Abstract
Background
Significant incidence, diagnostic difficulties, clinical relevance and therapeutic efficacy associated with the small number of publications on the primary esophageal motor disorders, motivated the present study.
Aim
To determine the manometric prevalence of these disorders and correlate them to the endoscopic and clinical findings.
Methods
A retrospective study of 2614 patients, being 1529 (58.49%) women and 1085 (41.51%) men. From 299 manometric examinations diagnosed with primary esophageal motor disorder, were sought-clinical data (heartburn, regurgitation, dysphagia, odynophagia, non-cardiac chest pain, pharyngeal globe and extra-esophageal symptoms) and/or endoscopic (hiatal hernia, erosive esophagitis, food waste) that motivated the performance of manometry.
Results
Were found 49 cases of achalasia, 73 diffuse spasm, 89 nutcracker esophagus, 82 ineffective esophageal motility, and six lower esophageal sphincter hypertension. In relation to the correlations, it was observed that in 119 patients clinical conditions were associated with dysphagia, found in achalasia more than in other conditions; in relationship between endoscopic findings and clinical conditions there was no statistical significance between data.
Conclusions
The clinical and endoscopic findings have little value in the characterization of the primary motor disorders of the esophagus, showing even more the need for manometry, particularly in the preoperative period of gastroesophageal reflux disease.
Keywords: Esophageal motility disorders, Endoscopy, Manometry
Abstract
Racional
A incidência significante, a dificuldade diagnóstica, a relevância clínica e a eficácia terapêutica associada ao pequeno número de publicações sobre os distúrbios motores primários do esôfago, motivou a realização do presente estudo.
Objetivo
Verificar a prevalência desses distúrbios em manometrias e relacioná-las aos achados endoscópicos e clínicos.
Métodos
Estudo retrospectivo de 2614 pacientes sendo 1529 (58,49%) do gênero feminino e 1085 (41,51%) do masculino. A partir de 299 exames manométricos com diagnóstico de distúrbio motor esofagiano primário, procuraram-se os dados clínicos (pirose, regurgitação, disfagia, odinofagia, dor torácica não cardíaca, globo faríngeo e sintomas extra-esofageanos) e/ou endoscópicos (hérnia de hiato, esofagite erosiva, resíduos alimentares) que motivaram a realização da manometria.
Resultados
Foram encontrados 49 casos de acalásia, 73 de espasmo difuso, 89 de esôfago em quebra-nozes, 82 de motilidade esofagiana ineficaz, e seis de esfíncter esofagiano inferior hipertensivo. Em relação às correlações, observou-se em 119 pacientes analisados que, na clínica associada às afecções, a disfagia foi mais encontrada na acalásia do que nas outras afecções; na relação entre os achados endoscópicos e as afecções não houve relevância estatística entre os dados.
Conclusões
Os achados clínicos e endoscópicos têm pequeno valor na caracterização das doenças motoras primárias do esôfago, evidenciando ainda mais a necessidade da manometria, particularmente no pré-operatório da doença do refluxo gastroesofágico.
INTRODUCTION
The esophageal motility disorders include any condition whose symptoms are mainly dysphagia and chest pain and, thus, suspected of esophageal origin19. They may be as uncomfortable feeling of "ball" in the throat (pharyngeal globe), or it can be more noticeable in swallowing. It is common symptom reported by up to 46% of apparently healthy individuals and with peak incidence in middle age5. Dysphagia is common symptom with different forms of presentation, but always with difficulty in swallowing for solids, pastes and/or liquids. Depending on the severity and frequency, may lead patients to weight loss and malnutrition4,7,13.
The prevalence of functional pain, presumably of esophageal origin, is not known. However, pain in non-cardiac chest affects up to 26% of the general population and has no gender predilection11. The gastroesophageal reflux disease is the most common cause for non-cardiac pain, representing up to 60% of patients. Thus, exclude cardiac chest pain not related to gastroesophageal reflux should be the first goal of any diagnostic evaluation3,6.
Functional diseases of the esophagus are motility disorders that can be primary, if the motor alteration is the very expression of the disease, or secondary, if the underlying disease is systemic and esophageal involvement is only one of its manifestations. Examples of secondary are: diabetes mellitus, chronic idiopathic pseudo-obstruction, scleroderma, mixed connective tissue disease, rheumatoid arthritis, systemic lupus erythematosus, Chagas disease, alcoholism, amyloidosis, myxedema and multiple sclerosis13. As the pathophysiological processes in the secondary motor disorders are relatively well defined, it is easy to understand the origin of the abnormality affecting motor function13. However, in the absence of obvious cause, the classification of the main motor disorders is based on the lower esophageal sphincter and esophageal peristalsis abnormalities, and recorded by manometry.
Such disorders are currently more understood and can be explained on the basis of inhibitory defect or defective excitatory innervation of esophageal body and lower sphincter. Included in this group are achalasia, diffuse esophageal spasm, nutcracker esophagus, lower esophageal sphincter hypertension, ineffective esophageal motility and lower esophageal sphincter hypotension8.
The objective of this study is to determine the prevalence of primary esophageal motor disorders and relate them to the endoscopic and clinical findings in order to better be characterized.
METHODS
Were analyzed retrospectively 2614 manometric exams, being 1529 (58.49%) in women and 1085 (41.51%) in men, realized in private gastroenterology service, in which primary motor disorders of the esophagus were searched. Were found 299 cases in which were sought clinical and/or endoscopic data that motivated the exams.
Regarding manometry, were evaluated the lower esophageal sphincter (LES), the average respiratory pressure and maximal expiratory pressure evaluated by four radial channels, plus LES relaxation percentage. In the esophageal body was evaluated the presence of peristalsis, the wave conducted percentile (peristaltic) as well as amplitude and duration of the waves. There was also assessment of the upper esophageal sphincter pressure as the average of the four radial channels, in addition to relaxation and synchrony with the pharyngeal contraction.
For the diagnosis of primary esophageal motor disorder the following definitions were followed: 1) achalasia - absence of esophageal peristalsis7,12; 2) Nutcracker esophagus - Richter and Gothenburg criteria - characterized, respectively, by the presence of peristaltic contractions of greater amplitude or equal to 180 mmHg measured from the mean amplitude of 3 cm and 8 cm above LES16 and amplitude of contraction of the esophageal body greater than 180 mmHg at any level16; 3) ineffective esophageal motility - 30% or more of water swallowing with distal amplitudes below 30 mmHg8; 4) diffuse spasm - simultaneous contraction of the distal esophagus in over 20% of the water swallowing, amplitude of contractions higher than 30 mmHg, and normal intermittent peristalsis22; 5) hypertensive lower esophageal sphincter - LES pressure more than 45 mmHg with normal LES peristalsis and relaxation8.
From the analysis of these data were selected the ones with diagnosis of primary motor disorders of the esophagus. Using the same chart, data were correlated from 119 patients, the endoscopy and clinical manifestations usually associated with primary motor disorders of the esophagus, ie, heartburn, chest pain of presumed esophageal origin, dysphagia, odynophagia, regurgitation, pharyngeal globe and extra-esophageal symptoms, particularly cough and hoarseness. Endoscopic evaluation looked for food residue in the esophagus, hiatal hernia and erosive esophagitis.
For statistical analysis, the chi-square test (χ2) or Fisher's exact test (p)21were applied, in order to compare prevalence between genders as well as to compare the motor disorders on manometry in relation to symptoms and endoscopic findings. The significance level was set at 0.05 or 5.0%.
RESULTS
Primary functional disorders
Were found, according to the esophageal manometry, 49 cases of achalasia; 73 of diffuse spasm; 82 of ineffective esophageal motility; 89 of the esophagus Nutcracker, 21 by the criterion of Richter and 68 by Gothenburg´s; and six lower esophageal sphincter hypertension.
In addition, from esophageal manometry with primary motor disorder, only 119 had medical records with clinical and endoscopic examinations subject to analysis, thus the remainder of the examination was not considered in the statistical study.
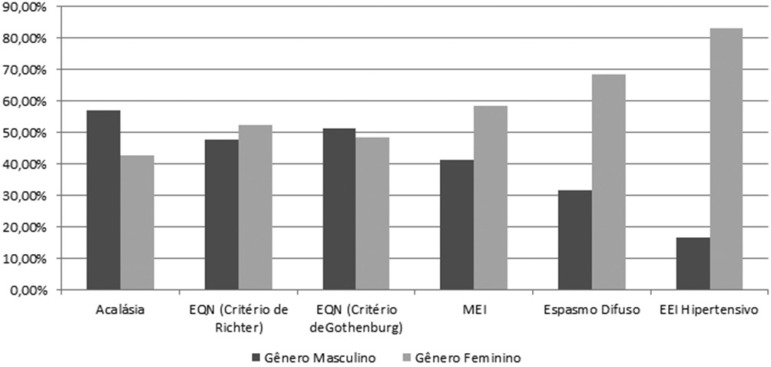
In achalasia, esophageal Nutcracker both criteria, and ineffective esophageal motility, the percentages were similar for both genders; but, in diffuse spasm and LES hypertension was predominance of women (Figure 1).
FIGURE 1.
Gender versus primary esophageal disorders
Achalasia (n=14)
Associated clinical findings
Heartburn was found in eight patients (57.14%); insufficiency in nine (64.29%); dysphagia in nine (64.29%); non-cardiac chest pain in six (41.86%); extra-esophageal symptoms (cough and hoarseness) in two (14.29%). The pharyngeal globe complaints and sore throat were not identified in any of the analyzed patients with manometric diagnosis of achalasia.
Endoscopic findings
It was verified the presence of hiatal hernia in eight patients (57.14%); erosive esophagitis in four (28.57%); and only one (7.14%) had residual food at the esophageal lumen.
Diffuse spasm (n=33)
Associated clinical findings
Heartburn was reported in 24 patients (72.72%); regurgitation in 21 (63.63%); dysphagia in 12 (36.36%); non-cardiac chest pain in eight (24.24%); two pharyngeal globe (6.06%); three odynophagia (9.09%); extra-esophageal symptoms (cough and hoarseness) in five (15.15%).
Endoscopic findings
The presence of hiatal hernia was described in 22 patients (66.66%); and erosive esophagitis in 13 (39.39%). Was not found any food waste on these patients.
Ineffective esophageal motility (n=29)
Associated clinical findings
Heartburn was present in 21 patients (72.41%); regurgitation in 21 (72.41%); dysphagia in four (13.79%); non-cardiac chest pain in four (13.79%); pharyngeal globe in six (20.69%); one odynophagia (3.45%); and extra-esophageal symptoms (cough and hoarseness) in 13 patients (44.83%).
Endoscopic findings
Hiatal hernia was present in 18 patients (63.07%); erosive esophagitis in 17 (58.62%); and food waste in one patient (3.45%).
Nutcracker esophagus (n=40)
According to the Richter criterion (n=17)
Associated clinical findings
Heartburn was found in 13 patients (76.47); regurgitation in six (35.29%); dysphagia in four (23.53%); non-cardiac chest pain in four (23.53%); two pharyngeal globe (11.76%); and extra-esophageal symptoms (cough and hoarseness) in three (17.65%). Odynophagia was not found in any patient.
Endoscopic findings
Erosive esophagitis was found in nine patients (52.94%); and hiatal hernia in 13 (76.47%). In none was confirmed the presence of food waste on exam.
According to the Gothenburg criterion (n=23)
Associated clinical findings
Heartburn was found in 20 patients (86.96%); regurgitation in 10 (43.48%); dysphagia in seven (30.43%); non-cardiac chest pain in six (26.09%); pharyngeal globe in five (21.74%); two odynophagia (8.70%); and extra-esophageal symptoms (cough and hoarseness) in 11 (47.83%).
Endoscopic findings
Was found hiatal hernia in 20 patients (86.96%); and erosive esophagitis in seven (30.43%). No patient showed the presence of food waste through endoscopy.
Lower esophageal sphincter hypertension (n=3)
Associated clinical findings
Heartburn was found in two patients (66.66%); regurgitation in one (33.33%); dysphagia in one (33.33%); non-cardiac chest pain in one (33.33%); pharyngeal globe in one (33.33%); sore throat in one (33.33%); and extra-esophageal symptoms (cough and hoarseness) in two.
Endoscopic findings
The presence of hiatal hernia was found in two patients (66.66%); erosive esophagitis and in one (33.33%). There was no residual food with endoscopy.
Table 1 summarizes the clinical and endoscopic data analyzed findings.
TABLE 1.
Incidence of clinical and endoscopic findings correlated to manometric data (n= 119)
| Achalasia (n=14) | Diffuse esophageal spasm (n=33) | Ineffective esophageal motility (n=29) | Nutcracker esophagus (n=40) | Lower esophageal sphincter hypertension (n=3) | |||
|---|---|---|---|---|---|---|---|
| Richter (n=17) | Gothenburg (n=23) | ||||||
| Associated clinical findings | Pyrosis | 8 (57,14%) | 24 (72,72%) | 21 (72,41%) | 13 (76,47%) | 20 (86,96%) | 2 (66,66%) |
| Regurgitation | 9 (64,29%) | 21 (63,63%) | 21 (72,41% | 6 (35,29%) | 10 (43,48%) | 1 (33,33%) | |
| Disphagia | 9 (64,29%) | 12 (36,36%) | 4 (13,79%) | 4(23,53%) | 7 (30,43%) | 1 (33,33%) | |
| Non-cardiac chest pain | 6 (41,86%) | 8 (24,24%) | 4 (13,79%) | 4 (23,53%) | 6 (26,09%) | 1 (33,33%) | |
| Extra-esophageal symptoms | 2 (14,29%) | 5 (15,15%) | 13 (44,83%) | 3 (17,65%) | 11 (47,83%) | 2 (66,66%) | |
| Pharingeal globe | - | 2 (6,06%) | 6 (20,69%) | 2 (11,76%) | 5 (21,74%) | 1 (33,33%) | |
| Odinophagia | - | 3 (9,09%) | 1 (3,45%) | - | 2 (8,70%) | 1 (33,33%) | |
| Endoscopic findings | Hiatal hernia | 8 (57,14%) | 22 (66,66%) | 18 (63,07%) | 9 (52,94%) | 20 (86,96%) | 2 (66,66%) |
| Erosive esophagitis | 4 (28,57%) | 13 (39,39%) | 17 (58,62%) | 13 (76,47%) | 7 (30,43%) | 1 (33,33%) | |
| Residual waste in esophageal lumen | 1 (7,14%) | - | 1 (3,45%) | - | - | - | |
Associated clinical disorders and diseases (n=119)
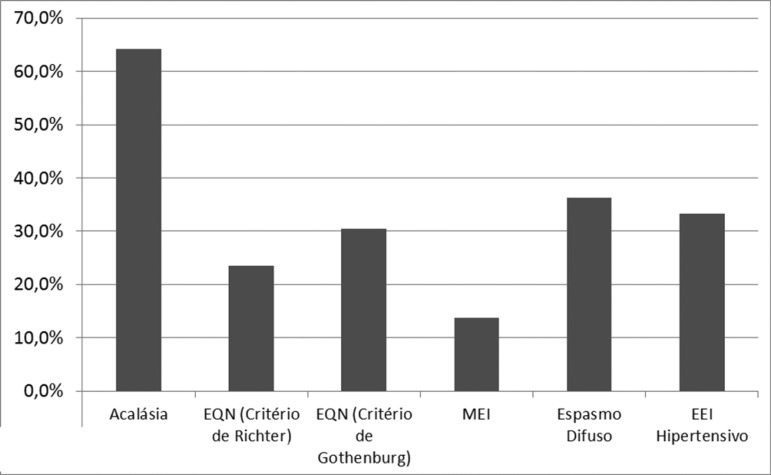
Dysphagia versus disorders
Dysphagia was more frequently found in achalasia than in other conditions (Figure 2).
FIGURE 2.
Dysphagia distribution between esophageal primary motor disorders
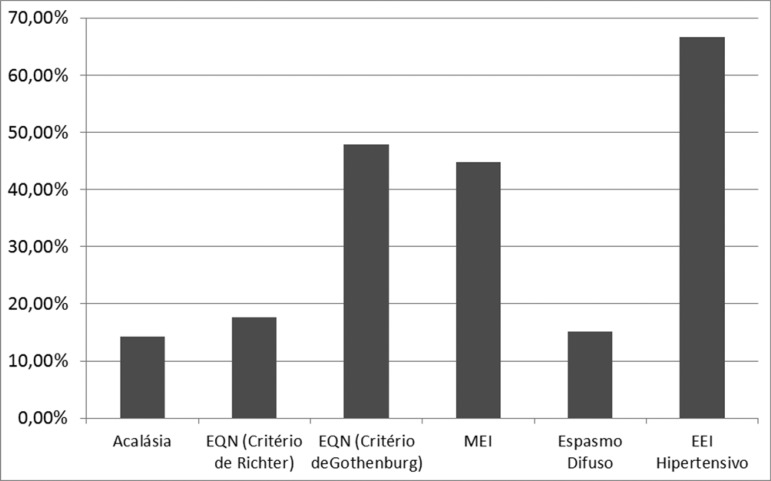
Extra-esophageal symptoms versus diseases
Hypertensive LES was the disosrder with more extra-esophageal symptoms (Figure 3)
FIGURE 3.
Distribution of extra-esophageal symptoms of primary esophageal motor diseases
Endoscopic findings and diseases
There was no statistical relevance of these data.
DISCUSSION
Esophageal manometry is considered the gold standard test for diagnosis of functional disorders of the esophagus. It is possible to identify the presence or absence of esophageal aperistalsis, no relaxation or incomplete LES relaxation, in the case of achalasia17.
Based on the results observed in this study it is clear that it cannot be taken into consideration only the heartburn and erosive esophagitis in the diagnosis of gastroesophageal reflux disease as criteria for performing surgical treatment, since there are also significant prevalence of this symptom and endoscopic finding in other primary functional disorders of the esophagus, so, demonstrating the need of manometry as a preoperative examination in patients with this condition.
Many studies report dysphagia and regurgitation as main symptoms of achalasia1,8,15 with prevalence rates above 90% and 76-91%, respectivamente1,14. In this paper, dysphagia was observed in only 64.29% of patients; even more common than in other primary motor disorders of the esophagus, it cannot be considered pathognomonic. Stand out from here the importance of dysphagia scales that could better characterize and allow proper comparison with the literature20. Its clinical importance lies in the fact that it is the main symptom of the primary functional diseases of the esophagus and its characterization is essential to the management of these patients2.
The cough and hoarseness symptoms were observed in all primary esophageal disorders, but more prevalent in hypertensive lower esophageal sphincter, although with the bias of the small sample in this condition.
The cases of Nutcracker esophagusl diagnosed by either Richter or Gothenburg criteria did not change significantly among the analyzed parameters.
Note that these data were obtained with conventional manometry and currently there is high-resolution manometry, which was developed with lumen catheters spaced less than 2 cm. This examination reveals the complex functional anatomy of esophageal peristalsis and esophagogastric junction9,10,18. It improves the ability to verify the effectiveness to conduct the bolus through the esophagus and the occurrence of reflux, compared to the conventional system9,10,18. Although in general the diagnostic correlation between the two is high, the new method improves the diagnostic yield, especially in cases of functional dysphagia.
The measurement of the esophagogastric pressure gradient increases diagnostic accuracy for achalasia in the differential diagnosis with diffuse spasm. It differs from the rapid rise in intra-bolus pressure (focal dysmotility or impaired function of the LES), which occurs in achalasia9,10,18.
Thus, the correlation between manometric findings and the future of the treatment of achalasia needs to be revised in the near future, including chagasic etiology23.
So, with this more accurate methodology it could be verified that in this study the cases of achalasia were underestimated, possibly requiring change on strategy, as that preferential treatment is surgical and effective.
CONCLUSION
The clinical and endoscopic findings have little value in the characterization of the primary motor disorders of the esophagus, showing even more the need for manometry, particularly in the preoperative period of gastroesophageal reflux disease.
Footnotes
Financial source: none
REFERENCES
- 1.Boeckxstaens GE, Zaninotto G, Richter JE. Achalasia. Lancet. 2014;383(9911):83–93. doi: 10.1016/S0140-6736(13)60651-0. [DOI] [PubMed] [Google Scholar]
- 2.Cuenca RM, Malafaia DT, Souza GM, Souza LRQ, Motta VP, Lima MRA, Garcia CJFS. Síndrome Disfágica. ABCD Arq Bras Cir Dig. 2007;20(2):116–118. [Google Scholar]
- 3.Dekel R, Fass R. Current Perspectives on the Diagnosis and Treatment of Functional Esophageal Disorders. Current gastroenterology reports. 2003;5(4):314–322. doi: 10.1007/s11894-003-0069-8. [DOI] [PubMed] [Google Scholar]
- 4.Domingues GR, Lemme EMO. Diagnóstico diferencial dos distúrbios motores esofagianos pelas características da disfagia. Arq Gastroenterol. 2001;38(1):14–18. doi: 10.1590/s0004-28032001000100004. [DOI] [PubMed] [Google Scholar]
- 5.Drossman DA, Li Z, Andruzzi E, Temple RD, Talley NJ, Thompson WG, et al. U.S. householders survey of functional gastrointestinal disorders. Prevalence, sociodemography, and health impact. Dig Dis Sic. 1993;38(9):1569–1580. doi: 10.1007/BF01303162. [DOI] [PubMed] [Google Scholar]
- 6.Drossman DA. The Functional Gastrointestinal Disorders and the Rome III Process. Gastroenterology. 2006;130(5):1377–1390. doi: 10.1053/j.gastro.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 7.Eckardt AJ, Eckardt VF. Current clinical approach to achalasia. World J Gastroenterol. 2009 Aug;15(32):3969–3975. doi: 10.3748/wjg.15.3969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fisichella PM, Carter SR, Robles LY. Presentation, diagnosis, and treatment of oesophageal motility disorders. Dig Liver Dis. 2012;44(1):1–7. doi: 10.1016/j.dld.2011.05.003. [DOI] [PubMed] [Google Scholar]
- 9.Fisichella PM, Jalilvand A, Lebenthal A. Diagnostic Evaluation of Achalasia: From the Whalebone to the Chicago Classification. World J Surg. 2015 Jan 10; doi: 10.1007/s00268-014-2939-7. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 10.Fox MR, Bredenoord AJ. Oesophageal high-resolution manometry: moving from research into clinical practice. Gut. 2008;57(3):405–423. doi: 10.1136/gut.2007.127993. [DOI] [PubMed] [Google Scholar]
- 11.Locke 3rd GR, Talley NJ, Fett SL, Zinsmeister AR, Melton 3rd LJ. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted County, Minnesota. Gastroenterology. 1997;112(5):1448–1456. doi: 10.1016/s0016-5085(97)70025-8. [DOI] [PubMed] [Google Scholar]
- 12.Mikaeli J, Farrokhi F, Bishehsari F, Mahdavinia M, Malekzadeh R. Gender effect on clinical features of achalasia: a prospective study. BMC Gastroenterol. 2006;6(12) doi: 10.1186/1471-230X-6-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mittal RK, Bhalla V. Oesophageal Motor Functions and its Disorders. Gut. 2004;53(10):1536–1542. doi: 10.1136/gut.2003.035618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moonen AJ, Boeckxstaens GE. Management of Achalasia. Gastroenterol Clin N AM. 2013 Mar;42(1):45–55. doi: 10.1016/j.gtc.2012.11.009. [DOI] [PubMed] [Google Scholar]
- 15.Pandolfino JE, Kahrilas PJ. Presentation, Diagnosis, and Management of Achalasia. Clin Gastroenterol Hepatol. 2013 Aug;11(8):887–897. doi: 10.1016/j.cgh.2013.01.032. [DOI] [PubMed] [Google Scholar]
- 16.Pilhall M, Börjesson M, Rolny P, Mannheimer C. Diagnosis of Nutcracker Esophagus, Segmental or Diffuse Hypertensive Patterns, and Clinical Characteristics. Dig Dis Sci. 2002 Jun;47(6):1381–1388. doi: 10.1023/a:1015343119090. [DOI] [PubMed] [Google Scholar]
- 17.Pohl D, Tutuian R. Achalasia: an Overview of Diagnosis and Treatment. J Gastrointestin Liver Dis. 2007;16(3):297–303. [PubMed] [Google Scholar]
- 18.Richter JE. High-resolution manometry in diagnosis and treatment of achalasia: help or hype. Curr Gastroenterol Rep. 2014 Dec;16(12):420–420. doi: 10.1007/s11894-014-0420-2. [DOI] [PubMed] [Google Scholar]
- 19.Ritcher JE. Oesophageal motility disorders. Lancet. 2001 Sep;358(9284):823–828. doi: 10.1016/S0140-6736(01)05973-6. [DOI] [PubMed] [Google Scholar]
- 20.Sallum RAA, Duarte AF, Cecconello I. Analitic review of disphagia scales. ABCD Arq Bras Cir Dig. 2012;25(4):279–232. doi: 10.1590/s0102-67202012000400013. [DOI] [PubMed] [Google Scholar]
- 21.Siegel S, Castellan NJJ. Estatística não paramétrica para ciências do comportamento. 2. ed. Porto Alegre: Penso; 2006. p. 448. [Google Scholar]
- 22.Tsuboi K, Mittal SK. Diffuse esophageal spasm: has the term lost its relevance? Analysis of 217 cases. Dis Esophagus. 2011;24:354–359. doi: 10.1111/j.1442-2050.2010.01146.x. [DOI] [PubMed] [Google Scholar]
- 23.Vicentine FP, Herbella FA, Allaix ME, Silva LC, Patti MG. High-resolution manometry classifications for idiopathic achalasia in patients with Chagas' disease esophagopathy. J Gastrointest Surg. 2014 Feb;18(2):221–224. doi: 10.1007/s11605-013-2376-1. [DOI] [PubMed] [Google Scholar]