Abstract
Objective
We sought to determine if, after adjusting for economic status, race is an independent risk factor for glycemic control among diabetic patients in a large primary care patient population.
Design, Setting, Participants
We performed a retrospective chart review of 264,000 primary care patients at our large, urban academic medical center to identify patients with a diagnosis of diabetes (n=25,123). Zip code was used to derive median income levels using US Census Bureau demographic information. Self-reported race was extracted from registration data.
Main Outcome Measures
The prevalence of diabetes, average glycated hemoglobin (A1c), and prevalence of uncontrolled diabetes of White and Black patients at all income levels were determined.
Results
White patients had a lower average A1c level and a lower prevalence of diabetes than Black patients in all income quartiles (P<.001). Among White patients, the prevalence of diabetes (P<.001), uncontrolled diabetes (P<.001), and A1c level (P=.014) were inversely proportional to income level. No significant difference in the prevalence of diabetes (P=.214), A1c level (P=.282), or uncontrolled diabetes related to income was seen in Black patients (P=.094).
Conclusions
Race had an independent association with diabetes prevalence and glycemic control. Our study does not support two prominent theories that economic and insurance status are the main factors in diabetes disparities, as we attempted to control for economic status and nearly every patient had insurance. It will be important for future analysis to explore how health care system factors affect these observed gaps in quality.
Keywords: Diabetes Mellitus, Health Care Disparities, Diabetes Complications, Racial Disparities, Socioeconomic Factors
Introduction
Type 2 diabetes mellitus is a prevalent disease with significant morbidity and possible mortality if left uncontrolled.1 Minority populations and those of low economic status have been shown to have higher prevalence of diabetes,2-6 worse glycemic control,7-12 and increased complications.2,3,13-15
It is unclear whether race and economic status are independent risk factors for poor glycemic control. Some suggest that economic status has a stronger association with diabetes prevalence and control than race,16,17 whereas others suggest that race may play a larger role.9 Recent health care system reforms that provide increased access to primary care offer significant reductions in barriers to entering the health system but do not necessarily fully mitigate the deleterious effect of adverse social circumstances on health. We undertook an analysis of disparities in diabetes prevalence and control by race and income using a sample of patients with insurance who have accessed primary care services. A clearer understanding of the impact of each of these social determinants may not only guide interventions at the social policy level, but also inform health system leaders and providers on the potential value of developing services tailored to the specific needs of their patients.
The purpose of this study was to determine if race is an independent risk factor for glycemic control among diabetic patients after adjusting for economic status using zip code of residence as a surrogate for income level.
Methods
We performed a retrospective chart review of all patients aged ≥ 18 years who were seen at any of the Henry Ford Medical Group’s outpatient primary care clinics from January 1, 2012 to June 30, 2012. Henry Ford Medical Group is one of the nation’s largest group practices.18 Composed of racially diverse urban and suburban practices, it serves some of the wealthiest and poorest communities in the country.19 Furthermore, almost all of the patients have insurance, with >50% having Medicare or Medicaid and the rest with other types of insurance; only 1% of patients are self-pay. In our study, we included only patients who provided demographic data including self-identified ethnicity and home address with a Michigan zip code. Zip code data were available for all patients. Diabetes was defined as at least two office visits billed with an International Classification of Diseases, Ninth edition, (ICD-9) code of 250.xx and at least 1 glycated hemoglobin (A1c) value on file in the patient’s history. The most recent A1c on file was used for analysis. As we did not have income data for the patients, median income levels were derived from the US Census Bureau from 2000 based on zip code of residence. Income quartiles were derived using the median income level of the entire outpatient group and divided into 4 relatively equal subgroups. We compared the prevalence of diabetes, the average A1c, and the prevalence of uncontrolled diabetes (defined as A1c >9) between Whites and Blacks at all income levels. Patients who self-identified as “other” races (5.5% of total patients) were not included in our analysis.
Statistical Analysis
A Cochran-Armitage trend test was used to detect significant trends in prevalence of diabetes and uncontrolled diabetes across income quartiles. A chi-square test was used to detect differences in the prevalence of diabetes between Whites and Blacks at each income quartile and associations of uncontrolled diabetes with race. A Wilcoxon Rank Sum test was used to detect associations between race and A1c level. A Spearman Correlation was used to detect significant trends in A1c levels across income quartiles.
Results
Of the 264,000 patients in our database, 25,123 had diabetes. Median household income quartiles, from first to fourth, were <$35,229, $35,230-$49,518, $49,519-$67,777, and >$67,778.
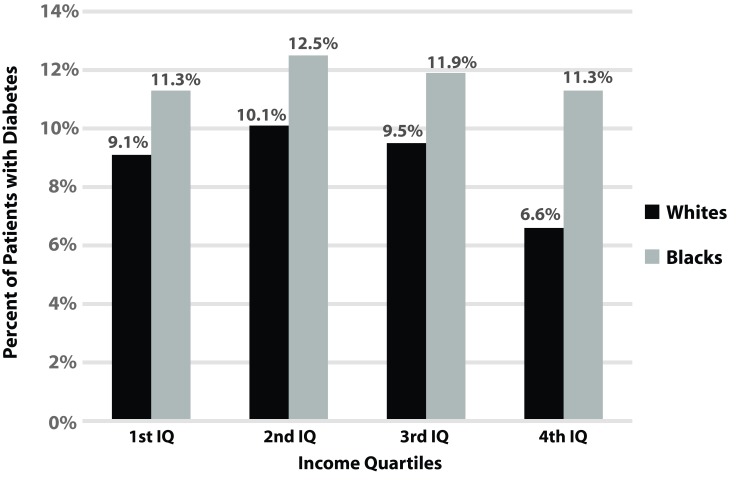
Data analysis showed a significant trend in the prevalence of diabetes related to income level, with the highest income quartile having the lowest prevalence of diabetes (P<.001; Figure 1). A difference was also seen among White patients (P<.001) but not among Black patients (P=.214). White patients had a statistically significant lower prevalence of diabetes than Black patients at all income levels.
Figure 1. Diabetes trends across income levels as related to race.
A Cochran-Armitage trend test revealed a statistically significant trend in the prevalence of diabetes related to income level, with the highest income quartile having the lowest prevalence of diabetes (P<.001) among White patients. This difference is not seen among Black patients (P=.214). A chi-square test showed that Black patients have a statistically significant higher overall prevalence of diabetes than White patients in all income quartiles (P<.001). Median household income quartiles, from first to fourth, were <$35,229, $35,230-$49,518, $49,519-$67,777, and >$67,778. IQ, interquartile.
White patients had a lower average A1c level than Black patients in all income quartiles (P<.001; Table 1) There was also a statistically significant trend in A1c level among White patients related to income level, with the A1c level being inversely proportional to income (P=.014). No significant difference by income was seen among Black patients (P=.282).
Table 1. Associations of A1c with race and income.
| Setting | Whites, mean + SD | Blacks, mean + SD | White vs Blacka, P |
| Overall | 7.29 + 1.33 | 7.68 + 1.77 | ≤.001 |
| 1st income quartile (≤$35,229) | 7.45 + 1.53 | 7.69 + 1.80 | .002 |
| 2nd income quartile ($35,230 - $49,518) | 7.31 + 1.36 | 7.74 + 1.80 | ≤.001 |
| 3rd income quartile ($49,519 - 67,777) | 7.26 + 1.29 | 7.68 + 1.72 | ≤.001 |
| 4th income quartile (≥$67,778) | 7.24 + 1.26 | 7.49 + 1.62 | .014 |
| Spearman correlation P | .014 | .282 |
SD; standard deviation.
a. Wilcoxon Rank Sum.
There was a significant trend in prevalence of uncontrolled diabetes among White patients related to income level, with the prevalence of uncontrolled diabetes being inversely proportional to income level (P<.001; Table 2). White patients had a lower prevalence of uncontrolled diabetes compared with Black patients in all income quartiles (P<.001). No significant difference by income was seen among Black patients (P=.094).
Table 2. Associations of elevated A1c (>9) with race and income.
| Setting | Elevated last A1c | Whites, N (%) | Blacks, N (%) | White vs Blacka, P |
| Overall | no | 9,107 (90.0) | 8,443 (81.7) | ≤.001 |
| yes | 1,011 (10.0) | 1,893 (18.3) | ||
| 1st income quartile (≤$35,229) | no | 921 (86.2) | 3,739 (81.9) | ≤.001 |
| yes | 147 (13.8) | 827 (18.1) | ||
| 2nd income quartile ($35,230 - $49,518) | no | 2,530 (90.0) | 2,462 (80.2) | ≤.001 |
| yes | 281 (10.0) | 609 (19.8) | ||
| 3rd income quartile ($49,519 - $67,777) | no | 3,227 (90.3) | 1,392 (81.7) | ≤.001 |
| yes | 346 (9.7) | 312 (18.3) | ||
| 4th income quartile (≥$67,778) | no | 2,429 (91.1) | 850 (85.4) | ≤.001 |
| yes | 237 (8.9) | 145 (14.6) | ||
| Cochran-Armitage Trend Test P | <.001 | .094 |
a. Chi-square.
Discussion
We found that in a large, diverse patient population, race had a significant association with diabetes prevalence and glycemic control, even after controlling for economic status based on zip code. Black patients had a consistently higher prevalence and worse control of the disease when compared with White patients. Reasons for this disparity deserve further investigation. Our study does not support two prominent theories that economic status17,20,21 and insurance status6 are the main associated factors. While it is retrospective and therefore cannot address causation, we attempted to control for economic status by stratifying patients into income levels based on zip code. Furthermore, the effect of insurance was minimized as a confounding factor, as nearly every patient included had insurance. Some prior studies have found similar results after controlling for economic status.17,22,23 Our finding that race has an independent association with diabetes prevalence and control is important for characterizing and addressing the underlying causes of health disparities in diabetic patients.
Notably, we found that economic status is associated with prevalence and control of diabetes in White patients, but not in Black patients. While prior studies have also demonstrated an association between socioeconomic status and disease,12,17,20 our study is unique in that this relationship was significant only in White patients. Possible explanations for this finding include biological factors outweighing income factors,24-27 societal barriers,21 cultural differences,6,28,29 or inadequacy of zip code to accurately reflect socioeconomic status.20
In addition, we have demonstrated that access to care alone does not seem to be the sole factor associated with racial disparities in diabetes. Although it certainly has been demonstrated in previous studies that access to care makes a difference in the quality of treatment,30,31 it does not appear to be enough to bridge the gap in diabetic health disparities.10 Others have postulated reasons for this including the comprehensive and dynamic nature of access to care that includes many aspects instead of just mere “access.”17,22 The Institute of Medicine report, Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care,23 found that a consistent body of research demonstrates significant disparities in the quality of care that is provided in the US health system, highlighting the disturbing trends that continue today.
There were some limitations to our study. Since our definition of diabetes was based on two ICD-9 codes, we may have included some non-diabetic patients that may have been miscoded, and some diabetic patients may have been missed. Furthermore, a retrospective review of medical chart data collected for clinical purposes has known limitations; however, we believe that these findings will inform future prospective investigations as well as quality improvement interventions.
Conclusions
It will be important for future analysis to explore how health care system factors such as primary care physician alignment, variations in insurance co-payment, provider treatment inertia, and patient/provider communication impact these observed gaps in quality. Future studies could also focus on identifying effective approaches to addressing the social factors that adversely affect patient ability to manage their disease, including medication access, lifestyle changes, and participation in diabetes education services.
Acknowledgments
We acknowledge the help of Dr. Melissa Matzumura Kuan and Dr. Cesar Ochoa Perez for their help in generating ideas for the paper, as well as Sarah Whitehouse and Stephanie Stebens who assisted with editing and preparing the paper.
References
- 1. American Diabetes Association . Diagnosis and classification of diabetes mellitus. Diabetes Care. 2011;34(suppl 1):S62-S69. 10.2337/dc11-S062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kirk JK, Bell RA, Bertoni AG, et al. Ethnic disparities: control of glycemia, blood pressure, and LDL cholesterol among US adults with type 2 diabetes. Ann Pharmacother. 2005;39(9):1489-1501. 10.1345/aph.1E685 [DOI] [PubMed] [Google Scholar]
- 3. Harris MI, Klein R, Cowie CC, Rowland M, Byrd-Holt DD. Is the risk of diabetic retinopathy greater in non-Hispanic blacks and Mexican Americans than in non-Hispanic whites with type 2 diabetes? A U.S. population study. Diabetes Care. 1998;21(8):1230-1235. 10.2337/diacare.21.8.1230 [DOI] [PubMed] [Google Scholar]
- 4. Kirk JK, Passmore LV, Bell RA, et al. Disparities in A1C levels between Hispanic and non-Hispanic white adults with diabetes: a meta-analysis. Diabetes Care. 2008;31(2):240-246. 10.2337/dc07-0382 [DOI] [PubMed] [Google Scholar]
- 5. Insaf TZ, Strogatz DS, Yucel RM, Chasan-Taber L, Shaw BA. Associations between race, lifecourse socioeconomic position and prevalence of diabetes among US women and men: results from a population-based panel study. J Epidemiol Community Health. 2014;68(4):318-325. 10.1136/jech-2013-202585 [DOI] [PubMed] [Google Scholar]
- 6. Miller ST, Schlundt DG, Larson C, et al. Exploring ethnic disparities in diabetes, diabetes care, and lifestyle behaviors: the Nashville REACH 2010 community baseline survey. Ethn Dis. 2004;14(3)(suppl 1):S38-S45. [PubMed] [Google Scholar]
- 7. Ricci-Cabello I, Ruiz-Pérez I, Olry de Labry-Lima A, Márquez-Calderón S. Do social inequalities exist in terms of the prevention, diagnosis, treatment, control and monitoring of diabetes? A systematic review. Health Soc Care Community. 2010;18(6):572-587. 10.1111/j.1365-2524.2010.00960.x [DOI] [PubMed] [Google Scholar]
- 8. Kaplan SH, Billimek J, Sorkin DH, Ngo-Metzger Q, Greenfield S. Reducing racial/ethnic disparities in diabetes: the Coached Care (R2D2C2) project. J Gen Intern Med. 2013;28(10):1340-1349. 10.1007/s11606-013-2452-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Harris MI, Eastman RC, Cowie CC, Flegal KM, Eberhardt MS. Racial and ethnic differences in glycemic control of adults with type 2 diabetes. Diabetes Care. 1999;22(3):403-408. 10.2337/diacare.22.3.403 [DOI] [PubMed] [Google Scholar]
- 10. Kirk JK, D’Agostino RB Jr, Bell RA, et al. Disparities in HbA1c levels between African-American and non-Hispanic white adults with diabetes: a meta-analysis. Diabetes Care. 2006;29(9):2130-2136. 10.2337/dc05-1973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Campbell JA, Walker RJ, Smalls BL, Egede LE. Glucose control in diabetes: the impact of racial differences on monitoring and outcomes. Endocrine. 2012;42(3):471-482. 10.1007/s12020-012-9744-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Meyer PA, Penman-Aguilar A, Campbell VA, Graffunder C, O’Connor AE, Yoon PW; Centers for Disease Control and Prevention (CDC) . Conclusion and future directions: CDC Health Disparities and Inequalities Report - United States, 2013. MMWR Surveill Summ. 2013;62(suppl 3):184-186. [PubMed] [Google Scholar]
- 13. Stark Casagrande S, Fradkin JE, Saydah SH, Rust KF, Cowie CC. The prevalence of meeting A1C, blood pressure, and LDL goals among people with diabetes, 1988-2010. Diabetes Care. 2013;36(8):2271-2279. 10.2337/dc12-2258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Crowe M, Sartori A, Clay OJ, et al. Diabetes and cognitive decline: investigating the potential influence of factors related to health disparities. J Aging Health. 2010;22(3):292-306. 10.1177/0898264309357445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Shen JJ, Washington EL. Identification of diabetic complications among minority populations. Ethn Dis. 2008;18(2):136-140. [PubMed] [Google Scholar]
- 16. Link CL, McKinlay JB. Disparities in the prevalence of diabetes: is it race/ethnicity or socioeconomic status? Results from the Boston Area Community Health (BACH) survey. Ethn Dis. 2009;19(3):288-292. [PMC free article] [PubMed] [Google Scholar]
- 17. Levesque JF, Harris MF, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. 2013;12(1):18. 10.1186/1475-9276-12-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. .Henry Ford Health System. About Henry Ford Health System. http://www.henryford.com/body.cfm?id=37460. Accessed August 4, 2014.
- 19. . United States Census Bureau http://www.census.gov/main/www/cen2000.html. Accessed August 4, 2014.
- 20. Osborn CY, de Groot M, Wagner JA. Racial and ethnic disparities in diabetes complications in the northeastern United States: the role of socioeconomic status. J Natl Med Assoc. 2013;105(1):51-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. LaVeist TA, Thorpe RJ Jr, Galarraga JE, Bower KM, Gary-Webb TL. Environmental and socio-economic factors as contributors to racial disparities in diabetes prevalence. J Gen Intern Med. 2009;24(10):1144-1148. 10.1007/s11606-009-1085-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Peek ME, Cargill A, Huang ES. Diabetes health disparities: a systematic review of health care interventions. Med Care Res Rev. 2007;64(5)(suppl):101S-156S. 10.1177/1077558707305409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Smedley BD, Stith AY, Nelson AR; Institute of Medicine Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care . Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: The National Academies Press; 2003. [PubMed] [Google Scholar]
- 24. Agrawal L, Emanuele NV, Abraira C, et al. Ethnic differences in the glycemic response to exogenous insulin treatment in the Veterans Affairs Cooperative Study in Type 2 Diabetes Mellitus (VA CSDM). Diabetes Care. 1998;21(4):510-515. 10.2337/diacare.21.4.510 [DOI] [PubMed] [Google Scholar]
- 25. Harris SS. Does vitamin D deficiency contribute to increased rates of cardiovascular disease and type 2 diabetes in African Americans? Am J Clin Nutr. 2011;93(5):1175S-1178S. 10.3945/ajcn.110.003491 [DOI] [PubMed] [Google Scholar]
- 26. Manickam B, Neagu V, Kukreja SC, Barengolts E. Relationship between glycated hemoglobin and circulating 25-hydroxyvitamin D concentration in African American and Caucasian American men. Endocr Pract. 2013;19(1):73-80. 10.4158/EP12168.OR [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Zhang Q, Wang Y, Huang ES. Changes in racial/ethnic disparities in the prevalence of Type 2 diabetes by obesity level among US adults. Ethn Health. 2009;14(5):439-457. 10.1080/13557850802699155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Calvin D, Quinn L, Dancy B, et al. African Americans’ perception of risk for diabetes complications. Diabetes Educ. 2011;37(5):689-698. 10.1177/0145721711416258 [DOI] [PubMed] [Google Scholar]
- 29. Miech RA, Kim J, McConnell C, Hamman RF. A growing disparity in diabetes-related mortality U.S. trends, 1989-2005. Am J Prev Med. 2009;36(2):126-132. 10.1016/j.amepre.2008.09.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Rhee MK, Cook CB, Dunbar VG, et al. Limited health care access impairs glycemic control in low income urban African Americans with type 2 diabetes. J Health Care Poor Underserved. 2005;16(4):734-746. 10.1353/hpu.2005.0100 [DOI] [PubMed] [Google Scholar]
- 31. Heisler M, Smith DM, Hayward RA, Krein SL, Kerr EA. Racial disparities in diabetes care processes, outcomes, and treatment intensity. Med Care. 2003;41(11):1221-1232. 10.1097/01.MLR.0000093421.64618.9C [DOI] [PubMed] [Google Scholar]