Abstract
Symptomatic anterior instability of the hip is typically iatrogenic in nature and poses a challenging problem for the orthopaedist. With early recognition, capsular repair and plication are often effective in restoring stability. Cases involving multiple instability episodes or those with delayed presentation, however, may have patulous and deficient capsular tissue precluding successful capsulorrhaphy. Capsular reconstruction may play an important role in restoring stability in these difficult cases. We present an arthroscopic technique for iliofemoral ligament reconstruction, with Achilles tendon allograft, to address instability of the hip due to anterior capsular deficiency.
The hip is an inherently stable joint with highly congruent bony architecture, reinforcing capsular ligaments, and dynamic muscular stabilizers.1, 2 The iliofemoral ligament (IFL) has been recognized as the dominant anterior stabilizer of the hip, primarily resisting anterior translation of the femoral head and external rotation of the extended hip.2 Several reported cases of iatrogenic instability after hip arthroscopy led many authors to speculate that an unrepaired anterior capsulotomy or capsulectomy should be avoided in the at-risk patient with subtle or borderline dysplastic features,3, 4, 5, 6, 7, 8 especially when concomitant labral debridement and iliopsoas tenotomy are performed. Of these cases, 2 were salvaged with a total hip replacement,3, 6 2 were successfully treated with closed reduction and physiotherapy,8 2 underwent capsular repair or plication,5, 7 and 1 required open capsular reconstruction with iliotibial band autograft because of capsular deficiency.4 We present an arthroscopic technique for IFL reconstruction with Achilles tendon allograft (Fig 1) for recurrent anterior hip instability (Video 1).
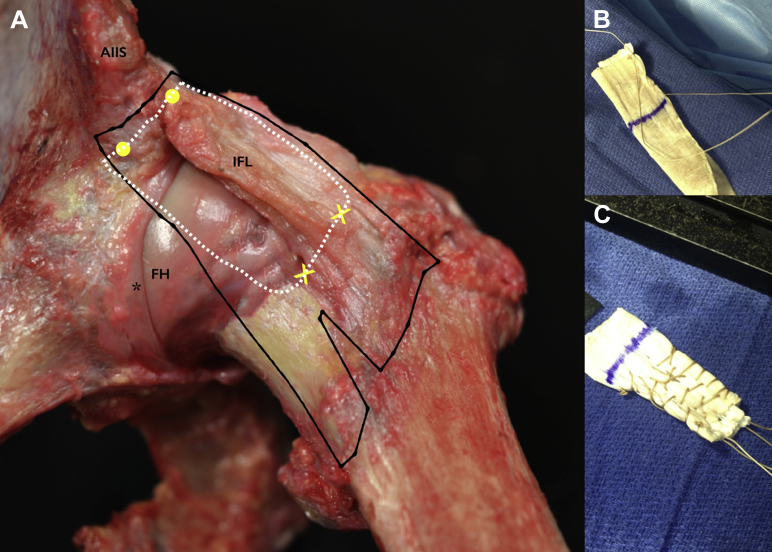
Fig 1.
Cadaveric specimen and graft preparation. (A) Left hip. The black lines outline the native iliofemoral ligament (IFL), the white dotted line represents the capsular allograft, the yellow dots represent the proximal anchors, the yellow X's represent the anastomosis to the zona orbicularis, and the asterisk indicates the labrum. (B) The Achilles tendon allograft is prepared by choosing a portion of uniform thickness and consistency, folding over once onto itself, and suturing the free ends with a running No. 2-0 Vicryl suture. (C) Substance of graft reinforced with running Krackow sutures using No. 1 Vicryl.
Photograph in A courtesy of Jorge Chahla. (AIIS, anterior inferior iliac spine; FH, femoral head.)
Surgical Technique
Preoperative and Intraoperative Evaluation
The indications for capsular reconstruction include hip instability with radiographic evidence of capsular deficiency. In addition, chronic iliopsoas inflammation due to capsular deficiency, in patients who are otherwise poor candidates for iliopsoas release, may be addressed with capsular reconstruction. Patients with dysplastic features who have previously undergone arthroscopic labral debridement, iliopsoas tenotomy, capsulectomy, or unrepaired capsulotomy are those most commonly encountered. These patients should also be evaluated for bony deficiency and torsional malalignment because inattention to these important factors may lead to failure of soft-tissue reconstructive procedures.
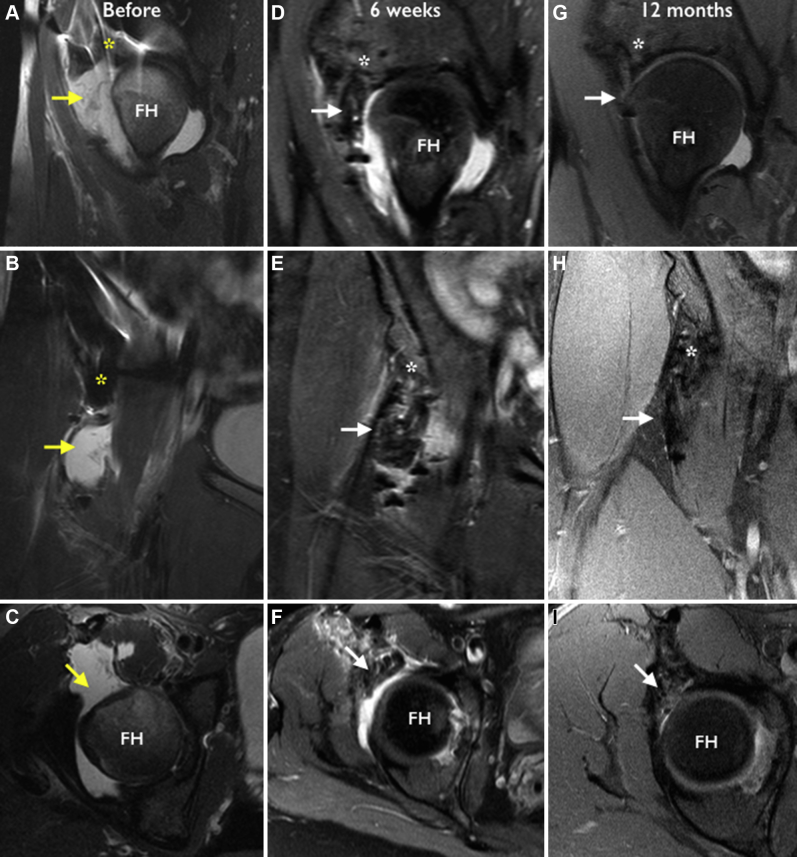
Preoperative evaluation is comprehensive and includes computed tomography of the pelvis and knees to assess acetabular coverage, acetabular version, and femoral torsion. Preoperative magnetic resonance imaging is necessary to evaluate for capsular and labral deficiency because both may need to be addressed simultaneously (Fig 2). The Beighton score for ligamentous laxity is computed. General anesthesia is induced with muscle relaxation to allow for adequate hip distraction and safe instrumentation. Before preparation and draping, an examination under anesthesia is carried out to assess bilateral passive range of motion and joint laxity characteristics. The hip is moved through a full range of motion to try to assess the position of least stability, which is compared with the in-office examination findings. Fluoroscopic examination is performed with gentle manual distraction to assess laxity, and comparison is made with the contralateral side. Arthroscopy is carried out by a previously described technique with the patient in the supine position.9
Fig 2.
MRI of the right hip before and after capsular reconstruction with an Achilles allograft. Left column shows sagittal, coronal, and axial views of the hip joint, respectively, prior to surgery with the deficient anterior capsule (yellow arrows). Some proximal capsular stump can be visualized at its insertion beneath the anterior inferior iliac spine (AIIS) (yellow asterisks). MRI of the same hip 6 weeks post-op (D-F) and 12 months post op (G-I). Intra-articular fluid is fully contained and anterior capsular congruity has been re-established, as indicated by the white arrows. Proximal fixation anchors are indicated by the white asterisks. Black artifacts (seen mainly in D-F) represent suture and knots. (FH, femoral head; MRI, magnetic resonance image.)
Because of the presence of anterior capsular deficiency, the standard interportal capsulotomy is not necessary to improve the mobility of instrumentation. Typically, the iliopsoas muscle-tendon unit is directly apposed to the femoral head and anterior labrum, with no capsule between them (Fig 3A). The joint is carefully inspected, and pathology of both the central and peripheral compartments is addressed before proceeding with capsular reconstruction.
Fig 3.
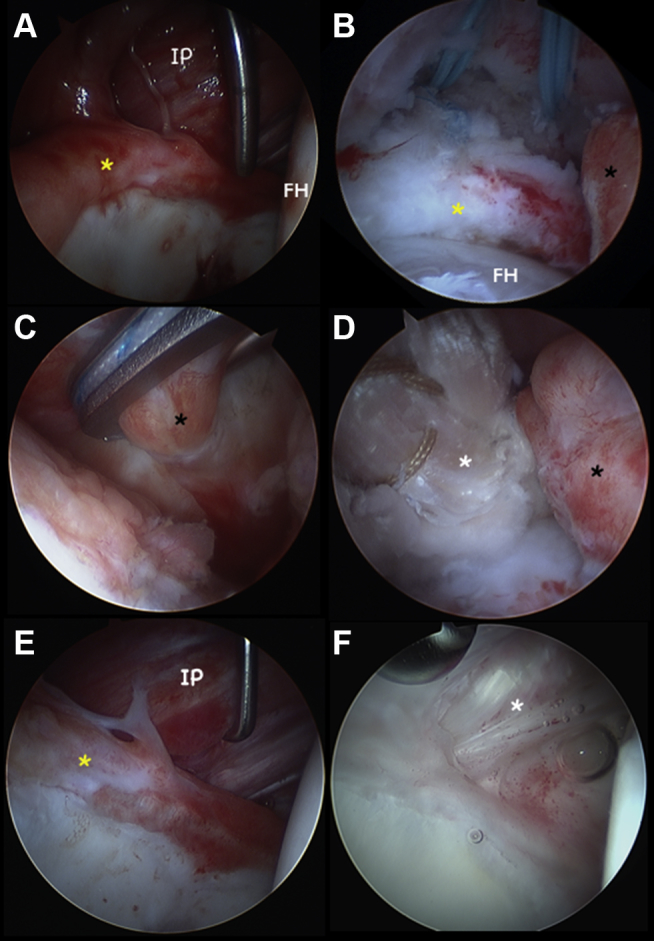
Intra-operative pictures of the same patient from Figure 2. (A) Iliopsoas muscle visualized with 30° arthroscope in mid-trochanteric portal under dry conditions, no capsule is seen. The iliopsoas is directly abutting the anterior labrum (yellow asterisk). (B) Arthroscope (70°) in mid-trochanteric portal viewing proximally in the peripheral compartment with traction released, with the labrum (yellow asterisk) resting nicely on the FH. Double loaded anchors placed in acetabular rim for proximal fixation. The distal capsular stump at the level of the zona orbicularis is seen to the right (black asterisk). (C) Speed stitch utilized to capture the distal capsular stump (black asterisk) near the zona orbicularis for suture passagee, while viewing “inside-out” with a 70° arthroscope in the mid-trochanteric portal. (D) Excellent approximation of distal capsular stump (black asterisk) with achilles graft (white asterisk) after tying the first suture. (E) Before view with 30-degree arthroscope through mid-trochanteric portal revealing inflamed anterior labrum (yellow asterisk, hours 1:30 to 3 are seen) post recurrent anterior dislocation. It is clear that no anterior capsule is present as the ilio-psoas muscle is seen (IP) behind/above the labrum. Femoral head is seen on the right. (F) A second look arthroscopy 12 month later depicting the same view. The well-incorporated Achilles allograft is seen (white asterisk). (IP, iliopsoas, FH, femoral head.)
Graft Preparation
An Achilles tendon allograft is prepared on the back table after inspecting for tissue integrity, quality, and size. The calcaneal bone block is removed before graft preparation. Sizing of the allograft should be performed according to preoperative magnetic resonance imaging measurements of the anticipated defect, along with intraoperative corroboration of these measurements at varying hip positions. The mid portion of the graft is used to ensure uniform consistency and thickness before preparation.
Preparation of Fixation Points
The acetabular rim is gently freshened with a burr (4.0-mm spherical burr; Stryker, Kalamazoo, MI) to expose the anatomic proximal insertion of the IFL: from the iliopsoas recess (approximately 3-o’clock position) to the posterolateral portion of the anterior inferior iliac spine (AIIS) (approximately 12-o’clock position). Care is taken to avoid excessive acetabuloplasty, unless required, as the rim is prepared for anchor placement and proximal graft fixation. All suture anchors (Iconix, 2.3-mm double loaded; Stryker) are drilled and inserted from the midanterior portal along the exposed rim, spaced 8 to 10 mm apart (Fig 3B). Straight and curved drill guides (12° or 25°; Stryker) should be available to achieve the appropriate drill trajectory. Two to three anchors are placed medially along the exposed rim, at the base of the AIIS and away from the labrum, re-creating the anatomic origin of the proximal IFL. The sutures associated with these anchors are marked with a surgical pen and organized with individual hemostats. Traction is released, and attention is directed to the peripheral compartment. The hip is moved through flexion and rotation to assess the capsular gap in these positions. Remnant capsular tissue in the area of the zona orbicularis (ZO) is freshened with an arthroscopic shaver in preparation for distal anastomosis (Fig 3C). The distal fixation point is a soft tissue–to–soft tissue anastomosis at the ZO, which often marks the distal extent of capsular deficiency in accordance with the majority of capsulectomy procedures.
Proximal Graft Fixation
The hip is placed in slight flexion for ease of peripheral compartment visualization and instrumentation. A third, distal anterolateral accessory (DALA) portal is established for graft manipulation. The sutures from the previously placed anchors are passed through the proximal portion of the graft using a free needle, with each pair of suture limbs spaced 2 to 3 mm apart. Only 1 of the double-loaded sutures is used to simplify suture management. The distance between successive pairs of suture limbs should correspond with the distance between anchors on the acetabular rim. Before knot tying, the most medial and lateral pairs of suture limbs are passed through a single knot pusher, which confers a tabularized shape to the graft on entry into the joint. We avoid the use of a cannula for this step because the more compliant native tissue can better accommodate the graft size required for this procedure. Once in the joint, anatomic positioning and fixation of the proximal graft is achieved by tying arthroscopic knots (Fig 3 D-F). This may be carried out with or without traction applied, according to surgeon preference. This stage is commonly performed while viewing in an inside-out manner as the knots are placed on top of the graft and underneath the iliopsoas muscle. Traction is released, and the distal portion of the graft is introduced into the joint by use of arthroscopic graspers and tissue manipulators through the DALA portal.
Distal Graft Fixation
Capsular augmentation to the ZO may be accomplished with a variety of suture-shuttling devices, yielding side-to-side and end-to-side anastomoses. We prefer the SpeedStitch (SS) suture passer (ArthroCare, Austin, TX) to secure the graft distally. The main advantage of the SS device is that it enables inside-out work with the arthroscope deep to the graft and obviates dissection of the musculocapsular plane for visualization, which can generate unnecessary bleeding (Fig 3C). Another important advantage of the SS device is the ability to grasp and manipulate tissue to assess thickness, mobility, and tension before suture passage. Clear cannulas are also helpful at this stage to simplify suture management (Transport Cannula; Stryker). A fourth, accessory portal may be useful to improve the trajectory for suture passage.
Distal fixation is performed with ultrahigh-strength suture or No. 2 Vicryl (Ethicon, Somerville, NJ). By use of the DALA portal and fourth, accessory portal, all sutures are shuttled through the distal graft and the ZO before knots are tied because suture passage is more difficult after knot tying. The hip is moved through a physiological range of motion to assess for soft-tissue and graft tension, which will guide postoperative guidelines for rehabilitation. Sutures are typically tied with the hip in 10° of flexion and neutral rotation, although the exact position may vary from patient to patient (Fig 3 D-F).
Postoperative Management
Postoperatively, the patient is placed in a hip abduction brace for 5 weeks (DJO Hip Brace; DJO Global, Vista, CA). The brace is locked in the range of 10° to 50° of flexion, preventing extension and external rotation of the hip joint. Non–weight bearing with crutches is maintained for the first 3 weeks, followed by toe-touch weight bearing during weeks 3 to 6 postoperatively. Hip extension and external rotation should be avoided for 6 weeks. Stationary bicycle exercises with minimal resistance should be initiated on postoperative day 1, with adherence to range-of-motion precautions. Passive circumduction is similarly performed within recommended limits starting on postoperative day 1. After 6 weeks, the patient is transitioned to full weight bearing and range-of-motion restrictions are lifted. Progressive strengthening and conditioning are carried out with formal physical therapy, and the patient is expected to start jogging at 12 weeks postoperatively, barring other restrictions from concomitant procedures.
Discussion
Multiple factors have been attributed to iatrogenic hip instability after hip arthroscopy: ligamentous laxity, previous capsulectomy, unrepaired capsulotomy, labral debridement, ligamentum teres debridement, long traction time, and traumatic fall.3, 4, 5, 6, 7, 8 Inadequate capsular repair after hip arthroscopy, especially in patients with dysplastic or borderline dysplastic characteristics, hyperlaxity, and anterior instability, has been reported to be a risk factor for hip instability.10 The IFL is a condensation of anterior capsular fibers originating at the AIIS and terminating along the intertrochanteric line, and it provides primary restraint against extension, external rotation, and anterior translation of the hip.2 Given these anatomic and biomechanical considerations, when repair of the IFL is carried out during hip arthroscopy, it is important to avoid external rotation in combination with extension during the first 4 to 6 weeks postoperatively to allow for adequate healing.
A deficient anterior capsule and IFL should be suspected in patients presenting with a history of multiple hip arthroscopies or open hip surgical procedures with persistent instability symptoms. Inadequate anterior restraint may lead to multiple episodes of subluxation or dislocation, which can further damage the anterior capsule and lead to chronic instability. In patients with dysplastic features and anterior undercoverage, the iliopsoas acts as a dynamic stabilizer and should be preserved.
Although several capsular repair techniques have been described,11, 12 to our knowledge, this is the first description of an arthroscopic reconstruction of the IFL. We have presented a safe, efficient, and reliable technique for arthroscopic capsular reconstruction. Technical pearls of this technique are described in Table 1.
Table 1.
Indications, Contraindications, and Technical Pearls for Capsular Reconstruction
| Indications |
| Symptomatic hip instability with radiographic evidence of capsular deficiency |
| Chronic iliopsoas inflammation due to anterior capsular deficiency |
| Contraindications |
| Coxarthrosis (Tönnis grade 3 or 4)—consider total hip arthroplasty |
| Acetabular dysplasia—consider periacetabular osteotomy with or without capsular reconstruction |
| Technical pearls |
| Perform appropriate graft sizing and preparation in accordance with preoperative MRI. |
| Minimize traction time while working in the peripheral compartment. |
| Use curved drill guides to optimize the trajectory for placement of all suture anchors along the acetabular rim. |
| Place the leg in gentle flexion and external rotation before tightening the graft distally. |
| Individualize the degree of capsular augmentation and desired position of stability for each patient. |
MRI, magnetic resonance imaging.
Hip instability due to capsular deficiency is a largely preventable complication of hip arthroscopy. Given the growing prevalence of hip arthroscopy, we aim to raise awareness of this unique iatrogenic complication, which may be avoided with careful preoperative planning and meticulous capsular management.
Footnotes
The authors report the following potential conflict of interest or source of funding: O.M-D. receives support from Smith & Nephew and ArthroCare.
Supplementary Data
A right hip is viewed with a 30° arthroscope inserted through the mid-trochanteric portal. Deficiency of the anterior capsule is noted, with the iliopsoas muscle-tendon unit directly abutting the anterior labrum. The acetabular rim is freshened with a burr, and all suture anchors are placed along the anatomic origin of the iliofemoral ligament from the 12- to 3-o’clock position, spaced 8 to 10 mm apart (2 to 3 anchors in total). Proximal sutures are passed through the graft before inserting the graft into the hip and securing with arthroscopic knots. Distal fixation is performed with a SpeedStitch device, securing the graft to the remnant capsule at the level of the zona orbicularis. During graft fixation, all viewing is carried out through the mid-trochanteric portal in the peripheral compartment, visualizing the articular side of the graft, while working through the midanterior portal and distal anterolateral accessory portal.
References
- 1.Bowman K.F., Jr., Fox J., Sekiya J.K. A clinically relevant review of hip biomechanics. Arthroscopy. 2010;26:1118–1129. doi: 10.1016/j.arthro.2010.01.027. [DOI] [PubMed] [Google Scholar]
- 2.Wagner F.V., Negrao J.R., Campos J. Capsular ligaments of the hip: Anatomic, histologic, and positional study in cadaveric specimens with MR arthrography. Radiology. 2012;263:189–198. doi: 10.1148/radiol.12111320. [DOI] [PubMed] [Google Scholar]
- 3.Benali Y., Katthagen B.D. Hip subluxation as a complication of arthroscopic debridement. Arthroscopy. 2009;25:405–407. doi: 10.1016/j.arthro.2009.01.012. [DOI] [PubMed] [Google Scholar]
- 4.Dierckman B.D., Guanche C.A. Anterior hip capsuloligamentous reconstruction for recurrent instability after hip arthroscopy. Am J Orthop (Belle Mead NJ) 2014;43:E319–E323. [PubMed] [Google Scholar]
- 5.Matsuda D.K. Acute iatrogenic dislocation following hip impingement arthroscopic surgery. Arthroscopy. 2009;25:400–404. doi: 10.1016/j.arthro.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 6.Mei-Dan O., McConkey M.O., Brick M. Catastrophic failure of hip arthroscopy due to iatrogenic instability: Can partial division of the ligamentum teres and iliofemoral ligament cause subluxation? Arthroscopy. 2012;28:440–445. doi: 10.1016/j.arthro.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 7.Ranawat A.S., McClincy M., Sekiya J.K. Anterior dislocation of the hip after arthroscopy in a patient with capsular laxity of the hip. A case report. J Bone Joint Surg Am. 2009;91:192–197. doi: 10.2106/JBJS.G.01367. [DOI] [PubMed] [Google Scholar]
- 8.Sansone M., Ahlden M., Jonasson P., Sward L., Eriksson T., Karlsson J. Total dislocation of the hip joint after arthroscopy and ileopsoas tenotomy. Knee Surg Sports Traumatol Arthrosc. 2012;21:420–423. doi: 10.1007/s00167-012-2300-3. [DOI] [PubMed] [Google Scholar]
- 9.Mei-Dan O., McConkey M.O., Young D.A. Hip arthroscopy distraction without the use of a perineal post: Prospective study. Orthopedics. 2013;36:e1–e5. doi: 10.3928/01477447-20121217-10. [DOI] [PubMed] [Google Scholar]
- 10.Bedi A., Galano G., Walsh C., Kelly B.T. Capsular management during hip arthroscopy: From femoroacetabular impingement to instability. Arthroscopy. 2011;27:1720–1731. doi: 10.1016/j.arthro.2011.08.288. [DOI] [PubMed] [Google Scholar]
- 11.Harris J.D., Slikker W., III, Gupta A.K., McCormick F.M., Nho S.J. Routine complete capsular closure during hip arthroscopy. Arthrosc Tech. 2013;2:e89–e94. doi: 10.1016/j.eats.2012.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mei-Dan O., Young D.A. A novel technique for capsular repair and labrum refixation in hip arthroscopy using the SpeedStitch. Arthrosc Tech. 2013;1:e107–e112. doi: 10.1016/j.eats.2012.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A right hip is viewed with a 30° arthroscope inserted through the mid-trochanteric portal. Deficiency of the anterior capsule is noted, with the iliopsoas muscle-tendon unit directly abutting the anterior labrum. The acetabular rim is freshened with a burr, and all suture anchors are placed along the anatomic origin of the iliofemoral ligament from the 12- to 3-o’clock position, spaced 8 to 10 mm apart (2 to 3 anchors in total). Proximal sutures are passed through the graft before inserting the graft into the hip and securing with arthroscopic knots. Distal fixation is performed with a SpeedStitch device, securing the graft to the remnant capsule at the level of the zona orbicularis. During graft fixation, all viewing is carried out through the mid-trochanteric portal in the peripheral compartment, visualizing the articular side of the graft, while working through the midanterior portal and distal anterolateral accessory portal.