Abstract
Background
Trigger points, which have been defined as highly localized, hyperirritable locations in a palpable taut band of skeletal muscle fibers, have been identified with a variety of musculoskeletal conditions. The incidence of trigger point pain is high, with studies showing them as the primary source of pain in 30-85% of patients presenting in a primary care setting or pain clinic. Dry needling has emerged as a possible intervention for trigger points, but its effectiveness has not yet fully been determined.
Purpose
To assess and provide a summary on the current literature for the use of dry needling as an intervention for lower quarter trigger points in patients with various orthopedic conditions.
Study Design
Systematic review
Methods
CINAHL, NCBI-PubMed, PEDro, SPORTDiscus, Cochrane Library, and APTA's PTNow were searched to identify relevant randomized controlled trials. Six studies meeting the inclusion criteria were analyzed using the PEDro scale.
Results
Four of the studies assessed by the PEDro scale were deemed ‘high’ quality and two were ‘fair’ quality. Each of the six included studies reported statistically significant improvements with dry needling for the reduction of pain intensity in the short-term. Only one study reported a statistically significant improvement in short-term functional outcomes; however, there was no maintenance of improved function at long-term follow-up. Furthermore, none of the studies reported statistically significant changes regarding the effect of dry needling on quality of life, depression, range of motion, or strength.
Conclusion
A review of current literature suggests that dry needling is effective in reducing pain associated with lower quarter trigger points in the short-term. However, the findings suggest that dry needling does not have a positive effect on function, quality of life, depression, range of motion, or strength. Further high quality research with long-term follow-up investigating the effect of dry needling in comparison to and in conjunction with other interventions is needed to determine the optimal use of dry needling in treating patients with lower quarter trigger points.
Levels of Evidence
1
Keywords: Dry needling, lower quarter, systematic review
INTRODUCTION
Trigger points (TrPs) have been associated with nearly every musculoskeletal pain condition, including but not limited to radiculopathies, joint dysfunctions, disc pathologies, tendonitis, craniomandibular dysfunction, spinal dysfunction, pelvic pain, urologic disorders, post-herpetic neuralgia, and complex regional pain syndrome.1,2 Although universally accepted criteria defining TrPs have not been established,3 they are typically classified as either active or latent.1 An active TrP is described as a highly localized, hyperirritable location in a palpable, taut band of skeletal muscle fibers.2 It is spontaneously painful and its palpation reproduces pain in typical patterns for each TrP that may, but need not radiate to distal sites.3–5 A latent TrP has the same physical characteristics as an active TrP, but requires manual palpation to elicit pain.4 Latent TrPs may reside in a pain-free skeletal muscle and become activated and become an active TrP when a continuous stimuli is applied.6 While literature regarding the prevalence of TrPs is sparse, epidemiologic studies from the United States have shown that TrPs were the primary source of pain in 30-85% of patients presenting in a primary care setting or pain clinic,2 whereas other studies have reported that TrPs are often undiagnosed by physicians and physical therapists.2,7–9 Undiagnosed TrPs may lead to chronic musculoskeletal conditions with progressive scar tissue formation.3,10 There is general agreement that development of TrPs can be the result of direct trauma, muscle overuse resulting from sustained or repetitive muscle contractions, or habitual postures that place abnormal stresses on various muscle groups.3,5 Evidence suggests that the first phase of TrP formation consists of the development of contractured muscle fibers or a taut band, although the exact mechanisms of this phenomenon are not well defined.5 It is hypothesized that TrPs develop at motor end plates, which leads to excessive release of acetylcholine resulting in a sustained contraction of sarcomeres.3 Sustained sarcomere contractions leads to compression of blood vessels, which creates hypoxic conditions.3 Due to local hypoxia, a sustained contraction cannot be achieved due to energy insufficiencies.11 Researchers also hypothesize that muscle pain causes spasms to develop, thus increasing pain intensity and the number of spasms in that muscle.5 Cagnie et al12 suggested that TrPs can provide nociceptive input that disturbs the balance in pain modulation due to impaired inhibition and/or enhanced pain facilitation, which may lead to central sensitization. While the proposed mechanisms of TrP formation remain debatable, evidence is consistent regarding the clinical manifestations. These include local and/or referred pain, disturbed motor function, muscle weakness, increased muscle tension preventing full lengthening of the muscle, restricted range of motion (ROM), and diminished joint function and stability.1,5,13
Many techniques have been used to treat TrPs, such as stretching, massage, ischemic compression, laser therapy, thermotherapy, ultrasound, transcutaneous electrical nerve stimulation (TENS), and biofeedback, but no one particular intervention has been proven successful.2,14–16 Another method gaining increased attention for treatment of TrPs is dry needling (sometimes referred to as intramuscular stimulation, Westernized acupuncture, and medical acupuncture).2 Dry needling is defined as the penetration of a solid needle through the skin without introduction of any drug10,17 to stimulate TrPs and connective tissue for the management of neuromusculoskeletal pain.10,17,18 It is cost-effective, low risk, minimally invasive, and is easy to learn through appropriate training and certification.2 Dry needling has been shown to be an effective method of treatment in alleviating symptoms caused by TrPs; however, the exact mechanism of action has yet to be determined.1,2,12 Proposed mechanisms include mechanical disruption of the integrity of dysfunctional endplates,19,20 alterations in the length and tension of muscle fibers and stimulation of mechanoreceptors,21 increased muscle blood flow and oxygenation,22–28 and endogenous opioid release affecting peripheral and central sensitization,29 among others.12 Strong pressure stimulation from a monofilament needle sends strong neural impulses to the dorsal horn, which breaks the TrP pain-spasm-pain cycle through the gate control theory.30 In a study by Kubo et al,22 researchers found that dry needling increased blood flow to the needle insertion site for up to 30 minutes after the needle was removed. An additional proposed mechanism of increased blood flow is due to an axonal reflex.31 Clinical studies have shown that insertion of a needle into the point of maximum pain and eliciting a local twitch response results in the largest therapeutic effects,32,33 such as restoration of ROM, less use of pain medication, improved quality of life (QoL), and pain relief.34
Kietrys et al34 conducted a systematic review and meta-analysis examining the effectiveness of dry needling for upper quarter myofascial pain. Three of the four studies 35–37 in the meta-analysis favored the use of dry needling and found a large therapeutic effect of dry needling compared to sham or control.34 To the best of the authors’ knowledge, there are currently no systematic reviews investigating the effectiveness of dry needling as an intervention for alleviating TrPs in the lower quarter, which includes the joints, musculature and connective tissue of the lumbar spine and lower extremity. The authors of this review hypothesize that a review of the literature will reveal similar outcomes in the therapeutic effect of dry needling in lower quarter TrPs as those shown in the systematic review and meta-analysis conducted by Kietrys et al34 for the upper quarter. In this review, lower quarter is considered to be all joints and musculature inferior to the thoracolumbar junction. The purpose of this systematic review is to assess and provide a summary of the current literature for the use of dry needling as an intervention for lower quarter TrPs in patients with various orthopedic conditions.
METHODS
Information Sources
A review of six databases was performed by four authors from November 2014 to February 2015. The databases included: Cumulative Index to Nursing and Allied Health Literature (CINAHL), United States National Library of Medicine (NLM) at the National Institutes of Health (Pubmed), Physiotherapy Evidence Database (PEDro), SPORTDiscus, Cochrane Library, and the American Physical Therapy Association's (APTA) PTNow.
Search and Eligibility Criteria
The search terms used in all databases included: ‘(dry needling OR acupuncture OR intramuscular stimulation) AND (trigger point OR myofascial pain)’. Selection of search terms were based on a publication by Dunning et al,17 which states that the APTA, among other sources, has also used “intramuscular stimulation” and “acupuncture” to describe the intervention of dry needling. Furthermore, “acupuncture” and “dry needling” were also used interchangeably in a recent APTA sponsored publication.38 Inclusion of “acupuncture” in the search terms produced a greater number of results; however, studies utilizing only traditional acupuncture, which relies on principles and diagnoses from Traditional Chinese Medicine (TCM),17 as the method of needle insertion were excluded from consideration. Search results were limited to: (1) clinical trials or reviews, (2) text in the English language, (3) use of dry needling to the lower extremity and/or lumbar region for various conditions, (4) inclusion of individuals with muscular TrPs in the lower quarter, and (5) use of dry needling compared to another intervention such as sham dry needling or no intervention. Only randomized clinical trials (RCTs) were considered for inclusion; however, reference lists of systematic reviews and literature reviews were explored for relevant studies related to dry needling. To maximize the number of search results, no date range limitations were placed on the search. The initial search using the aforementioned inclusion criteria returned studies between the years of 1983 to 2014. To be as inclusive as possible, all studies within this date range were screened for eligibility.
Study Selection
Four authors independently searched databases using the search terms listed above. The authors compiled a list of studies to be screened for eligibility based on title and abstract. After reading the full text of eligible studies, the individuals documented reasons for exclusion. The authors excluded studies that (1) utilized traditional acupuncture as the method of needle application, (2) were written in a non-English language, (3) included injection treatments, such as platelet-rich plasma or OnabotulinumtoxinA, (4) treated the upper quarter only, and (5) were not RCTs. Studies not published in the English language were excluded due to the potential risk of translation error associated with translating the text to English. Discrepancies in the studies to be included and/or excluded were discussed amongst all four authors until a consensus decision was reached.
Risk of Bias
Each of the six studies were independently reviewed by the same four authors and scored with the Physiotherapy Evidence Database (PEDro) scale. Discrepancies in scoring were resolved by a group consensus. The PEDro scale is a methodological quality assessment tool that was designed to evaluate RCTs and contains a 10-point scale to measure internal validity.39 There are 11 total items appearing on the PEDro scale; however, criterion one is not included in the overall score, as it represents external validity.39 Table 1 contains a description of each of the ten criteria. The studies included in this review were assigned methodological quality ratings as recommended by Walser et al.40 A PEDro score of seven or greater was considered to be of ‘high’ quality.40 Additionally, a study that received a score of five to six was said to be ‘fair’ quality and a score of four or below was found to be ‘poor’ quality.40
Table 1.
Pedro scoring of included studies
| Study | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total Score | Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cotchett et al.47 | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | 9/10 | High |
| Edwards et al.3 | Y | Y | Y | N | N | Y | Y | N | Y | Y | 7/10 | High |
| Huguenin et al.14 | Y | N | Y | Y | N | Y | Y | N | Y | Y | 7/10 | High |
| Mayoral et al.49 | Y | Y | Y | Y | N | Y | Y | N | Y | Y | 8/10 | High |
| Itoh et al.48 | Y | N | Y | Y | N | Y | N | N | Y | Y | 6/10 | Fair |
| Macdonald et al.50 | Y | N | Y | N | N | Y | Y | N | Y | N | 5/10 | Fair |
| % of yes per criterion | 100% | 50% | 100% | 66% | 0% | 100% | 83% | 16% | 100% | 83% | Score Avg: 7/10 |
Y = Criterion satisfied; N = Criterion not satisfied
2. Random allocation to groups
3. Allocation was concealed
4. Similar groups at baseline regarding prognostic factors
5. Blinding of all subjects
6. Blinding of therapists who administered the therapy
7. Blinding of all assessors who measured at least one key outcome
8. Measure of at least one outcome for more than 85% of subjects
9. All subjects received the intervention or “intention to treat” was stated
10. Between-group statistical comparisons for at least one key outcome
11. Point measures and measures of variability for at least one key outcome
Data Collection Process and Synthesis of Results
One individual extracted data from each article and the remaining three authors verified the information regarding study methods and outcome measures. The information extracted regarding methods was as follows: (1) study design, (2) study participants, (3) description of dry needling technique and the duration and frequency of treatment for experimental group, (4) description of intervention for comparison group, and (5) outcome measures including, but not limited to, the Visual Analog Scale (VAS), Foot Health Status Questionnaire (FHSQ) pain subscale, Short Form McGill Pain Questionnaire (SFMPQ), Western Ontario McMaster Universities Osteoarthritis Index (WOMAC) and Pressure Pain Threshold (PPT). Two impairment measures, ROM and peak isometric strength, were also extracted from the included studies. When considering outcome measures, the following information was extracted: (1) group means at the baseline and each follow-up period and (2) statistical analysis of group differences. Results from various reported outcome measures were analyzed to determine if the experimental group was considered superior, equal, or inferior to the comparison group. Although pain was assessed by an outcome measure in all included studies, a meta-analysis was not performed because the studies were not found to be clinically homogenous with regard to patient demographics, treatment duration or follow-up time frames.
While there was considerable variability in tests and measures, each of the six studies included in the review utilized the VAS to assess response to treatment. The VAS was found to have high test-retest reliability (r = 0.94, p < 0.001) before and after attending an outpatient clinic with literate patients.41 The intraclass correlation coefficient (ICC) was 0.97 with a confidence interval of 0.96 to 0.98.42 The SFMPQ was found to have high interrater reliability (ICC = 0.96) for total pain in a patient population with OA.41 Based upon construct validity, the SFMPQ moderately correlated to the WOMAC (r = 0.36) in patients with hip and knee OA.41 The WOMAC also has been found to have high test-retest reliability (ICC = 0.77) for patients with hip and knee OA.43 The WOMAC has been proven to have high test-retest reliability, not only when measured immediately, but when reassessed at six months (ICC = 0.91) and 12-months (ICC = 0.86) after initial injury.44 The Foot Health Status Questionnaire (FHSQ) pain subscale was found to have a Cronbach's alpha of 0.88 and an ICC of 0.86 for test-retest reliability.45
RESULTS
Study Selection and Characteristics
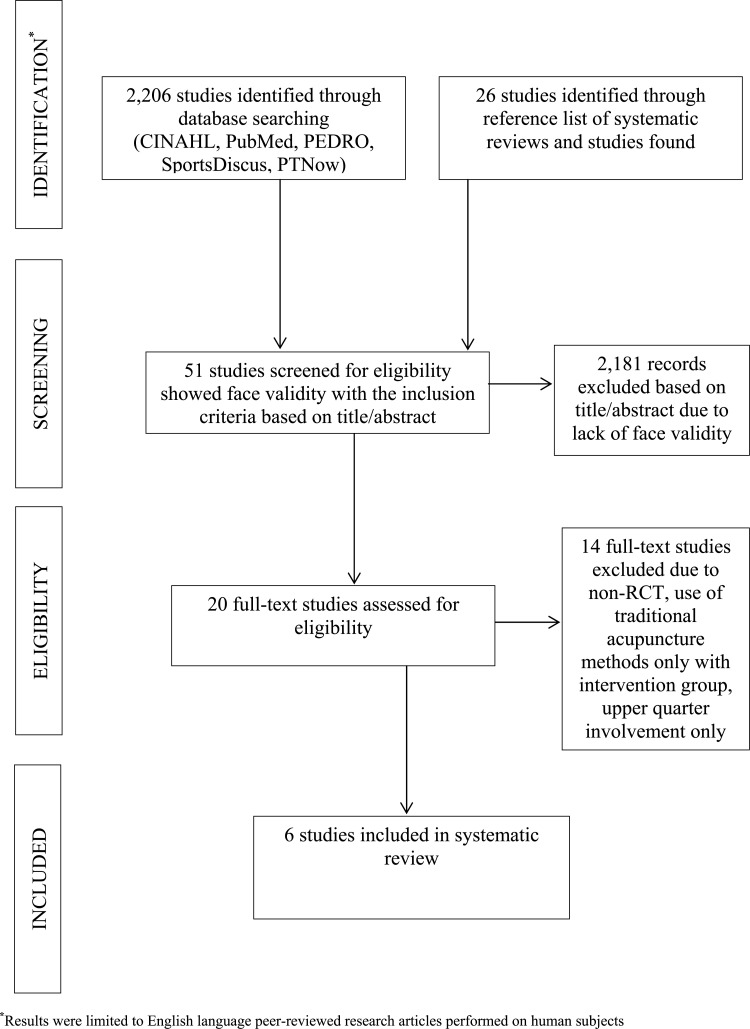
A total of 20 studies were considered for inclusion based on title and abstract. After a full-text review of each study was performed, six studies met the inclusion criteria (Figure 1). Reasons for exclusion included use of traditional acupuncture methods only and presence of upper quarter TrPs only with the intervention group. Each of the six studies selected for inclusion were RCTs. Outcome measures used to assess pain intensity included VAS, FHSQ pain subscale, SFMPQ, WOMAC, and PPT. Outcome measures used to assess function and disability included the FHSQ foot function subscale, Roland Morris Questionnaire (RMQ), and WOMAC physical function subscale. Impairment measures extracted from the studies included ROM and peak isometric strength. ROM measurements of the hip are commonly used to assess pain the lumbar region and posterior thigh.46 Measurements of hip ROM are used to monitor treatment response to gluteal trigger points.14 ROM of knee flexion and extension along with peak isometric strength of knee flexors and extensors at a single point were analyzed in post operative total knee arthroplasty (TKA) subjects. A detailed list of selected studies can be found in Table 2.
Figure 1.
Study Selection
Table 2.
Summary of included studies
| Study | Purpose of Study | Participants | Intervention | Time Frame of Study | Outcome Measures and Tests | Results |
|---|---|---|---|---|---|---|
| Cotchett et al47 | To evaluate how effective trigger point dry needling is as a treatment for plantar heel pain. | The study included 84 patients, >18 y.o. with plantar heel pain with symptom duration of at least one month. | Patients received either sham or real dry needling for 1 treatment per week, 30 minutes duration, for 6 weeks to the gastroc-soleus complex, quadratus plantae, flexor digitorum brevis, and abductor hallucis. Each needle was inserted for 5 minutes. | The subjects participated for 6 weeks and were followed for 12 weeks. Outcomes were measured at 2, 4, 6, and 12 weeks. |
|
Both groups had decreased pain after 12 weeks, evident by the statistically significant differences in VAS (p < 0.007) and FHSQ (p < 0.026) scores. Overall, real dry needling was favored over sham dry needling. |
| Edwards et al3 | To evaluate the effectiveness of combining superficial dry needling with active stretching for deactivating TrPs. | The study included 40 subjects, mostly female, with an active TrP. The TrP was most commonly reported in the upper body. | The subjects were divided into three groups: needling and stretching (13), stretching only (13), and control (13). The average number of dry needling sessions was 3.7. The needles were kept subcutaneously for an average of 3.4 minutes. | The groups received treatment for 3 weeks and had no treatment for the subsequent 3 weeks. |
|
The dry needling and stretching group required fewer follow-up visits after the study compared to the other groups. The mean number of treatment sessions was lower for the stretching only group (2.9) compared to needling and stretching group (4.6). SFMPQ decreased (p < 0.009) and PPT increased (p < 0.10) in the needling-stretching group. |
| Huguenin et al14 | To evaluate placebo and therapeutic dry needling on SLR††, pain, tightness, and hip IR in male athletes with posterior thigh pain due to TrPs. | The study included 85 male runners (59 completed measures before and after intervention, 58 completed the measures at 24 hours, and 52 completed the measures at 72 hours) with posterior thigh pain. | The subjects received either therapeutic or placebo dry needling to gluteal TrPs on one occasion. | Outcome measures were collected before treatment, immediately after, 24 hours post, and 72 hours post treatment for a total of 3 days for the study. |
|
No significant change in VAS scores for gluteal pain after running, but both groups improved in hamstring tightness (p < 0.001) and hamstring pain (p < 0.001). There was no significant change in ROM. Patient report was a good indicator of dry needling success. |
| Itoh et al48 | To determine whether acupuncture at TrPs is more effective than standard acupuncture for treating chronic low back pain in the geriatric population. | The study included 35 subjects (25 women, 10 men) age 65-81 with chronic low back pain. | Subjects were divided evenly into three groups: standard acupuncture, superficial acupuncture, and deep acupuncture. They received treatment to posterior thigh, gluteal, and lumbar musculature. There were a total of 6 30-minute treatment sessions, once per week. | The study was conducted over 12 weeks with two phases of treatment, each lasting 3 weeks. |
|
The group that received dry needling to deep TrPs reported less pain intensity (p < 0.5) and improved QoL (p < 0.01), compared to the other groups. |
| MacDonald et al50 | To examine the effectiveness of superficial acupuncture compared to placebo in the treatment of chronic low back pain. | The study included 17 subjects (12 female, 5 male) with chronic low back pain. | Eight subjects received acupuncture and 9 received placebo dry needling. Needles were inserted 4mm into the skin over TrPs for 5 minutes in the acupuncture group. The placebo group received electrical transcutaneous stimulation to the lumbar region. | Treatments were performed once per week for a maximum of 10 weeks. The number of treatments was reduced if further improvement failed to occur or if symptoms worsened in response to treatment. | No specific outcome measures were used, however, pain was assessed numerically (1- minimal, 2- moderate, 3-severe), area of pain was mapped on a dermatome body chart, and mood was measured from 1 (normal) to 5 (abnormal state). | The acupuncture group had pain relief (p < 0.01), reduction in pain activity score NS#, decreased physical signs (p < 0.01), and decreased pain severity (p < 0.01) compared to the placebo group. The measurements were statistically significant with p < 0.05. |
| Mayoral et al49 | To examine the effectiveness of dry needling to placebo in the prevention of pain after a total knee arthroplasty. | The study included 40 subjects (29 female, 11 male) with a scheduled total knee replacement surgery and presence of TrPs. | The subjects were assigned to a true dry needling group or a sham dry needling group. They were assessed prior to surgery and at months 1, 3, and 6 after surgery. Dry needling was applied under anesthesia. | Subjects were examined prior to surgery and at 1, 3, and 6 months post-surgery. |
|
Subjects who received true dry needling had less pain at 1 month with statistical significant differences in the VAS (p = 0.294). There was no statistical significance between groups for the WOMAC (p = 0.837 pain, p = 0.805 stiffness, p = 0.149 function) or ROM (p = 0.539) at baseline. |
QoL = Quality of Life; TrP = Trigger Point; TrPs = Trigger Points; ROM = Range of Motion; IR = Internal Rotation; SLR = Straight Leg Raise; NS = Not Significant
The average age of participants in the Cotchett et al47 and Edwards et al3 studies was 56 years. Participants in the Itoh et al48 and Mayoral et al49 studies had an average age of 72 years. Huguenin et al14 and MacDonald et al50 did not report age characteristics. Application of dry needling included either the “multiple insertion” or superficial technique, while comparison interventions included sham or placebo dry needling, placebo TENS, stretching or no treatment.3,14,47–50 The multiple insertion technique involves insertion of the needle followed by withdrawing it partially and then advancing the needle into the skin repeatedly.47 Placebo dry needling is applying the tip of a blunted needle on the surface of the skin.14 Duration and frequency of treatment ranged from a single session to one or more sessions per week for up to 10 weeks.3,14,47–50
Methodological Quality Assessment
Each of the six studies was independently reviewed by the same four authors who performed the database searches and assessed for methodological quality using the PEDro scale. Four of the studies3,14,47,49 were deemed to be high quality (PEDro score > 7), while two studies48,50 were determined to be fair quality (PEDro scores of 5 and 6).40 Four of the PEDro criteria were seen in all six studies: random allocation to groups, similar groups at baseline regarding prognostic factors, blinding of all assessors who measured at least one key outcome and between-group statistical comparisons for at least one key outcome.3,14,47–50 None of the studies included blinding of the therapists who administered the treatment, which was expected due to the use of dry needling as the intervention. 3,14,47–50 Table 1 contains the PEDro scores for each individual study.
Bias Within and Across Studies
Three of the studies3,14,50 demonstrated gender differences between groups that can be seen in Table 2. In the Mayoral et al study,49 VAS scores greater than 40-mm represented significant pain, which is present in almost half of the patients that undergo a TKA. As a result, Mayoral et al49 used a change in VAS of greater than 40-mm to demonstrate a significant decrease in VAS scores with dry needling instead of comparing all VAS scores. The use of VAS in this manner could introduce bias because Mayoral et al49 chose their own significant decrease in VAS scores instead of implementing a valid measure.51 Lastly, in the study by Huguenin et al,14 one author, McCrory, was affiliated with the study and the journal that it was published in. According to Thaler et al,52 publication bias exists when the publication of research depends on the nature and origin of the research and the direction of the results. Thus, the selective publication or non-publication of scientific literature has the potential to negatively influence the ability to draw objective conclusions regarding patient care and resource allocation.52 Being that the author was affiliated with the journal, the potential existed for publication bias.
Effect of Dry Needling on Pain Intensity
Cotchett et al47 (n = 84) investigated the effects of trigger point dry needling compared to sham dry needling in the management and treatment of plantar heel pain. Primary outcome measures were first-step pain (pain when getting out of bed in the morning) over the previous week, as measured with a 100-mm VAS (minimal important difference (MID) of 19 mm)53 and foot pain, which was measured using the pain subscale of the FHSQ, where 0 represents “worst foot health” and 100 represents “best foot health” (MCID = 13 points).47,53 At the primary end point (6 weeks), statistically significant differences existed between groups for first-step pain (p = 0.002) and FHSQ (p = 0.029), both favoring the treatment group.47 At 12 weeks, statistically significant differences in first-step pain (p = 0.007) and FHSQ (p = 0.026) favoring the treatment group persisted; however, the MCID for both outcome measures was not met at either measurement period.47
Edwards et al3 (n = 40) compared the effects of superficial dry needling and stretching (G1) to stretching alone (G2) and to no intervention (G3) in subjects with pain due to TrPs. Outcome measures used to assess pain were the SFMPQ and PPT of the primary TrP. Measurements were taken prior to intervention and at three and six week follow-ups. Fifty percent of the subjects in G1 presented with TrPs not in the upper quarter, while 16% and 47% of the subjects in G2 and G3, respectively, had TrPs outside of the upper quarter. At six weeks, statistically significant differences in favor of G1 existed in SFMPQ scores (p = 0.043) compared to G3 and in PPT scores (p = 0.011) compared to G2.3 No other statistically significant differences existed between groups at either follow-up point.
Huguenin et al14 (n = 59) evaluated the effect of therapeutic and placebo dry needling in subjects with posterior thigh pain. Pain in the gluteals and hamstrings was measured on separate VAS scales at rest and during activity. Measurements were performed at baseline, immediately after treatment, 24 hours after treatment, and 72 hours after treatment. There was no significant change in gluteal pain at rest or during activity at any measurement time frame following treatment.14 Both the treatment and placebo groups reported significant improvements in hamstring pain (p < 0.001) immediately after interventions, but there was no significant change in subsequent measurements and no significant difference in the magnitude of the change related to group allocation (p>0.013).14
Itoh et al48 (n = 35) conducted a study to determine whether acupuncture for TrPs is an effective treatment for LBP in the elderly when compared to standard acupuncture at traditional points. Subjects were divided into three groups: (1) superficial TrP (S-TrP), (2) deep TrP (D-TrP), and (3) standard acupuncture (SA). The S-TrP and D-TrP groups received treatment at TrPs, while the SA group received treatment at traditional points for LBP.48 Pain intensity was measured with the VAS, administered immediately before the first treatment and at one, two, three, six, seven, eight, nine, and 12 weeks after the first treatment.48 In the D-TrP group, statistically significant improvements were seen in VAS scores (p < 0.01) at four weeks compared to the initial pretreatment measurement; however, this improvement was reversed by the end of the study.48 There were no significant differences between pretreatment scores and follow-up scores for the SA or S-TrP groups.48
MacDonald et al50 (n = 17) investigated whether superficial acupuncture applied to TrPs was more effective than placebo TENS in treating chronic LBP. Subjective pain assessments included patient reported VAS scores at rest and during activity and patient perceived pain relief, also measured by VAS. Clinical observers noted the presence or absence of the following physical signs at the beginning and end of each course of treatment: gait impairment, spinal mobility impairment, loss of lordosis, scoliosis, impaired straight leg raising, pain on hip movements, crossed leg pain, femoral nerve stretch test, pelvic tilt, sensory deficits, motor deficits, and reflex changes.50 Only complete resolution of positive pre-treatment physical signs were taken into consideration when determining the effect of treatment on physical signs pain reduction.50 Observers also scored the severity of pain numerically and mapped the area of pain on a dermatome body chart.50 At the end of a course of treatment, the percent change in the severity of pain and the area it occupied on the dermatome chart were noted. Statistically significant differences were observed in the following outcomes: pain relief after each treatment (p < 0.01), activity pain score reduction (p < 0.05), physical signs reduction (p < 0.01), and severity and pain area reduction (p < 0.01).50
Mayoral et al49 (n = 40) examined whether dry needling of TrPs was superior to placebo in the treatment of pain following TKA. The outcome measures used to assess pain were the VAS and WOMAC. The WOMAC index is the most widely used instrument to evaluate symptomatology and function in patients with OA of the knee.49 It contains 24 questions: five about pain, two about stiffness, and 17 about difficulty with physical functions.49 Only the pain subscale scores are reported in this results section for the purposes of the systematic review. Measurements were taken at baseline and at one, three, and six months following surgery. The WOMAC pain scores were worse at baseline and at all follow-up examinations in the treatment group; however, the between group differences were not statistically significant.49 Because the baseline values of the VAS were higher in the treatment group, the authors analyzed the variation rate at one month post-surgery and percentage of subjects that had a VAS score >40-mm or were pain free (VAS = 0). Variation rate was calculated according to the following formula: [(value at one month – baseline value)/baseline value] x 100 for VAS scores.49 According to Brander et al,54 VAS scores > 40-mm are considered to represent a significant level of pain. Statistically significant differences in favor of the treatment group were found for variation rates for VAS score (p = 0.048), percentage of subjects with VAS scores >40 (p = 0.003), and percentage of subjects that were pain free (p = 0.042).49 The difference in VAS variation rate across groups suggests that subjects in the treatment group experienced a greater reduction in significant pain (VAS>40) compared to the sham group. The subjects in the treatment group reached the same pain levels (as measured by percentage of subjects with VAS>40) in one month as subjects in the sham group reached in six months.49 No values were reported for subsequent follow-up measurements.
Effect of Dry Needling on Function and Disability
Cotchett et al47 reported FHSQ foot function subscale scores at baseline and at six and 12 week follow-ups. No significant differences in FHSQ foot function subscale scores existed between the real and sham dry needling groups at either six week (p = 0.875) or 12 week (p = 0.889) measurements.47 Itoh et al48 measured functional impairment with the RMQ. In the D-TrP group, a statistically significant difference was observed between pretreatment and four week RMQ scores (p < 0.01), while no significant reductions in the scores for this period occurred in the SA or S-TrP groups.48 No significant differences existed between groups by the end of the study.48 Mayoral et al49 observed lower quarter functional impairment as measured by the WOMAC physical function scale in the treatment group compared to the sham dry needling group. However, the differences between groups were statistically insignificant at all measurement points.49 The remaining studies3,14,50 did not publish any data pertaining to function.
Peak isometric strength and ROM functional measurements were analyzed by Huguenin et al14 and Mayoral et al.49 Huguenin et al14 stated that there was no significant difference in hip internal rotation ROM and straight leg raise when comparing the treatment and control groups. Mayoral et al49 found no differences between groups regarding ROM and peak isometric strength at all follow-up visits. ROM results were explained by joint limitations due to the arthroplasty limitations and scar tissue formation in the knee joint capsule.49 Isometric strength was measured using a single contraction versus isotonic and endurance measures.
Discussion
The purpose of this systematic review was to determine whether there is sufficient evidence to support the use of dry needling as an effective intervention for the treatment of lower quarter TrPs in patients with orthopedic conditions.
Summary of Evidence
The literature review revealed six RCT studies3,14,47–50 that analyzed the effectiveness of dry needling for the reduction of symptoms associated with muscular TrPs. While considerable variations in dry needling methods exist, the studies included in this review employed either the superficial dry needling or “multiple insertion” technique. The superficial dry needling technique involved inserting the needle to a depth of 3 to 4-mm in the area immediately overlying the TrP.48,50 In the “multiple insertion” technique, needles were repeatedly inserted and withdrawn into multiple loci of TrP regions to a depth necessary to penetrate the TrP with the goal of eliciting a “local twitch response”,10 which correlates to increased effectiveness of dry needling, according to Hong.33 Three of the studies14,47,49 included in the review utilized the “multiple insertion” technique, two3,50 applied the superficial dry needling technique, and one48 analyzed both. Only one study48 compared standard acupuncture (SA) to superficial (S-TrP) and deep dry needling (D-TrP). In both SA and D-TrP groups, needles were inserted to a depth of 20mm, while the subjects in the S-TrP group received treatment consistent with the superficial technique described above.
The VAS was used to measure pain intensity in all six selected studies.3,14,47–50 MacDonald et al50 enlisted unbiased clinical observers to assess physical signs and symptoms of pain using non-standardized numeric scales. In addition, Edwards et al3 measured pain pressure threshold to assess pain response to dry needling. Overall, the results of the studies demonstrated statistically significant positive outcomes with the use of dry needling for reducing pain associated with lower quarter TrPs in the short-term. Only one study49 administered outcome measures beyond three months of treatment; however, a statistically significant difference in pain intensity between dry needling and sham groups was not observed at the six-month follow-up. The combination of dry needling and stretching used by Edwards et al3 showed greater improvement in symptoms compared to stretching alone. A notable finding by Itoh et al48 was the superior analgesic effect with increased depth of dry needling, as evidenced by greater reduction in pain intensity experienced by the D-TrP group compared to the S-TrP group. This is consistent with the findings of Ceccherelli et al55,56 and was also confirmed in a separate study conducted by Itoh et al.57 From the results of Itoh et al,48 researchers can speculate that dry needling combined with other interventions may enhance the positive effects on TrPs; however, there is not enough research at this time to confirm this hypothesis.
In addition to pain intensity, three of the six studies47–49 examined the effect of dry needling on function and disability. The researchers implemented different outcome measures to quantify these effects. Cotchett et al47 and Mayoral et al49 found no statistically significant functional improvement as measured by the FHSQ foot function subscale and WOMAC physical function scale, respectively. Itoh et al48 was the only one of the three studies to demonstrate that dry needling had a positive effect on function. Of the three groups in the study, only the D-TrP group showed a statistically significant improvement in RMQ scores, providing further evidence of improved outcomes with deep dry needling compared to superficial dry needling techniques.
Other outcome measures used to analyze the effects of dry needling included the Depression Anxiety Stress Scales (DASS-21), SF-36 for QoL, WOMAC stiffness subscale, FHSQ general foot health subscale, VAS for tightness, ROM, and peak isometric strength. Five3,47–50 out of the six studies found a statistically significant improvement in outcomes resulting from dry needling intervention.
According to the PEDro scale (Table 1), four3,14,47,49 of the six studies are high quality, indicating greater internal validity,24 while the remaining two studies48,50 received fair scores. The main threats to internal validity were non-concealed allocation to groups (50% of studies14,48,50 included), non-blinding of subjects and therapists (0% of studies3,14,47–50 included), paucity of attrition information (only 16% of studies48 included), and lack of intention-to-treat analysis (83% of studies3,14,48–50 included). All of the studies3,14,47–50 included are RCTs, which is considered level 1b quality of evidence.58 Considering the strength of the PEDro scores and level of evidence, the results of dry needling as an intervention are relevant to all healthcare providers assessing patients with pain and functional limitations associated with TrPs in the lower quarter.
Limitations
The primary limitation of this systematic review is the paucity of literature available based on the chosen inclusion criteria. The search of the previously stated databases returned a paltry amount of evidence investigating the effects of dry needling for lower quarter TrPs. As evidenced by Figure 1, of the 2,232 potential studies screened for eligibility, only six were identified for inclusion.
A second limitation of this review is the chosen search criteria placed on the studies. The Centre for Evidence-Based Medicine (CEBMa) ranks Systematic Reviews and Meta-analyses as level Ia and RCTs as Ib. Therefore, only RCTs were included in the search criteria in order to present findings based on the highest quality of evidence, as defined by the CEBMa.58 While the PEDro scale is specifically designed to assess the quality of RCTs, it was the sole method of investigating internal validity across all studies in the review. Clinically relevant findings from lower levels of evidence may have been excluded from consideration. The authors also did not include any unpublished studies or studies not written in the English language.
Another limitation was subject sample size and population. For example, five3,14,48–50 out of six studies included a relatively small sample of subjects, which ranged from 17 to 84 subjects (Table 2). In the study by Edwards et al,3 G2 included 13 subjects of which 84% had TrPs of the upper body, but the other groups were similar in composition. Three studies3,14,50 consisted of subject populations that were significantly different in regards to gender. Huguenin et al14 included 59 males recruited from Australian rules football teams.
Five of the six studies3,14,48–50 did not report any MCIDs in their publications. Cotchett et al47 was the only study to report MCIDs; however, the MCIDs were calculated by the authors, rather than adhering to published values.45,59 The majority of results were based upon statistical significance, and clinically significant findings were not reported. Since clinical significance was not reported, no inferences can be made on the practicality of dry needling in a clinical setting.
An important limitation is the lack of subject and author blinding. Two studies3,50 did not implement blinding of subjects. The lack of blinding can misconstrue the intervention outcomes because patients can perceive that the treatment is beneficial or not, given their symptoms. Furthermore, in all studies,3,14,47–50 the treating therapists were not blinded due to the nature of the interventions. The authors of the studies3,14,47–50 were not blinded to subject groups or interventions provided to the subjects.
All studies3,14,47–50 included in the systematic review consisted of varying follow-up periods ranging from 24 hours to six months (Table 2). No single study investigated the long-term effects of dry needling past six months. Furthermore, only one3 of the six studies included in this review investigated the short-term effect of dry needling combined with stretching. None of the studies examined the short- or long-term effects of dry needling in comparison to or conjunction with other physical therapy interventions. Therefore, recommendations can only be made on the short-term effects of dry needling as a sole method of treatment for the purposes of this review.
An additional limitation of this review is the potential of publication bias. In the study by Huguenin et al,14 one author was affiliated with the publisher at the time of publication. Publication bias may reduce the report of negative results or access of information not beneficial to the study outcomes and has the potential to negatively influence the ability to draw objective conclusions regarding patient care and resource allocation.52
In the studies by Mayoral et al49 and MacDonald et al50 there were non-standardized outcome measures that threatened external validity. The studies utilized clinical observers instead of validated outcome measures, which may have decreased interrater reliability. Clinical observers do not have the same reliability and reproducibility that a verified outcome measure contains, as subjective assessments may be prone to error. Additionally, due to the limited number of studies included in the systematic review, the authors did not have the ability to define inclusion criteria regarding specific outcome measures. While all six of the studies utilized a VAS to measure pain intensity, there was a general lack of consistency regarding other outcome measures. Although the reported outcome measures are subjective in nature, they have been proven to be valid and reliable (refer to Data Collection Process and Synthesis of Results section for provided values).
CONCLUSION
The purpose of this systematic review was to assess and provide a summary of the current literature for the use of dry needling for TrPs in the lower quarter. Muscular TrPs of active or latent origin are commonly associated with many musculoskeletal conditions of the lower quarter, as evidenced by this systematic review. The results of the studies included in this review suggest that dry needling is an effective intervention for reducing pain associated with lower quarter TrPs in the short-term. The findings suggest that dry needling does not have positive short or long-term effects on function, QoL, depression, ROM, or strength. There may be additional benefit in utilizing dry needling in combination with other therapeutic interventions (i.e., stretching and exercise) for the treatment of TrPs; however, further research is required to validate this assertion.
Future Research
This systematic review provides the potential foundation for future research and clinical application of dry needling due to the results of the studies. Further studies investigating the effect of dry needling in comparison to and in conjunction with other interventions would be beneficial to optimize outcomes in clinical settings. Standardized, valid outcome measures should be implemented and analyzed for both statistical and clinical significance in future studies in order to reveal the effectiveness of dry needling with respect to various orthopedic conditions. Furthermore, long-term follow-up measurements should be obtained in order to determine whether dry needling is able to produce lasting, positive effects on pain and disability associated with lower quarter TrPs.
REFERENCES
- 1.Dommerholt J Bron C Franssen J. Myofascial trigger points: an evidence-informed review. J Man Manip Ther. 2006;14:203-221. [Google Scholar]
- 2.Kalichman L Vulfsons S. Dry needling in the management of musculoskeletal pain. J Am Board Fam Med. 2010;23:640-646. [DOI] [PubMed] [Google Scholar]
- 3.Edwards J Knowles N. Superficial dry needling and active stretching in the treatment of myofascial pain--a randomised controlled trial. Acupunct Med. 2003;21:80-86. [DOI] [PubMed] [Google Scholar]
- 4.Gerber LH Sikdar S Armstrong K et al. A systematic comparison between subjects with no pain and pain associated with active myofascial trigger points. PM&R. 2013;5:931-938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dommerholt J. Dry needling - peripheral and central considerations. J Man Manip Ther. 2011;19:223-227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Celik D Mutlu EK. Clinical implication of latent myofascial trigger point. Curr Pain Headache Reports. 2013;17:353. [DOI] [PubMed] [Google Scholar]
- 7.Feinberg BI Feinberg RA. Persistent pain after total knee arthroplasty: treatment with manual therapy and trigger point injections. J Musculoskelet Pain. 1998;6:85-89. [Google Scholar]
- 8.Ingber RS. Iliopsoas myofascial dysfunction: a treatable cause of “failed” low back syndrome. Arch PMR. 1989;70:382-386. [PubMed] [Google Scholar]
- 9.Tay A Chua K Chan K-F. Upper quarter myofascial pain syndrome in Singapore: characteristics and treatment. J Musculoskelet Pain. 2000;8:49-56. [Google Scholar]
- 10.Chou LW Kao MJ Lin JG. Probable mechanisms of needling therapies for myofascial pain control. eCAM. 2012:705327:1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Simons DG. Diagnostic criteria of myofascial pain caused by trigger points. J of Musculoskelet Pain. 1999;7:111-120. [Google Scholar]
- 12.Cagnie B Dewitte V Barbe T et al. Physiologic effects of dry needling. Curr Pain Headache Reports. 2013;17:348. [DOI] [PubMed] [Google Scholar]
- 13.Bron C Dommerholt JD. Etiology of myofascial trigger points. Curr Pain Headache Reports. 2012;16:439-444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huguenin L Brukner PD Mccrory P et al. Effect of dry needling of gluteal muscles on straight leg raise: a randomised, #placebo |controlled, double blind trial. Brit J Sport Med. 2005;39:84-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Borg-Stein J Simons DG. Focused review: myofascial pain. Arch Phys Med Rehabil. 2002;83:S40-7, S48-9. [DOI] [PubMed] [Google Scholar]
- 16.Cummings TM White AR. Needling therapies in the management of myofascial trigger point: a systematic review. Arch Phys Med Rehabil. 2001;82:986-92. [DOI] [PubMed] [Google Scholar]
- 17.Dunning J Butts R Mourad F et al. Dry needling: a literature review with implications for clinical practice guidelines. Phys Ther Rev. 2014;19:252-265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.APTA Department of Practice and APTA State Government Affairs. Physical Therapists & The Importance of Dry Needling: An Educational Resource Paper. The American Physical Therapy Association. 2012. [Google Scholar]
- 19.Simons DF Travell J Simons LE Myofascial pain and dysfunction: the trigger point manual. 2nd ed. Balitmore, MD: Williams and Wilkins; 1999. [Google Scholar]
- 20.Giamberardino MA Affaitati G Fabrizio A et al. Effects of treatment of myofascial trigger points on the pain of fibromyalgia. Curr Pain Headache Rep. 2011;15(5):393-9. [DOI] [PubMed] [Google Scholar]
- 21.Baldry P. Acupuncture, trigger points and musculoskeletal pain. 3rd ed. Brookline, MA: Churchill Livingstone; 2005. [Google Scholar]
- 22.Kubo K Yajima H Takayama M et al. Effects of acupuncture and heating on blood volume and oxygen saturation of human Achilles tendon in vivo. Eur J Appl Physiol. 2010;109:545-550. [DOI] [PubMed] [Google Scholar]
- 23.Cagnie B Barbe T De Ridder E et al. The influence of dry needling of the trapezius muscle on muscle blood flow and oxygenation. J Manipulative Physiol Ther. 2012;35(9):685–91. [DOI] [PubMed] [Google Scholar]
- 24.Sandberg M Larsson B Lindberg LG et al. Different patterns of blood flow response in the trapezius muscle following needle stimulation (acupuncture) between healthy subjects and patients with fibromyalgia and work-related trapezius myalgia. Eur J Pain. 2005;9(5):497–510. [DOI] [PubMed] [Google Scholar]
- 25.Sandberg M Lundeberg T Lindberg LG et al. Effects of acupuncture on skin and muscle blood flow in healthy subjects. Eur J Appl Physiol. 2003;90(1–2):114–9. 39. [DOI] [PubMed] [Google Scholar]
- 26.Sandberg M Lindberg LG Gerdle B. Peripheral effects of needle stimulation (acupuncture) on skin and muscle blood flow in fibromyalgia. Eur J Pain. 2004;8(2):163–71. [DOI] [PubMed] [Google Scholar]
- 27.Kubo K Yajima H Takayama M et al. Changes in blood circulation of the contralateral achilles tendon during and after acupuncture and heating. Int J Sports Med. 2011;32(10):807–13. [DOI] [PubMed] [Google Scholar]
- 28.Ohkubo M Hamaoka T Niwayama M et al. Local increase in trapezius muscle oxygenation during and after acupuncture. Dyn Med. 2009;8:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Patel N. Physiology of pain. In: Patel N Kopf A, eds. Guide to pain management in low-resource settings. 2010. p. 13-18. [Google Scholar]
- 30.Hong CZ. Myofascial pain therapy. J of Musculoskelet Pain. 2004;12:37-43. [Google Scholar]
- 31.Kashiba H Ueda Y. Acupuncture to the skin induces release of substance P and calcitonin gene-related peptide from peripheral terminals of primary sensory neurons in the rat. Am J Clin Med. 1991;19:189–197. [DOI] [PubMed] [Google Scholar]
- 32.Lewit K. The needle effect in the relief of myofascial pain. Pain. 1979;6:83-90. [DOI] [PubMed] [Google Scholar]
- 33.Hong CZ. Lidocane injection versus dry needling to myofascial trigger point: the importance of the local twitch response. Am J Phys Med Rehab. 1994;73:256-263. [DOI] [PubMed] [Google Scholar]
- 34.Kietrys DM Palombaro KM Azzaretto E et al. Effectiveness of dry needling for upper-quarter myofascial pain: a systematic review and meta-analysis. J Orthop Sports Phys. 2013;43:620-634. [DOI] [PubMed] [Google Scholar]
- 35.Ilbuldu E Cakmak A Disci R Aydin R. Comparison of laser, #dry |needling, and placebo laser treatments in myofascial pain syndrome. Photomed Laser Surg. 2004;22:306-311. [DOI] [PubMed] [Google Scholar]
- 36.Itoh K Katsumi Y Hirota S et al. Randomised trial of trigger point acupuncture compared with other acupuncture for treatment of chronic neck pain. Complement Ther Med. 2007;15:172-179. [DOI] [PubMed] [Google Scholar]
- 37.Tekin L Akarsu S Durmus¸ O et al. The effect of dry needling in the treatment of myofascial pain syndrome: a randomized double-blinded placebo controlled trial. Clin Rheumatol. 2013;32:309-315. [DOI] [PubMed] [Google Scholar]
- 38.Whitehurst DG Bryan S Hay EM et al. Cost-effectiveness of acupuncture care as an adjunct to exercise-based physical therapy for osteoarthritis of the knee. Phys Ther. 2011;91:630–641. [DOI] [PubMed] [Google Scholar]
- 39.Maher C Sherrington C Herbert R et al. Reliability of the PEDro Scale for Rating Quality of Randomized Controlled Trials. Phys Ther. 2003;83:713-721. [PubMed] [Google Scholar]
- 40.Walser RF Meserve BB Boucher TR. The effectiveness of thoracic spine manipulation for the management of musculoskeletal conditions: a systematic review and meta-analysis of randomized clinical trials. J Man Manip Ther. 2009;17:237–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hawker GA Mian S Kendzerska T et al. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthrit Care Res (Hoboken). 2011;63 Suppl 11:S240-52. [DOI] [PubMed] [Google Scholar]
- 42.Bijur PE Silver W Gallagher EJ. Reliability of the Visual Analog Scale for Measurement of Acute Pain. Acad Emerg Med. 2001;8:1153–1157. [DOI] [PubMed] [Google Scholar]
- 43.Stratford PW Kennedy DM Woodhouse LJ et al. Measurement properties of the WOMAC LK 3.1 pain scale. Osteoarthr Cartilage. 2007;15:266-272. [DOI] [PubMed] [Google Scholar]
- 44.Greco N Anderson A Mann B et al. Responsiveness of the International Knee Documentation Committee Subjective Knee Form in comparison to the Western Ontario and McMaster Universities Osteoarthritis Index, modified Cincinnati Knee Rating System, and Short Form 36 in patients with focal articular cartilage defects. Am J Sport Med. 2010;38:891-902. [DOI] [PubMed] [Google Scholar]
- 45.Riskowski JL Hagedorn TJ Hannan MT. Measures of foot function, #foot |health, and foot pain: American Academy of Orthopedic Surgeons Lower Limb Outcomes Assessment: Foot and Ankle Module (AAOS-FAM), Bristol Foot Score (BFS), Revised Foot Function Index (FFI-R), Foot Health Status Questionnaire (FHSQ), Manchester Foot Pain and Disability Index (MFPDI), Podiatric Health Questionnaire (PHQ), and Rowan Foot Pain Assessment (ROFPAQ). Arthrit Care Res (Hoboken). 2011;63 Suppl 11:S229-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Toomey M. In: Zuluaga M Briggs C Carlisle J et al. Sports physiotherapy: applied science and practice. Melbourne: Churchill Livingstone, 1998. [Google Scholar]
- 47.Cotchett MP Munteanu SE Landorf KB. Effectiveness of trigger point dry needling for plantar heel pain: a randomized controlled trial. Phys Ther. 2014;94:1083-1094. [DOI] [PubMed] [Google Scholar]
- 48.Itoh K Katsumi Y Kitakoji H. Trigger point acupuncture treatment of chronic low back pain in elderly patients – a blinded RCT. Acupunct Med. 2004;22:170-177. [DOI] [PubMed] [Google Scholar]
- 49.Mayoral O Salvat I Martín MT et al. Efficacy of myofascial trigger point dry needling in the prevention of pain after total knee arthroplasty: a randomized, double-blinded, placebo-controlled trial. Evid Based Complement Alternat Med. 2013;2013:1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Macdonald AJ Macrae KD Master BR et al. Superficial acupuncture in the relief of chronic low back pain. Ann Roy Coll Surg. 1983;65:44-46. [PMC free article] [PubMed] [Google Scholar]
- 51.Jensen MP Chen C Brugger AM. Interpretation of visual analog scale ratings and change scores: a reanalysis of two clinical trials of post-operative pain. J Pain. 2003;4:407-14. [DOI] [PubMed] [Google Scholar]
- 52.Thaler K Kien C Nussbaumer B et al. Inadequate use and regulation of interventions against publication bias decreases their effectiveness: a systematic review. J Clin Epidemiol. 2015;68:792-802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Landorf KB Radford JA Hudson S. Minimal Important Difference (MID) of two commonly used outcome measures for foot problems. J Foot Ankle Res. 2010;3:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Brander VA Stulberg SD Adams AD et al. Predicting total knee replacement pain: a prospective, observational study. Clin Orthop Relat R. 2003;416:27-36. [DOI] [PubMed] [Google Scholar]
- 55.Ceccherelli F Bordin M Gagliardi G et al. Comparison between superficial and deep acupuncture in the treatment of the shoulder's myofascial pain: a randomized and controlled study. Acupunct Electrother Res. 2001;26:229-38. [DOI] [PubMed] [Google Scholar]
- 56.Ceccherelli F Rigoni MT Gagliardi G Ruzzante L. Comparison of superficial and deep acupuncture in the treatment of lumbar myofascial pain: a double-blind randomized controlled study. Clin J Pain. 2002;18:149-153. [DOI] [PubMed] [Google Scholar]
- 57.Itoh K Minakawa Y Kitakoji H. Effect of acupuncture depth on muscle pain. Chin Med. 2011;6:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Phillips B Ball C Sackett D et al. Oxford Centre for Evidence-based Medicine – Levels of Evidence (March 2009). Available at: http://www.cebm.net/index.aspx?o=1025. Accessed April 22, 2015.
- 59.Lee S Hobden E Stiell I Wells G. Clinically important change in the Visual Analog Scale and adequate pain control. Acad Emerg Med. 2003;10:1128-1130. [DOI] [PubMed] [Google Scholar]