusted OR | Confidence Interval | P |
| Sociodemographic | |||
| Age (increase by 1 year) | 1.04 | 1.00-1.08 | .051 |
| Sex (female) | 2.46 | 1.14-5.29 | .021 |
| Marital status (married) | .52 | .22-1.20 | .126 |
| Education (> high school) | .28 | .26-1.47 | .280 |
| Clinical | |||
| Charlson comorbidity index (CCI>3) | 1.89 | .72-4.99 | .196 |
| BMI | .97 | .90-1.05 | .470 |
| Hypertension duration | .80 | .96-1.03 | .797 |
| Presence of symptoms | 1.04 | .46-2.36 | .935 |
| Family history | .69 | .22-2.14 | .516 |
| Psychosocial | |||
| Life events | .74 | .34-1.64 | .463 |
| Depression | .92 | .87-.98 | .005 |
| Medication adherence self efficacy (MASES) | 1.01 | .97-1.06 | .605 |
| Morisky adherence scale | .92 | .64-1.33 | .668 |
| Medical outcome social support scale (MOS) | 1.00 | .99-1.01 | .948 |
| PANAS – positive affect | .99 | .94-1.03 | .513 |
| PANAS – negative affect | .96 | .92-1.01 | .116 |
| Perceived stress scales (PSS) | .95 | .90-.99 | .027 |
Table 3. Multivariate analysis of success.
| Predictors | Adjusted OR | Confidence interval | P |
| Age | 1.04 | 1.00-1.09 | .070 |
| Sex (female) | 2.95 | 1.29-6.73 | .010 |
| Depression (Cesd10) | .92 | .85-1.00 | .047 |
| Perceived stress scales (PSS) | 1.00 | .93-1.08 | .969 |
| Randomization group | 1.33 | .57-3.10 | .503 |
Model adjusted for significant univariate predictors (age, sex, depression and perceived stress scores).
Success is defined as achieving the outcome of blood pressure <140/90 mm Hg.
In an intent-to-treat analysis, 82% of patients in both arms achieved blood pressure control at 12 months (respectively, 82.2% of controls vs 83.7% of the intervention). However, there was no difference in rates of participants achieving blood pressure control between the two study groups. The intervention arm did not emerge as a significant predictor of success, defined as blood pressure in the target range of <140/90 (OR=1.33, CI=.57-3.10, P=.50) (Table 3).
Similar analyses were conducted to determine predictors of 12-month adherence and whether randomization group was a predictor of adherence. On bivariate analysis, younger age (OR=1.05; CI=1.01-1.09; P=.020), having lower self-efficacy (OR=1.08; CI=1.04-1.13; P<.001), reporting more perceived stress (OR=0.91; CI=.87-.96; P<.001) and depressive symptoms (OR=.92; CI=.87-.97; P=.003) at baseline predicted poorer adherence at 12 months. In multivariate analyses, only low self-efficacy remained significant (OR=1.06; CI=1.02-1.10; P=.006). Randomization group did not predict adherence (OR=.64; CI=.29-1.45; P=.286).
Changes in Psychosocial Variables
Percentages of patients achieving positive psychosocial changes, such as increased social support or positive affect and decreased levels of depression, negative affect and perceived stress, did not significantly differ between the two study groups. As for negative changes, a significant difference emerged only in social support. Specifically, there was an unexpected finding that participants in the intervention arm were two-fold more likely to report a decrease in social support than controls at the conclusion of the study (33% vs 17%; P=.026). The reason for this paradoxical finding is unclear and may reflect discordance between social support that is needed and that which is provided for one to effectively change their health behavior.
Discussion
TRIUMPH demonstrated that it was feasible to conduct a blood pressure control intervention in a community-based and federally qualified health center practice setting. Overall, 82% of participants in both arms achieved blood pressure control. However, TRIUMPH did not demonstrate a significant difference in achieving blood pressure control between the two groups. As we considered possible reasons for this finding, we explored characteristics of the study design and characteristics of the participants. Possible reasons for our findings include that the intervention of positive affect, self-affirmation, and motivational interview was not an effective mediator of blood pressure control above patient education. Alternatively, the patient education protocol may not have been sufficiently distinct from the intervention. In this study, control participants were exposed to education about hypertension and were asked to develop a behavioral contract for medication adherence. Moreover, this study was not cluster-randomized which makes contamination a major concern. The same research assistants were used for delivering the intervention as in the control arm. The fact that participants in both arms received calls at the same interval may have been a form of social support which dampened intervention effects. Providers who had patients in both the control and intervention group may have learned aspects of the experiment and inadvertently shared this with control patients. Therefore, by including an attention control group as a comparator, we may have created more challenges to demonstrating a difference. A more traditional usual care approach may have demonstrated greater differences.
Our study was conducted among patients seeking care in federally qualified health centers or community health centers. Patients in these populations may have particular challenges to blood pressure control and may experience a greater burden social challenges.35 Recognizing this potential need for greater resources, our research assistants were equipped with knowledge about social resources that could be provided in the event a study participant was in need. This was done without regard to group assignment. During the follow-up calls, participants in both groups reported loss of a job, eviction, or the unexpected death of a loved one. The research assistants provided supportive counseling to both arms and made referrals to social services. Therefore, both groups may have received additional social support, which, in and of itself, is a potent modifier of medication adherence.36 At the conclusion of the study, participants in both groups were asked to describe the most helpful aspect of the study. Participants in both groups reported that having the research assistant call them on a regular basis was most helpful. The majority of remarks focused on the interaction with the research assistant to whom they were assigned. For example, one participant stated “knowing that (the research assistant) was going to be calling was helpful, she motivated me.” Another participant said “what helped me take my medication was that I knew that (the research assistant) was going to call and ask about my blood pressure.” An active intervention arm that had a more structured and systematic response to social determinants of health and psychosocial stressors may have proven even more effective.
Another interesting finding was the inverse association between higher psychosocial factors and lower rates of blood pressure control. After baseline factors were accounted for, the relationship with depressive symptoms remained significant. The association between depressive symptoms and blood pressure is well-known. The mechanism linking depressive symptoms with poor blood pressure control may be through poor health habits or self-care such as poor medication adherence, poor dietary adherence, physical inactivity, or poor sleep.37-39 Earlier studies have also demonstrated enhanced sympathetic and cardiovascular activity as potential pathophysiologic mechanisms linking depressive symptoms with blood pressure.40-42 Future studies that delve deeper into the potential pathways linking depressive symptoms and blood pressure may provide greater insight.
In this study, a greater proportion of patients in the intervention reported a decrease in perceived social support. Studies have demonstrated the importance of social support for health behavior change. There are specific actions by social networks that have been deemed as helpful or unhelpful.43,44 Therefore, it is possible that the social support that was present at the beginning of the study may not have been adequate to support health behavior changes. It is possible that participants who were engaging in healthy behaviors as stipulated by the intervention did not perceive support in this effort.43-45 Studies need to better match social support or provide education to social networks as well, so that they may be able to support health behavior change.
Limitations of this study is the preponderance of women which may reflect lower tendency for men to go to primary care settings and therefore, have less opportunities to participate in clinical trials.46,47 Previous studies have shown that being male is a correlate of difficult to control blood pressure.35,48 Therefore, interventions that over-sample for men would advance the ability to address sex differences in blood pressure control. Future studies will need to recruit from non-traditional settings where men may be more likely to seek help such as barbershops.49 Another limitation was that the same study personnel administered the follow-up calls to maintain continuity and therefore were not blinded to randomization group and any protocol-specific issues. A separate team of interventionists administering the intervention may further help to minimize potential for contamination. While balancing the frequency of calls is important to equalize attention, future studies will need to make sure that the content of each call differs. One approach would be to have automated calls to patients with an interactive voice response system that can prompt participants to respond to specific questions and minimize conversations that are not directly related to the study.
Conclusion
The results of TRIUMPH demonstrate the importance of addressing the psychosocial context of blood pressure medication adherence and blood pressure control. We also achieved success in 82% of the patients in this setting, which is above the national average of approximately 50% and which is much higher than rates for community health settings.35,50 While these findings did not demonstrate a difference in control between the two arms, lessons learned can be used to refine behavioral interventions for blood pressure control.
Acknowledgments
The authors would like to dedicate this manuscript in memory of Anna Rodriguez without whom this study would not have been possible.
Funding
Center of Excellence in Health Disparities Research and Community Engagement (CEDREC) NIMHD P60 MD003421-02.
References
- 1. Gillespie CD, Hurvitz KA; Centers for Disease Control and Prevention (CDC) . Prevalence of hypertension and controlled hypertension - United States, 2007-2010. MMWR Surveill Summ. 2013;62(3)(suppl 3):144-148. [PubMed] [Google Scholar]
- 2. Krousel-Wood M, Thomas S, Muntner P, Morisky D. Medication adherence: a key factor in achieving blood pressure control and good clinical outcomes in hypertensive patients. Curr Opin Cardiol. 2004;19(4):357-362. 10.1097/01.hco.0000126978.03828.9e [DOI] [PubMed] [Google Scholar]
- 3. Siegel D, Lopez J, Meier J. Antihypertensive medication adherence in the Department of Veterans Affairs. Am J Med. 2007;120(1):26-32. 10.1016/j.amjmed.2006.06.028 [DOI] [PubMed] [Google Scholar]
- 4. Forsyth J, Schoenthaler A, Chaplin WF, Ogedegbe G, Ravenell J. Perceived discrimination and medication adherence in black hypertensive patients: the role of stress and depression. Psychosom Med. 2014;76(3):229-236. 10.1097/PSY.0000000000000043 [DOI] [PubMed] [Google Scholar]
- 5. Charlson ME, Wells MT, Peterson JC, et al. Mediators and moderators of behavior change in patients with chronic cardiopulmonary disease: the impact of positive affect and self-affirmation. Transl Behav Med. 2014;4(1):7-17. 10.1007/s13142-013-0241-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ogedegbe G, Mancuso CA, Allegrante JP, Charlson ME. Development and evaluation of a medication adherence self-efficacy scale in hypertensive African-American patients. J Clin Epidemiol. 2003;56(6):520-529. 10.1016/S0895-4356(03)00053-2 [DOI] [PubMed] [Google Scholar]
- 7. Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143-164. 10.1177/1090198104263660 [DOI] [PubMed] [Google Scholar]
- 8. Strecher VJ, DeVellis BM, Becker MH, Rosenstock IM. The role of self-efficacy in achieving health behavior change. Health Educ Q. 1986;13(1):73-92. 10.1177/109019818601300108 [DOI] [PubMed] [Google Scholar]
- 9. Milner W, Rollnick S. Motivational Interviewing. New York and London: Guilford Press; 2002. [Google Scholar]
- 10. Boutin-Foster C, Scott E, Rodriguez A, et al. The Trial Using Motivational Interviewing and Positive Affect and Self-Affirmation in African-Americans with Hypertension (TRIUMPH): from theory to clinical trial implementation. Contemp Clin Trials. 2013;35(1):8-14. 10.1016/j.cct.2013.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ogedegbe G, Chaplin W, Schoenthaler A, et al. A practice-based trial of motivational interviewing and adherence in hypertensive African Americans. Am J Hypertens. 2008;21(10):1137-1143. 10.1038/ajh.2008.240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ogedegbe G, Schoenthaler A, Richardson T, et al. An RCT of the effect of motivational interviewing on medication adherence in hypertensive African Americans: rationale and design. Contemp Clin Trials. 2007;28(2):169-181. 10.1016/j.cct.2006.04.002 [DOI] [PubMed] [Google Scholar]
- 13. Pressman SD, Cohen S. Does positive affect influence health? Psychol Bull. 2005;131(6):925-971. 10.1037/0033-2909.131.6.925 [DOI] [PubMed] [Google Scholar]
- 14. Isen AM. Some Perspectives on Positive Affect and Self-Regulation. Psychol Inq. 2000;11(3):184-187. [Google Scholar]
- 15. Erez A, Isen AM. The influence of positive affect on the components of expectancy motivation. J Appl Psychol. 2002;87(6):1055-1067. 10.1037/0021-9010.87.6.1055 [DOI] [PubMed] [Google Scholar]
- 16. Koole SL, Smeets K, Van Knippenberg A, Dijksterhuis A. The cessation of rumination through self-affirmation. J Pers Soc Psychol. 1999;77(1):111-125. 10.1037/0022-3514.77.1.111 [DOI] [Google Scholar]
- 17. Harris PR, Epton T. The impact of self‐affirmation on health cognition, health behaviour and other health‐related responses: a narrative review. Soc Personal Psychol Compass. 2009;3(6):962-978. 10.1111/j.1751-9004.2009.00233.x [DOI] [Google Scholar]
- 18. McQueen A, Klein WM. Experimental manipulations of self-affirmation: A systematic review. Self Ident. 2006;5(4):289-354. 10.1080/15298860600805325 [DOI] [Google Scholar]
- 19. . Schuz N, Schuz B, Eid M When risk communication backfires: randomized controlled trial on self-affirmation and reactance to personalized risk feedback in high-risk individuals. Health psychology : official journal of the Division of Health Psychology, American Psychological Association. May 2013;32(5):561-570. [DOI] [PubMed]
- 20. Steele CM. A threat in the air. How stereotypes shape intellectual identity and performance. Am Psychol. 1997;52(6):613-629. 10.1037/0003-066X.52.6.613 [DOI] [PubMed] [Google Scholar]
- 21. Olson E, Van Wye G, Kerker B, Thorpe L, Frieden TR. NYC Community Health Profiles. Take Care Central Harlem. 2006;20(42):1-16. [Google Scholar]
- 22. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373-383. 10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- 23. Radloff LS. The use of the Center for Epidemiologic Studies Depression Scale in adolescents and young adults. J Youth Adolesc. 1991;20(2):149-166. 10.1007/BF01537606 [DOI] [PubMed] [Google Scholar]
- 24. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385-396. 10.2307/2136404 [DOI] [PubMed] [Google Scholar]
- 25. Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54(6):1063-1070. 10.1037/0022-3514.54.6.1063 [DOI] [PubMed] [Google Scholar]
- 26. Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32(6):705-714. 10.1016/0277-9536(91)90150-B [DOI] [PubMed] [Google Scholar]
- 27. Boutin-Foster C, Ravenell JE, Greenfield VW, Medmim B, Ogedegbe G. Applying qualitative methods in developing a culturally tailored workbook for black patients with hypertension. Patient Educ Couns. 2009;77(1):144-147. 10.1016/j.pec.2009.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Charlson ME, Boutin-Foster C, Mancuso CA, et al. ; Translational Behavioral Science Research Consortium . Randomized controlled trials of positive affect and self-affirmation to facilitate healthy behaviors in patients with cardiopulmonary diseases: rationale, trial design, and methods. Contemp Clin Trials. 2007;28(6):748-762. 10.1016/j.cct.2007.03.002 [DOI] [PubMed] [Google Scholar]
- 29. Steele CM. A threat in the air. How stereotypes shape intellectual identity and performance. Am Psychol. 1997;52(6):613-629. 10.1037/0003-066X.52.6.613 [DOI] [PubMed] [Google Scholar]
- 30. Wright JM, Mattu GS, Perry TL Jr, et al. Validation of a new algorithm for the BPM-100 electronic oscillometric office blood pressure monitor. Blood Press Monit. 2001;6(3):161-165. 10.1097/00126097-200106000-00008 [DOI] [PubMed] [Google Scholar]
- 31. . Yacoub M, Jampana R., Dettenborn L., Gerin W., Pickering T.G.. Automated blood pressure (BP) readings as a substitute for physician readings in outpatient settings. Paper presented at: Paper presented at: 17th Annual Scientific Meeting of the American Society of Hypertension 2003; New York, NY 10.1016/S0895-7061(03)00243-7 [DOI] [Google Scholar]
- 32. Perloff D, Grim C, Flack J, et al. Human blood pressure determination by sphygmomanometry. Circulation. 1993;88(5 Pt 1):2460-2470. 10.1161/01.CIR.88.5.2460 [DOI] [PubMed] [Google Scholar]
- 33. Chobanian AV, Bakris GL, Black HR, et al. ; Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee . Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206-1252. 10.1161/01.HYP.0000107251.49515.c2 [DOI] [PubMed] [Google Scholar]
- 34. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507-520. 10.1001/jama.2013.284427 [DOI] [PubMed] [Google Scholar]
- 35. Olomu AB, Gourineni V, Huang JL, et al. Rate and predictors of blood pressure control in a federal qualified health center in Michigan: a huge concern? J Clin Hypertens (Greenwich). 2013;15(4):254-263. 10.1111/jch.12067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. DiMatteo MR. Social support and patient adherence to medical treatment: a meta-analysis. Health Psychol. 2004;23(2):207-218. 10.1037/0278-6133.23.2.207 [DOI] [PubMed] [Google Scholar]
- 37. Abreu-Silva EO, Todeschini AB. Depression and its relation with uncontrolled hypertension and increased cardiovascular risk. Curr Hypertens Rev. 2014;10(1):8-13. 10.2174/157340211001141111144533 [DOI] [PubMed] [Google Scholar]
- 38. Rubio-Guerra AF, Rodriguez-Lopez L, Vargas-Ayala G, Huerta-Ramirez S, Serna DC, Lozano-Nuevo JJ. Depression increases the risk for uncontrolled hypertension. Exp Clin Cardiol. 2013;18(1):10-12. [PMC free article] [PubMed] [Google Scholar]
- 39. Dickson VV, McCarthy MM, Katz SM. How do depressive symptoms influence self-care among an ethnic minority population with heart failure? Ethn Dis. 2013;23(1):22-28. [PubMed] [Google Scholar]
- 40. . Light KC, Kothandapani RV, Allen MT Enhanced cardiovascular and catecholamine responses in women with depressive symptoms. International journal of psychophysiology : official journal of the International Organization of Psychophysiology. Mar 1998;28(2):157-166. [DOI] [PubMed]
- 41. Cené CW, Dennison CR, Powell Hammond W, Levine D, Bone LR, Hill MN. Antihypertensive medication nonadherence in black men: direct and mediating effects of depressive symptoms, psychosocial stressors, and substance use. J Clin Hypertens (Greenwich). 2013;15(3):201-209. 10.1111/jch.12056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Wang PS, Bohn RL, Knight E, Glynn RJ, Mogun H, Avorn J. Noncompliance with antihypertensive medications: the impact of depressive symptoms and psychosocial factors. J Gen Intern Med. 2002;17(7):504-511. 10.1046/j.1525-1497.2002.00406.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Boutin-Foster C. In spite of good intentions: patients’ perspectives on problematic social support interactions. Health Qual Life Outcomes. 2005;3(1):52. 10.1186/1477-7525-3-52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Boutin-Foster C. Getting to the heart of social support: a qualitative analysis of the types of instrumental support that are most helpful in motivating cardiac risk factor modification. Heart Lung. 2005;34(1):22-29. 10.1016/j.hrtlng.2004.09.002 [DOI] [PubMed] [Google Scholar]
- 45. Boutin-Foster C, Alexander J. Development and validation of the Tangible, Informational, and Emotional Social Support Survey. J Cardiopulm Rehabil. 2006;26(5):307-313. 10.1097/00008483-200609000-00006 [DOI] [PubMed] [Google Scholar]
- 46. Galdas PM, Cheater F, Marshall P. Men and health help-seeking behaviour: literature review. J Adv Nurs. 2005;49(6):616-623. 10.1111/j.1365-2648.2004.03331.x [DOI] [PubMed] [Google Scholar]
- 47. Ferdinand KC, Patterson KP, Taylor C, Fergus IV, Nasser SA, Ferdinand DP. Community-based approaches to prevention and management of hypertension and cardiovascular disease. J Clin Hypertens (Greenwich). 2012;14(5):336-343. 10.1111/j.1751-7176.2012.00622.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. . Flack JM, Sica DA, Bakris G, et al. Management of High Blood Pressure in Blacks: An Update of the International Society on Hypertension in Blacks Consensus Statement. Hypertension. November 1, 2010 2010;56(5):780-800. [DOI] [PubMed]
- 49. Ravenell J, Thompson H, Cole H, et al. A novel community-based study to address disparities in hypertension and colorectal cancer: a study protocol for a randomized control trial. Trials. 2013;14(1):287. 10.1186/1745-6215-14-287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Centers for Disease Control and Prevention (CDC) . Vital signs: awareness and treatment of uncontrolled hypertension among adults--United States, 2003-2010. MMWR Morb Mortal Wkly Rep. 2012;61:703-709. [PubMed] [Google Scholar]