Abstract
Objective
Adverse experiences in childhood may influence cardiovascular risk in adulthood. We examined the prospective associations between types of psychosocial adversity as well as having multiple adversities (e.g., cumulative risk) with carotid intima-media thickness (IMT) and its progression among young adults. Higher cumulative risk score in childhood was expected to be associated with higher IMT and its progression.
Methods
Participants were 2265 men and women (age range: 24-39 years in 2001) from the on-going Cardiovascular Risk in Young Finns study whose carotid IMT were measured in 2001 and 2007. A cumulative psychosocial risk score, assessed at the study baseline in 1980, was derived from four separate aspects of the childhood environment that may impose risk (childhood stressful life-events, parental health behavior family, socioeconomic status, and childhood emotional environment).
Results
The cumulative risk score was associated with higher IMT in 2007 (b=.004; se=.001; p<.001) and increased IMT progression from 2001 to 2007 (b=.003; se=.001; p=.001). The associations were robust to adjustment for conventional cardiovascular risk factors in childhood and adulthood, including adulthood health behavior, adulthood socioeconomic status and depressive symptoms. Among the individual childhood psychosocial risk categories, having more stressful life-events was associated with higher IMT in 2001 (b=.007; se=.003; p=.016) and poorer parental health behavior predicted higher IMT in 2007 (b=.004; se=.002; p=.031) after adjustment for age, sex and childhood cardiovascular risk factors.
Conclusions
Early life psychosocial environment influences cardiovascular risk later in life and considering cumulative childhood risk factors may be more informative than individual factors in predicting progression of preclinical atherosclerosis in adulthood.
Keywords: cardiovascular diseases, cumulative risk score, psychosocial
Atherosclerotic diseases such coronary heart disease and stroke are leading causes of death in the world. Such diseases start to develop early in life and thus have a long preclinical phase. Carotid artery intima-media thickness (IMT) has been shown to be a surrogate measure of preclinical atherosclerosis (1). Childhood biological risk factors such as obesity and high LDL-cholesterol predict increased IMT (2-4) and IMT progression (5-7) in adulthood, suggesting that the risk for the development of atherosclerosis begins relatively early in life. In addition to the established biological risk factors, exposure to adverse psychosocial environment during childhood has been suggested to contribute to poor cardiovascular health in adulthood (8). Low socioeconomic status (SES) (9-11) poor parenting practices, (12, 13) and adverse events (14) during childhood or adolescence have been found to predict later cardiovascular risks.
Instead of concentrating on single risk factors, researchers have increasingly started to investigate the possible effects of an cumulation of psychosocial risk factors (15). In a cross-sectional study, co-occurrence of stress related factors was found to be associated with higher IMT at least in African American women (16). In addition, in a longitudinal study of large cohort, a cumulative psychosocial risk factor score was related to increased risk of coronary heart disease (17). However, we are not aware of any prospective studies that have examined the accumulation of childhood psychosocial risk factors as predictor of preclinical atherosclerosis.
The aim of the current study was to investigate whether early childhood psychosocial environmental risks are associated with adult IMT, a marker of pre-clinical atherosclerosis. A ‘risky families’ model (13) that characterizes ‘risky families’ as aggressive and conflictive, and having negative and unsupportive relationships between family members, is used as a theoretical basis for the current study. Family SES has been tied to most of the risky family attributes (13), whereas stressful events, such as parental divorce, contribute to (or partly define) level of conflict in the family. Additionally, parental health behaviors can be seen as a part of psychosocial risk factors as they reflect parental modeling and unhealthy environment, i.e., they are an integral part of the childhood environment affecting future health and health behavior of their children (e.g., parental smoking has been associated with increased risk of offspring’s smoking initiation (18)). Thus, the following four categories of psychosocial risk were used to measure childhood environment: emotional environment, socioeconomic environment, stressful events, and parental health behaviors. We examined whether these individual risk categories and their composite score during childhood predict IMT and IMT progression during early adulthood over and above well-established biological risk factors for IMT (5). In addition, we examined whether associations would persist after controlling for four possible pathways, i.e., adult biological risk factors, adult health behavior, adulthood SES, and adulthood depressive symptoms, that have been hypothesized to link early psychosocial adversity with IMT (5, 19, 20). Based on previous findings, we hypothesized that childhood psychosocial cumulative risk score would be associated with higher IMT and its progression in a linear fashion and that these associations would persist after controlling traditional cardiovascular risk factors in childhood and adulthood.
Methods
Participants
Participants were selected from the ongoing population based Cardiovascular Risk in Young Finns study that began in 1980 (21, 22). The original sample included 3596 children and adolescents (aged 3 – 18 in 1980) and participants of the original sample were randomly selected from the national register that covers the whole population of Finland. Follow-up data collections have been conducted in 1983, 1986, 1989, 2001, 2007, and 2010/2011. Written informed consent was obtained from participants who were at least 9 years old and from the parents of younger participants. Research plan and data collection procedures were accepted by five universities (Helsinki, Turku, Tampere, Kuopio and Oulu) review boards, and data collection was conducted according to WHO standards as well as the Helsinki Declaration.
For the present study follow-up examinations from years 2001 and 2007 were used. 2265 participants (mean age 31.7 years in 2001; age range 24-39) had complete IMT data from the year 2001, and thus these participants formed the current study sample. Multiple imputation method was used to keep the maximum number of participants in the analyses. Imputation model, which contained demographics, dichotomized childhood psychosocial risk factors, childhood and adulthood biological risk factors, and adulthood measures in 2001 and 2007, was created to impute any missing data in childhood risk factors in 1980, adulthood covariates in 2001, and adulthood measures in 2007. Except for two variables, hospitalization of the father and father’s obesity, which contained 16% and 14% missing data, respectively, most childhood variables had only small amount of missing data (between 0% and 5%). Adulthood variables in 2001 contained only small proportion of missing data (between 0% and 7%), whereas between 19% and 22% of data was missing in 2007. Thus, 456 missing IMT values from 2007 were imputed. Multiple imputation was done using chained equations procedure in Stata 13.1 to obtain 25 imputed datasets (23).
Attrition analysis showed that the excluded participants had had higher number of parental health behavior and socioemotional risks (p < .05) than included participants, but there were no differences in the amount of other childhood risks or childhood covariates.
Measures
Childhood psychosocial risk factors
Childhood risk factors were assessed by parental reports at the baseline examination in 1980. Four separate psychosocial risk categories were formed: (1) stressful life-events, (2) parental health behaviors, (3) family socioeconomic factors, and (4) socioemotional factors. Scores for each psychosocial risk category were derived by summing up the components using the following logic: 1 point was assigned when a component conferred risk and 0 points when the component did not confer risk. In addition to developing a score for each individual risk category, a total cumulative risk score was calculated by summing together scores from all the individual psychosocial risk categories. Because there are no clinically established thresholds for many of the components used to indicate risk in the current study, the cut-off points were defined based on theoretical and empirical knowledge. For example, the cut-off points for SES were based on a previous suggestion of suitable cut-off points for childhood SES (24), and the cut-off points for emotional scales (life satisfaction, parental nurturance) were based on the highest quartile as is conventional in psychosocial health studies examining the association of psychosocial factors with health (15). The naturally occurring cut-off points were, for instance, having a mental disorder (no/yes), being a smoker (no/yes) (25), or having a life event (no/yes) (14). Similar approach has also been used in two recent studies (26, 27). Specific components of the risk categories are shown in Table 1 and described in detail below.
Table 1.
Childhood risk categories and their components
| Risk category and component | Measure/scale |
|---|---|
| Stressful life-events |
|
| Moving | Change of residence at least three times during childhood |
| Change of school | Change of school at least once during childhood |
| Family break-up | Parental divorce or separation |
| Loss | Death of family member/significant person |
| Hospitalization and/or serious illness | Long-term hospitalization (>2 weeks) or serious disease in the family |
|
|
|
| Risky parental health behavior |
|
| Excess energy intake (mother) | Body-mass index ≥30.0 |
| Excess energy intake (father) | Body-mass index ≥30.0 |
| Smoking (mother) | Daily smoking |
| Smoking (father) | Daily smoking |
| Physical inactivity (mother) | < 3 times per week |
| Physcial inactivity (father) | < 3 times per week |
|
|
|
| Unfavorable socioeconomic environment |
|
| Low occupational status | Manual occupationa |
| Low educational level | Comprehensive schoola |
| Low family income | Annual income in lowest quartile |
| Occupational instability | Unemployment, long-term sick-leave, disability pensionb |
|
|
|
| Unfavorable emotional family environment |
|
| Parental mental disorder | Any diagnosis for mental disorderb |
| Emotionally distant caregiving | The nurturance scalec |
| High parental dissatisfaction | The dissatisfaction scalec |
| Heavy alcohol use pattern | Heavy intoxication (>6 units) weeklyb |
Both parents had to fulfill this criterion.
Either parent had to fulfill this criterion.
Main caregiver in the household replied; in single parent-households, the available parent replied
-
(1)
Stressful life events were derived based on scores for the following six experiences: moving residence, school changes, divorce in the family, deaths of significant persons (parents, siblings) and hospitalization and/or serious illness in the family. School change was included as a component of stressful life events as it captures possible peer group change. Presence of each event during participant’s childhood was assigned 1 point, otherwise the experience was assigned 0.
-
(2)
Parental health behaviors included the following six behaviors: mothers’ and fathers’ body mass index (BMI), smoking status, and levels of regular physical activity. The following cut-off points were used to establish the presence of high risk level each category: either or both mother and father were obese (BMI>30 kg/m2), mother or father or both were current smokers, either father and mother or both reported no regular physical activity.
-
(3)
Four components were used to derive a risk score for family socioeconomic factors: education (number of completed school years), occupational status (high non-manual, lower non –manual and manual), family income, and parents’ employment history. The following cut-off points were used to define high risk levels: low education (less than 9 years), manual occupation, low income (lowest 25%), and unsteady employment history (unemployment spells, long-term sickness absences spells, retired parents due to sickness). Family education and family occupational status were defined according to the parent with the highest education or occupational status.
-
(4)
Socioemotional factors were derived based on four factors, including parent’s mental health status, parents’ child-rearing style, parents’ life satisfaction and parents’ alcohol abuse. Mental health status was measured with the following question: “Have you ever been diagnosed by a health professional as having a mental health problem? (no/yes)”. Responding “yes” was considered as high risk, i.e. 0=low risk, 1=high risk. Parents’ child-rearing style was measured using a five-point scale that was derived from the Operation Family study (28). This scale contains seven items assessing two different child-rearing dimensions, i.e. emotional significance (e.g., “I enjoy spending time with my child” (1=all the time…5=very seldom) and tolerance (“My child prevents me from fulfilling my needs” (1=all the time…5=very seldom), which form a uniform scale. Details of the scale have been reported elsewhere (29). Providing a negative response, i.e. 4 or 5 in a five-point scale, to any item of the scale was used to indicate high risk. Parents’ life satisfaction scale was also based on the Operation Family study (28), and it contains three questions that measure parental satisfaction as a mother/father, as a spouse, and with her/his work role (e.g. “I am satisfied as a mother”; 1=not at all, 5=very much). A response of being dissatisfied with any of the three life areas was classified as high risk. Parent’s heavy alcohol use was included as a component of the socioemotional environment because of evidence indicating that unhealthy drinking is harmful to emotional development (30). Parent’s heavy alcohol use was measured as a number of heavy drinking occasions during year and an answer “Once a week” was used as the cut-off point for high risk.
Childhood and adulthood biological risk factors
At the baseline and follow-ups, weight and height were measured, and BMI was calculated by dividing participants’ weight in kilograms by their squared height in meters. In 1980, blood pressure was measured using a standard mercury sphygmomanometer. However, an ultrasound device was used among 3-year-olds. Adulthood clinic measurements were performed in 2001 and 2007. Clinic staff using a random zero sphygmomanometer measured systolic blood pressure. A mean of three measures was used. Standard enzymatic methods were used to measure serum HDL-cholesterol from blood samples. The Friedewald’s equation was used to calculate the LDL-cholesterol concentration. Details of the used methods have been described and reported previously (21)
Adulthood carotid artery ultrasound studies
B-mode ultrasound studies of the left carotid artery were performed in 2001 and 2007 with standardized protocols that have been described previously (2, 5). At least 4 measurements of the far wall were taken approximately 10 mm proximal to the bifurcation to derive maximum carotid IMT during both study years. IMT progression was measured by subtracting the 2001 value from the 2007 value.
Adulthood health behavior
All health behaviors were self-reported in 2001 and 2007. Current smoking (yes/no) was assessed and information on alcohol consumption was assessed by asking individuals to report the frequency with which they consumed at least six portions of alcohol (one portion equals 12 g of alcohol) at a time (6-point scale ranging from 0 = once a year or never to 5 = at least twice a week). Physical activity was measured using Physical Activity Index (31), which measures intensity, frequency, and duration of physical activity during leisure time.
Adulthood SES
Educational level and occupational status were self-reported in 2001 and 2007, and used as indicators of SES. Educational level was classified as follows: 1=low (comprehensive school); 2=intermediate (secondary education): 3=high (academic, graduated from a polytechnic or studying at or graduated from a university). Occupational status was based on the Central Statistical Office of Finland classification: 1 = manual (e.g., factory worker, waiter, cleaner); 2 = lower grade non-manual (e.g., clerical employee, sales representative, secretary); 3 = higher grade non-manual (e.g., general manager, lawyer, physician, secondary school teacher).
Adulthood depressive symptoms
Depressive symptoms were assessed in 2001 and 2007 using a modified version of the Beck Depression Inventory (BDI) (32). Whereas the original BDI is a 21-item questionnaire that offers four alternative response statements for each item, the modified version of the BDI consists of 21 items presenting the second mildest response statements of the original BDI. Respondents are asked to rate each statement on a 5-point scale (1=not at all; 5= very much). Overall mean score was then calculated. Internal consistency of the modified version of the BDI was good (Cronbach’s alpha ranging from 0.92 to 0.93) and it has been shown that the modified version of the BDI provides more information on less severe depression than the clinical Beck Depression Inventory II (33).
Statistical Analyses
Linear regression analysis was used to analyze the association between the cumulative risk score, each psychosocial risk category, and IMT thickness in 2001 and 2007, and IMT progression from 2001 to 2007. All analyses were adjusted for age and sex. In addition, four separate adjustment models (childhood biological conditions, adulthood biological conditions, adulthood health behaviors and adulthood psychological functioning) were used to examine the extent to which different sets of covariates may attenuate the association between childhood risk categories and adulthood IMT. Thus, additional adjustments were done for [1] childhood cardiovascular risk factors (BMI, systolic blood pressure and LDL cholesterol), [2] adulthood cardiovascular risk factors (BMI, systolic blood pressure, and LDL cholesterol), [3] adulthood health behavior (smoking, alcohol consumption and physical activity), [4] adulthood SES and depressive symptoms, and in these analyses covariates from the same year as the IMT measure were used. However, in the analysis of IMT progression, changes in covariates were used instead. IMT in 2001 was used as a covariate in the IMT progression analyses as the IMT in 2001 may affect the magnitude of change. To avoid possible multicollinearity, we only used cardiovascular covariates that have been shown to be associated with IMT or its progression (5). Exposure and outcomes measures were not standardized.
Results
Characteristics of the study participants are shown in Table 2. Older age was associated with higher IMT in 2001 (b=.006; se=.0004; p<0.001) and 2007 (b=.007; se=.0004; p<0.001), and with more rapid IMT progression (b=.003; se=.0003; p<0.001). Men had higher levels of IMT in 2001 (b=.021; se=.004; p<0.001) and 2007 (b=.033; se=.004; p<0.001), and their IMT progression was faster (b=.020; se=.004; p<0.001) when compared to women.
Table 2.
Characteristics of the study group (n=2265). Values are means or proportions and standard errors (SE).
| Male | SE | Range | Female | SE | Range | |
|---|---|---|---|---|---|---|
| Number of participants | 1018 | 1247 | ||||
| Age (2001) | 31.69 | 5.01 | 24-39 | 31.67 | 4.97 | 24-39 |
| Childhood measures | ||||||
| Stressful life events | 0.41 | 0.02 | 0-3 | 0.42 | 0.02 | 0-3 |
| Health behavioral risks | 1.06 | 0.04 | 0-5 | 1.16 | 0.03 | 0-6 |
| Socioeconomic risks | 1.10 | 0.04 | 0-5 | 1.14 | 0.04 | 0-5 |
| Socioemotional risks | 0.39 | 0.02 | 0-3 | 0.39 | 0.02 | 0-3 |
| Cumulative risk score | 2.97 | 0.07 | 0-10 | 3.11 | 0.06 | 0-10 |
| LDL cholesterol, mmol/L | 3.28 | 0.02 | 9.2-36.9 | 3.41 | 0.02 | 1.7-7.6 |
| Systolic blood pressure, mm|Hg | 113.79 | 0.41 | 78-174 | 112.06 | 0.31 | 68-144 |
| Body mass index, kg/m2 | 18.00 | 0.10 | 9.2-36.9 | 17.85 | 0.09 | 9.9-35.6 |
| Adulthood measures (2001) | ||||||
| Carotid intima-media thickness, mm | 0.59 | 0.00 | 0.4-1.3 | 0.57 | 0.00 | 0.4-1 |
| Body mass index, kg/m2 | 25.73 | 0.13 | 15.7-47.8 | 24.53 | 0.13 | 15.7-47.3 |
| LDL cholesterol, mmol/L | 3.42 | 0.03 | −0.7-7.9 | 3.16 | 0.02 | 0-6.7 |
| Systolic blood pressure, mm|Hg | 121.56 | 0.39 | 86.7-180 | 112.60 | 0.35 | 80.7-166.7 |
| Smoking | ||||||
| Yes | 0.57 | 0.02 | 0.71 | 0.01 | ||
| No | 0.43 | 0.02 | 0.29 | 0.01 | ||
| Alcohol consumption | 2.15 | 0.04 | 0-5 | 1.08 | 0.03 | 0-5 |
| Physical activity indexa | 8.93 | 0.07 | 5-15 | 8.81 | 0.05 | 5-15 |
| Educational levelb | 2.16 | 0.02 | 1-3 | 2.19 | 0.02 | 1-3 |
| Occupational statusc | 1.91 | 0.03 | 1-3 | 2.13 | 0.02 | 1-3 |
| Depressive symptomsd | 1.95 | 0.02 | 1-4.6 | 2.13 | 0.02 | 1-4.6 |
Note. Except for childhood risk factors, body mass index in childhood, physical activity and educational level, there were differences between men and women (p < .01).
Physical activity was measured using Physical Activity Index.
Educational level was classified as follows: 1=low; 2=intermediate; 3=high.
Occupational status was classified as follows: 1=manual; 2=lower grade non-manual; 3=higher grade non-manual.
Depressive symptoms were assessed using modified BDI
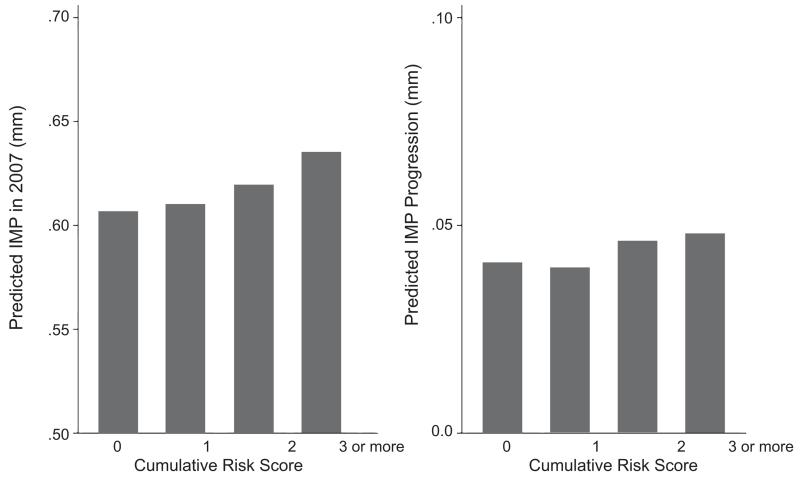
Higher cumulative psychosocial risk score predicted higher IMT in 2007 and faster IMT progression after adjusting for age and sex (Table 3). Adjustment for childhood cardiovascular risk factors did not affect the association between the cumulative risk score and IMT in 2007, but slightly attenuated the association between the cumulative risk score and IMT progression. Additional adjustment for adulthood cardiovascular risk factors slightly attenuated the association between the cumulative risk score and IMT in 2007, but did not affect the association between the cumulative risk score and IMT progression. Further adjustment for adulthood health behaviors, depressive symptoms, and SES did not attenuate the associations. The associations between the cumulative risk score with IMT in 2007 and IMT progression are illustrated in Figure 1.
Table 3.
Associations (non-standardized betas, standard errors and p-values) between cumulative risk score and childhood risk categories (stressful life events, health behavioral risks, socioeconomic risks and socioemotional risks) with adulthood IMT measures
| IMT 2001 | IMT 2007 | IMT change | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Cumulative risk score | b | se | p | b | se | p | b | se | p |
|
| |||||||||
| Base Model | 0.002 | 0.001 | 0.066 | 0.004 | 0.001 | <0.001 | 0.003 | 0.001 | 0.001 |
| Model 1 | 0.001 | 0.001 | 0.16 | 0.003 | 0.001 | 0.002 | 0.002 | 0.001 | 0.004 |
| Model 2 | 0.001 | 0.001 | 0.34 | 0.002 | 0.001 | 0.026 | 0.002 | 0.001 | 0.005 |
| Model 3 | 0.001 | 0.001 | 0.43 | 0.002 | 0.001 | 0.027 | 0.002 | 0.001 | 0.007 |
| Model 4 | 0.001 | 0.001 | 0.24 | 0.002 | 0.001 | 0.034 | 0.002 | 0.001 | 0.009 |
|
| |||||||||
| Stressful life-events | b | se | p | b | se | p | b | se | p |
|
| |||||||||
| Base Model | 0.006 | 0.003 | 0.020 | 0.005 | 0.003 | 0.11 | 0.001 | 0.003 | 0.65 |
| Model 1 | 0.007 | 0.003 | 0.016 | 0.005 | 0.003 | 0.10 | 0.001 | 0.003 | 0.64 |
| Model 2 | 0.006 | 0.003 | 0.021 | 0.004 | 0.003 | 0.21 | 0.001 | 0.003 | 0.70 |
| Model 3 | 0.006 | 0.003 | 0.028 | 0.004 | 0.003 | 0.21 | 0.001 | 0.003 | 0.71 |
| Model 4 | 0.006 | 0.003 | 0.032 | 0.004 | 0.003 | 0.21 | 0.001 | 0.003 | 0.72 |
|
| |||||||||
| Health behavioral risks | b | se | p | b | se | p | b | se | p |
|
| |||||||||
| Base Model | 0.003 | 0.002 | 0.12 | 0.005 | 0.002 | 0.010 | 0.004 | 0.002 | 0.035 |
| Model 1 | 0.002 | 0.002 | 0.22 | 0.004 | 0.002 | 0.031 | 0.003 | 0.002 | 0.074 |
| Model 2 | 0.002 | 0.002 | 0.31 | 0.003 | 0.002 | 0.13 | 0.003 | 0.002 | 0.095 |
| Model 3 | 0.002 | 0.002 | 0.35 | 0.003 | 0.002 | 0.14 | 0.003 | 0.002 | 0.098 |
| Model 4 | 0.002 | 0.002 | 0.27 | 0.003 | 0.002 | 0.14 | 0.003 | 0.002 | 0.11 |
|
| |||||||||
| Socioeconomic risks | b | se | p | b | se | p | b | se | p |
|
| |||||||||
| Base Model | 0.000 | 0.002 | 0.98 | 0.004 | 0.002 | 0.039 | 0.004 | 0.002 | 0.015 |
| Model 1 | −0.001 | 0.002 | 0.60 | 0.002 | 0.002 | 0.16 | 0.003 | 0.002 | 0.054 |
| Model 2 | −0.002 | 0.002 | 0.35 | 0.001 | 0.002 | 0.41 | 0.003 | 0.002 | 0.061 |
| Model 3 | −0.002 | 0.002 | 0.35 | 0.002 | 0.002 | 0.39 | 0.003 | 0.002 | 0.064 |
| Model 4 | −0.001 | 0.002 | 0.56 | 0.002 | 0.002 | 0.38 | 0.003 | 0.002 | 0.068 |
|
| |||||||||
| Socioemotional risks | b | se | p | b | se | p | b | se | p |
|
| |||||||||
| Base Model | −0.001 | 0.003 | 0.81 | −0.001 | 0.003 | 0.80 | −0.001 | 0.003 | 0.85 |
| Model 1 | 0.000 | 0.003 | 0.97 | 0.000 | 0.003 | 0.934 | 0.000 | 0.003 | 0.91 |
| Model 2 | 0.001 | 0.003 | 0.84 | 0.001 | 0.003 | 0.84 | 0.000 | 0.003 | 0.94 |
| Model 3 | 0.000 | 0.003 | 0.97 | 0.001 | 0.003 | 0.87 | 0.000 | 0.003 | 0.92 |
| Model 4 | 0.000 | 0.003 | 0.96 | 0.000 | 0.003 | 0.89 | 0.000 | 0.003 | 0.93 |
Note. Childhood risk categories were inserted simultaneously in the same regression model and the following four adjustment models (childhood biological risk factors, adulthood biological risk factors, adulthood health behaviors and adulthood psychological functioning) were used to examine the extent to which different sets of covariates may attenuate the association between childhood risk categories and adulthood IMT:
| Base model. | Adjusted for age and sex |
|---|---|
| Model 1 (childhood biological risk factors). | Base model + childhood BMI, LDL cholesterol, and systolic blood pressure |
| Model 2 (adulthood biological risk factors). | Model 1 + adulthood BMI, LDL cholesterol, and systolic blood pressure |
| Model 3 (adulthood health behavior). | Model 2 + adulthood smoking, alcohol consumption, and physical activity |
| Model 4 (adulthood psychological functioning). | Model 3 + adulthood depressive symptoms and socioeconomic status |
Figure 1.
Predicted values of IMT in 2007 and IMT progression by childhood cumulative risk score. Values are adjusted for age, sex, childhood and adulthood cardiovascular risk factors (BMI, LDL cholesterol, systolic blood pressure, smoking, alcohol consumption, physical activity, depressive symptoms, and socioeconomic status. See Table 3 for statistical details.
Multivariate associations, i.e., all childhood risk categories were inserted simultaneously in the same regression model, between each childhood psychosocial risk category and the IMT measures are presented in Table 3. Higher exposure to stressful life events predicted higher IMT in 2001, worse parental health behavioral predicted higher IMT in 2007, and poorer family socioeconomic environment predicted IMT progression (Base Model: adjusted for age and sex). When adjusted for childhood cardiovascular risk factors, the association between parent health behaviors and IMT in 2007 was slightly attenuated, whereas the association between the family socioeconomic environment and IMT progression did not remain statistically significant (Model 1: adjusted for childhood cardiovascular risk factors). When additionally adjusted for adulthood cardiovascular risks, the association between childhood stressful life events and IMT in 2001 was slightly attenuated, whereas the association between parent health behaviors and IMT in 2007 was significantly diluted (Model 2). Further adjustment for adulthood health behavior did not affect the association between stressful life-events and IMT in 2001 (Model 3.)
Additional analyses
A significant interaction between the cumulative psychosocial risk score and sex in relation to adult IMT in 2001 was found (p=.033). Higher psychosocial risk score predicted higher 2001 IMT in men (b=.003; se=.001; p=.017), but not in women (p=.87). However, a similar interaction was not found in relation to adult IMT in 2007 (p=.14) or to IMT progression (p=.68).
Correlations between individual childhood risk factors, childhood risk categories, childhood cumulative risk score and adulthood IMT measures using non-imputed data are presented in Table S1, Supplemental Digital Content 1. From the individual childhood risk factors, change of school, low educational level and occupational instability had the highest correlations (r > .08) with IMT in 2001 and 2007. Additionally, low occupational level was correlated with higher IMT in 2007. Correlations between psychosocial risk categories were low (r’s range between −.03 and .22), and the correlations between IMT measures were: r=.61 between IMT in 2001 and IMT in 2007, r=−.39 between IMT in 2001 and IMT progression, and r=.48 between IMT in 2007 and IMT progression.
To examine whether the imputation of IMT values in 2007 affected the results, additional analyses were performed using data where imputation for adulthood variables was not used. Results of these analyses are presented in Table S2, Supplemental Digital Content 2, and they are similar in direction and magnitude when compared to results in Table 3.
Discussion
The current study demonstrates that cumulative childhood psychosocial risk factors in youth predict higher IMT and increased IMT progression in adulthood in a sample from general population followed up over 27 years. Whereas some individual categories of psychosocial risk factors were associated with higher IMT and IMT progression, these associations were not consistent over the IMT measurement points, and they were also attenuated after the models were adjusted for adulthood cardiovascular factors and health behaviors. These findings suggest that it might be more informative to consider childhood risk factors cumulatively than individually in predicting IMT and its progression in adulthood.
Current findings are in line with previous suggestion that considering a combination of psychosocial factors provides a better indicator of total psychosocial risk burden than any single risk factor (15), and that exposure to several psychosocial factors may have greater health-impacts than exposure to single factors (15, 17, 34). A recent prospective study presented such a cumulative effect; children who had experienced several psychosocial disadvantages during their childhood had higher metabolic risk 32 years later in adulthood (12). Taken together, these findings suggest that a future focus should be to examine accumulated risk across multiple domains, in addition to concentrating on individual risk factors.
There is a vast amount of literature showing that childhood socioeconomic factors are connected to cardiovascular health in adulthood (24, 35), and specific studies have shown that both childhood and adulthood socioeconomic position are associated with IMT and IMT progression in adulthood (20, 36, 37). In a previous study using the same dataset, the association between childhood SES and IMT in 2001 was not found (9). Here, higher family socioeconomic risk was associated with higher IMT in 2007 and its progression; these associations were attenuated when models were adjusted for other cardiovascular risk factors and health behaviors, which may be in part because these conditions and behaviors both result from childhood socioeconomic risk and increase risk of preclinical atherosclerosis. Thus, these variables may in fact indicate pathways linking psychosocial risk to preclinical atherosclerosis.
There is strong evidence that parental cardiovascular disease is a risk factor for offspring cardiovascular disease (38, 39), and parental history of cardiovascular disease has also been found to be associated with subclinical atherosclerosis (40-42). Prior work has also indicated that parental smoking is associated with increased IMT (43). In fact, parental health behavior most likely reflects both genetic and environmental effects. Most of the observed associations in the current study were attenuated when adulthood cardiovascular risk factors and health behavior were controlled for. This suggests that one pathway from childhood psychosocial risk factors to the development of atherosclerosis might go through adult health behavior (2, 44).
The current study also reported an association between stressful life events and preclinical atherosclerosis was found, however, this result did not replicate at the later time when IMT was measured. Previous studies have shown contradicting evidence on whether life-events may contribute to the development of atherosclerotic diseases. Death of a child has been associated with future myocardial infarction (45), but accumulated life events have not been consistently demonstrated to be associated with heart disease (46). It is possible that more recent stressful life events could have stronger health effects than the distal ones, which may partly explain the current finding.
Whereas it has been hypothesized that childhood emotional environment is a strong predictor of cardiovascular health (13), no association between childhood emotional environment risks and adulthood IMT was found in the current study. There are number of studies that have found connection between childhood adversity and adulthood general cardiovascular health (47). Although, there are limited number of studies that have examined the specific association between childhood adversity and adulthood IMT (48), recently, in a sample of 1402 middle-aged women, retrospectively reported history of childhood sexual abuse was associated with higher IMT (49). Childhood emotional environment has been typically found to highly correlate with SES (13), thus emotional environment might not have independent effects on subclinical atherosclerosis in adulthood.
The effect of cumulative psychosocial risk score on IMT was evident earlier in men than in women. Whereas previous studies using the same data have shown that psychosocial risk factors are typically more strongly associated with IMT among men (19, 50), there is also some evidence that cumulative psychosocial risk factors are stronger predictors of CHD in women (17). Thus, future research should examine in more detail whether psychosocial risk factors are differently associated with preclinical atherosclerosis between men and women.
Current findings may have important clinical significance. It has been shown in older adults that increase of 0.1 mm in common carotid IMT over five years may increase the subsequent risk of coronary events by around 50% (51), and being a smoker has been associated with 0.009 mm progression of IMT over average of 6 years follow-up (7). In the current study, increase of one risk factor in total childhood psychosocial risk score was associated with 0.002 mm increase in IMT. Thus, for example 5 risk factors would turn into 5% increase the risk of coronary events and have the same impact to IMT progression than being a current smoker.
Although this study did not directly test the mechanisms by which childhood adversity might lead to development of atherosclerosis, several plausible mechanisms were implicated. First of all, in the current study, the associations between individual risk categories and IMT and its progression were largely attenuated when the analysis were controlled for adulthood biological risk factors and health behaviors. This suggests that these adult behaviors and conditions may be potential mediating mechanisms. Second, allostatic load, which refers to physiologic wear and tear created by exposure to repeated or chronic stressful experiences, has been proposed to be one of the pathways explaining how exposure to adverse experiences can influence health and alter biological functioning (52, 53). Chronic stress has also been associated with higher food intake (54), which indicates that exposure to adverse psychosocial environment during childhood could lead poorer eating habits later in life. Third, a number of biological mechanisms linking childhood adversity to atherosclerosis have also been suggested. Numerous studies have demonstrated an association between high levels of adversity and higher inflammation (55), suggesting that inflammation is a key process linking early adversity and later cardiovascular health. Exposure to adversity has been also shown to alter hypothalamic-pituitary-adrenal axis function (56), and sympathetic activation (57).
Study limitations
The strength of the current study is its population based sample and longitudinal design with 27-year follow-up. However, the current study naturally also has some limitations. First, the measures of the childhood psychosocial risk categories were formulated in a rather simple way, i.e., continuous factors were dichotomized. It has been shown that dichotomizing continuous variables reduces information – and thus it is not often recommended (58). However, in a recent review on cumulative risk factors, it was concluded that in some cases dichotomizing is the best option to form a cumulative risk score as it is parsimonious, does not make assumptions about the relative strengths of multiple risk factors or their collinearity, and enables testing of cumulative effects (15). Although there are other ways to form risk scores (e.g., factor analytic methods), they are rather complicated and do not necessarily produce more reliable results than the traditional dichotomizing (15).
Secondly, some of the participants were already 18 years old when their parents answered the childhood psychosocial risk questionnaires. Thus, it is possible that their answers reflect, for example, their attitudes toward their teenage children rather than small children. Third, for some of the variables used in the risk score, the cut-offs points could be easily justified, whereas for some variables it was more difficult.
Fourth, our measurement battery did not include assessment of a number of childhood exposures, such as physical, sexual, or emotional abuse, family violence, or drug use. Most of the families that participated in the current study were not ‘risky families’ – but instead they represented the normal range of Finnish families with rather minor differences in child-rearing practices. Our measurement battery might produce misclassification as families with severe abuse or neglect might have been classified as non-risky. Thus, future studies need to examine whether exposure to more adverse child-rearing practices in childhood is associated with future cardiovascular health.
Fifth, due to long follow-up time, over 30% of the original participants were lost. It has been previously shown that this attrition is partly systematic, i.e., participants who dropped out were more often men and younger than those who continued, (21), and in the current study participants lost to follow-up had higher emotional risks than the included participants. Thus, it is possible that some effect sizes were underestimated due to attrition. Last, the large number of analyses may have increased Type 1 error. In addition to false positive findings, this could also produce inconsistencies between different time points.
Conclusions
The current prospective study shows that cumulative childhood psychosocial risks are associated with higher IMT 27-years later and that it may also contribute to 6-year progression of IMT. These results highlight the potential importance of early psychosocial and behavioral factors in the social environment in primary prevention of atherosclerotic diseases.
Supplementary Material
Acknowledgments
Source of Funding:
This work was supported by the Academy of Finland [grants nos. 258578 to M.H., 258711 to L.K-J., 265977 to M.E.]; the Finnish Cultural Foundation to C.H.; the Emil Aaltonen Foundation to M.H.; Signe and Ane Gyllenberg Foundation to L.K-J. and M.H.; Alli Paasikivi Foundation to M.H.; Juho Vainio Foundation to L.P-R.; Research Funds of the University of Helsinki to M.H; the Medical Research Council (K013351) to M.Kivimäki; the Economic and Social Research Council professorial fellowship to M.Kivimäki; and the Medical Research Fund of Tampere University Hospital to N.H-K.
The Young Finns Study has been financially supported by the Academy of Finland: grants 126925, 121584, and 124282, the Social Insurance Institution of Finland, Kuopio, Tampere and Turku University Hospital Medical Funds, Juho Vainio Foundation, Paavo Nurmi Foundation, Finnish Foundation of Cardiovascular Research and Finnish Cultural Foundation, Tampere Tuberculosis Foundation and Emil Aaltonen Foundation.
Acronyms
- IMT
intima-media thickness
- BMI
body mass index
- BDI
Beck Depression Inventory
- LDL
low-density lipoprotein
- SES
socioeconomic status
Footnotes
Conflicts of Interest
No conflicts of interest declared.
References
- 1.Lorenz MW, Markus HS, Bots ML, Rosvall M, Sitzer M. Prediction of clinical cardiovascular events with carotid intima-media thickness a systematic review and meta-analysis. Circulation. 2007;115:459–467. doi: 10.1161/CIRCULATIONAHA.106.628875. [DOI] [PubMed] [Google Scholar]
- 2.Raitakari OT, Juonala M, Kähönen M, Taittonen L, Laitinen T, Mäki-Torkko N, Järvisalo MJ, Uhari M, Jokinen E, Rönnemaa T. Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood. JAMA: the journal of the American Medical Association. 2003;290:2277–2283. doi: 10.1001/jama.290.17.2277. [DOI] [PubMed] [Google Scholar]
- 3.Magnussen CG, Venn A, Thomson R, Juonala M, Srinivasan SR, Viikari JS, Berenson GS, Dwyer T, Raitakari OT. The Association of Pediatric Low-and High-Density Lipoprotein Cholesterol Dyslipidemia Classifications and Change in Dyslipidemia Status With Carotid Intima-Media Thickness in AdulthoodEvidence From the Cardiovascular Risk in Young Finns Study, the Bogalusa Heart Study, and the CDAH (Childhood Determinants of Adult Health) Study. J.Am.Coll.Cardiol. 2009;53:860–869. doi: 10.1016/j.jacc.2008.09.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li S, Chen W, Srinivasan SR, Bond MG, Tang R, Urbina EM, Berenson GS. Childhood cardiovascular risk factors and carotid vascular changes in adulthood. JAMA: the journal of the American Medical Association. 2003;290:2271–2276. doi: 10.1001/jama.290.17.2271. [DOI] [PubMed] [Google Scholar]
- 5.Juonala M, Viikari JS, Kähönen M, Taittonen L, Laitinen T, Hutri-Kähönen N, Lehtimäki T, Jula A, Pietikäinen M, Jokinen E. Life-time risk factors and progression of carotid atherosclerosis in young adults: the Cardiovascular Risk in Young Finns study. Eur.Heart J. 2010;31:1745–1751. doi: 10.1093/eurheartj/ehq141. [DOI] [PubMed] [Google Scholar]
- 6.Koskinen J, Kähönen M, Viikari JS, Taittonen L, Laitinen T, Rönnemaa T, Lehtimäki T, Hutri-Kähönen N, Pietikäinen M, Jokinen E. Conventional Cardiovascular Risk Factors and Metabolic Syndrome in Predicting Carotid Intima-Media Thickness Progression in Young Adults The Cardiovascular Risk in Young Finns Study. Circulation. 2009;120:229–236. doi: 10.1161/CIRCULATIONAHA.108.845065. [DOI] [PubMed] [Google Scholar]
- 7.Johnson HM, Douglas PS, Srinivasan SR, Bond MG, Tang R, Li S, Chen W, Berenson GS, Stein JH. Predictors of carotid intima-media thickness progression in young adults the Bogalusa Heart study. Stroke. 2007;38:900–905. doi: 10.1161/01.STR.0000258003.31194.0a. [DOI] [PubMed] [Google Scholar]
- 8.Miller GE, Chen E, Parker KJ. Psychological stress in childhood and susceptibility to the chronic diseases of aging: moving toward a model of behavioral and biological mechanisms. Psychol.Bull. 2011;137:959. doi: 10.1037/a0024768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kivimäki M, Smith GD, Juonala M, Ferrie JE, Keltikangas-Järvinen L, Elovainio M, Pulkki-Råback L, Vahtera J, Leino M, Viikari JS. Socioeconomic position in childhood and adult cardiovascular risk factors, vascular structure, and function: cardiovascular risk in young Finns study. Heart. 2006;92:474–480. doi: 10.1136/hrt.2005.067108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Poulton R, Caspi A, Milne BJ, Thomson WM, Taylor A, Sears MR, Moffitt TE. Association between children’s experience of socioeconomic disadvantage and adult health: a life-course study. The Lancet. 2002;360:1640–1645. doi: 10.1016/S0140-6736(02)11602-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clark AM, DesMeules M, Luo W, Duncan AS, Wielgosz A. Socioeconomic status and cardiovascular disease: risks and implications for care. Nature Reviews Cardiology. 2009;6:712–722. doi: 10.1038/nrcardio.2009.163. [DOI] [PubMed] [Google Scholar]
- 12.Danese A, Moffitt TE, Harrington H, Milne BJ, Polanczyk G, Pariante CM, Poulton R, Caspi A. Adverse childhood experiences and adult risk factors for age-related disease: depression, inflammation, and clustering of metabolic risk markers. Arch.Pediatr.Adolesc.Med. 2009;163:1135. doi: 10.1001/archpediatrics.2009.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Repetti RL, Taylor SE, Seeman TE. Risky families: Family social environments and the mental and physical health of offspring. Psychol.Bull. 2002;128:330–366. [PubMed] [Google Scholar]
- 14.Korkeila J, Vahtera J, Korkeila K, Kivimaki M, Sumanen M, Koskenvuo K, Koskenvuo M. Childhood adversities as predictors of incident coronary heart disease and cerebrovascular disease. Heart. 2010;96:298–303. doi: 10.1136/hrt.2009.188250. [DOI] [PubMed] [Google Scholar]
- 15.Evans GW, Li D, Sepanski Whipple S. Cumulative Risk and Child Development. Psychological Bulletin. 2013;139:1342–96. doi: 10.1037/a0031808. [DOI] [PubMed] [Google Scholar]
- 16.Troxel WM, Matthews KA, Bromberger JT, Sutton-Tyrrell K. Chronic stress burden, discrimination, and subclinical carotid artery disease in African American and Caucasian women. Health Psychology. 2003;22:300–309. doi: 10.1037/0278-6133.22.3.300. [DOI] [PubMed] [Google Scholar]
- 17.Thurston RC, Kubzansky LD. Multiple sources of psychosocial disadvantage and risk of coronary heart disease. Psychosom.Med. 2007;69:748–755. doi: 10.1097/PSY.0b013e31815772a3. [DOI] [PubMed] [Google Scholar]
- 18.Gilman SE, Rende R, Boergers J, Abrams DB, Buka SL, Clark MA, Colby SM, Hitsman B, Kazura AN, Lipsitt LP, Lloyd-Richardson EE, Rogers ML, Stanton CA, Stroud LR, Niaura RS. Parental smoking and adolescent smoking initiation: an intergenerational perspective on tobacco control. Pediatrics. 2009;123:e274–81. doi: 10.1542/peds.2008-2251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Elovainio M, Keltikangas-Jarvinen L, Kivimaki M, Pulkki L, Puttonen S, Heponiemi T, Juonala M, Viikari JS, Raitakari OT. Depressive symptoms and carotid artery intima-media thickness in young adults: the Cardiovascular Risk in Young Finns Study. Psychosom.Med. 2005;67:561–567. doi: 10.1097/01.psy.0000170340.74035.23. [DOI] [PubMed] [Google Scholar]
- 20.Kestilä P, Magnussen CG, Viikari JS, Kähönen M, Hutri-Kähönen N, Taittonen L, Jula A, Loo B, Pietikäinen M, Jokinen E. Socioeconomic Status, Cardiovascular Risk Factors, and Subclinical Atherosclerosis in Young Adults The Cardiovascular Risk in Young Finns Study. Arterioscler.Thromb.Vasc.Biol. 2012;32:815–821. doi: 10.1161/ATVBAHA.111.241182. [DOI] [PubMed] [Google Scholar]
- 21.Raitakari OT, Juonala M, Rönnemaa T, Keltikangas-Järvinen L, Räsänen L, Pietikäinen M, Hutri-Kähönen N, Taittonen L, Jokinen E, Marniemi J, Jula A, Telama R, Kähonen M, Lehtimäki T, Åkerblom HK, Viikari JS. Cohort profile: the cardiovascular risk in Young Finns Study. Int.J.Epidemiol. 2008;37:1220–1226. doi: 10.1093/ije/dym225. [DOI] [PubMed] [Google Scholar]
- 22.Åkerblom HK, Uhari M, Pesonen E, Dahl M, Kaprio EA, Nuutinen EM, Pietikäinen M, Salo MK, Aromaa A, Kannas L. Cardiovascular Risk in Young Finns. Ann.Med. 1991;23:35–39. doi: 10.3109/07853899109147928. [DOI] [PubMed] [Google Scholar]
- 23.White IR, Royston P, Wood AM. Multiple imputation using chained equations: Issues and guidance for practice. Stat.Med. 2011;30:377–399. doi: 10.1002/sim.4067. [DOI] [PubMed] [Google Scholar]
- 24.Galobardes B, Smith GD, Lynch JW. Systematic review of the influence of childhood socioeconomic circumstances on risk for cardiovascular disease in adulthood. Ann.Epidemiol. 2006;16:91–104. doi: 10.1016/j.annepidem.2005.06.053. [DOI] [PubMed] [Google Scholar]
- 25.Lloyd-Jones D, Hong Y, Labarthe D, Mozaffarian D, Appel L, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli G. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 26.Pulkki-Raback L, Elovainio M, Hakulinen C, Lipsanen J, Hintsanen M, Jokela M, Kubzansky LD, Hintsa T, Serlachius A, Laitinen T, Pahkala K, Mikkila V, Nevalainen J, Hutri-Kahonen N, Juonala M, Viikari J, Raitakari OT, Keltikangas-Jarvinen L. Cumulative effect of psychosocial factors in youth on ideal cardiovascular health in adulthood: the cardiovascular risk in young Finns study. Circulation. 2015;131:245–253. doi: 10.1161/CIRCULATIONAHA.113.007104. [DOI] [PubMed] [Google Scholar]
- 27.Elovainio M, Pulkki-Råback L, Hakulinen C, Ferrie J, Jokela M, Hintsanen M, Hintsa T, Raitakari OT, Keltikangas-Järvinen L. Childhood risk factors and development of depressive symptoms: The 32-year prospective Young Finns follow-up study. Journal of Epidemiology & Community Heath. 2015 doi: 10.1136/jech-2014-205352. [DOI] [PubMed] [Google Scholar]
- 28.Makkonen T, Ruoppila I, Rönkä T, Timonen S, Valvanne L, Österlund K. Operaatio perhe-isä ja synnytys: tutkimus perhesynnytyksestä, vierihoidosta ja esikoisperheen vuorovaikutuksesta (“Operation Family”) Mannerheim League of Child Welfare; Helsinki: 1981. Child Rep. No. A 34 ed. [Google Scholar]
- 29.Hakulinen C, Jokela M, Hintsanen M, Pulkki-Råback L, Hintsa T, Merjonen P, Josefsson K, Kähönen M, Raitakari O, Keltikangas-Järvinen L. Childhood family factors predict developmental trajectories of hostility and anger: a prospective study from childhood into middle adulthood. Psychol.Med. 2013;43:2417–2426. doi: 10.1017/S0033291713000056. [DOI] [PubMed] [Google Scholar]
- 30.Johnson JL, Leff M. Children of substance abusers: Overview of research findings. Pediatrics. 1999;103:1085–1099. [PubMed] [Google Scholar]
- 31.Telama R, Yang X, Viikari J, Välimäki I, Wanne O, Raitakari O. Physical activity from childhood to adulthood: a 21-year tracking study. Am.J.Prev.Med. 2005;28:267–273. doi: 10.1016/j.amepre.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 32.Beck AT, Steer RA. Manual for the Revised Beck Depression Inventory. 1987 [Google Scholar]
- 33.Rosenström T, Jokela M, Puttonen S, Hintsanen M, Pulkki-Råback L, Viikari JS, Raitakari OT, Keltikangas-Järvinen L. Pairwise measures of causal direction in the epidemiology of sleep problems and depression. PloS one. 2012;7:e50841. doi: 10.1371/journal.pone.0050841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bauman LJ, Silver EJ, Stein RE. Cumulative social disadvantage and child health. Pediatrics. 2006;117:1321–1328. doi: 10.1542/peds.2005-1647. [DOI] [PubMed] [Google Scholar]
- 35.Power C, Kuh D, Morton S. From developmental origins of adult disease to life course research on adult disease and aging: insights from birth cohort studies. Public Health. 2013;34:7–28. doi: 10.1146/annurev-publhealth-031912-114423. [DOI] [PubMed] [Google Scholar]
- 36.Lynch J, Kaplan GA, Salonen R, Cohen RD, Salonen JT. Socioeconomic status and carotid atherosclerosis. Circulation. 1995;92:1786–1792. doi: 10.1161/01.cir.92.7.1786. [DOI] [PubMed] [Google Scholar]
- 37.Lamont D, Parker L, White M, Unwin N, Bennett S, Cohen M, Richardson D, Dickinson HO, Adamson A, Alberti K. Risk of cardiovascular disease measured by carotid intima-media thickness at age 49-51: lifecourse study. BMJ. 2000;320:273–278. doi: 10.1136/bmj.320.7230.273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lloyd-Jones DM, Nam B, D’Agostino RB, Sr, Levy D, Murabito JM, Wang TJ, Wilson PW, O’Donnell CJ. Parental cardiovascular disease as a risk factor for cardiovascular disease in middle-aged adults. JAMA: the journal of the American Medical Association. 2004;291:2204–2211. doi: 10.1001/jama.291.18.2204. [DOI] [PubMed] [Google Scholar]
- 39.Chow CK, Islam S, Bautista L, Rumboldt Z, Yusufali A, Xie C, Anand SS, Engert JC, Rangarajan S, Yusuf S. Parental History and Myocardial Infarction Risk Across the WorldThe INTERHEART Study. J.Am.Coll.Cardiol. 2011;57:619–627. doi: 10.1016/j.jacc.2010.07.054. [DOI] [PubMed] [Google Scholar]
- 40.Wang TJ, Nam B, D’Agostino RB, Wolf PA, Lloyd-Jones DM, MacRae CA, Wilson PW, Polak JF, O’Donnell CJ. Carotid Intima-Media Thickness Is Associated With Premature Parental Coronary Heart Disease The Framingham Heart Study. Circulation. 2003;108:572–576. doi: 10.1161/01.CIR.0000081764.35431.DE. [DOI] [PubMed] [Google Scholar]
- 41.Juonala M, Viikari JS, Räsänen L, Helenius H, Pietikäinen M, Raitakari OT. Young Adults With Family History of Coronary Heart Disease Have Increased Arterial Vulnerability to Metabolic Risk Factors The Cardiovascular Risk in Young Finns Study. Arterioscler.Thromb.Vasc.Biol. 2006;26:1376–1382. doi: 10.1161/01.ATV.0000222012.56447.00. [DOI] [PubMed] [Google Scholar]
- 42.Zureik M, Touboul P, Bonithon-Kopp C, Courbon D, Ruelland I, Ducimetière P. Differential association of common carotid intima-media thickness and carotid atherosclerotic plaques with parental history of premature death from coronary heart disease the EVA Study. Arterioscler.Thromb.Vasc.Biol. 1999;19:366–371. doi: 10.1161/01.atv.19.2.366. [DOI] [PubMed] [Google Scholar]
- 43.Gall S, Huynh QL, Magnussen CG, Juonala M, Viikari JS, Kahonen M, Dwyer T, Raitakari OT, Venn A. Exposure to parental smoking in childhood or adolescence is associated with increased carotid intima-media thickness in young adults: evidence from the Cardiovascular Risk in Young Finns study and the Childhood Determinants of Adult Health Study. Eur.Heart J. 2014;35:2484–2491. doi: 10.1093/eurheartj/ehu049. [DOI] [PubMed] [Google Scholar]
- 44.Juonala M, Viikari JS, Kähönen M, Laitinen T, Taittonen L, Loo B, Jula A, Marniemi J, Räsänen L, Rönnemaa T. Alcohol consumption is directly associated with carotid intima–media thickness in Finnish young adults: The Cardiovascular Risk in Young Finns Study. Atherosclerosis. 2009;204:e93–e98. doi: 10.1016/j.atherosclerosis.2008.11.021. [DOI] [PubMed] [Google Scholar]
- 45.Li J, Hansen D, Mortensen PB, Olsen J. Myocardial Infarction in Parents Who Lost a Child A Nationwide Prospective Cohort Study in Denmark. Circulation. 2002;106:1634–1639. doi: 10.1161/01.cir.0000031569.45667.58. [DOI] [PubMed] [Google Scholar]
- 46.Andersen I, Diderichsen F, Kornerup H, Prescott E, Rod NH. Major life events and the risk of ischaemic heart disease: does accumulation increase the risk? Int.J.Epidemiol. 2011;40:904–913. doi: 10.1093/ije/dyr052. [DOI] [PubMed] [Google Scholar]
- 47.Loucks EB, Almeida ND, Taylor SE, Matthews KA. Childhood family psychosocial environment and coronary heart disease risk. Psychosom.Med. 2011;73:563–571. doi: 10.1097/PSY.0b013e318228c820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Low CA, Salomon K, Matthews KA. Chronic life stress, cardiovascular reactivity, and subclinical cardiovascular disease in adolescents. Psychosom.Med. 2009;71:927–931. doi: 10.1097/PSY.0b013e3181ba18ed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Thurston RC, Chang Y, Derby CA, Bromberger JT, Harlow SD, Janssen I, Matthews KA. Abuse and subclinical cardiovascular disease among midlife women: the study of women’s health across the nation. Stroke. 2014;45:2246–2251. doi: 10.1161/STROKEAHA.114.005928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hintsanen M, Kivimäki M, Elovainio M, Pulkki-Råback L, Keskivaara P, Juonala M, Raitakari OT, Keltikangas-Järvinen L. Job strain and early atherosclerosis: the Cardiovascular Risk in Young Finns Study. Psychosom.Med. 2005;67:740–747. doi: 10.1097/01.psy.0000181271.04169.93. [DOI] [PubMed] [Google Scholar]
- 51.Chambless LE, Heiss G, Folsom AR, Rosamond W, Szklo M, Sharrett AR, Clegg LX. Association of coronary heart disease incidence with carotid arterial wall thickness and major risk factors: the Atherosclerosis Risk in Communities (ARIC) Study, 1987-1993. Am.J.Epidemiol. 1997;146:483–494. doi: 10.1093/oxfordjournals.aje.a009302. [DOI] [PubMed] [Google Scholar]
- 52.McEwen BS, Stellar E. Stress and the individual. Mechanisms leading to disease. Arch.Intern.Med. 1993;153:2093–2101. [PubMed] [Google Scholar]
- 53.Danese A, McEwen BS. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiol.Behav. 2012;106:29–39. doi: 10.1016/j.physbeh.2011.08.019. [DOI] [PubMed] [Google Scholar]
- 54.Adam TC, Epel ES. Stress, eating and the reward system. Physiol.Behav. 2007;91:449–458. doi: 10.1016/j.physbeh.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 55.Miller G. Health psychology: Developing biologically plausible models linking the social world and physical health. Annu.Rev.Psychol. 2009;60:501–524. doi: 10.1146/annurev.psych.60.110707.163551. [DOI] [PubMed] [Google Scholar]
- 56.Heim C, Newport DJ, Heit S, Graham YP, Wilcox M, Bonsall R, Miller AH, Nemeroff CB. Pituitary-adrenal and autonomic responses to stress in women after sexual and physical abuse in childhood. JAMA. 2000;284:592–597. doi: 10.1001/jama.284.5.592. [DOI] [PubMed] [Google Scholar]
- 57.Gunnar M, Quevedo K. The neurobiology of stress and development. Annu.Rev.Psychol. 2007;58:145–173. doi: 10.1146/annurev.psych.58.110405.085605. [DOI] [PubMed] [Google Scholar]
- 58.MacCallum RC, Zhang S, Preacher KJ, Rucker DD. On the practice of dichotomization of quantitative variables. Psychol.Methods. 2002;7:19–40. doi: 10.1037/1082-989x.7.1.19. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.