Abstract
Background
Emerging evidence suggests poor core stability is a risk factor for low back and lower extremity injuries in athletes. Recently the trunk stability test (TST) and unilateral hip bridge endurance test (UHBE) were developed to clinically assess core stability. Although these and other clinical tests of core stability exist, how well they assess core stability when compared to biomechanical measures of isolated core stability has not been thoroughly evaluated.
Purpose/Hypothesis
The purposes of this study were to 1) determine concurrent validity of two novel clinical core stability assessments (TST and UHBE), and 2) assess relationships between these assessments and the trunk endurance and Y-Balance tests. The authors’ hypothesized that the TST and UHBE would be highly correlated to the lab-based biomechanical measure of isolated core stability. Also, the TST and UHBE would be moderately correlated with each other, but not with the trunk extensor endurance and Y-Balance.
Study Design
Cross-Sectional design
Methods
Twenty healthy active individuals completed the TST (recorded number of errors), UHBE (s), trunk extensor endurance (s), Y-Balance (% leg length) test (YBT), and biomechanical test of core stability.
Results
Correlational analyses revealed a small, non-significant association between TST and biomechanical measures (rs = 0.2 – 0.22), while a moderate, significant relationship existed between UHBE and biomechanical measures (rs = −0.49 to −0.56, p < 0.05). There was little to no relationship between TST and UHBE (r = −0.07 to – 0.21), or TST and extensor endurance (r = −0.18 to −0.24). A moderate, significant association existed between TST and two reach directions of the YBT (r = −0.41 to −0.43, p < 0.05).
Conclusions
Study data support the utility of UHBE as a clinical measure of core stability. The poor relationship between the TST and biomechanical measures, combined with observation of most control faults occurring in the lower extremity (LE) suggest the TST may not be an appropriate clinical test of core stability.
Levels of Evidence
Level 3
Keywords: athletic injuries, neuromuscular control, core stability
INTRODUCTION
Many sporting activities require complex coordination between the upper and lower extremities. The core (trunk, pelvis, and hip) functions as the central link between the upper and lower extremities, and stability of this region is proposed to be a requisite for optimal athletic performance and injury prevention.1 The kinetic chain theory describes core stability as the ability to control the position and motion of the trunk and pelvis relative to the extremities in order to allow for optimal force production, dissipation, and transfer to the extremities during movement.1
Optimal core stability is dependent upon both muscle capacity (strength and endurance) and neuromuscular control. Neuromuscular control is defined as the ability to accurately orchestrate a synchronized muscular response to internal and external perturbations based on sensory information in order to control the position or movement of the body.2,3 While the anatomical definition of the core is not universally agreed upon, most definitions include musculature associated with the trunk, pelvis and hips. These muscles are activated prior to extremity movement, which indicates that the core provides proximal stability upon which movement of the extremities occurs.4 Additionally, optimal core stability is important for performance of athletic tasks that result in perturbations of the athletes body outside of their base of support.5
Poor core stability has been identified as a risk factor for low back and extremity injuries in athletes.6–9 In light of this information, core stability training has gained popularity in clinical settings for prevention and rehabilitation of upper and lower extremity injuries in athletes.10 Therefore, there is a need for valid assessments of core stability that can readily be applied in a clinical setting.
Clinical assessments of muscle endurance are commonly used to evaluate core stability. Numerous tests of core muscle endurance (prone plank, side plank, abdominal curl, trunk extension) have been described for assessing core stability in healthy adults and athletic populations.11–13 Decreased trunk/pelvis/hip extensor muscle endurance has been shown to be predictive of future low back pain (odds ratio: 3.4, 95% CI, 1.2-10) in a non-athletic population.14
While poor neuromuscular control of the core has been reported as a risk factor for lower extremity and low back injury, there is a paucity of clinical tests that assess this aspect of core stability.6,8 Hip bridging is commonly used as a lumbar stabilization exercise and is believed to challenge multi-planar lumbopelvic control when performed unilaterally. In light of the fact that a unilateral hip bridge requires significant activation of the lumbar multifidus and erector spinae muscles, key stabilizing muscles of the region, a unilateral hip bridge test (UHBE) (Figure 1) may be appropriate to use as a means of assessing muscle capacity and neuromuscular control aspects of core stability.15,16
Figure 1.
Unilateral Hip Bridge Endurance Test. Test requires an individual to maintain a neutral pelvis in both the transverse and sagittal planes for as long as possible with one leg planted and one leg extended.
Noehren et al17 recently described a new clinical test of core stability; the trunk stability test (TST), which they suggest tests core neuromuscular control (Figure 2a). The trunk stability test was designed as a clinical version of a valid and reliable lab-based test of core neuromuscular control.17–20 Findings from their study revealed poorer TST performance in a group of subjects undergoing ACL rehabilitation.17 The authors suggest that this finding indicated impairments of core neuromuscular control.17
Figure 2.
A. Trunk Stability Test (TST). B. Lab-based biomechanical test of isolated core stability. The lab-based test reduces influence of the lower extremities by strapping the legs together and supporting the feet on the footplate that is attached to the chair thereby eliminating control of the chair through the lower extremities. The TST requires the same trunk and arm position as the lab-based test; however, one foot is allowed to remain in contact with the floor.
The Y-Balance Test (YBT) is another clinical test used to assess lower extremity and trunk neuromuscular control during a dynamic single-limb balancing task.21,22 Recent studies have demonstrated usefulness of the YBT for predicting lower and upper extremity injuries in high school and collegiate athletes.23,24,25
Poor core stability is recognized as a risk factor for musculoskeletal injury; however, most clinical measures of core stability have not been validated against lab-based biomechanical measures of core stability. This has resulted in knowledge gaps that hinder a clinician's ability to accurately assess core stability. The purposes of this study were to 1) determine the concurrent validity of two novel clinical assessments of core stability (TST and UHBE test), and 2) assess the relationships between these novel assessments and currently used clinical core stability measures of trunk endurance test and YBT. The authors hypothesized that the TST and UHBE test would demonstrate a moderate to strong correlation with lab-based biomechanical measures of isolated core neuromuscular control. The authors further hypothesized that TST and UHBE test would be moderately correlated with each other, but not with the trunk extensor endurance test and YBT.
METHODS
Study Design
A cross-sectional design was used to assess the relationship between two novel clinical measures of core stability (UHBE test and TST) and a lab-based biomechanical test of isolated core stability, as well as the relationship between two novel clinical measures and two commonly used clinical measures of core stability. The TST was chosen as it was modeled after the lab-based biomechanical test used in the current study and has not been validated against this measure.17,19 Commonly used clinical measures of core stability were chosen based on current evidence and published procedures were used. Standardized procedures were developed for the novel clinical assessments.
Subjects
Twenty healthy active subjects were recruited to participate in the study (11 males; age 23.5+/−1.7 years; height 173.0+/−8.3 cm; weight 71.9+/−15.5 kg). All subjects participated in physical activities 4-6 days per week. These activities included strength training, cardiovascular exercise, and club sports. Prior to the start of any testing procedures, all participants signed informed consent documents approved by the Institutional Review Board. Inclusion criteria were anyone between the ages of 18-40 and considered to be regularly active. Subjects were excluded if they presented with any of the following: concussion (current or within the previous six months), current leg, trunk or neck injury, a diagnosed balance disorder, and/or a current head cold, sinus infection, or inner ear infection.
Procedures
Following completion of the intake forms, subjects performed a series of clinical and lab-based measures with standardized rest periods between tests (5 minutes) and trials (1 minute). The trunk extensor endurance test (Figure 3) was performed first as two trials of this test were conducted and it was necessary to separate them within the protocol. The second trial was completed at the end of the testing session. To perform the trunk extensor endurance test, subjects were positioned prone on a treatment table with the iliac crests at the edge of the table and their upper trunk hanging down from the edge of the table. Mobilization belts were used to secure the subject to the table at the buttocks, thigh, and lower leg. Subjects were instructed to place their arms across their chest and raise their torso until it was parallel to the floor. An examiner then placed a digital inclinometer on the subjects back between their shoulder blades, the subject was told to hold this position for as long as possible, and the amount of time the position could be maintained was recorded via a stopwatch. The test was terminated when the trunk angle changed 10 ° from the start position or the subject stopped on their own volition. Two trials were performed and the average was used in subsequent analyses.
Figure 3.
Trunk Extensor Endurance Test. The trunk extensor endurance test requires an individual to maintain neutral trunk and pelvic alignment in the sagittal plane for as long as possible.
Subjects then performed the TST and lab-based measures of core neuromuscular control. The order of testing for these two assessments was randomly determined. The trunk stability test required subjects to sit on either a 65cm or 75cm Swiss ball with both feet on the ground. Ball size was, in part, determined by the height of the subject. For all subjects it was essential that the size of the ball allowed both ankles to be in a neutral position (0 ° dorsiflexion) with the knees and hips in 90 + /- 10 degrees of flexion. Subjects were asked to sit up tall with their arms across their chest and extend one knee so that the heel of the lifted leg was at the height of the stationary ankle. Subjects performed one 30s practice trial on each leg with their eyes open while attempting to maintain the position of the raised foot for the duration of the trial. Following the practice trial, three trials per leg were collected where the individual repeated the same testing procedures except with their eyes closed. If they moved out of the test position, they were instructed to return to the test position as quickly as possible. Throughout the 30-second trial an examiner visually assessed and recorded deviations from the test position (errors).17 Errors included: plant foot moving, uncrossing the arms, raised foot touches ground, eyes open, and reaching for the table. Additionally the amount of time that an individual error existed was recorded. Subjects were allowed to open their eyes; however, this would be recorded as an error. The time from when they opened their eyes until they returned to the test position was counted and each second from the initial error to the return to position was recorded as an error. For example, if the subject placed the foot on the ground and opened their eyes, two errors were recorded. The number of seconds from the last error (i.e. eyes open) to the return to the testing position was counted (i.e. 3 seconds) and that 3-second period was counted as three errors. The total errors for each trial were recorded and the average of the three trials was used for analysis. The TST has a reported measurement error of 0.25 errors and within-session reliability [ICC (3,k)] of 0.93.17
Lab-based biomechanical measures of isolated core neuromuscular control were obtained from an unstable sitting test (Figure 2b).19,20,26 This apparatus and test isolates neuromuscular control to the core by minimizing involvement of the lower extremities through use of straps and a footplate that is attached directly to the chair. The seat is attached to a solid hemisphere (44 cm diameter), which sits atop a force plate. Padded safety railings surrounded the subject in the event that they lost their balance. Details of the apparatus design and protocol have been previously reported.18 Center of pressure (CoP) measures derived from the force plate data collected during the unstable sitting test were used to quantify core neuromuscular control by use of a 95% confidence ellipse (CEA) that represents 95% of the area that CoP traveled during the test, and mean velocity (MVEL) which represents the mean displacement of the CoP per second. Subjects performed three-60s trials in which they were instructed to close their eyes, sit up tall with their arms across their chest, and move as little as possible during the trial. The average of three trials was used for analysis. A larger CEA and higher MVEL are representative of poor control of the body's center of mass, or poor core stability. These variables have been previously validated and used to identify poor core neuromuscular control in patients with low back pain.18,20,26
The UHBE test was performed with the subject lying supine with their arms across their chest, knees in flexion, and feet flat on the table. The subject performed a double-leg hip bridge, and once a neutral spine and pelvis position were achieved the subject was instructed to extend one knee (randomly determined) so their leg was straight and their thighs were parallel to one another. Subjects were instructed to hold this position as long as possible. The test was terminated when they were no longer able to maintain a neutral pelvic position as noted by 10-degree change in transverse or sagittal plane alignment. Pelvic positioning in the transverse plane was monitored by a digital inclinometer attached to a mobilization belt that was tightly secured to the individual's pelvis. A second rater visually assessed sagittal plane alignment. Two trials were performed on each side and the average of each side was used for subsequent analyses.
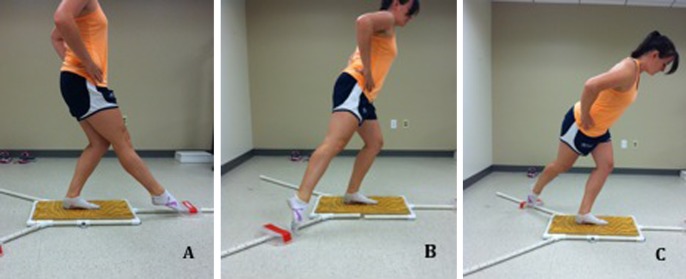
The YBT (Figure 4) was performed as described by Pilsky et al, 2009.27 Subjects were given six practice trials on each leg in each direction prior to performing three recorded trials. Hands had to remain on hips and foot in full contact with the support surface to be considered a good trial. Trials were averaged for each direction, normalized to the subject's leg length, and expressed as a percentage of leg length.
Figure 4.
Y-Balance Test (YBT). A) Anterior Reach (YBT ANT); B) Posteromedial Reach (YBT PM); C) Posterolateral Reach (YBT PL). YBT tests require balance and control in dynamic single-limb stance while reaching as far as possible in three directions.
Statistical Analysis
All data were tested for normal distribution via the Shapiro-Wilk test. Paired t-Tests were used to assess for side differences with the UHBE, TST, and YBT. One-tailed Pearson's and Spearman's rho correlations were used to examine relationships between the trunk stability and UHBE tests and lab-based biomechanical measures, and the TST, UBHE, YBT and trunk extensor endurance test clinical measures. Significance was set at p ≤ 0.05. All data analyses were conducted using Statistical Package for the Social Sciences (SPSS v22, Chicago, IL). Correlations were interpreted according to Cohen [0.1 = weak; 0.3 = moderate; 0.5 = strong].28
RESULTS
Descriptive statistics for clinical and lab-based biomechanical measures are reported in Table 1. All data, except mean CoP velocity and 95% confidence ellipse area, were normally distributed. There were no significant differences in side-to-side performance of the UHBE test or any YBT direction, thus the values were averaged to produce one score for the UHBE test and one score for each direction of the YBT. There was a significant difference in performance between sides of the TST; therefore sides were analyzed separately. The UHBE test demonstrated a significant, moderate to strong negative correlation with lab-based biomechanical measures of isolated core stability (Table 2). There was little to no correlation between TST and lab-based biomechanical measures of core stability (Table 2). The TST was significantly and moderately correlated to the YBT, but not UHBE and trunk extensor endurance test (Table 3). There was a small and non-significant correlation between UHBE and trunk extensor endurance test and YBT (Table 3). A breakdown of the location of errors by body region for the TST is located in Table 4.
Table 1.
Performance statistics for the biomechanical and clinical tests
| Variable | Mean ± SD | Range (Min-Max) |
|---|---|---|
| EC_CEA (mm2) | 344.6 ± 276.5 | 94.2 - 1063.9 |
| EC_MVEL (mm/s) | 10.4 ±5.1 | 4.6 - 23.8 |
| L_TST (errors) | 5.1 ± 4.0 | 0.0 - 14.0 |
| R_TST (errors) | 6.5 ±3.9 | 0.3 - 16.3 |
| UHBE (s) | 23.0 ±16.5 | 3.1 - 59.5 |
| TEE (s) | 78.6 ± 24.2 | 43.3 - 120.7 |
| YBT_ANT (%LL) | 81.7 ±6.3 | 68.5 - 95.7 |
| YBT_PM (%LL) | 96.1 ±8.2 | 74.2 - 114.3 |
| YBT_PL (%LL) | 90.3 ± 7.7 | 76.3 - 106.7 |
Table 2.
Relationship between the novel clinical tests and biomechanical measure of core stability.
| EC CEA | EC MVEL | |
|---|---|---|
| L TST | 0.02 (0.46) | −0.14 (0.27) |
| R TST | 0.22 (0.18) | 0.06 (0.41) |
| UHBE* | −0.49 (0.01) | −0.56 (0.01) |
1 Data represents Spearman's rho value (p value).
Abbreviations: EC_CEA: Eyes Closed 95% Confidence Ellipse Area of the CoP; EC_MVEL: Eyes Closed Mean Velocity of CoP; L_TST: Left Foot planted Trunk Stability Test; R_TST; Right Foot planted Trunk Stability Test; UHBE: Unilateral Hip Bridge Endurance.
Bold italics p ≤ 0.05
represents combined sides
Table 3.
Relationship between different clinical measures of core stability
| TEE | YBT ANT* | YBT PM* | YBT PL* | |
|---|---|---|---|---|
| L_TST | −0.18 (0.22) | −0.09 (0.36) | −0.41(0.04) | −0.42 (0.03) |
| R_TST | −0.24 (0.16) | −0.08 (0.37) | −0.35 (0.06) | −0.43(0.03) |
| UHBE* | 0.27 (0.12) | 0.05 (0.42) | −0.08 (0.37) | −0.27 (0.12) |
1 Data represents Pearson's r value (p value).
Abbreviations: L_TST: Left Foot planted Trunk Stability Test; R_TST: Right Foot planted Trunk Stability Test; UHBE: Unilateral Hip Bridge Endurance; TEE: Trunk Extensor Endurance; YBT_ANT: Y-Balance Test Anterior Reach; YBT_PM: Y-Balance Test Posteromedial Reach; YBT_PL: Y-Balance Test Posterolateral Reach
represents combined sides
Bold italics: p ≤ 0.05
Table 4.
Breakdown of location of errors recorded for the trunk stability test
| Upper Extremity/Trunk | Eyes Opening | Lower Extremity | Total | |
|---|---|---|---|---|
| TST Errors* | 65 | 20 | 473 | 558 |
| Percent Total (%) | 11.7 | 3.6 | 84.8 | 100 |
1Data represent recorded errors for all subjects across all trials. Upper extremity/trunk errors included any instance the arms came uncrossed, the subject reached for the wall/table, or the trunk/shoulder touched the wall/table. Lower extremity errors included any instance the plant foot moved, the lifted leg touched the ground, or the lifted leg/foot touched the plant foot. The average number of errors per person (sides combined) was 5.8 ± 3.7.
Abbreviations: TST: trunk stability test.
Represents combined sides
DISCUSSION
The primary purpose of this study was to determine the concurrent validity of two novel clinical assessments (TST and UHBE test) of core stability. The UHBE test was significantly correlated with lab-based biomechanical measures of core stability, thereby partially supporting our hypothesis. Data revealed that the UHBE test explains 24-31% of the variance in the lab-based biomechanical measures of isolated core stability. Since the lab-based biomechanical measures of core stability and UHBE test require control of the lumbopelvic region to maintain stability in the testing position, the moderate relationship between these tests support the use of the UHBE test as a clinical measure of core stability. There was no significant association between the TST and the lab-based biomechanical measures. This finding is contrary to our hypothesis and suggests that the TST does not primarily measure isolated core stability, despite the fact that it was modeled as a clinical version of a lab-based seated core stability test.17,19
The TST demonstrated a significant relationship with the YBT and explained up to 19% of the YBT variance. In addition, 85% of the errors recorded during the TST were related to lower extremity deviations while 11% were related to the trunk or upper extremity deviations (Table 4). Previous work has demonstrated that performance on the YBT appears to be primarily driven by lower extremity control.22 The lack of a relationship between the TST and isolated core stability lab-based tests, combined with the predominance of lower extremity errors on the trunk stability test suggests that the TST may not be a good assessment of core stability performance.
Interestingly, the TST was significantly correlated to posteromedial and posterolateral directions of the YBT but not the anterior direction. The significant and moderate relationship between the posteromedial and posterolateral directions of the YBT and the TST may be due to the increased demand for ankle stability and control during tasks that incorporate trunk and hip motion (such as the trunk counterbalancing in the YBT or sitting on a Swiss ball).23,29–31 It is also plausible that optimal lower extremity neuromuscular control strategies are essential for correct performance of the TST, and only when this fails does compensation need to occur further up the kinetic chain at the pelvis/trunk. Further research is needed to evaluate the mechanics of how the test is performed, such as muscle activation and timing patterns and/or kinematics.
Relationships between the TST, UHBE, trunk extensor endurance and YBT provide further insight into these clinical assessments of core stability and dynamic single-limb balance. The TST and UHBE tests were not significantly related to each other, suggesting that they assess different regions of the kinetic chain. The TST may assess lower extremity control while the UHBE test primarily assesses lumbopelvic control. The small, non-significant relationships between the UHBE and trunk extensor endurance tests suggest these tests are measuring different aspects of core stability (neuromuscular control vs. muscle capacity). The lack of a relationship between the trunk extensor endurance and UHBE tests might be explained if it is considered that the UHBE test may primarily address multi-planar lumbopelvic neuromuscular control and localized muscle capacity, while the trunk extensor endurance test primarily assesses global extensor muscle endurance. A follow-up analysis of the relationship between the trunk extensor endurance test and lab-based tests found a moderate and significant correlation (EC_CEA = -.45, p < .05; EC_MVEL = . 47, p, .05). Interestingly, the trunk extensor endurance test, accounts for 20-22% of the variance in the lab-based measure of core stability. This relationship suggests that the lab-based biomechanical test requires both multi-planar neuromuscular control for stability and extensor muscular endurance. The extensor muscle endurance aspect of the test could be based on the position required (upright sitting) and repeated 60s trials; however, this finding requires further investigation. Together, these findings provide preliminary support for the use of the UHBE and trunk extensor endurance tests as complimentary clinical measures, potentially capturing both neuromuscular control and muscle capacity aspects of core stability. However, further work is needed to support this idea as well as to determine if additional tests can further compliment the assessment of core stability. In addition, more research is necessary on the UHBE to determine normative values and minimal detectable change scores, which will make the test clinically useful.
Acknowledged limitations in this study may restrict the generalizability of the findings. This study utilized a small sample, which may have been underpowered to find a moderate correlation. No previous injury history information was available on this cohort of young healthy individuals. While injury history is a reported risk factor for future injuries, the influence of prior injury (particularly in the lower extremity) on task performance is not available in this study. Therefore it cannot be said with full confidence that these relationships do not shift in light of injury history or that this test is predictive of injury. This subject group, while recreationally active, does not represent a sample of competitive athletes, and therefore the performance of these tests in competitive athletes should be assessed. In addition, it should be noted that the lab-based biomechanical test emphasizes isolated trunk/pelvic control with emphasis on neuromuscular control of an upright-seated posture and thus the current findings do not represent all aspects of core stability. Future work seeking to assess validity of clinical tests of core stability should consider these limitations.
CONCLUSIONS
These findings preliminarily support use of the UHBE test as clinical measure of core stability. Future work is needed to determine both the psychometric properties and clinical utility of the UHBE test to identify poor core stability and predict injury. While the trunk stability test was not correlated with the lab-based measures of core stability it demonstrated a significant association with the Y-Balance test. Though future work is needed to fully understand this relationship, these data do not support use of the TST as a clinical tool to assess core neuromuscular control. Identification of other clinical assessments of core stability that are helpful in clinical decision-making remains a research priority.
References
- 1.Kibler WB Press J Sciascia A. The role of core stability in athletic function. Sports Med. 2006;36(3):189-198. [DOI] [PubMed] [Google Scholar]
- 2.Silfies SP Ebaugh D Pontillo M et al. Critical Review of the Impact of “Core Stability” on Upper Extremity Athletic Injury and Performance. Braz J Phys Ther. 2015;In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zazulak B Cholewicki J Reeves NP. Neuromuscular control of trunk stability: clinical implications for sports injury prevention. J Am Acad Orthop Surg. 2008;16(9):497-505. [PubMed] [Google Scholar]
- 4.Hodges PW Richardson CA. Contraction of the abdominal muscles associated with movement of the lower limb. Phys Ther. 1997;77(2):132-142; discussion 142-134. [DOI] [PubMed] [Google Scholar]
- 5.Gribble AD Hertel J. Considerations for normalizing measures of the Star Excursion Balance Test. Meas Phys Educ Exerc Sci. 2003;7(2):89-100. [Google Scholar]
- 6.Cholewicki J Silfies SP Shah RA et al. Delayed trunk muscle reflex responses increase the risk of low back injuries. Spine. 2005;30(23):2614-2620. [DOI] [PubMed] [Google Scholar]
- 7.Ireland ML Willson JD Ballantyne BT et al. Hip strength in females with and without patellofemoral pain. J Orthop Sports Phys Ther. 2003;33(11):671-676. [DOI] [PubMed] [Google Scholar]
- 8.Zazulak BT Hewett TE Reeves NP et al. Deficits in neuromuscular control of the trunk predict knee injury risk: a prospective biomechanical-epidemiologic study. Am J Sports Med. 2007;35(7):1123-1130. [DOI] [PubMed] [Google Scholar]
- 9.Zazulak BT Hewett TE Reeves NP et al. The effects of core proprioception on knee injury: a prospective biomechanical-epidemiological study. Am J Sports Med. 2007;35(3):368-373. [DOI] [PubMed] [Google Scholar]
- 10.Willardson JM. Core stability training: applications to sports conditioning programs. J Strength Cond Res. 2007;21(3):979-985. [DOI] [PubMed] [Google Scholar]
- 11.Leetun DT Ireland ML Willson JD et al. Core stability measures as risk factors for lower extremity injury in athletes. Med Sci Sports Exerc. 2004;36(6):926-934. [DOI] [PubMed] [Google Scholar]
- 12.McGill SM Childs A Liebenson C. Endurance times for low back stabilization exercises: clinical targets for testing and training from a normal database. Arch Phys Med Rehabil. 1999;80(8):941-944. [DOI] [PubMed] [Google Scholar]
- 13.Okada T Huxel KC Nesser TW. Relationship between core stability, functional movement, and performance. J Strength Cond Res. 2011;25(1):252-261. [DOI] [PubMed] [Google Scholar]
- 14.Alaranta H Luoto S Heliovaara M et al. Static back endurance and the risk of low-back pain. Clin Biomech. 1995;10(6):323-324. [DOI] [PubMed] [Google Scholar]
- 15.Miller MM Grooms D Schussler E et al. Single Leg Glute Bridge: A Clinical Test for Gluteal Muscle Endurance. Med Sci Sports Exerc. 2013;45(5):430-430. [Google Scholar]
- 16.Okubo Y Kaneoka K Imai A et al. Electromyographic analysis of transversus abdominis and lumbar multifidus using wire electrodes during lumbar stabilization exercises. J Orthop Sports Phys Ther. 2010;40(11):743-750. [DOI] [PubMed] [Google Scholar]
- 17.Noehren B Abraham A Curry M et al. Evaluation of proximal joint kinematics and muscle strength following ACL reconstruction surgery in female athletes. J Orthop Res. 2014;32(10):1305-1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sung W Abraham M Plastaras C et al. Trunk motor control deficits in acute and subacute low back pain are not associated with pain or fear of movement. Spine. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cholewicki J Polzhofer GK Radebold A. Postural control of trunk during unstable sitting. J Biomech. 2000;33(12):1733-1737. [DOI] [PubMed] [Google Scholar]
- 20.Radebold A Cholewicki J Polzhofer GK et al. Impaired postural control of the lumbar spine is associated with delayed muscle response times in patients with chronic idiopathic low back pain. Spine. 2001;26(7):724-730. [DOI] [PubMed] [Google Scholar]
- 21.de la Motte S Arnold BL Ross SE. Trunk-rotation differences at maximal reach of the star excursion balance test in participants with chronic ankle instability. J Athl Train. 2015;50(4):358-365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fullam K Caulfield B Coughlan GF et al. Kinematic analysis of selected reach directions of the Star Excursion Balance Test compared with the Y-Balance Test. J Sport Rehabil. 2014;23(1):27-35. [DOI] [PubMed] [Google Scholar]
- 23.Plisky PJ Rauh MJ Kaminski TW et al. Star Excursion Balance Test as a predictor of lower extremity injury in high school basketball players. J Orthop Sports Phys Ther. 2006;36(12):911-919. [DOI] [PubMed] [Google Scholar]
- 24.Smith CA Chimera NJ Warren M. Association of y balance test reach asymmetry and injury in division I athletes. Med Sci Sports Exerc. 2015;47(1):136-141. [DOI] [PubMed] [Google Scholar]
- 25.Garrison JC Arnold A Macko MJ et al. Baseball players diagnosed with ulnar collateral ligament tears demonstrate decreased balance compared to healthy controls. J Orthop Sports Phys Ther. 2013;43(10):752-758. [DOI] [PubMed] [Google Scholar]
- 26.Silfies SP Cholewicki J Radebold A. The effects of visual input on postural control of the lumbar spine in unstable sitting. Hum Movement Sci. 2003;22(3):237-252. [DOI] [PubMed] [Google Scholar]
- 27.Plisky PJ Gorman PP Butler RJ et al. The reliability of an instrumented device for measuring components of the star excursion balance test. N Am J Sports Phys Ther. 2009;4(2):92-99. [PMC free article] [PubMed] [Google Scholar]
- 28.Cohen J. Statistical Power Analysis for the Behavioral Sciences. New Jersey: Lawrence Erlbaum Associates, Inc.; 1988. [Google Scholar]
- 29.Smith CA Chimera NJ Wright NJ et al. Interrater and intrarater reliability of the functional movement screen. J Strength Cond Res. 2013;27(4):982-987. [DOI] [PubMed] [Google Scholar]
- 30.Hale SA Hertel J Olmsted-Kramer LC. The effect of a 4-week comprehensive rehabilitation program on postural control and lower extremity function in individuals with chronic ankle instability. J Orthop Sports Phys Ther. 2007;37(6):303-311. [DOI] [PubMed] [Google Scholar]
- 31.Hertel J Braham RA Hale SA et al. Simplifying the star excursion balance test: analyses of subjects with and without chronic ankle instability. J Orthop Sports Phys Ther. 2006;36(3):131-137. [DOI] [PubMed] [Google Scholar]