Abstract
Obesity has reached epidemic proportions with serious health consequences. Techniques used to measure body fat (BF) yield variable BF estimates, and this variability may lead to underestimation or overestimation of BF and subsequent treatment options. The measurements that are most accurate (Dual-Energy X-ray Absorptiometry (DEXA) and Air Displacement Plethysmography (ADP)) are expensive and often unavailable. The purpose of this study is to find the commonly available BF measurement that is the most accurate and practical for individual body types in the general population and compare these measurements to ADP (BOD POD®) as the standard. Field measurements include skinfolds (SKF), upper, lower, and whole body bioelectrical impedance (BI), waist and hip circumference ratios, body mass index calculations (BMI), and ADP. Our data indicate that BI is the least accurate measurement of body fat in males and females (paired t-tests of % body fat: BI vs. ADP, p0.05). However, preliminary data suggest female- specific SKF equations more accurately predict body fat in obese males than male-specific SKF equations. Given the current obesity trends, it is imperative to update these formulae to accurately reflect the current population.
Keywords: Air displacement plethysmography, bioelectrical impedance, body composition, fat mass, lean mass, skinfold equations
INTRODUCTION
Obesity is taking on epidemic proportions worldwide. According to the Centers for Disease Control (CDC), obesity (excessive body fat) is caused by an energy imbalance: consuming too many calories while expending too few. Although energy imbalance largely impacts whether a person will become obese, the contributions of genes, metabolism, behavior, environment, and socioeconomic status have an impact as well (21, 28). With notable exceptions, obesity is largely preventable with modifications to diet and exercise patterns
Obesity has health consequences beyond those associated with physical inactivity. According to the CDC, the major health risks include coronary heart disease, type II diabetes, hypertension, osteoarthritis, sleep apnea, and respiratory problems (16). Obesity can decrease life span by 3–7 years mostly because of vascular disease (8). Obesity also has economic consequences. Finkelstein et al., estimate that medical expenses due to obesity approach $147 billion dollars per year in 2008 in the United States (12), and this cost is expected to continue to rise. This is a major problem for all Americans including those who are obese and of normal body weight because everyone must pay for these medical expenses through increased taxes or increased cost of health care and rehabilitation. Obesity affects everyone, not only the person suffering from this disease; therefore, it is critical that obesity can be diagnosed and the treatment of obesity (loss of body fat) accurately measured.
Body fat can be estimated using various techniques, including skinfold thickness (SKF) (19, 20), bioelectrical impedance (BI) (5), hydrostatic weighing, air displacement plethysmography (ADP) (26), Magnetic Resonance Imaging (MRI), doubly labeled water (DLW) (33), and Dual-Energy X-ray Absorptiometry (DEXA). Estimating body fat using these methods yields variable results. ADP has been shown to be an accurate and reliable method of measuring body fat in adults (26). DEXA, MRI, and DLW are also highly accurate; however, draw backs, such as exposure to radiation, the time-consuming nature of measurements (33), limited availability of instrumentation, and high purchase and operating costs preclude the use of DEXA, MRI, and DLW on a broad scale. SKF measurements using equations from Jackson and Pollock have also been found to be accurate using different equations for males and females (19, 20). BI values using a four terminal device has been reported to be both accurate (8) and inaccurate (38), with variable data. Jackson and researchers found that BI is slightly less accurate than other body fat measurement techniques (18). There is currently conflicting research data on a variety of anthropometric measurements of body composition analysis.
All body fat measurement techniques described here estimate body fat; however, some methods more accurately predict body fat than others. These body fat measurements generate an estimate for both fat mass and lean mass (all other tissue). Other techniques, such as body mass index (BMI) (obesity equal to or greater than 30 kg/m2 and overweight or pre-obese as a BMI equal to or greater than 25 kg/m2), circumference measurements (neck, waist, thigh, etc.), and waist-to-hip circumference ratios are used to determine relative disease risk and classify individuals as normal body weight, overweight, or obese. In the field or clinical practice, inexpensive, portable, and easy to use devices or techniques are preferred in the determination of percent body fat or relative disease risk without sacrificing accuracy.
As a result of the current obesity epidemic, the population from whom the initial validation of SKF thicknesses, waist-hip ratios, and BI measurements as correlates with other body fat measurement techniques is no longer representative. Our study examines the variability of these body fat measurements when used for the current, more obese/overweight population. The purpose of this study is to illustrate the variability of commonly available body fat measurement techniques compared with ADP. We hypothesize that the accuracy of body fat measurements will decrease as percent body fat increases. Knowing that health risks increase as percent body fat increases, it is important to make a clinical diagnosis of obesity; therefore, practitioners should select the appropriate body fat measurement technique for clients based on body fat categories, sex, and body fat distribution. Our two primary objectives of this study are 1.) to illustrate the variability of commonly available body fat measurement techniques compared with ADP, and 2.) to assess how the amount of body fat mass will influence the accuracy of the body fat measurement.
METHODS
Participants
A total of 27 subjects, 11 males and 16 females between the ages of 19 and 66 years (table 1), were recruited from the Wright State University main campus population through fliers posted around campus. Subjects stated an interest through e-mail and were given more information on the study. A time was then arranged for the subjects to come to the research lab to have a body composition assessment. Informed consent was understood and signed by all participants before any testing began. The study protocol and consent form were approved by the Wright State University Institutional Review Board. Body composition assessment was performed using ADP, BI, SKF measurements, BMI, and waist and hip circumference measurements. These measurements were then used to classify participants into disease risk categories.
Table 1.
General characteristics of the sample population.
| Age (years) | Height (cm) | Weight (Kg) | % Body Fat (ADP) | |
|---|---|---|---|---|
| Mean | 34.22 | 169.94 | 81.28 | 29.5 |
| STDEV | 14.71 | 9.1 | 23.84 | 12.06 |
| Minimum | 19 | 156 | 44 | 2.5 |
| Maximum | 66 | 193 | 147 | 53.2 |
Protocol
Air Displacement Plethysmography
ADP (Life Measurement Inc., BOD POD®, Concord, CA, USA) is used to determine percent fat and fat free mass in adults. Mass is measured using an electronic scale and volume is determined through differential pressure transduction. Body density is calculated from mass and volume with the BOD POD® software. Percent body fat and lean tissue are determined from body density calculations. The subject wore a Lycra® swim suit, biking shorts, or similar clothing, and a swim cap covering the hair to prevent air trapping under clothing while all ADP tests were conducted. ADP is used in this study as the standard reference (± 3%) for percent body fat.
Bioelectrical Impedance
Upper (Body Logic Body Fat Analyzer, OMRON Healthcare Group, Kyoto, Japan), lower (Taylor Body Fat Scale, Taylor Precision Products, Oak Brook, IL, USA), and full body (Omron Full Body Sensor Body Composition Monitor and Scale, OMRON Healthcare Group, Kyoto, Japan) BI measurements were performed and percent body fat generated. BI works by sending a small electrical current of 50 kHz and 0.5 mA through the body to determine the amount of total body water. Body fat percentage is calculated through a formula that uses the measured body water, electric resistance, height, weight, age, and gender. Muscles, blood vessels, and bones have high water content and conduct electricity easily. Body fat, however, is a poor electrical conductor. There were no clinical validations for BI found, despite its common use as a tool for measuring body composition in a variety of non-research settings.
Skinfold Thickness measurements
SKF thickness measurements were determined at nine locations and two 3-site and one 7-site formulae (table 2) were used to calculate percent body fat for males (19) and females (20). Male formulae were used for male subjects and female formulae were used for female subjects only. All SKF thicknesses were taken on the right side of the body; duplicate measurements were taken for all SKF thicknesses after the first complete set of measurements were taken. If values were not within 1–2 mm, a third set of SKF thicknesses were taken. Research quality Lange Skinfold Calipers (Beta Technology, Santa Cruz, CA, USA) were used for all measurements.
Table 2.
Skinfold measurement formulae.
| Sex | Measurement locations | Formula |
|---|---|---|
| Male | Chest, midaxillary region, triceps, subscapular region, abdomen, suprailium, thigh | Body density = 1.112–0.00043499(sum of SKF)+0.00000055(sum of SKF)2−0.00028826(age) |
| Male | Chest, abdomen, thigh | Body density = 1.10938–0.0008267(sum of SKF)+0.0000016(sum of SKF)2−0.0002574(age) |
| Male | Chest, triceps, subscapular region | Body density = 1.112025–0.0013125(sum of SKF)+0.0000055(sum of SKF)2−0.000244(age) |
| Female | Chest, midaxillary region, triceps, subscapular region, abdomen, suprailium, thigh | Body density = 1.097–0.00046971(sum of SKF)+0.00000056(sum of SKF)2−0.00012828(age) |
| Female | Triceps, suprailium, thigh | Body density = 1.099421–0.0009929(sum of SKF)+0.0000023(sum of SKF)2−0.0001392(age) |
| Female | Triceps, suprailium, abdomen | Body density = 1.089733–0.0009245(sum of SKF)+0.0000025(sum of SKF)2−0.0000979(age) |
Body Mass Index
Calculated value; weight (kg)/height (m2) (Seca digital scale and stadiometer, Seca Corporation, Hanover, MD) (22).
Waist and Hip Circumference measurements
A nonelastic tape measure (Gulick Measuring Tape, The Therapy Connection at HPMS, Inc., Windham, NH, USA) was placed horizontally at narrowest part of the waist or slightly above the navel to measure waist circumference. Hip circumference was measured at the greatest posterior extension of the hip. Duplicate measurements were taken. If values were not within 5 mm of each other, a third measurement was taken. This ratio categorizes individuals as high disease risk or none (2).
Statistical Analysis
Variability among body fat measurement techniques was determined by Pearson correlations of skinfold thickness equations, bioelectrical impedance measurements, body mass index and waist-hip ratios with air displacement plethysmography were determined with P-values reported to show significant correlations and the coefficient of determination (R2) values reported to show the degree of variance between body fat measurement techniques. Significance was accepted when P<0.05. To best illustrate the variability in body fat measurement techniques, Bland-Altman graphs were made for skinfold thickness equations and bioelectrical impedance measurements compared with air displacement plethysmography. Our Bland-Altman graphs plot the difference between two body fat measurement techniques (such as female 7-site SKF vs. ADP, etc.) as a function of the average of those two body fat measurement techniques. Bias ± standard deviation of bias and the 95% limit of agreement for the Bland-Altman results are reported to show the average discrepancy between body fat measurement techniques. Variability in body fat measurement techniques between under/normal weight vs. overweight/obese individuals were made by comparing the fraction of the variance between body fat measurement techniques (BI, SKF) and ADP as R2. Figures were prepared and all statistical analyses were performed using GraphPad Prism version 5.04 for Windows, GraphPad Software, San Diego California USA, www.graphpad.com.
RESULTS
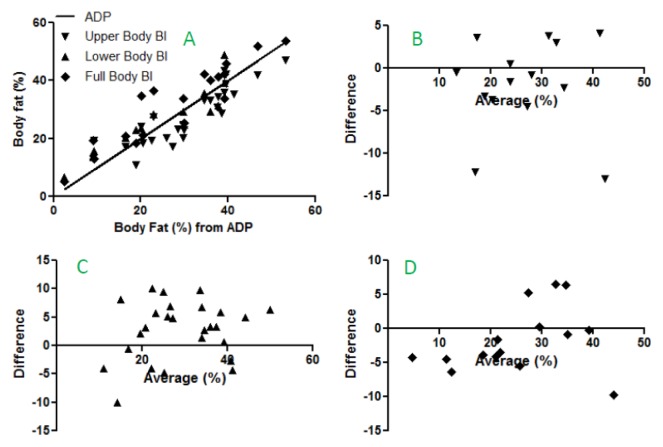
As one would expect given that each measurement made was a determination of body fat, significant correlations were found between all body fat measurement techniques and air displacement plethysmography (ADP) (P<0.05); however, the variance among these body fat measurement techniques is considerable (R2 ranging from 0.36 in the female waist-hip ratio to 0.94 in male 7-site skinfold thickness). Bioelectrical impedance (BI) measurements are not sex specific, so correlation between BI and ADP are made with all study subjects (figure 1). Pearson correlation of BI and ADP show a significant relationship for upper body BI (P<0.0001, R2=0.78), lower body BI (P<0.0001, R2=0.84), and full body BI (P<0.0001, R2=0.86) (figure 1a). Bland-Altman bias show variation in upper body BI (−1.9 ± 5.4 with 95% limits of agreement from −12.4 to 8.6; figure 1b), lower body BI (2.7 ± 5.2 with 95% limits of agreement from −7.4 to 12.8; Figure 1c), and full body BI (−1.7 ± 4.8 with 95% limits of agreement from −11.1 to 7.6; figure 1d).
Figure 1.
Comparisons of upper, lower, and full body bioelectrical impedance to air displacement plethysmography for combined male and female data. Pearson correlation of bioelectrical impedance and air displacement plethysmography (a); Pearson correlation P-value <0.0001. R2 values for upper body BI, lower body BI, full body BI are 0.78, 0.84, 0.86 respectively. Bland-Altman graphs for upper body BI (b), lower body BI (c), and full body BI (d).
Accuracy of body fat measurement techniques changes with percent body fat. For example, male SKF equations for under/normal weight males correlate strongly with body fat determined by ADP; however, for overweight/obese males, this correlation is greatly reduced (table 3). Panel A in figures 1–3 show Pearson Correlations for body fat measurement techniques compared with ADP. Individual data points above the line of identity are overestimates of body fat, while those that fall below the line of identity are underestimates of body fat. Panels B–D in figures 1–3 show Bland-Altman graphs which represent average discrepancy between body fat measurement techniques; while these graphs give some indication of a trend towards more or less variability, they do not statistically evaluate variability.
Table 3.
Variability of body fat measurement techniques between underweight/normal weight and overweight/obese individuals. R2 determined from correlation of measurement technique with air displacement plethysmography.
| Sex | Measurement technique | R2 (under/normal weight) | R2 (overweight/obese) |
|---|---|---|---|
| MF | Upper body bioelectrical impedance | 0.18 | 0.78 |
| MF | Lower body bioelectrical impedance | 0.96 | 0.54 |
| MF | Full body bioelectrical impedance | 0.70 | 0.74 |
| F | Female TST SKF | 0.05 | 0.56 |
| F | Female 7-site SKF | 0.16 | 0.56 |
| F | Female TSA SKF | 0.13 | 0.03 |
| M | Male CAT SKF | 0.97 | 0.48 |
| M | Male 7-site SKF | 0.99 | 0.70 |
| M | Male CTS SKF | 0.91 | 0.63 |
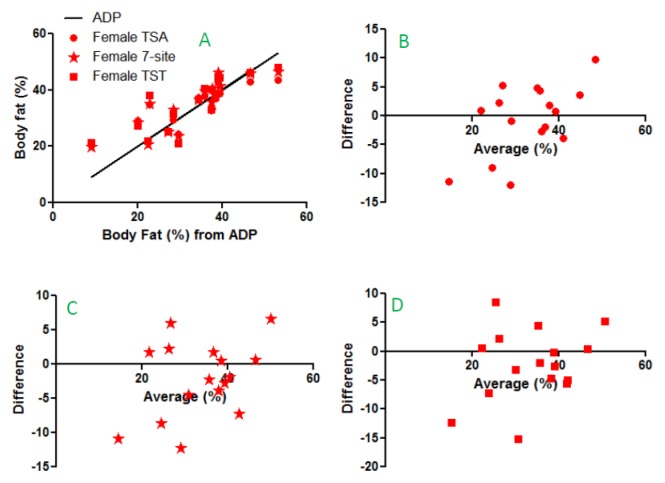
Figure 2.
Pearson correlation of female skinfold thicknesses and air displacement plethysmography (a). Pearson correlation P-value <0.0001. R2 values for Female TSA, 7-site, and TST SKF are 0.7, 0.74, and 0.68 respectively. Bland-Altman graphs for TSA SKF (b), 7-site SKF (c), and TST SKF (d).
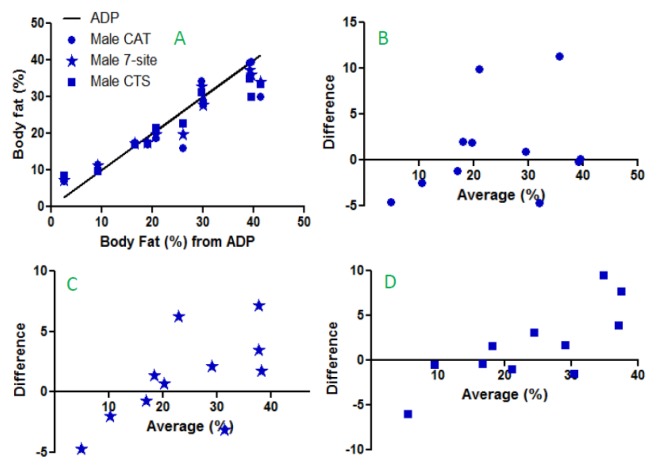
Figure 3.
Pearson correlation of male SKF and air displacement plethysmography (a). Pearson correlation P-value <0.0001. R2 values for Male CAT, 7-site, and CTS SKF are 0.83, 0.94 and 0.94 respectively. Bland-Altman graphs for CAT SKF (b), 7-site SKF (c), and CST SKF (d).
Skinfold thickness equations (SKF) are sex specific, so correlations between SKF and ADP are shown separately for females and males (figures 2 and 3). Pearson correlation of female SKF and ADP show a significant relationship for female TSA (triceps, suprailium, abdomen) SKF (P<0.0001, R2=0.70), female 7-site (abdomen, chest, subscapular, suprailium, triceps, midaxillary, thigh) SKF (P<0.0001, R2=0.74), and female TST (triceps, suprailium, thigh) SKF (P<0.0001, R2=0.68) (figure 2a). Bland-Altman bias show variation in female TSA SKF (−0.5 ± 6.1 with 95% limits of agreement from −12.5 to 11.5; figure 2b), female 7-site SKF (−2.1 ± 5.5 with 95% limits of agreement from −13.0 to 8.7; figure 2c), and female TST SKF (−2.3 ± 6.2 with 95% limits of agreement from −14.4 to 9.9; figure 2d).
Pearson correlation of male SKF and ADP show a significant relationship for male CAT (chest, abdomen, thigh) SKF (P<0.0001, R2=0.83), male 7-site (abdomen, chest, subscapular, suprailium, triceps, midaxillary, thigh) SKF (P<0.0001, R2=0.94), and male CST (chest, subscapular, triceps) SKF (P<0.0001, R2=0.94) (figure 3a). Bland-Altman bias show variation in male CAT SKF (1.2 ± 5.2 with 95% limits of agreement from −9.0 to 11.4; figure 3b), male 7-site SKF (1.1 ± 3.7 with 95% limits of agreement from −6.1 to 8.3; figure 3c), and male CST SKF (1.7 ± 4.4 with 95% limits of agreement from −6.9 to 10.2; figure 3d).
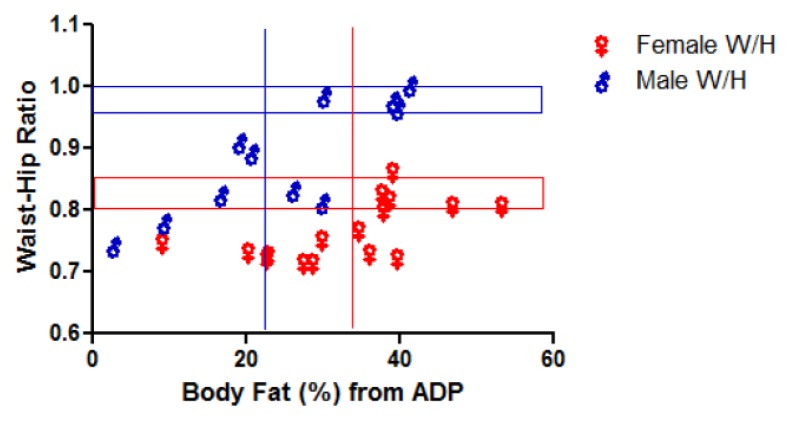
Waist-to-hip ratios are a useful measurement to get an idea of abdominal fat deposition compared with skinfold thickness which measure subcutaneous fat deposition. Waist-to-hip ratio for males and females are shown in figure 4 with the range of onset of high disease risk indicated with horizontal boxes (male in blue, female in red) for waist-to-hip ratio and vertical lines indicating the overweight mark for ADP. While the units for waist-to-hip ratio (unit-less) and ADP (%) are different, Pearson correlation for female waist-to-hip ratio is significant (P=0.01, R2=0.36) and male waist-to-hip ratio is also significant (P=0.001, R2=0.71).
Figure 4.
Waist-to-hip ratio is significantly correlated with air displacement plethysmography for both males (P=0.01, R2=0.36) and females (P=0.001, R2=0.71). Red and blue lines indicate normal female (red) and male (blue) waist-hip ratio ranges (7) and percent body fat values (23).
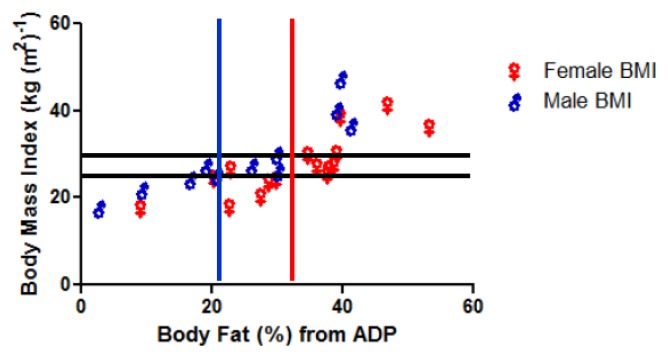
Body mass index (BMI) and ADP also have different units (kg (m2)−1 vs. %, respectively), yet are significantly correlated for female (P=0.0001, R2=0.65) and male (P=0.0002, R2=0.79). Pearson correlation for both female and male BMI with ADP are shown in figure 5. Horizontal lines indicate overweight and obesity onset for BMI, while vertical lines indicate the overweight mark for body fat percentage from ADP.
Figure 5.
Body Mass Index is correlated with air displacement plethysmography for both males (P=0.0001, R2=0.65) and females (P=0.0002, R2=0.79). Red and blue lines indicate normal female (red) and male (blue) percent body fat values (23). Horizontal black lines indicate overweight and obese BMI levels.
DISCUSSION
Our data illustrate the variability of commonly available body fat measurement techniques. Of the three BI measurements (upper body, lower body, and full body), lower body BI shows the greatest variability (figure 1c). Not surprisingly, 7-site SKF equations for both males and females are the most accurate of all of the SKF equations used given that the more data points in a relationship, the more likely it is to be accurate. For male SKF equations, there is an increase in variability with greater percent body fat (table 3, figure 3c, figure 3d). The variability in our data is similar to that reported in the anthropometric literature based on ethnicity, age, clinical disease manifestation, and athletic training type and intensity. For example, variability in the accuracy of bioelectrical impedance (BI) is evidenced by conflicting results in published research. BI is not accurate for measuring body fat in African American women (14), division 3 collegiate wrestlers (10), Japanese women (27), elderly subjects (4), obese women (15), overweight women (38), patients with end-stage renal disease (13), and in women with primarily abdominal body fat patterning (37). Despite the inaccuracies in these specific populations, BI was found to be accurate in middle aged men (31), nonobese women (15), elderly Mexican men and women (1), healthy adults (25, 5), elite adolescent male and female volleyball players (30), and lower body fat shaped women (37). In this study, we focused on body fat categories and the changing population structure (increase in percentage of overweight and obese people within the population). This is important because with the obesity epidemic, people and their health care providers need to know an accurate body fat percentage to realize their potential disease risk.
Bioelectrical impedance is a common technique used to measure body fat in the general population because it is easily accessible, simple, and inexpensive. In BI measurements (figure 1), lower body BI shows the greatest variability in percent body fat regardless of body composition (figure 1c) where the difference scale in the Bland-Altman graph is larger than upper body or full body BI. Given the prevalence of scales containing lower body BI measurement devices for use in the home, this inaccuracy may perpetuate misconceptions regarding body fat by the general population. Full body BI is designed to be more reliable, and in our study, showed the least variability (figure 1d); however, our full body BI measurements mostly underestimated percent body fat when compared with air displacement plethysmography (ADP) (figure 1a, figure 1d). We believe that underestimating percent body fat is more problematic than overestimating percent body fat. BI consistently underestimated percent body fat in obese children and adolescents (3, 24). Percent body fat from BI was also consistently underestimated in non-obese children (3). BI is less accurate than anthropometric prediction models (18). These results are consistent with the BI analysis in this study.
Skinfold thickness (SKF) measurements are purported to be more accurate (19, 20), but require training and experience to yield reliable estimates of percent body fat. In our study, the female 7-site SKF (abdomen, chest, subscapular, suprailium, triceps, midaxillary, thigh) exhibited the least variability when compared with ADP (figure 2c) likely because measuring seven anatomical locations yields a more accurate correlation with body fat than the other two 3-site SKF equations (triceps, suprailium, abdomen ( TSA) and triceps, suprailium, thigh (TST)). Female TSA overestimates percent body fat in underweight and normal weight females and underestimates percent body fat in overweight and obese females (figure 2a, figure 2b). There is less variability in SKF thickness measurements compared with ADP in males than in females (figure 3). All three male SKF thickness equations (chest, abdomen, thigh (CAT) and abdomen, chest, subscapular, suprailium, triceps, midaxillary, thigh (7-site) and chest, subscapular, triceps (CST)) tend to overestimate percent body fat in underweight males, are accurate for normal weight males; however, the greater the percent body fat, the less accurate are male SKF equations (figure 3b, figure 3c, figure 3d). These overweight and obese individuals are the groups for whom new SKF thickness equations are clearly indicated to reflect the increase in the percent of the population who are overweight or obese.
Accurate SKF measurements were reported by Sardinha et al. (31), who stated that SKF measurements using Jackson and Pollock equations are “fairly good and good” when compared to ADP and DEXA in middle-aged men. Similar results were found stating that SKF measurements using Jackson and Pollock equations are accurate (15, 30, 35, 6). However, SKF measurements using Jackson and Pollock equations should probably not be used to predict percent body fat in overweight or obese people (15, 6). In addition to variability and accuracy of SKF thickness measurements with body fat, studies using SKF measurements report variable results for different populations. SKF measurements using Jackson and Pollock equations have been found to be inaccurate in healthy Chinese adults (11), subjects with higher percent body fat and women (29), Hispanic men and women and African American men (17), formerly obese patients (32), high and low body density (36), obese women (15), adult males (9), obese Brazilian women (6), and in tracking percent fat changes in highly trained athletes (34).
In contrast to SKF thicknesses, which consider only subcutaneous fat, waist-hip ratio estimates body fat distribution accounting for body fat within the abdominal region, making it a valuable tool to assess health risk. An increased ratio (increased abdominal fatness) is associated with glucose intolerance, insulin resistance, elevated blood pressure, elevated blood lipid levels, cardiovascular disease, diabetes mellitus, hypertension stroke, and increased risk of death (7). Figure 4 shows comparisons between waist-hip ratio and ADP; horizontal boxes indicate the onset of high disease risk based on age, while vertical lines differentiate normal weight from overweight individuals. These two categorizations match well, with the exception of four females and two males who are categorized as overweight/obese based on ADP, but not at high disease risk, based on waist-hip ratio. Either waist-hip ratio is not a good predictor for these six individuals, or alternatively their excess fat may not pose a high disease risk.
Body mass index (BMI) is probably the most common, well-known, and utilized method of categorizing underweight, normal weight, overweight, and obese individuals. Based on Kyle et al.’s categorization levels for comparing BMI to percent body fat, our study subjects fit within these categories; however, even within the same BMI, body fat mass index varies considerably. For example, at a BMI of 25 kg/m2, body fat mass index ranges from 2.1 kg/m2 to 7.6 kg/m2 (23).
We hypothesized that the accuracy of field and common clinical practice body fat methods would diminish as body fat increased. Inaccuracies were most prevalent for male SKF equations as percent body fat increased. While care was taken to minimize measurement error, some variability in all of our comparisons may be due to hydration state of study subjects, when they had last exercised or eaten. Study subjects were instructed to not exercise or eat for four hours prior to body fat measurements; oral assurance of this was given by all study subjects, but there was no objective verification. Intra-individual variability among body fat measurement techniques requires solution. One method to resolve variability is to utilize multiple body fat measurement techniques for each individual.
It is imperative to update body fat measurement correlations with highly accurate body fat measurements (DLW, DEXA, or MRI) to reflect the change in our current population because of the obesity epidemic. Our study identifies this variability, and indicates that future studies of a much larger population reflecting an increase in body fat as well as how increased body fat affects ethnicities differently, ages differently, and disease state differently must now be done. If individuals have access to MRI, DEXA, ADP, or DLW, they can be confident of an accurate body fat estimation; however, if only simpler body fat measurement techniques (SKF, BI) are available to the general population, it is critical to create updated formulae for the determination of body fat. Until new equations are developed for obese populations, caution when using standard equations should be exercised. If individuals are misdiagnosed as being overweight, instead of obesity class 1, 2, or 3, they may be told to change their lifestyles without the assistance of medication or may not receive the treatment necessary for their condition. Obesity related diseases could then progress further without intervention. In contrast, if individuals are misdiagnosed as being obese when they are overweight or normal weight, expensive and unnecessary treatments may be used to help the patient lose weight, further contributing to increased health care costs.
ACKNOWLEDGEMENTS
We would like to thank the Department of Biological Sciences at Wright State University for the use of equipment. Research supported by the Wright State Women in Science Giving Circle grant (LKH), the Undergraduate Research Opportunities Program (BLR), and the University Honors program at Wright State University (BLR). We would also like to thank Deanne DuVal for her assistance. This research project partially fulfilled the requirements of an undergraduate honor’s thesis (BLR).
REFERENCES
- 1.Aleman-Mateo H, Esparza Romero J, Macias Morales N, Salazar G, Wyatt J, Valencia M. Determination of body composition using air displacement plethysmography, anthropometry and bio-electrical impedance in rural elderly Mexican men and women. J Nutr Health Aging. 2004;8:344–349. [PubMed] [Google Scholar]
- 2.American College of Sports Medicine. Guidelines for exercise testing and prescription. 8th ed. Philadelphia: Lippincott Williams & Wilkins; 2010. [Google Scholar]
- 3.Azcona C, Köek N, Frühbeck G. Fat mass by air-displacement plethysmography and impedance in obese/non-obese children and adolescents. Int J Pediatr Obes. 2006;1:176–182. doi: 10.1080/17477160600858740. [DOI] [PubMed] [Google Scholar]
- 4.Bertoli S, Battezzati A, Testolin G, Bedogni G. Evaluation of air-displacement plethysmography and bioelectrical impedance analysis vs. dual-energy X-ray absorptiometry for the assessment of fat-free mass in elderly subjects. Eur J Clin Nutr. 2008;62:1282–1286. doi: 10.1038/sj.ejcn.1602847. [DOI] [PubMed] [Google Scholar]
- 5.Biaggi R, Vollman M, Nies M, et al. Comparison of air-displacement plethysmography with hydrostatic weighing and bioelectrical impedance analysis for the assessment of body composition in healthy adults. Am J Clin Nutr. 1999;69:898–903. doi: 10.1093/ajcn/69.5.898. [DOI] [PubMed] [Google Scholar]
- 6.Bottaro M, Heyward V, Bezerra A, Wagner D. Skinfold method vs. dual-energy X-ray absorptiometry to assess body composition in normal and obese women. J Exerc Physiol. 2002;5:11–18. [Google Scholar]
- 7.Bray GA, Gray DS. Obesity Part 1 Pathogenesis. West J Med. 1988;149:429–441. [PMC free article] [PubMed] [Google Scholar]
- 8.Christakis N, Fowler J. The spread of obesity in a large social network over 32 years. New England J Med. 2007;357:370–379. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- 9.Clark R, Kuta J, Sullivan J. Prediction of percent body fat in adult males using dual energy X-ray absorptiometry, skinfolds, and hydrostatic weighing. Med Sci Sports Exerc. 1993;25:528–535. [PubMed] [Google Scholar]
- 10.Dixon C, Deitrick R, Pierce J, Cutrufello P, Drapeau L. Evaluation of the BOD POD and leg-to-leg bioelectrical impedance analysis for estimating percent body fat in National Collegiate Athletic Association Division III Collegiate Wrestlers. J Strength Cond Res. 2005;19:85–91. doi: 10.1519/14053.1. [DOI] [PubMed] [Google Scholar]
- 11.Eston R, Fu F, Fung L. Validity of conventional anthropometric techniques for predicting body composition in healthy Chinese adults. Br J Sports Med. 1995;29:52–6. doi: 10.1136/bjsm.29.1.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual Medical Spending Attributable To Obesity: Payer-And Service-Specific Estimates. Health Affairs. 2009;28(5):w822–w831. doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- 13.Flakoll P, Kent P, Neyra R, Levenhagen D, Chen K, Ikizler T. Bioelectrical impedance vs. air displacement plethysmography and dual-energy X-ray absorptiometry to determine body composition in patients with end-stage renal disease. J Parenteral Eternal Nutr. 2004;28:13–21. doi: 10.1177/014860710402800113. [DOI] [PubMed] [Google Scholar]
- 14.Gartner A, Dioum A, Delpeuch F, Maire B, Schutz Y. Use of hand-to-hand impedancemetry to predict body composition of African women as measured by air displacement plethysmography. Eur J Clin Nutr. 2004;58:523–531. doi: 10.1038/sj.ejcn.1601839. [DOI] [PubMed] [Google Scholar]
- 15.Heyward V, Cook K, Hicks V, Jenkins K, Quatrochi J, Wilson W. Predictive accuracy of three field methods for estimating relative body fatness of nonobese and obese women. Int J Sport Nutr. 1992;2:75–86. doi: 10.1123/ijsn.2.1.75. [DOI] [PubMed] [Google Scholar]
- 16.Hou X, Jai W, Bao Y, Lu H, Jiang S, Zuo Y, Gu H, Xiang K. Risk factors for overweight and obesity, and changes in body mass index of Chinese adults in Shanghai. BMC Public Health. 2008;8:389. doi: 10.1186/1471-2458-8-389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jackson A, Ellis K, McFarlin B, Sailors M, Bray M. Cross-validation of generalised body composition equations with diverse young men and women: The Training Intervention and Genetics of Exercise Response (TIGER) Study. Br J Nutr. 2009;101:871–878. doi: 10.1017/S0007114508047764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jackson A, Pollock M, Graves J, Mahar M. Reliability and validity of bioelectrical impedance in determining body composition. J Appl Physiol. 1988;64:529–534. doi: 10.1152/jappl.1988.64.2.529. [DOI] [PubMed] [Google Scholar]
- 19.Jackson AS, Pollock M. Generalized equations for predicting body density of men. Br J Nutr. 1978;40:497–504. doi: 10.1079/bjn19780152. [DOI] [PubMed] [Google Scholar]
- 20.Jackson AS, Pollock ML, Ward A. Generalized equations for predicting body density of women. Med Sci Sports Exerc. 1980;12:175–182. [PubMed] [Google Scholar]
- 21.Janssen I, Katzmarzyk P, Ross R. Waist circumference and not body mass index explains obesity-related health risk. Am J Clin Nutr. 2004;79:379–384. doi: 10.1093/ajcn/79.3.379. [DOI] [PubMed] [Google Scholar]
- 22.Khosla T, Lowe CR. Indices of obesity derived from body weight and height. Br J Prev Soc Med. 1967;21:122–128. doi: 10.1136/jech.21.3.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kyle UG, Schutz Y, Dupertuis YM, Pichard C. Body composition interpretation: Contributions of the fat-free mass index and the body fat mass index. Nutrition. 2003;19:597–604. doi: 10.1016/s0899-9007(03)00061-3. [DOI] [PubMed] [Google Scholar]
- 24.Lazzer S, Bedogni G, Agosti F, De Col A, Mornati D, Sartorio A. Comparison of dual-energy X-ray absorptiometry, air displacement plethysmography and bioelectrical impedance analysis for the assessment of body composition in severely obese Caucasian children and adolescents. Br J Nutr. 2008;100:918–924. doi: 10.1017/S0007114508922558. [DOI] [PubMed] [Google Scholar]
- 25.Levenhagen D, Borel M, Welch D, Piasecki J, Piasecki D, Chen K, Flakoll P. A comparison of air displacement plethysmography with three other techniques to determine body fat in healthy adults. J Parenteral Eternal Nutr. 1999;23:293–299. doi: 10.1177/0148607199023005293. [DOI] [PubMed] [Google Scholar]
- 26.McCrory MA, Gomez TD, Bernauer EM, Molé PA. Evaluation of a new air displacement plethysmograph for measuring human body composition. Med Sci Sports Exerc. 1995;27:1686–1691. [PubMed] [Google Scholar]
- 27.Miyatake N, Takenami S, Kawasaki Y, Fujii M. Comparison of air displacement plethysmograph and bioelectrical impedance for assessing body composition changes during weight loss in Japanese women. Diabetes Obes Metab. 2005;7:268–272. doi: 10.1111/j.1463-1326.2004.00395.x. [DOI] [PubMed] [Google Scholar]
- 28.Peeters A, Barendregt J, Willekens F, Mackenbach J, Al Mamun A, Bonneux L. Obesity in adulthood and its consequences for life expectancy: a life-table analysis. Ann Intern Med. 2003;138:24–32. doi: 10.7326/0003-4819-138-1-200301070-00008. [DOI] [PubMed] [Google Scholar]
- 29.Peterson M, Czerwinski S, Siervogel R. Development and validation of skinfold-thickness prediction equations with a 4-compartment model. Am J Clin Nutr. 2003;77:1186–1191. doi: 10.1093/ajcn/77.5.1186. [DOI] [PubMed] [Google Scholar]
- 30.Portal S, Rabinowitz J, Adler-Portal D, Burstein R, Lahav Y, Meckel Y, Nemet D, Eliakim A. Body fat measurements in elite adolescent volleyball players: correlation between skinfold thickness, bioelectrical impedance analysis, air-displacement plethysmography, and body mass index percentiles. J Pediatr Endocrinol Metab. 2010;23:395–400. doi: 10.1515/jpem.2010.061. [DOI] [PubMed] [Google Scholar]
- 31.Sardinha L, Lohman T, Teixeira P, Guedes D, Going S. Comparison of air displacement plethysmography with dual-energy X-ray absorptiometry and 3 field methods for estimating body composition in middle-aged men. Am J Clin Nutr. 1998;68:786–793. doi: 10.1093/ajcn/68.4.786. [DOI] [PubMed] [Google Scholar]
- 32.Scherf J, Franklin B, Lucas C, Stevenson D, Rubenfire M. Validity of skinfold thickness measures of formerly obese adults. Am J Clin Nutr. 1986;43:128–35. doi: 10.1093/ajcn/43.1.128. [DOI] [PubMed] [Google Scholar]
- 33.Schoeller D, van Santen E, Peterson D, Dietz W, Jaspan J, Klein P. Total bosy water measurement in humans with 18O and 2H labeled water. Am J Clin Nutr. 1980;33:2686–2693. doi: 10.1093/ajcn/33.12.2686. [DOI] [PubMed] [Google Scholar]
- 34.Silva A, Fields D, Quitério A, Sardinha L. Are skinfold-based models accurate and suitable for assessing changes in body composition in highly trained athletes? J Strength Cond Res. 2009;23:1688–1696. doi: 10.1519/JSC.0b013e3181b3f0e4. [DOI] [PubMed] [Google Scholar]
- 35.Sinning W, Dolny D, Little K, Cunningham L, Racaniello A, Siconolfi S, Sholes J. Validity of “generalized” equations for body composition analysis in male athletes. Med Sci Sports Exerc. 1985;17:124–130. [PubMed] [Google Scholar]
- 36.Smith J, Mansfield E. Body composition prediction in university football players. Med Sci Sports Exerc. 1984;16:398–405. [PubMed] [Google Scholar]
- 37.Swan P, McConnell K. Anthropometry and bioelectrical impedance inconsistently predicts fatness in women with regional adiposity. Med Sci Sports Exerc. 1999;31:1068–1075. doi: 10.1097/00005768-199907000-00023. [DOI] [PubMed] [Google Scholar]
- 38.Varady K, Santosa S, Jones P. Validation of handheld bioelectrical impedance analysis with magnetic resonance imaging for the assessment of body composition in overweight women. Am J Hum Biol. 2007;19:429–433. doi: 10.1002/ajhb.20609. [DOI] [PubMed] [Google Scholar]