Abstract
Background
While routine HIV testing in the general population is a national recommendation, actual practice may vary.
Purpose
To determine risk factors associated with HIV testing after the adoption of a New York State law in 2010 mandating that health care providers offer HIV testing in all clinical settings.
Methods
Survey data from Monroe County, New York, were collected in 2012 for adults aged 18-64 years and analyzed in 2014. Logistic regression was used to identify risk factors independently associated with HIV testing and high-risk behavior.
Results
Among adults aged 18-34, fewer Whites were offered HIV testing in the past year by their doctors compared with Blacks (34% vs 64%) despite having similar rates of any HIV high-risk behavior (20% overall). For adults aged 35-64 years, fewer Whites than Blacks were ever tested for HIV (42% vs 71%), offered HIV testing in past year (17% vs 40%), and reported any HIV high-risk behavior (3% vs 13%). Latinos showed intermediate levels. With logistic regression analysis, ever tested for HIV was independently associated with only race/ethnicity; offered HIV testing in the past year was associated with females, Blacks and Latinos, aged 18-34 years, and having a routine health checkup in past year; any HIV high-risk behavior was associated with only younger age.
Conclusions
To improve HIV testing rates as well as compliance with state laws and national guidelines, targeted efforts should be considered that improve perceptions of risk and emphasize the value of routine HIV screening, including those directed at White adults and their health care providers.
Keywords: HIV Testing, Health Screening Disparities, Public Health
Introduction
The number of people living with HIV in the US is estimated to be 1.1 million, including approximately 20% who are unaware of their infection.1 Currently, only 35% – 37% of the US general population has been ever tested for HIV; in Canada, this rate is similar, at 37%.2-4 An HIV diagnosis is important for appropriate linkage to care, treatment of HIV, reducing associated complications, increasing life expectancy, improving quality of life, and decreasing transmission of HIV to others.5 Accordingly, in 2006, the Centers for Disease Control and Prevention (CDC) recommended routine rather than risk-based HIV screening for those aged 13-64 years.6 In 2013, the US Preventive Services Task Force (USPSTF) gave a similar screening guideline an “A” rating, its highest endorsement, which public and private health insurers use to determine coverage of preventive services.7-9
Following the CDC’s revised HIV screening recommendation, nearly all states have adopted compatible laws and administrative codes.10 In 2010, New York State mandated that health care providers offer HIV testing to every individual aged 13-64 years receiving health services.11,12 However, data assessing compliance with this change in policy are limited.12 Moreover, while racial/ethnic disparities in HIV testing have been previously documented using national data, it is unclear to what extent such differences would persist in settings where routine HIV screening is mandated.13-15 For example, compared with Blacks and Hispanics, fewer Whites reported being tested for HIV due to believing they were unlikely exposed; among those ever tested for HIV, Whites were also less likely to report positive future testing intentions.14 Subsequent to the CDC’s 2006 revised HIV testing recommendations, national data have shown an increase in HIV testing among Blacks but not among Whites.15 Beyond these testing patterns, each year in the United States, there are about 50,000 people newly infected with HIV (14% are unaware of their infection), about 1.2 million people living with HIV, and about 13,700 deaths among people with an AIDS diagnosis.16 Compared with Whites, Blacks and Hispanics are disproportionately affected by HIV, with more individuals being diagnosed and living with HIV but fewer being treated with antiretroviral therapy and surviving.16,17
A better understanding of HIV testing patterns among racial/ethnic subgroups at the local level may inform how to improve overall HIV testing rates through targeted community and public health efforts. Therefore, the purpose of our study was to examine HIV testing and risk patterns following changes in New York State HIV testing requirements among adults, including racial/ethnic subgroups, by using population-based data from Monroe County, an urban community located in upstate New York. Further, we sought to assess risk factors independently associated with HIV testing and high-risk behavior.
Methods
Data Sources
To assess HIV testing and risk patterns among US adults, a few population-based surveys have been used: the Behavioral Risk Factor Surveillance System (BRFSS); the National Health and Nutrition Examination Survey (NHANES); and the National Health Interview Survey (NHIS).13 In the past, these surveys have asked respondents one of several types of questions: 1) Have you ever been tested for HIV?; 2) Have you been tested for HIV in the past year?; and 3) Have you engaged in any HIV high-risk behavior? Only the NHIS has asked respondents all three question types; however, beginning in 2011, it removed question types 2 and 3. To the authors’ knowledge, no previously published, population-based survey has explicitly asked respondents about being “offered” an HIV test ever or in the past year. This is not a trivial point because while state laws and regulations may mandate that HIV testing is offered by health care providers, a patient may still decline, and both factors impact testing rates. Therefore, with respect to examining HIV testing and risk patterns more completely, national data are limited.
For our study, the main data source was the 2012 Monroe County Adult Health Survey (MCAHS), a telephone-administered, household-based survey that utilized a methodology and included questions similar to those used in other health surveys, details of which are included elsewhere.18 These data were collected as part of the routine surveillance efforts undertaken by the local health department and, therefore, do not require institutional review board (IRB) approval. The overall response rate was 23%, which included landline (78% of respondents) and cellular-only (22%) phone users. For such population-based surveys, response rates are typically less than optimal, particularly among urban communities, and have decreased over time.19-21 For example, in the 2012 HIV/AIDS Attitudinal Tracking Survey, which was commissioned by the Public Health Agency of Canada, the response rate was 16% among the general population.4 Moreover, empirical research has shown that no arbitrary threshold in response rate ensures accuracy of the survey data; indeed, some higher response rate surveys have been shown to be comparable to or less accurate than lower response rate surveys.22-24 Nevertheless, to adjust for potential nonresponse and/or undercoverage bias, the data were weighted using an iterative, “raking” procedure, which matches marginal totals between the survey sample and target population on key variables.25 The CDC recently adopted this same weighting methodology for its national surveys.26
The main outcomes included affirmative responses to the following questions: 1) Have you ever been tested for HIV?; 2) Have you been offered an HIV test in the past year (ie, 12 months) by your doctor?; and 3) Have you engaged in any HIV high-risk behavior (ie, injection drug use, unprotected anal sex, treatment for a sexually transmitted infection, multiple sexual partners, exchanged sex for money/drugs)? Racial/ethnic comparisons included the following categories: White (non-Latino), Latino (Hispanic), and Black (non-Latino). Other racial/ethnic groups (less than 5%) were excluded. Consistent with prior reports on HIV testing among adults, the study population was restricted to those aged 18-64 years.13 Potential risk factors associated with HIV testing and risk behavior included: race/ethnicity; age; sex; residence; educational attainment; marital status; sexual orientation; household poverty level; current employment status; current health insurance status; health insurance status over past two years; routine health checkup in past year; needed but did not seek health care due to cost; self-rated health status; and frequent mental distress (ie, stress, depression, and/or problems with emotions) in past month.
Data Analysis
The number of individuals available for the analysis was fixed; however, this study was sufficiently powered (ie, >80%) to detect a medium standardized effect size (ie, signal-to-noise ratio of about .45) with a two-sided alpha of .05.27 Observations with missing values for the considered variables accounted for <1% of the total and were excluded from the multivariate analyses. For outcome comparisons by race/ethnicity, differences in prevalence rates were considered statistically significant if the 95% confidence intervals (CIs) were non-overlapping. In determining the independent risk factors associated with each outcome, logistic regression analysis was performed to derive a parsimonious model that allowed straightforward interpretation of the results. Specifically, variable selection was based upon Bayesian information criterion (BIC) to optimize parsimony and external sample data validity rather than relying on an arbitrary P cutoff, as previously described.28,29 For each outcome, separate models were developed and odds ratios (ORs) with 95% CIs are reported for all associated risk factors. Final point estimates and variances were determined using survey-specific procedures in Stata version 12 (College Station, Texas, 2011) to account for the probability sampling design.
Results
This study included 1,073 respondents (weighted total of 442,000): 799 (346,000) Whites, 108 (31,000) Latinos, and 166 (65,000) Blacks. Similar to other urban communities, Monroe County is a relatively diverse study population. For example, the racial/ethnic distribution included 78% White, 15% Black and 7% Latino. Those aged 18-34 accounted for 36%, while females represented 52%. Approximately 30% of respondents resided in the inner city and 27% fell within 200% of the federal poverty level. Most individuals reported having health insurance (91%) as well as having a routine health checkup in the past year (69%). Other population characteristics are summarized in Table 1.
Table 1. Summary characteristics of study population, Monroe County, New York, 2012.
| Variable | Unweighted Frequency (Total = 1,073) | Weighted Frequency (Total = 442,000) | |
| n | n | % | |
| Race/ethnicity | |||
| White | 799 | 346,000 | 78.3 |
| Latino | 108 | 31,000 | 7.0 |
| Black | 166 | 65,000 | 14.7 |
| Age, years | |||
| 18-34 | 181 | 160,000 | 36.2 |
| 35-64 | 892 | 282,000 | 63.8 |
| Female | 652 | 230,000 | 52.0 |
| Residence | |||
| City | 532 | 131,000 | 29.7 |
| Suburb | 541 | 311,000 | 70.3 |
| Educational attainment: college graduate | 444 | 186,000 | 42.2 |
| Marital status: married | 488 | 194,000 | 44.0 |
| Sexual orientation: LGB | 47 | 16,000 | 3.6 |
| Household federal poverty level: 0-200% | 315 | 119,000 | 26.8 |
| Currently employed | 661 | 292,000 | 66.2 |
| Currently health insured | 975 | 403,000 | 91.2 |
| Ever without health insurance in past 2 years | 183 | 72,000 | 16.4 |
| Routine health checkup in past year | 784 | 305,000 | 69.1 |
| Needed but did not seek healthcare due to cost | 102 | 40,000 | 9.1 |
| Self-rated health status: fair/poor | 188 | 533,000 | 12.1 |
| Frequent mental distress for 14+ days in past month | 109 | 42,000 | 9.5 |
LGB, lesbian, gay, or bisexual.
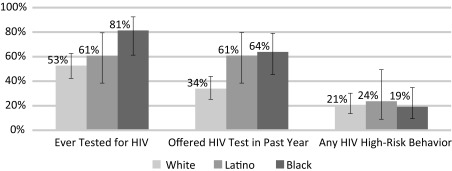
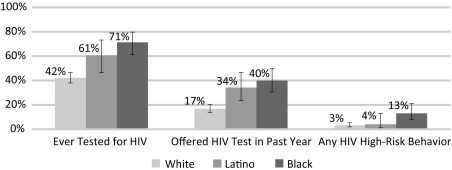
Several demographic patterns were observed for HIV testing and risk behavior (Table 2, Figures 1 and 2). Among adults aged 18-34 years, fewer Whites were offered HIV testing in the past year by their doctors compared to Blacks (34% vs 64%) despite having similar rates of any HIV high-risk behavior (20% overall). For adults aged 35-64, fewer Whites than Blacks were ever tested for HIV (42% vs 71%), offered HIV testing in the past year (17% vs 40%), and reported any HIV high-risk behavior (3% vs 13%). Latinos showed intermediate levels. In general, age-specific prevalence rates were higher for those aged 18-34 than those aged 35-64 for all outcomes (Table 2).
Table 2. Prevalence patterns in HIV testing and high-risk behavior, Monroe County, New York, 2012.
| Age 18-34 | Age 35-64 | |||||||
| Variable | All, % (95% CI) | White, % (95% CI) | Latino, % (95% CI) | Black, % (95% CI) | All, % (95% CI) | White, % (95% CI) | Latino, % (95% CI) | Black, % (95% CI) |
| Ever tested for HIV | 59.2 (50.8–67.1) | 52.7 (42.4–62.6) | 60.8 (38.4–79.4) | 81.4 (61.2–92.4) | 46.7 (42.9–55.2) | 42.2 (38.0–46.7) | 60.6 (46.4–73.2) | 71.3 (61.1–79.7) |
| Offered HIV test in past year | 42.5 (34.7–50.7) | 33.9 (25.2–43.9) | 60.9 (38.4–79.6) | 63.9 (45.5–79.0) | 20.5 (17.6–23.7) | 16.8 (13.7–20.3) | 34.2 (23.5–46.7) | 39.9 (30.6–50.1) |
| Any HIV high-risk behavior | 20.7 (14.8–28.2) | 20.7 (13.6–30.2) | 23.7 (9.0–49.4) | 19.2 (9.5–34.8) | 4.5 (3.1–9.7) | 3.2 (1.9–5.3) | 4.1 (1.2–13.1) | 13.1 (7.9–21.1) |
CI, confidence interval. Study population included 1,073 respondents (weighted total of 442,000): 799 (346,000) Whites, 108 (31,000) Latinos, and 166 (65,000) Blacks. Final point estimates and variances were determined using survey-specific procedures (Stata version 12, College Station, Texas, 2011).
Figure 1. Prevalence patterns in HIV testing and high-risk behavior, age 18-34, by race/ethnicity, Monroe County, New York, 2012.
Total study population included 1,073 respondents (weighted total of 442,000): 799 (346,000) Whites, 108 (31,000) Latinos, and 166 (65,000) Blacks. For each percentage, the vertical error bar represents the 95% CI. Differences between percentages were considered statistically significant if the CIs were non-overlapping. Final point estimates and variances were determined using survey-specific procedures (Stata version 12, College Station, Texas, 2011).
Figure 2. Prevalence patterns in HIV testing and high-risk behavior, age 35-64, by race/ethnicity, Monroe County, New York, 2012.
Total study population included 1,073 respondents (weighted total of 442,000): 799 (346,000) Whites, 108 (31,000) Latinos, and 166 (65,000) Blacks. For each percentage, the vertical error bar represents the 95% CI. Differences between percentages were considered statistically significant if the CIs were non-overlapping. Final point estimates and variances were determined using survey-specific procedures (Stata version 12, College Station, Texas, 2011).
The logistic regression analyses are summarized in Table 3. In the “ever tested for HIV” model, the only independently associated factor was race/ethnicity: the OR for Latinos (compared with Whites) was 1.8 (95% CI 1.0 – 3.3); for Blacks, the OR was 3.8 (2.3 – 6.4). For the outcome, “offered HIV testing in the past year,” the associated factors were: females (OR = 2.7 [1.7 – 4.0]); Blacks (2.4 [1.5 – 3.8]) and Latinos (3.1 [1.8 – 5.4]); age 18-34 (3.0 [2.0 – 4.5]), and having a routine health checkup in past year (2.5 [1.5 – 4.1]). Finally, in the “any HIV high-risk behavior” model, the only associated factor was younger age (1.7 [1.1 – 2.4]).
Table 3. Logistic regression analyses for HIV testing and high-risk behavior, Monroe County, New York, 2012.
| Model | OR | 95% CI |
| Model 1—Ever tested for HIV | ||
| Race/ethnicity | ||
| Latino (vs White) | 1.8 | 1.0 – 3.3 |
| Black (vs White) | 3.8 | 2.3 – 6.4 |
| Model 2—Offered HIV test in past year | ||
| Race/ethnicity | ||
| Latino (vs White) | 3.1 | 1.8 – 5.4 |
| Black (vs White) | 2.4 | 1.5 – 3.8 |
| Age 18-34 (vs 35-64) | 3.0 | 2.0 – 4.5 |
| Female (vs male) | 2.7 | 1.7 – 4.0 |
| Routine health checkup in past year | 2.5 | 1.5 – 4.1 |
| Model 3—Any HIV high-risk behavior | ||
| Age 18-34 (vs 35-64) | 1.7 | 1.1 – 2.4 |
OR, odds ratio; CI, confidence interval. Variable selection algorithm based on Bayesian information criterion using the add-on “bicdrop1” module in Stata version 12 (College Station, Texas, 2011). For each model, potential variables included: race/ethnicity; age; sex; residence; educational attainment; marital status; sexual orientation; household poverty level; current employment status; current health insurance status; health insurance status over past two years; routine health checkup in past year; needed but did not seek health care due to cost; self-rated health status; and frequent mental distress in past month. Final point estimates and variances were determined using survey-specific procedures (Stata version 12).
Discussion
Based on the results of our population-based study from upstate New York, we found that significant racial/ethnic disparities exist in HIV testing among younger adults despite comparable patterns in HIV risk behavior, with fewer Whites being offered testing in the past year than Blacks. Importantly, the “offered-an-HIV-test” finding may be an indicator of health care provider behavior, which to the authors’ knowledge, has not been previously reported. These results are striking, given that in New York State, individuals aged 13-64 years, regardless of risk profile, must be offered HIV testing in all health settings based on a statewide law adopted two years earlier. Our study also identified other factors independently associated with HIV testing patterns.
Takahashi et al previously found that among adults reporting behaviors that increase their risk for HIV, most individuals do not consider themselves to be at-risk and have not been recently tested.30 Others have also shown that primary care providers do not routinely assess HIV risk for their patients and may assume those at risk for HIV will request HIV testing when needed.31,32 In New York State, the most frequently identified barrier to adopting routine HIV testing in physicians’ practices was the perception that few patients in the practice were at risk for HIV.12 Our findings reported here may suggest important differences in the perception of risk among White adults as well as among those who provide health care services to them. In both instances, better awareness about the HIV risk behaviors and the importance of routine HIV screening may improve overall HIV testing rates.
Notably, after adjusting for age and routine health care utilization, this study found that females were more likely to be offered HIV testing in the past year. One explanation might be the type of health care provider that females visit. Prior studies have shown that HIV testing rates are higher for patients receiving health services from obstetricians/gynecologists.33-35 As others have discussed, during a routine gynecological exam, it may be easier to recommend HIV testing in the context of general screening for sexually transmitted infections since sexual activity is assumed. Pregnancy may also increase the likelihood of HIV testing, given that the CDC and the American College of Obstetrics and Gynecology recommend opt-out HIV testing for pregnant women.6,36
There were other factors independently associated with being offered an HIV test in the past year: aged 18-34 years and having a routine health checkup in the past year. Health care providers may perceive younger adults to be more at risk for HIV and, therefore, may be more likely to offer them HIV testing. Indeed, this view is consistent with previous HIV testing data based on self-reports from medical providers and the general population.12,13 In addition, our analysis showed that the only factor independently associated with engaging in any HIV high-risk behavior was younger age. With respect to having a routine health checkup, the relationship with HIV testing is not surprising since health care utilization may increase opportunities for HIV testing.
Interestingly, certain indicators of health care access—for example, employment, poverty level, health insurance status, and unmet health care needs due to costs—were not independently associated with HIV testing and risk behavior. This may suggest that Monroe County, or more generally, New York State, offers a number of resources to ensure the availability of HIV testing in the community. In New York State, about 43% of non-elderly adults have been ever tested for HIV, which is higher than the US rate of 37%.3 Historically, New York State has led the nation in HIV prevention funding.37 Under the Affordable Care Act, a greater number of people will have access to HIV testing and more patients with HIV/AIDS will have their health insurance covered through Medicaid and state-based exchanges, given the updated recommendations of the USPSTF.7,8 Nevertheless, based on the current study, it seems likely that achieving optimal HIV testing rates will require additional strategies, as noted above.
When interpreting the findings reported here, several important limitations should be kept in mind. First, this study used cross-sectional survey data and, therefore, the temporal relationship between outcomes and potential risk factors could not be examined directly. Second, the information collected was based on self-reports. Having laboratory-confirmed, population-based HIV testing data from all practice settings would be ideal, but these are not currently available. Indeed, while mandated reporting of positive HIV results already exists, similar requirements for negative HIV results do not, which contribute to the general testing rate. Third, this population-based study represents the experience of an urban community, which may not be generalizable to other settings. However, the prevalence rates for a number of indicators reported here are comparable to those published from prior population-based data. Further, as discussed earlier, the analysis included a rigorous statistical approach that minimized the likelihood of spurious associations and optimized external sample validity.
Conclusion
In conclusion, using recent population-based data, our study found significant racial/ethnic disparities in HIV testing despite comparable patterns in HIV risk behavior among younger adults, with fewer Whites being offered testing in the past year than Blacks. Together, these findings suggest that steps beyond national guidelines and state laws are necessary to increase HIV testing rates overall. Targeted educational efforts to improve perceptions of risk and emphasize the value of routine screening may help in this regard, especially among Whites and, importantly, their health care providers.
Acknowledgments
No external funding was used for this analysis. The authors would like to thank Susette Langston for her assistance in the preparation of this manuscript.
Informed Consent
The data used for the analyses were collected as part of the routine surveillance efforts of the local health department and, therefore, institutional review board (IRB) approval was not required.
References
- 1. Chen M, Rhodes PH, Hall IH, Kilmarx PH, Branson BM, Valleroy LA; Centers for Disease Control and Prevention (CDC) . Prevalence of undiagnosed HIV infection among persons aged ≥13 years--National HIV Surveillance System, United States, 2005-2008. MMWR Morb Mortal Wkly Rep. 2012;61(suppl):57-64. [PubMed] [Google Scholar]
- 2. Centers for Disease Control and Prevention Early Release of Selected Estimates Based on Data from the 2012 National Health Interview Survey: Human Immunodeficiency Virus Testing. Atlanta, GA: Centers for Disease Control and Prevention; 2013. [Google Scholar]
- 3. . Kaiser Family Foundation Percentage of Persons Aged 18-64 Who Reported Ever Receiving an HIV Test. KCMU analysis of the Centers for Disease Control and Prevention (CDC)'s Behavioral Risk Factor Surveillance System (BRFSS) 2012. Results. Menlo Park, CA: Kaiser Family Foundation;2013. [Google Scholar]
- 4. EKOS Research Associates 2012 HIV/AIDS Attitudinal Tracking Survey: Final Report. Ottawa, Ontario: EKOS Research Associates; 2012. [Google Scholar]
- 5. Janssen RS, Holtgrave DR, Valdiserri RO, Shepherd M, Gayle HD, De Cock KM. The Serostatus Approach to Fighting the HIV Epidemic: prevention strategies for infected individuals. Am J Public Health. 2001;91(7):1019-1024. 10.2105/AJPH.91.7.1019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. . Branson BM, Handsfield HH, Lampe MA, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR. Recommendations and reports : Morbidity and mortality weekly report. Recommendations and reports / Centers for Disease Control. Sep 22 2006;55(RR-14):1-17; quiz CE11-14. [PubMed]
- 7. Bayer R, Oppenheimer GM. Routine HIV testing, public health, and the USPSTF--an end to the debate. N Engl J Med. 2013;368(10):881-884. 10.1056/NEJMp1214535 [DOI] [PubMed] [Google Scholar]
- 8. Martin EG, Schackman BR. Updating the HIV-testing guidelines--a modest change with major consequences. N Engl J Med. 2013;368(10):884-886. 10.1056/NEJMp1214630 [DOI] [PubMed] [Google Scholar]
- 9. Moyer VA; U.S. Preventive Services Task Force* . Screening for HIV: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2013;159(1):51-60. [DOI] [PubMed] [Google Scholar]
- 10. Neff S, Goldschmidt R. Centers for Disease Control and Prevention 2006 human immunodeficiency virus testing recommendations and state testing laws. JAMA. 2011;305(17):1767-1768. 10.1001/jama.2011.564 [DOI] [PubMed] [Google Scholar]
- 11. . Neff S, Goldschmidt R.. The Compendium of State HIV Testing Laws. San Francisco, CA: National HIV/AIDS Clinicians' Consultation Center;2012. [Google Scholar]
- 12. . New York State Department of Health Chapter 308 of the Laws of 2010: HIV Testing Law. Mandated Report. Albany, NY2012. [Google Scholar]
- 13. Centers for Disease Control and Prevention HIV Testing Trends in the United States, 2000-2011. Atlanta, GA: Centers for Disease Control and Prevention; 2013. [Google Scholar]
- 14. Murray K, Oraka E. Racial and ethnic disparities in future testing intentions for HIV: United States, 2007-2010: results from the National Health Interview Survey. AIDS Behav. 2014;18(7):1247-1255. 10.1007/s10461-013-0638-2 [DOI] [PubMed] [Google Scholar]
- 15. Woodring JV, Kruszon-Moran D, Oster AM, McQuillan GM. Did CDC’s 2006 revised HIV testing recommendations make a difference? Evaluation of HIV testing in the US household population, 2003-2010. J Acquir Immune Defic Syndr. 2014;67(3):331-340. 10.1097/QAI.0000000000000303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. . Centers for Disease Control and Prevention . HIV in the United States: At a Glance. Atlanta, GA2015.
- 17. Fleishman JA, Yehia BR, Moore RD, Gebo KA, Agwu AL; HIV Research Network . Disparities in receipt of antiretroviral therapy among HIV-infected adults (2002-2008). Med Care. 2012;50(5):419-427. 10.1097/MLR.0b013e31824e3356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gilmore Research Group, Monroe County Department of Public Health 2012 Monroe County Adult Health Survey: Data Collection Report. Seattle, WA: Gilmore Research Group; 2012. [Google Scholar]
- 19. Califoria Health Interview Survey. CHIS 2009 Methodology Series: Report 4 - Response Rates. Los Angeles, CA: UCLA Center for Health Policy Research; 2011. [Google Scholar]
- 20. Johnson TP, Wislar JS. Response rates and nonresponse errors in surveys. JAMA. 2012;307(17):1805-1806. 10.1001/jama.2012.3532 [DOI] [PubMed] [Google Scholar]
- 21. Centers for Disease Control and Prevention Behavioral Risk Factor Surveillance System: 2012 Summary Data Quality Report. Atlanta, GA: Centers for Disease Control and Prevention; 2013. [Google Scholar]
- 22. Keeter S, Kennedy C, Dimock M, Best J, Craighill P. Gauging the impact of growing nonresponse on estimates from a national RDD telephone survey. Public Opin Q. 2006;70(5):759-779. 10.1093/poq/nfl035 [DOI] [Google Scholar]
- 23. Davern M, McAlpine D, Beebe TJ, Ziegenfuss J, Rockwood T, Call KT. Are lower response rates hazardous to your health survey? An analysis of three state telephone health surveys. Health Serv Res. 2010;45(5 Pt 1):1324-1344. 10.1111/j.1475-6773.2010.01128.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Yeager DS, Krosnick JA, Chang LC, et al. HS J. Comparing the accuracy of RDD telephone surveys and the internet surveys conducted with probability and non-probability samples. Public Opin Q. 2011;75(4):709-747. 10.1093/poq/nfr020 [DOI] [Google Scholar]
- 25. . Battaglia MP, Izrael D, Hoaglin DC, Frankel MR Tips and tricks for raking survey data (a.k.a. sample balancing). Paper presented at: Proceeedings of the Suvey Research Methods Section of the American Statistical Association,2004; Alexandria, VA.
- 26. Centers for Disease Control and Prevention (CDC) . Methodologic changes in the Behavioral Risk Factor Surveillance System in 2011 and potential effects on prevalence estimates. MMWR Morb Mortal Wkly Rep. 2012;61(22):410-413. [PubMed] [Google Scholar]
- 27. Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed Nahwah, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 28. Raftery AE. Bayesian model selection in social research. Sociol Methodol. 1995;25:111-163. 10.2307/271063 [DOI] [Google Scholar]
- 29. .BICDROP1: Stata module to estimate the probability a model is more likely without each explanatory variable [computer program]. Chestnut Hill, MA: Boston College Department of Economics; 2005.
- 30. Takahashi TA, Johnson KM, Bradley KA. A population-based study of HIV testing practices and perceptions in 4 U.S. states. J Gen Intern Med. 2005;20(7):618-622. 10.1111/j.1525-1497.2005.0112.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wenrich MD, Curtis JR, Carline JD, Paauw DS, Ramsey PG. HIV risk screening in the primary care setting. Assessment of physicians skills. J Gen Intern Med. 1997;12(2):107-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Epstein RM, Morse DS, Frankel RM, Frarey L, Anderson K, Beckman HB. Awkward moments in patient-physician communication about HIV risk. Ann Intern Med. 1998;128(6):435-442. 10.7326/0003-4819-128-6-199803150-00003 [DOI] [PubMed] [Google Scholar]
- 33. Kerr SH, Valdiserri RO, Loft J, et al. Primary care physicians and their HIV prevention practices. AIDS Patient Care STDS. 1996;10(4):227-235. 10.1089/apc.1996.10.227 [DOI] [PubMed] [Google Scholar]
- 34. Haas DM, Coe RM. Do physicians discuss HIV and AIDS with patients? A survey of physician practices. J Community Health. 1997;22(6):401-416. 10.1023/A:1025155914757 [DOI] [PubMed] [Google Scholar]
- 35. Wong EY, Jordan WC, Malebranche DJ, et al. HIV testing practices among black primary care physicians in the United States. BMC Public Health. 2013;13(1):96. 10.1186/1471-2458-13-96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. American College of Obstetrics and Gynecology Committee on Obstetric Practice . ACOG Committee Opinion No. 418: Prenatal and perinatal human immunodeficiency virus testing: expanded recommendations. Obstet Gynecol. 2008;112(3):739-742. 10.1097/AOG.0b013e318188d29c [DOI] [PubMed] [Google Scholar]
- 37. Kaiser Family Foundation State Health Facts: The Centers for Disease Control and Prevention (CDC) HIV/AIDS Funding (FY 2012). Menlo Park, CA: Kaiser Family Foundation; 2013. [Google Scholar]