Abstract
Kinesthesia, balance and agility (KBA) neuromuscular exercises are commonly used for rehabilitation of lower extremity injuries. KBA combined with strength training (ST) reportedly improves function among persons with knee osteoarthritis (OA), but independent effects of KBA are unknown. The purpose of this study was to determine the efficacy of KBA exercises, independent of ST, to improve function among persons with knee OA. Twenty participants (69.3, SD 11.4 y) were randomized to 8 weeks, 3-days per week, instructor-lead KBA or ST groups. Self-reported physical function (difficulty with daily living activities such as walking, bending, stair climbing, etc.) was measured at baseline and every two weeks. Community physical activity level, negative and positive outcome expectancies for exercise, self-reported knee stability, and timed 10-stair climb, 10-stair descent, and ‘get up and go’ 15 m walk were measured at baseline and follow-up. Physical function improved 59% (p = 0.02) with KBA and 40% (p = 0.02) with ST at 8 weeks. Community physical activity level improved only in KBA (p = 0.04); knee stability improved in both KBA (p = 0.04) and ST (p = 0.01). There were no significant between-group differences (p > 0.05). In conclusion, both interventions appear to improve function and knee stability among persons with symptomatic knee OA. As KBA has never been studied as an independent treatment program, our results indicate it is a promising stand-alone intervention worthy of further study.
Keywords: Degenerative arthritis, osteoarthrosis, neuromuscular training, proprioception, resistance exercise
INTRODUCTION
Symptomatic knee osteoarthritis (OA) is one of the most frequent causes of physical disability and pain among adults, affecting 12% of the U.S. population (5). It has been estimated that nearly half of all Americans will develop symptomatic OA in at least one knee by age 85 (22). Recent Osteoarthritis Research Society International (OARSI) recommendations for hip and knee OA management (33 – 35) reported 20 interventions were universally recommended by the published treatment guidelines reviewed. While OARSI failed to confirm the efficacy of some of these common treatments, e.g., ultrasound, massage, and heat/ice therapy (34), they continue to find good evidence for the efficacy of exercise interventions (35).
Various therapeutic exercise prescriptions have been used to help ameliorate knee OA symptoms and improve physical function related to activities of daily living (3, 4, 6, 8, 10, 13, 21, 28). Due to the prevalence of quadriceps weakness in persons with knee OA, leg strength training is commonly used in intervention programs (3, 21). Some evidence suggests that shorter programs that incorporate kinesthesia, balance and agility (KBA) techniques may result in more rapid symptom relief and functional improvements in comparison to traditional therapeutic exercise (6, 8).
KBA techniques are designed to improve dynamic joint stability using a series of physical activities which challenge a participant’s neuromuscular system to maintain balance and coordination. Most frequently, KBA is used to rehabilitate and prevent anterior cruciate ligament ruptures (11, 18, 19, 26) and ankle sprains (7, 20, 31) among athletes. KBA training has also been applied successfully in the rehabilitation of a 10-year old girl with bilateral knee juvenile rheumatoid arthritis (23). Among older persons, KBA training techniques, primarily balance training, are frequently used in fall prevention programs (17, 30). In recent years KBA training has been employed as a knee OA intervention. In a case study of an elderly female patient with dynamic knee instability related to OA, physical therapists reported success with a combination of KBA and therapeutic exercise (8). The patient’s recovery and return to recreational sports was rapid given that the program was only 12 sessions (2 per week for 6 weeks).
It has been established that proprioceptive acuity [i.e. the awareness of joint position (joint position sense), joint movement (kinesthesia), and sense of resistance (14)] declines both with age and as a result of osteoarthritis (29). These proprioceptive deficits may contribute towards reduced dynamic knee stability. KBA is designed to decrease proprioceptive impairment by using agility and balance exercises to activate, challenge, and adapt the nervous system’s proprioceptors. Decreasing proprioceptive deficit would thereby increase dynamic knee stability and improve activities of daily living function. In addition, joint instability and frontal plane joint laxity has been cited as a probable causative factor in both the development of knee OA and the further erosion of articular cartilage among persons with knee OA (15, 16, 27). Improved joint stability has the potential to both improve symptoms and slow the disease’s progression.
While empirical evidence is promising (3), only two published clinical trials of KBA training among persons with knee OA could be located (6, 28). The authors of an 8-week clinical trial (6) concluded that the addition of kinesthesia and balance exercises to strength training had added benefits over strength training alone in terms of all functional outcomes measured. However, it is unclear if the greater benefits obtained by the kinesthesia group are a direct result of the special training or simply from the greater total volume of training completed. Sekir and Gur (28) used a simple 6-week, two times per week multi-station KBA type exercise program to improve postural control, functional capacity, and knee pain among 22 persons with bilateral knee OA. Although the study group was small and the program had some strength training related elements included (i.e. stair climbing and chair rises), it does provide the only known published evidence to suggest that KBA type exercises in the absence of a specific strength training program may be beneficial.
With the exception of Sekir and Gur (28), KBA training for patients with knee OA has been advocated or studied only as an adjunct to traditional therapeutic training (e.g., 6, 8). The purpose of this pilot study was to determine the potential efficacy of KBA training as a stand alone intervention to improve physical function among persons with knee OA prior to embarking on a large scale clinical trial. A comparison was made with a “standard treatment” strength training protocol. It was hypothesized that KBA training would be more effective than strength training for improving physical function among persons with knee OA.
METHODS
Participants
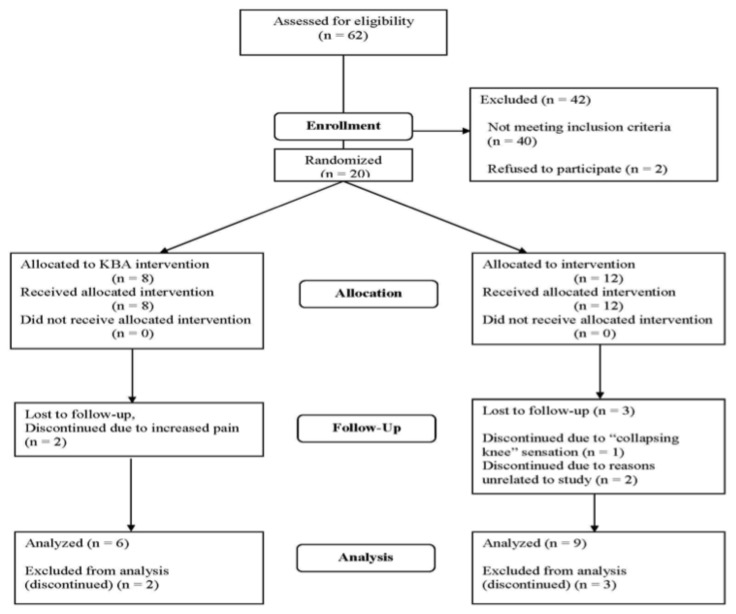
Twenty participants (69.3 SD 11.4 y) with physician diagnosed knee OA were recruited from the Tampa Bay Florida region via announcements, advertisements, word of mouth, and physician referral. Study inclusion and exclusion criteria are presented in Table 1. Among participants with bilateral knee OA the most symptomatic knee on the first day of testing, in the judgment of the participant, was designated as the study joint. A flow chart of participant recruitment is presented in Figure 1.
Table 1.
Study Inclusion and Exclusion Criteria.
| Inclusion Criteria: |
|---|
|
| Exclusion Criteria: |
|
|
|
Figure 1.
Flow Diagram of Subject Recruitment.
Protocol
The study was approved by The BayCare Pasco-Pinellas Institutional Review Board and registered at ClinicalTrials.gov (NCT00519922). A dynamic entry cohort was used. Testing was conducted at a not-for-profit research institute in Clearwater, Florida, USA. After explaining the risks, benefits, and procedures of the study, written informed consent was obtained. All baseline measures were repeated only at follow-up (8 weeks), with the exception of the osteoarthritis specific Western Ontario and McMaster University (WOMAC) scale (2), which was administered every two weeks. Height, weight, blood pressure, heart rate and a medical history were completed. Three paper and pencil surveys were administered: the Human Activity Profile (HAP) (9); the Self-Efficacy for Exercise (SEE) scale (25), and the WOMAC scale. WOMAC consists of three sub-scales titled: Pain, Stiffness, and Difficulty Performing Daily Activities [physical function (PF)]. PF was the primary outcome variable. Ancillary activities of daily living (ADL) outcomes included a timed 15-meter Get Up & Go (GUG) walk, timed 10-stair climb, and timed 10-stair descent. Reliability of GUG among persons with knee OA has been established (24).
Human Activity Profile
HAP estimated participants’ physical activity levels (outside the exercise program). HAP provides a Maximum Activity Score (MAS) which is the “highest oxygen-demanding activity that the respondent still performs” and an Adjusted Activity Score (AAS), “a measure of usual daily activities” (9).
Self-Efficacy for Exercise Scale
The SEE Outcome Expectancy for Exercise Positive (POEE) and Negative (NOEE) sub-scales determined participants’ beliefs about the benefits of exercise. SEE uses a 5-point Likert scale from 1 (strongly disagree) to 5 (strongly agree). Higher mean POEE scores indicate a more positive view of exercise benefits, while higher NOEE scores indicate a more negative view of exercise consequences.
Knee Stability
To assess knee stability, participants responded to the following question from the knee outcome survey - activities of daily living scale (KOS-ADLS) (12) at baseline and follow-up: To what degree does giving way, buckling, or shifting of the knee affect your level of daily activity? 0 – The symptom prevents me from all daily activity; 1 – The symptom affects my activity severely; 2 – The symptom affects my activity moderately; 3 – The symptom affects my activity slightly; 4 – I have the symptom but it does not affect my activity; 5 – I do not have giving way, buckling, or shifting of the knee.
Timed Functional Tests
All functional test protocols were explained and demonstrated by the investigator and timed with a stopwatch. GUG used two armless folding chairs placed 15 meters apart. The participant sat with arms folded across the chest. At the command “go” the participant rose from the chair, unfolded the arms, and walked as quickly as possible past the opposite chair. The fastest of three trials was recorded. For the stair climb, the participant stood at the bottom of the staircase. At the command “go” ten 15 cm high stairs were climbed as fast as possible. The stopwatch was stopped when both feet were on the landing. One trial was given and the time recorded. The same process was used from the top of the staircase for the stair decent. Participants were instructed not to pull themselves along the hand rail and to use a step over step pattern if possible.
Exercise Interventions
Using a random number table algorithm, participants were randomly assigned to a KBA group or comparator strength training (ST) group by a clerical staff member as they entered the study. Both were conducted in a not-for-profit hospital based wellness center in Clearwater, Florida, USA. Sessions were led by one of two instructors. Each holds an exercise science bachelors degree and is an American College of Sports Medicine Certified Health Fitness Specialist. The instructors were trained by the lead investigator, who also monitored sessions every 2–3 weeks to ensure protocols were followed. Both eight-week exercise interventions consisted of three 30 minute sessions per week on a Monday, Wednesday, Friday schedule. Both groups completed a five-minute walking warm-up and post-workout static stretching of the calf, hamstring, and quadriceps muscles. All exercises were progressed based on an individual participant’s tolerance for the given exercise.
KBA agility exercises (Table 2), were completed at a walking pace and progressed by adding more steps or increasing the pace. One set of agility exercises was conducted. Participants began with approximately 15 steps of each exercise and progressed to a maximum of approximately 75 steps. For balance training, Thera-Band® Stability Trainer pads (The Hygenic Corporation, 1245 Home Avenue, Akron, Ohio, USA) at 3 levels of softness were used. The pads allowed both appropriate starting difficulty and progression of difficulty level (i.e. the softer the pad, the greater the difficulty). Participants first demonstrated safe static balance on a stable surface (i.e. one-footed standing on floor for 10 seconds without losing balance) prior to progressing to the first level of the stability trainer pads. Once a participant demonstrated safe balance with both feet on the pad, he or she was progressed to one-footed standing on the pad. It was not required that any given participant progress through all levels of instability when a lower level continued to prove adequately challenging. Dynamic balance activities progressed in the same manner. Dynamic balance included the addition of small, rapid bouncing movements. In addition to softer pads, dynamic balance difficulty progressed with the addition of limb movements to further perturb balance and stimulate neuromuscular control mechanisms. Up to three sets of up to 30 seconds of each balance exercise were conducted.
Table 2.
KBA Agility Exercises.
| Wedding march: Step forward and slightly to one side with leading foot, bring trailing foot together with leading foot; alternate leading foot |
| Backward wedding march: As above, stepping backward |
| High knees march: Walk forward while flexing hip about 90 degrees |
| Side stepping: Stand with feet together, step to side with leading foot, bring trailing foot back to leading foot; repeat for prescribed number of steps, then repeat in opposite direction |
| Semi-tandem walk: Walk heel-to-toe with heel landing just in front of and medial to great toe of opposite foot |
| Tandem walk: Advanced version of above; heel lands directly in front of opposite foot |
| Cross-over walk: Walk forward bringing each foot across midline of body |
| Modified grapevine: Step to side with right foot, bring left foot behind right, step to side with right, bring left in front of right; repeat for prescribed number of steps; change leading foot and repeat in opposite direction |
| Toe walking: Walk forward on toes |
| Heel walking: Walk forward on heels |
All training for the ST condition was conducted on stable surfaces (i.e. standing, on floor, or sitting in a chair) and was primarily composed of open chain exercises to reduce any unintended KBA training transfer effects. ST utilized body weight and Thera-Band® color coded latex-free exercise bands (The Hygenic Corporation, 1245 Home Avenue, Akron, Ohio, USA) to provide resistance. Resistance exercises (Table 3) were progressed according to the individual participant’s improvement by increasing repetitions or going to the next level of resistance band. Participants performed 10 – 15 repetitions of each exercise. Participants began with the heaviest band tolerable, pulled to a length that safely and comfortably allowed completion of the prescribed number of repetitions for each exercise with good form (e.g., a 10 or 15-repetition maximum or RM). If a given participant was not able to complete the prescribed RM for a given exercise with the lightest (yellow) resistance band, he or she began with the greatest number of repetitions tolerable. Once the prescribed RM of a given exercise could be completed without difficulty, the next level of resistance band was used. Participants generally increased one, and in some cases two, resistance levels over the course of the eight weeks.
Table 3.
Strength Training (ST) Exercises.
| Seated resistance band exercises: Ankle extension, ankle flexion, knee extension, knee flexion, hip abduction, hip adduction, hip internal rotation, hip external rotation, leg press (hip and knee extension) |
| Other: Standing hip hyper-extension with resistance band; standing wall slides (partial squats) with a small “play ball” behind the back; supine heel slides (hip and knee flexion and extension) |
Statistical Analysis
The pilot study evaluated the difference in physical functioning between two groups: KBA and ST. KBA and ST are the independent variables. Subjects were tested at weeks 0, 2, 4, 6, and 8 with the WOMAC. The repeated measures ANOVA is the obvious statistical test for these data. This ANOVA would test for a difference between the overall response profiles between the KBA and ST groups. However, as we had an unbalanced design (i.e. unequal # of subjects between the KBA group and the ST group) and some missing data, it was prudent to select an alternate statistical approach. We utilized the paired t-test which affords the ability to control for variation among our study subjects (32). T-tests were run to quantify if the changes in scores within groups were significantly different from zero (p < 0.05) at the four study time points (weeks 2, 4, 6, and 8). T-tests were also run with the ancillary outcomes (baseline versus follow-up) for the same purpose. Unpaired T-tests were run to quantify if the changes in scores between groups were significantly different from zero (p < 0.05). Statistical Analysis Software (SAS) Version 9.1.3 (SAS Institute, Cary, NC) was used for all analyses.
RESULTS
Participant characteristics at baseline are presented in Table 4. Fifteen of the 20 participants completed the study; six of eight in the KBA group and nine of 12 in the ST group. Only data from participants that completed the study could be analyzed. If there were missing data at a given time point, the baseline score of the participant with missing data was not factored into the mean for that baseline versus time-point analysis. Both KBA participants that discontinued cited increased knee pain. Among the three ST participants that discontinued, one reported an increased sensation of a “collapsing knee” and the other two cited reasons unrelated to the study.
Table 4.
Participant Characteristics at Baseline (means ± SD).
| KBA (n=8) | ST (n=12) | |
|---|---|---|
| Age (years) | 69.29 (± 11.36) | 72.4 (± 11.02) |
| Body Mass Index (kg/m2) | 33.3 (± 8.35) | 31.91 (± 6.46) |
| SBP (mmHg) | 120.4 (±10.77) | 120.83 (± 11.58) |
| DBP (mmHg) | 66.5 (± 8.8) | 63.17 (± 5.15) |
| Resting HR (bpm) | 71.8 (± 9.3) | 68.67 (± 8.54) |
| % Female | 75 | 83 |
SBP - systolic blood pressure; DBP - diastolic blood pressure; HR - heart rate
WOMAC results are presented in Table 5. In cases where a participant was not available to complete the WOMAC at a given time point, only baseline versus time point results of the participants with complete data at that time point could be analyzed.
Table 5.
WOMAC Mean Change Scores versus Baseline.
| KBA | Strength Training | |||||||
|---|---|---|---|---|---|---|---|---|
| Variable (week) | Δ (SD) | % Δ | n | p | Δ (SD) | % Δ | n | p |
| Pain (2) | 0.00 (5.70) | 00.0 | 5 | 1.00 | −1.44 (2.60) | 15.3 | 9 | 0.13 |
| Pain (4) | −1.40 (4.39) | 22.6 | 5 | 0.52 | −3.11 (3.55) | 32.9 | 9 | 0.03 |
| Pain (6) | −4.25 (1.70) | 54.8 | 4 | 0.02 | −4.87 (3.39) | 49.4 | 8 | 0.005 |
| Pain (8) | −2.67 (4.41) | 39.0 | 6 | 0.20 | −4.00 (4.79) | 42.4 | 9 | 0.04 |
| Stiff (2) | −0.80 (1.30) | 17.4 | 5 | 0.24 | −0.88 (1.27) | 19.0 | 9 | 0.07 |
| Stiff (4) | −1.33 (2.94) | 34.8 | 6 | 0.32 | −2.00 (1.50) | 42.9 | 9 | 0.004 |
| Stiff (6) | −1.75 (1.50) | 46.7 | 4 | 0.10 | −1.12 (0.79) | 25.0 | 8 | 0.18 |
| Stiff (8) | −1.83 (2.14) | 47.8 | 6 | 0.09 | −2.11 (1.49) | 45.2 | 9 | 0.0002 |
| PF (2) | −10.20 (7.46) | 31.0 | 5 | 0.04 | −0.04 (10.70) | 00.0 | 9 | 0.99 |
| PF (4) | −16.76 (11.39) | 54.7 | 6 | 0.02 | −8.00 (8.10) | 26.5 | 9 | 0.02 |
| PF (6) | −16.50 (5.69) | 56.4 | 4 | 0.01 | −9.37 (15.94) | 30.2 | 8 | 0.14 |
WOMAC = Western Ontario and McMaster University Osteoarthritis Index
Sub-scale maximums are Pain = 20, Stiffness = 8, Physical Function (PF) = 68
Baseline scores (SD), KBA: Pain = 6.83 (4.07), Stiffness = 3.83 (2.56), PF = 30.67 (9.97); Strength Training: Pain = 9.44 (3.28), Stiffness = 4.67 (0.87), PF = 30.22
The KBA group improved physical function per the WOMAC PF scale, versus baseline, at weeks 2, 4, 6, and 8 (p < 0.05). The ST group demonstrated improvement on this scale at weeks 4 and 8 (p < 0.05). While the absolute amount of change in PF was larger in the KBA group at each time point, between group analyses revealed no differences between KBA and ST. WOMAC Stiffness was improved only in the ST group at weeks 4 and 8 with no significant between group differences at any time point (p > 0.05). WOMAC Pain improved at week 6 in the KBA group and at weeks 4, 6 and 8 in the ST group (p < 0.05). As with the other sub-scales, there were no significant between group differences.
Ancillary results are presented in Table 6. HAP MAS improved at week 8 follow-up only in KBA (p < 0.05). Both KBA and ST reported improved knee stability on the KOS-ADLS question (p < 0.05). While the absolute improvement on the three timed activities was greater for the KBA group, GUG and stair descent reached statistical significance only in the ST group (p < 0.05). No significant between group differences were found on ancillary outcomes.
Table 6.
Ancillarv Results: Means and Change Scores, Follow-up versus Baseline within Groups
| Strength Training | KBA | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Pre(SD) | Post(SD) | Δ(SD) | % Δ | n | p | Pre(SD) | Post(SD) | Δ (SD) | % Δ | n | p |
| GUG (sec) | 10.14 (4.85) | 8.92 (3.94) | −1.51 (1.45) | 14.5 | 5 | 0.08 | 13.13 (2.90) | 11.79 (2.57) | −1.34 (1.24) | 10.3 | 9 | 0.01 |
| 10-Stair climb (sec) | 7.47 (6.12) | 6.05 (3.91) | −1.70 (3.14) | 22.0 | 5 | 0.29 | 7.75 (1.55) | 6.96 (1.70) | −0.78 (1.30) | 10.2 | 9 | 0.11 |
| 10-Stair descent (sec) | 9.14 (9.47) | 6.20 (5.46) | −3.79 (4.89) | 37.9 | 5 | 0.16 | 9.97 (4.73) | 7.66 (4.10) | −2.31 (2.51) | 23.2 | 9 | 0.02 |
| HAPMAS | 70.83 (12.84) | 74.00 (10.79) | 3.16 (2.78) | 4.5 | 6 | 0.04 | 70.44 (7.25) | 70.44 (8.89) | 0.00 (3.77) | 0.0 | 9 | 1.00 |
| HAPAAS | 61.16 (16.42) | 64.33 (12.18) | 3.16 (4.87) | 5.2 | 6 | 0.17 | 55.78 (10.71) | 56.33 (12.44) | 0.55 (10.41) | 1.0 | 9 | 0.88 |
| SEE-POEE (1–5) | 3.97 (0.40) | 4.20 (0.76) | 0.23 (0.59) | 5.8 | 6 | 0.53 | 3.84 (0.56) | 4.06 (0.40) | 0.22 (0.50) | 5.8 | 9 | 0.35 |
| SEE-NOEE (1–5) | 2.53 (0.62) | 2.43 (0.82) | −0.10 (0.45) | 4.0 | 6 | 0.82 | 3.35 (0.31) | 3.04 (0.42) | −0.31 (0.53) | 9.3 | 9 | 0.09 |
| Knee buckling (0–5) | 3.00 (1.41) | 4.60 (0.54) | 1.60 (1.51) | 53.3 | 5 | 0.04 | 2.11 (0.93) | 3.22 (1.09) | 1.11 (1.17) | 52.7 | 9 | 0.01 |
GUG: 15 meter Get Up & Go walk; HAP: Human Activity Profile (both scales’ maximum = 94); SEE: Self-efficacv for Exercise, POEE: Positive Outcome Expectancv for Exercise, NOEE: Negative Outcome Expectancy for Exercise
DISCUSSION
Despite the limitations of the study, most notably participant numbers, both KBA and ST appeared to improve symptoms and physical functioning among middle-aged and older persons with symptomatic knee osteoarthritis. Both groups reported an improved sensation of knee stability after the 8-week exercise programs. Improved knee stability is hypothesized to be responsible for symptomatic improvements among persons with knee OA (3, 8). On each WOMAC sub-scale, both groups exceeded an established minimum clinically important improvement of 20 – 25% (1) from week 4 onward. The HAP MAS result indicates that the KBA group improved their maximal functional capacity for community based physical activity. HAP AAS improved similarly but did not reach statistical significance. HAP MAS and AAS were virtually unchanged with ST. KBA appears to be a promising stand-alone intervention for improving function, given our finding that the differences in change scores were not significantly different between KBA and strength training, an accepted intervention for knee OA symptoms. Percentage improvements in pain and stiffness were also similar between the two groups, and community physical activity levels improved only in KBA. These results complement those of Sekir and Gur (28) in supporting the potential of KBA as an independent treatment option. Our results also provide the first indication that KBA might improve physical functioning more rapidly than ST (KBA, 31 % PF improvement at week 2 versus no change with ST).
It remains to be determined if a combination of these two interventions, as employed by Fitzgerald, et al. (8), and in a clinical trial by Diracoglu, et al. (6), would be superior to either alone. Further research is needed to compare independent KBA and ST protocols to combination protocols in order to determine the most efficacious approach.
These results are encouraging but must be interpreted within the study limitations. Due to the pilot nature of this study the sample size was small, and there was not adequate power to show statistical significance of differences between groups. The results of the pilot study justify the need for further research on the independent effects of KBA exercise training, a simple, cost-effective, potentially home-based treatment.
Summary and Conclusion
Symptomatic knee OA is a common and growing condition that limits physical activity and mobility among many older persons. Among non-surgical options, various exercise therapies have been consistently beneficial for ameliorating knee OA symptoms (35). Still, it is important to define efficacious exercise protocols that are easy for patients to learn and apply. Our preliminary results indicate that a simple program of balance and agility exercises may improve physical function, decrease knee instability and increase physical activity levels. Should larger, follow up studies validate these findings we would more confidently be able to advocate KBA programs as an intervention to provide an enjoyable, easy to conduct set of exercises to improve the symptoms of knee osteoarthritis.
REFERENCES
- 1.Barr S, Bellamy N, Buchanan WW, Chalmers A, Ford PM, Kean WF, Kraag GR, Gerecz-Simon E, Campbell J. A comparative study of signal versus aggregate methods of outcome measurement based on the WOMAC Osteoarthritis Index. J Rheumatol. 1994;21:2106–2112. [PubMed] [Google Scholar]
- 2.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 3.Bennell K, Hinman R. Exercise as a treatment for osteoarthritis. Curr Opin Rheumatol. 2005;17:643–640. doi: 10.1097/01.bor.0000171214.49876.38. [DOI] [PubMed] [Google Scholar]
- 4.Bennell KL, Hunt MA, Wrigley TV, Hunter DJ, McManus FJ, Hodges PW, Li L, Hinman RS. Hip strengthening reduces symptoms but not knee load in people with medial knee osteoarthritis and varus malalignment: a randomised controlled trial. Osteoarthritis Cartilage. 2010 Feb 6; doi: 10.1016/j.joca.2010.01.010. [DOI] [PubMed] [Google Scholar]
- 5.Dillon CF, Rasch EK, Gu Q, Hirsh R. Prevalence of knee osteoarthritis in the United States: Arthritis data from the third National Health and Nutrition Examination Survey 1991–94. J Rheumatol. 2006;33:2271–2279. [PubMed] [Google Scholar]
- 6.Diracoglu D, Aydin R, Baskent A, Celik A. Effects of Kinesthesia and Balance Exercises in Knee Osteoarthritis. J Clin Rheumatol. 2005;11:303–310. doi: 10.1097/01.rhu.0000191213.37853.3d. [DOI] [PubMed] [Google Scholar]
- 7.Eils E, Rosenbaum D. A multi-station proprioceptive exercise program in patients with ankle instability. Med Sci Sports Exerc. 2001;33:1991–1998. doi: 10.1097/00005768-200112000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Fitzgerald GK, Childs JD, Ridge TM, Irrgang JJ. Agility and Perturpation Training for a Physically Active Individual with Knee Osteoarthritis. Phys Ther. 2002;82:372–382. [PubMed] [Google Scholar]
- 9.Fix AJ, Daughton DM. Human Activity Profile professional manual. Lutz, Fl: Psychological Assessment Resources, Inc; 1988. [Google Scholar]
- 10.Hicks JE, Perry MB, Gerber LH. Rehabilitation in the Management of Patients with Osteoarthritis. In: Moskowitz, et al., editors. Osteoarthritis: Diagnosis and Medical/Surgical Management. 3rd Edition. Philadelphia, Pa: Lippincott, William & Wilkins; 2001. pp. 413–446. [Google Scholar]
- 11.Hurd WJ, Chmielewski TL, Snyer-Mackler L. Perturbation-enhanced neuromuscular training alters muscle activity in female athletes. Knee Surg Sports Traumatol Arthrosc. 2006;14:60–69. doi: 10.1007/s00167-005-0624-y. [DOI] [PubMed] [Google Scholar]
- 12.Irrgang JJ, Snyder-Mackler L, Wainner RS, Fu FH, Harner CD. Development of a patient-reported measure of function of the knee. J Bone Joint Surg Am. 1998;80(8):1132e45. doi: 10.2106/00004623-199808000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Lange AK, Vanwanseele B, Fiatarone Singh MA. Strength training for treatment of osteoarthritis of the knee: a systematic review. Arthritis Rheum. 2008;59:1488–1494. doi: 10.1002/art.24118. [DOI] [PubMed] [Google Scholar]
- 14.Lephart SM, Riemann BL, Fu FH. Introduction to the Sensorimotor System. In: Lephart, Fu, editors. Proprioception and Neuromuscular Control in Joint Stability. Champaign, Il: Human Kinetics; 2000. pp. xvii–xxiv. [Google Scholar]
- 15.Lewek MD, Ramsey DK, Snyder-Mackler L, Rudolph KS. Knee stabilization in patients with medial compartment knee osteoarthritis. Arthritis Rheum. 2005;52:2845–2853. doi: 10.1002/art.21237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lewek MD, Rudolph KS, Snyder-Mackler L. Control of frontal plane knee laxity during gait in patients with medial compartment knee osteoarthritis. Osteoarthritis Cartilage. 2004;12:745–51. doi: 10.1016/j.joca.2004.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu-Ambrose T, Khan KM, Eng JJ, Janssen PA, Lord SR, McKay HA. Resistance and agility training reduce fall risk in women aged 75 to 85 with low bone mass: a 6-month randomized, controlled trial. J Am Geriatr Soc. 2004;52:657–665. doi: 10.1111/j.1532-5415.2004.52200.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu-Ambrose T, Taunton JE, MacIntyre D, McConkey P, Khan KM. The effects of proprioceptive or strength training on the neuromuscular function of the ACL reconstructed knee: a randomized clinical trial. Scan J Med Sci Sports. 2003;13:115–123. doi: 10.1034/j.1600-0838.2003.02113.x. [DOI] [PubMed] [Google Scholar]
- 19.Mandelbaum BR, Silvers HJ, Watanabe DS, Knarr JF, Thomas SD, Griffin LY, Kirkendall DT, Garrett W., Jr Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am J Sports Med. 2005;33:1003–1010. doi: 10.1177/0363546504272261. [DOI] [PubMed] [Google Scholar]
- 20.McGuine TA, Keen JS. The effect of a balance training program on the risk of ankle sprains in high school athletes. Am J Sports Med. 2001;34:1103–1111. doi: 10.1177/0363546505284191. [DOI] [PubMed] [Google Scholar]
- 21.Mikesky AE, Mazzuca SA, Brandt KD, Perkins SM, Damush T, Lane KA. Effects of strength training on the incidence and progression of knee osteoarthritis. Arthritis Rheum. 2006;55:690–699. doi: 10.1002/art.22245. [DOI] [PubMed] [Google Scholar]
- 22.Murphy L, Schwartz TA, Helmick CG, Renner JB, Tudor G, Koch G, Dragomir A, Kalsbeek WD, Luta G, Jordan JM. Lifetime risk of symptomatic knee osteoarthritis. Arthritis Rheum. 2008;59:1207–1213. doi: 10.1002/art.24021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Myer GD, Brunner HI, Melson PG, Paterno MV, Ford KR, Hewet TE. Specialized neuromuscular training to improve neuromuscular function and biomechanics in a patient with quiescent juvenile rheumatoid arthritis. Phys Ther. 2005;85:791–802. [PubMed] [Google Scholar]
- 24.Piva SR, Fitzgerald GK, Irrgang JJ, Bouzubar F, Starz TW. Get up and go test in patients with knee osteoarthritis. Arch Phys Med Rehab. 2004;85:284–289. doi: 10.1016/j.apmr.2003.05.001. [DOI] [PubMed] [Google Scholar]
- 25.Resnick B, Jenkins LS. Testing the reliability and validity of the Self-Efficacy for Exercise scale. Nurs Res. 2000;49:154–159. doi: 10.1097/00006199-200005000-00007. [DOI] [PubMed] [Google Scholar]
- 26.Risberg MA, Mork M, Jenssen HK, Holm I. Design and implementation of a neuromuscular training program following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2001;31:620–631. doi: 10.2519/jospt.2001.31.11.620. [DOI] [PubMed] [Google Scholar]
- 27.Rudolph KS, Schmitt LC, Lewek MD. Age-related changes in strength, joint laxity, and walking patterns: are they related to knee osteoarthritis? Phys Ther. 2007;87:1422–1432. doi: 10.2522/ptj.20060137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sekir U, Gur HA. Multi-Station Proprioceptive Exercise Program in Patients with Bilateral Knee Osteoarthritis: Functional Capacity, Pain and Sensoriomotor Function. A Randomized Controlled Trial. J Sports Sci Med. 2005;4:590–603. [PMC free article] [PubMed] [Google Scholar]
- 29.Swanik CB, Rubash HE, Barrack RL, Lephart SM. The role of proprioception in patients with DJD and following total knee arthroplasty. In: Lephart, Fu, editors. Proprioception and Neuromuscular Control in Joint Stability. Champaign, Il: Human Kinetics; 2000. pp. 323–338. [Google Scholar]
- 30.Toulotte C, Theyenon A, Fabre C. Effects of training and detraining on the static and dynamic balance in elderly fallers and non-fallers: a pilot study. Disabil Rehabil. 2006;28:125–133. doi: 10.1080/09638280500163653. [DOI] [PubMed] [Google Scholar]
- 31.Verhagen EA, van Mechelen W, de Vente W. The effect of preventive measures on the incidence of ankle sprains. Clin J Sport Med. 2000;10:291–296. doi: 10.1097/00042752-200010000-00012. [DOI] [PubMed] [Google Scholar]
- 32.Walker, Glenn A. Common Statistical Methods for Clinical Research with SAS Examples. Cary, NC: SAS Institute, Inc; 1997. pp. 87–114. [Google Scholar]
- 33.Zhang W, Moskowitz RW, Nuki G, Abramson S, Altman RD, Arden N, Bierma-Zeinstra S, Brandt KD, Croft P, Doherty M, Dougados M, Hochberg M, Hunter DJ, Kwoh K, Lohmander LS, Tugwell P. OARSI recommendations for the management of hip and knee osteoarthritis, part I: critical appraisal of existing treatment guidelines and systematic review of current research evidence. Osteoarthritis Cartilage. 2007;15:981–1000. doi: 10.1016/j.joca.2007.06.014. [DOI] [PubMed] [Google Scholar]
- 34.Zhang W, Moskowitz RW, Nuki G, Abramson S, Altman RD, Arden N, Bierma-Zeinstra S, Brandt KD, Croft P, Doherty M, Dougados M, Hochberg M, Hunter DJ, Kwoh K, Lohmander LS, Tugwell P. OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines. Osteoarthritis Cartilage. 2008;16:137–62. doi: 10.1016/j.joca.2007.12.013. [DOI] [PubMed] [Google Scholar]
- 35.Zhang W, Nuki G, Moskowitz RW, Abramson S, Altman RD, Arden NK, Bierma-Zeinstra S, Brandt KD, Croft P, Doherty M, Dougados M, Hochberg M, Hunter DJ, Kwoh K, Lohmander LS, Tugwell P. OARSI recommendations for the management of hip and knee osteoarthritis: part III: Changes in evidence following systematic cumulative update of research published through January 2009. Osteoarthritis Cartilage. 2010;18:476–499. doi: 10.1016/j.joca.2010.01.013. [DOI] [PubMed] [Google Scholar]