Abstract
Objective
Major lower extremity amputation is a common procedure that results in a profound change in a patient's life. We sought to determine the association between social support and outcomes after amputation. We hypothesized that patients with greater social support will have better post amputation outcomes.
Methods
From November 2011 to May 2013, we conducted a cross-sectional, observational, multicenter study. Social integration was measured by the social integration subset of the Short Form (Craig Handicap Assessment and Reporting Technique (CHART). Systemic social support was assessed by comparing a US and Tanzanian population. Walking function was measured using the 6MWT and quality of life (QoL) was measured using the EQ-5D.
Results
102 major lower extremity amputees were recruited. 63 patients were enrolled in the US with a mean age of 58.0. Forty-two (67%) were male. Patients with low social integration were more likely to be unable to ambulate (no walk 39% vs. slow walk 23% vs. fast walk 10%; P=.01) and those with high social integration were more likely to be fast walkers (no walk 10% vs. slow walk 59% vs. fast walk 74%; P=.01). This relationship persisted in a multivariable analysis. Increasing social integration scores were also positively associated with increasing quality of life scores in a multivariable analysis (β .002; SE .0008; P = .02). In comparing the US population with the Tanzanian cohort (39 subjects), there were no significant differences between functional or quality of life outcomes in the systemic social support analysis.
Conclusions
In the US population, increased social integration is associated with both improved function and quality of life outcomes among major lower extremity amputees. Systemic social support, as measured by comparing the US population with a Tanzanian population, was not associated with improved function or quality of life outcomes. In the US, steps should be taken to identify and aid amputees with poor social integration.
Introduction
Amputation due to dysvascular disease (diabetes and peripheral vascular disease (PVD)) accounts for the majority (82%) of amputation in the United States and the incidence is expected to rise with increasing rates of PVD and diabetes.1 In the year 2005, 1.6 million persons were living with the loss of a limb and it is projected this number will more than double by the year 2050 to 3.6 million.2 Major lower extremity (MLE) amputation results in extensive morbidity, including impaired function and decreased quality of life (QoL).3,4 These in turn lead to an increase in resource utilization.5
Among many surgeons, amputation is considered to be the end point of treatment. But life does go on for these patients. While much research is dedicated to preventing limb loss, amputations will continue to occur and patients will continue to need care. Besides an ethical obligation to care for these patients, improving outcomes is a necessity as our health care system shifts to population management and “pay for performance” structures.6 The ability to quantify the effect of a social support system can both help to risk-adjust patients to better align physician compensation with outcomes as well as help policy makers allocate limited healthcare resources more effectively.
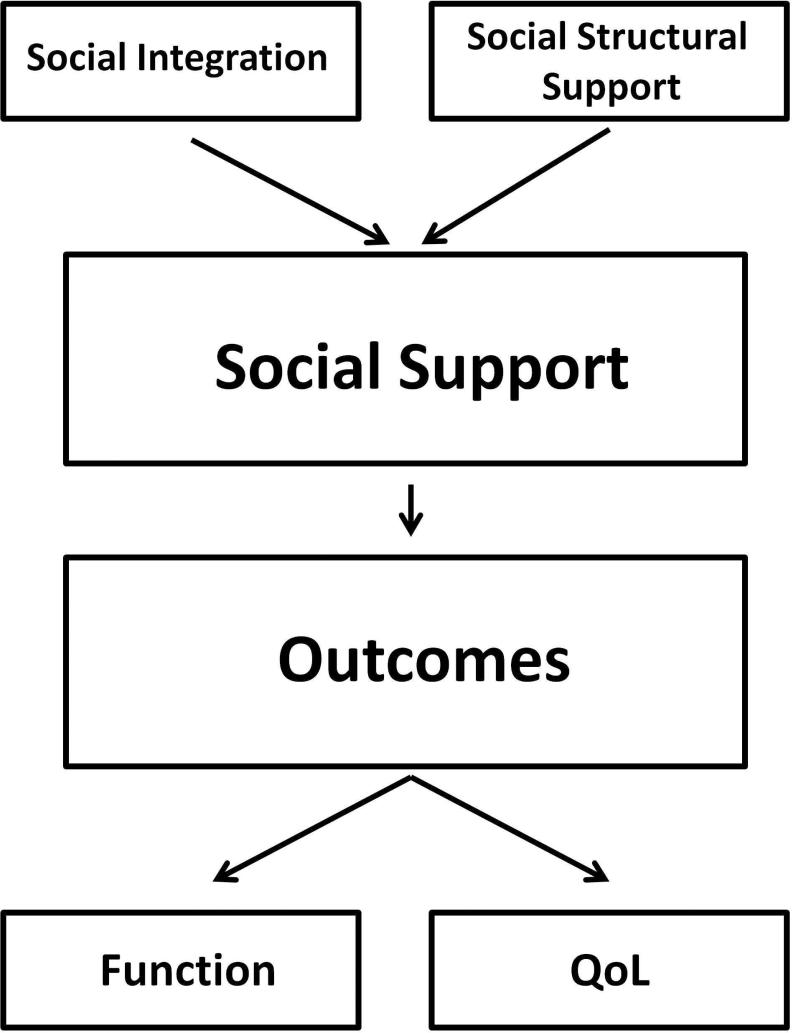
The link between social support and health outcomes has been well described.7-13 This study conceptualizes social support into two different elements: social integration and systemic social support (Figure 1). Social integration is defined as an objective state relating to the number of contacts and interaction between persons and their wider social network. Low levels of social integration has been linked to a number of negative health outcomes.7-13 Systemic social support is the support provided by a society to patients with impairment and handicap. This includes policy set by local and federal government, such as the Americans with Disabilities Act, and the attitudes of society at large to patients with disability.
Figure 1.
Relationship between Social Support and Outcomes.
The purpose of this study was to evaluate the effect of both social integration and systemic social support on functional and quality of life outcomes after MLE amputation. The authors hypothesize that MLE amputees with higher levels of social integration and systemic social support will have better function and improved QoL.
Materials and Methods
Patient Population
Following institutional review by the Partners Institutional Review Board (Protocol 2011-P-001913/4), 63 patients were enrolled from both the Brigham and Women's Vascular Surgery Clinic and the Spaulding Rehabilitation Hospital Outpatient Amputee Clinic between November 2011 to May 2013. Selection criteria included MLE amputation (ankle or above), age ≥ 18 and greater than 60 days out from the amputation. Patients with bilateral MLE amputations, an active stump problem or acute vascular disease were excluded from the study. Active stump problem was defined as any infection, wound or pain that interferes with ambulation with a prosthesis. Acute vascular disease was defined as any critical limb ischemia (non healing wound, gangrene, or rest pain). Informed consent was obtained from all patients.
Demographic information and medical history were collected. Race was self reported by subjects. Patients who had their amputation for either oncologic or congenital reasons were classified as “other”. Study data were collected and managed using REDCap (Research Electronic Data Capture) electronic data capture tools hosted at Partners Healthcare.14
Outcomes
Two outcomes were assessed - function and QoL. To assess function, the Six Minute Walk test (6MWT) was used.15 The 6MWT measures the distance a patient can ambulate in six minutes. The 6MWT has proven reliability and is well validated in the MLE amputee population.16 For analysis, three groups were formed: patients unable to walk, slow walkers and fast walkers. Slow and fast walkers were defined by walk distance in relation to the median 6MWT distance. Once subjects who were unable to walk had been taken out of the cohort, subjects that fell below the median 6MWT were considered slow walkers and patients above the median were considered fast walkers. As the 6MWT is sensitive to other comorbidities that can limit walking (stroke, COPD, etc), co-morbidity variables were collected. QoL was assessed using the EQ5D.17 The EQ-5D is a brief but reliable and valid test of QoL that generates health scores from 0-1, with lower scores indicating a lower QoL.
Social Integration
To operationalize social integration, the social integration subset of the Short Form Craig Handicap Assessment and Reporting Technique (CHART) was used.18 The CHART is a reliable test and has been validated in an amputee population.19 Scores are reported on a scale of 0-100 with lower scores indicating a lower level of social integration. For analysis, three categories of social integration were created: high, medium and low. As there was a significant ceiling effect in the results of the CHART, high social integration was defined as a perfect score of 100, medium and low social integration was determined based on the median social integration score for those subjects without perfect scores.
Systemic Social Support
The second goal of this study was to determine the association between systemic social support and outcomes after MLE amputation. To achieve this, the Boston population was compared with a Tanzanian cohort. Tanzania is an East African country that has recently undertaken a greater commitment to rights of the disabled, but has yet to demonstrate a meaningful change in the lives of people with disabilities.20 In addition, it lacks both the access and resources of the US health care system as well as legal protection such as the Americans with Disabilities Act. For the purpose of this study, we operationalized systemic social support at the country level, with the Boston population defined as having a “high” level of systemic social support and the Tanzanian population having a “low” level of systemic social support. The Kilimanjaro Christian Medical Center Ethics Board separately approved the project. Surveys and consents were translated into Swahili. As different cultures view health differently, a separate algorithm was used to derive health outcomes from the EQ-5D based on a sub-Saharan population.21
Statistical Analysis
Comparison of continuous variables was made using the Student t-test and ANOVA and categorical variables were compared with the Fisher's exact test and either the Cochran-Armitage Test for Trend or the Chi-square test as appropriate. For comparisons with more than two levels, within group differences were analyzed. In the multivariable analysis of the effect of social integration on function, a multivariable polytomous logistic regression model was used as there were three separate outcomes (no walk, slow walk, and fast walk). Due to the relatively low number of observations, only age and gender were included in the model along with social integration. For multivariable analysis of the effect of social integration on quality of life, a linear regression model was derived. All of the risk factors were considered for inclusion via bivariate linear regression and were included in the multivariable model if the p value was significant (p < .05). Similar methods were used to analyze the effect of systemic social support on both functional and quality of life outcomes. SAS statistical software (version 9.2; SAS Institutes Inc., Cary, NC, USA) was used for all analysis. All tests were two-sided with an alpha level of 0.05.
Results
Social Integration
Demographic
From November 2011 to May 2013, sixty-three patients were enrolled in the Boston cohort. Characteristics for the study population are summarized in Table I. The mean age was 58.0 years (range 21.9-92.7) and 42 (67%) of the group were male. There was a high incidence of comorbidities as 32 subjects had diabetes (51%), 11 (17%) had a history of cerebrovascular accident (CVA) and 5 (8%) had chronic obstructive pulmonary disease (COPD). Thirty-six patients (57%) had their amputations for dysvascular disease, which includes both PVD and diabetes. Finally, 49 (78%) had a below the knee amputation (BKA) with the balance having either an above the knee amputation (AKA) or a knee disarticulation. Distribution of variables among categories of social integration was mostly equal, with the exceptions being diabetes (Low: 10/13 (77%) vs. High: 14/37 (38%); P=.03), CVA (Low: 6/13 (46%) vs. High: 4/37 (11%); P=.01), and private insurance status (Low: 1/13 (8%) vs. High: 17/37 (46%); P=.04).
Table I.
Patient Demographics and Select Comorbidities both Overall and by Distribution of Social Integration Levels.
| All (n=63) | Low (n=13) | Social Integration Medium (n=13) | High (n=37) | P | |
|---|---|---|---|---|---|
| Age, mean (range), years | 58.0 (21.9-92.7) | 68.5 (52.2-92.7) | 60.0 (26.8-79.0) | 53.5 (21.9-81.8) | .009 |
| Gender | .45 | ||||
| Male | 42/63 (67) | 7/13 (53) | 10/13 (77) | 25/37 (68) | |
| Female | 21/63 (33) | 6/13 (46) | 3/13 (23) | 12/37 (32) | |
| Race | .70 | ||||
| Caucasian | 47/63 (75) | 10/13 (77) | 11/13 (85) | 26/37 (70) | |
| Black | 10/63 (16) | 2/13 (15) | 2/13 (15) | 6/37 (16) | |
| Other | 6/63 (9) | 1/13 (8) | 0/13 (0) | 5/37 (13) | |
| Obese (BMI > 30) | 14/63 (22) | 3/13 (21) | 2/13 (21) | 9/37 (24) | .79 |
| Comorbidities | |||||
| Smoke | 11/63 (17) | 2/13 (15) | 2/13 (15) | 7/37 (19) | .94 |
| Diabetes | 32/63 (51) | 10/13 (77) | 8/13 (61) | 14/37 (38) | .03 |
| CVA | 11/63 (17) | 6/13 (46) | 1/13 (8) | 4/37 (11) | .01 |
| COPD | 5/63 (8) | 2/13 (15) | 0/13 (0) | 3/37 (8) | .35 |
| Etiology | .04 | ||||
| Dysvascular | 36/63 (57) | 12/13 (92) | 8/13 (61) | 16/37 (43) | |
| Trauma | 18/63 (29) | 1/13 (8) | 4/13 (31) | 13/37 (35) | |
| Other | 9/63 (14) | 0/13 (0) | 1/13 (8) | 8/37 (22) | |
| Type | .28 | ||||
| BKA | 49/63 (78) | 11/13 (85) | 8/13 (61) | 30/37 (81) | |
| Knee/AKA | 14/63 (22) | 2/13 (15) | 5/13 (38) | 7/37 (19) | |
| Pre-operative Ambulatory Status | .65 | ||||
| Ambulatory | 54/61 (88) | 10/12 (83) | 11/13 (85) | 33/36 (92) | |
| Non-ambulatory | 7/61 (11) | 2/12 (17) | 2/13 (15) | 3/36 (8) | |
| Time from Amputation | .43 | ||||
| 3-12 mo | 21/63 (33) | 6/13 (46) | 5/13 (38) | 10/37 (27) | |
| 1-4 y | 19/63 (30) | 4/13 (31) | 5/13 (38) | 10/37 (27) | |
| > 5 y | 23/63 (36) | 3/13 (23) | 3/13 (23) | 17/37 (46) | |
| Employment | .09 | ||||
| Working | 11/63 (17) | 0/13 (0) | 1/13 (8) | 10/37 (27) | |
| Unemployed | 5/63 (8) | 3/13 (23) | 0/10 (0) | 2/37 (5) | |
| Retired | 21/63 (33) | 5/13 (38) | 5/13 (38) | 11/37 (30) | |
| On Disability | 26/63 (41) | 5/13 (38) | 7/13 (54) | 14/37 (38) | |
| Insurance (footnote) | .04 | ||||
| Private | 23/63 (36) | 1/13 (8) | 5/13 (38) | 17/37 (46) | |
| State | 40/63 (63) | 12/13 (92) | 8/13 (61) | 20/37 (54) | |
| Graduated High School | 53/63 (84) | 10/13 (77) | 10/13 (77) | 33/37 (89) | .42 |
| Marital Status | .14 | ||||
| Married | 26/63 (41) | 3/13 (23) | 4/13 (31) | 19/37 (51) | |
| Single | 37/63 (59) | 10/13 (77) | 9/13 (69) | 18/37 (49) |
P values are from the Chi-square test, except for age which is from a ANOVA.
BMI Body Mass Index; COPD Chronic Obstructive Pulmonary Disease; CVA Cerebral Vascular Accident; BKA Below the Knee Amputation; AKA Above the Knee Amputation.
Function
In the unadjusted analysis, there was a significant association between social integration and 6MWT results (Table II). Those with low social integration were more likely to be unable to ambulate (no walk 50% vs. slow walk 40% vs. fast walk 10%) and those with high social integration were more likely to be fast walkers (no walk 10% vs. slow walk 59% vs. fast walk 74%; P=.01). There was also decreased ambulatory function among older patients, females, obese subjects, diabetics, subjects with a history of CVA, subjects with a dysvascular etiology for their amputation, subjects with an AKA or knee disarticulation, subjects who had their amputations for less time, subjects without private insurance and subjects who did not graduate high school.
Table II.
Functional outcomes for MLE Amputees by Performance on the Six Minute Walk Test (6MWT).
| 6MWT | ||||
|---|---|---|---|---|
| No walk (n=10) | Slow (n=22) | Fast (n=31) | P | |
| Social Integration | .01 | |||
| Low | 5/10 (50) | 5/22 (23) | 3/31 (10) | |
| Medium | 4/10 (40) | 4/22 (18) | 5/31 (16) | |
| High | 1/10 (10) | 13/22 (59) | 23/31 (74) | |
| Age | .03 | |||
| <45 | 0/10 (0) | 3/13 (35) | 11/31 (35) | |
| 45-65 | 3/10 (30) | 10/22 (4) | 13/31 (42) | |
| > 65 | 7/10 (70) | 9/22 (41) | 7/31 (23) | |
| Gender | .004 | |||
| Male | 4/10 (40) | 12/22 (54) | 26/31 (84) | |
| Female | 6/10 (60) | 10/22 (45) | 5/31 (16) | |
| Race | .64 | |||
| Caucasian | 7/10 (70) | 16/22 (73) | 24/31 (77) | |
| Black | 2/10 (20) | 5/22 (23) | 3/31 (10) | |
| Other | 1/10 (10) | 1/22 (4) | 4/31 (13) | |
| Obese (BMI > 30) | 3/10 (30) | 8/22 (36) | 3/31 (10) | .06 |
| Comorbidities | ||||
| Smoke | 4/10 (40) | 2/22 (9) | 5/31 (16) | .22 |
| Diabetes | 8/10 (80) | 13/22 (59) | 11/31 (35) | .008 |
| CVA | 4/10 (40) | 6/22 (27) | 1/31 (3) | .003 |
| COPD | 1/10 (10) | 3/13 (35) | 1/31 (3) | .29 |
| Etiology | .01 | |||
| Dysvascular | 10/10 (100) | 14/22 (64) | 12/33 (39) | |
| Trauma | 0/10 (0) | 4/22 (18) | 14/33 (45) | |
| Other | 0/10 (0) | 4/22 (18) | 5/31 (16) | |
| Type | .01 | |||
| BKA | 5/10 (50) | 17/22 (77) | 27/31 (87) | |
| Knee/AKA | 5/10 (50) | 5/22 (23) | 4/31 (13) | |
| Pre-operative Ambulatory Status | .35 | |||
| Ambulatory | 7/8 (87) | 18/22 (82) | 29/31 (93) | |
| Non-ambulatory | 1/8 (12) | 4/22 (18) | 2/31 (6) | |
| Time from Amputation | .03 | |||
| 3-12 mo | 5/10 (50) | 10/22 (45) | 6/31 (19) | |
| 1-4 y | 4/10 (40) | 2/22 (9) | 13/31 (42) | |
| > 5 y | 1/10 (10) | 10/22 (45) | 12/33 (39) | |
| Employment | .11 | |||
| Working | 0/10 (0) | 2/22 (9) | 9/31 (29) | |
| Unemployed | 0/10 (0) | 2/22 (9) | 3/31 (10) | |
| Retired | 6/10 (60) | 9/22 (41) | 6/31 (19) | |
| On Disability | 4/10 (40) | 9/22 (41) | 13/31 (42) | |
| Insurance (footnote) | .009 | |||
| Private | 1/10 (10) | 6/22 (27) | 16/31 (52) | |
| State | 9/10 (90) | 16/22 (73) | 15/31 (48) | |
| Graduated High School | 5/10 (50) | 20/22 (91) | 28/31 (90) | .01 |
| Marital Status | .13 | |||
| Married | 3/10 (30) | 7/22 (32) | 16/31 (52) | |
| Single | 7/10 (70) | 15/22 (68) | 15/31 (48) | |
P values are from the Cochran-Armitage Trend Test for variables with two categories and the Chi-square test for variables with three or more categories.
BMI Body Mass Index; COPD Chronic Obstructive Pulmonary Disease; CVA Cerebral Vascular Accident; BKA Below the Knee Amputation; AKA Above the Knee Amputation.
In the multivariable polytomous logistic regression model for function, adjusting for age and gender, patients with high social integration were more likely to be slow walkers (OR 13.72; 95% CI 1.13-166.10) and fast walkers (OR 44.62; 95% CI 2.82-705.2) (Table III) than those with low social integration scores.
Table III.
Multivariable polytomous logistic regression model predicting category of Six Minute Walk Test (6MWT).
| Six Minute Walk Test (Unable to walk is referent group) | ||
|---|---|---|
| Slow |
Fast |
|
| Characteristic | OR (95% CI) | OR (95% CI) |
| Social Integration | ||
| Low | 1.00 (referent) | 1.00 (referent) |
| Medium | 0.64 (0.08-4.94) | 1.06 (0.11-10.67) |
| High | 13.72 (1.13-166.1) | 44.62 (2.82-705.2) |
| Age ≤ 65 | 3.53 (0.58-21.47) | 7.36 (1.07-50.58) |
| Male | 3.02 (0.47-19.31) | 14.13 (1.78-112.1) |
Quality of Life
In the unadjusted analysis, increasing social integration scores were positively associated with increasing quality of life scores (β .003; SE .0008; P < .001) (Table IV). Other associations with increased quality of life include female gender (β .18; SE .05; P = .001), having a BKA versus a higher amputation (β .16; SE .06; P = .01), and having graduated high school (β .18; SE .07; P = .01). Having diabetes was associated with a decrease in QoL (β -.12; SE .05; P = .03). This relationship persisted in the multivariable model, with increasing social integration scores being positively associated with increasing QoL scores (β .002; SE .0008; P = .02).
Table IV.
Unadjusted and Risk-adjusted Linear Regression Coefficients for Eq5D Score for Selected Variables. (R2= .48)
| Unadjusted | Multivariable | |||
|---|---|---|---|---|
| β (SE) | P | β (SE) | P | |
| Social Integration | 0.003 (0.0008) | < .001 | 0.002 (0.0008) | .02 |
| Age | −0.003 (0.001) | .07 | 0.0003 (0.002) | .84 |
| Gender | 0.18 (0.05) | .001 | 0.17 (0.05) | < .001 |
| Race | ||||
| Caucasian | REF | |||
| Black | −0.15 (0.07) | .04 | ||
| Other | −0.06 (0.09) | .51 | ||
| Obese (BMI > 30) | −.03 (.07) | .67 | ||
| Comorbidities | ||||
| Smoke | .01 (.04) | .87 | ||
| Diabetes | −0.12 (0.05) | .03 | −0.11 (0.05) | .02 |
| CVA | −0.04 (0.08) | .54 | ||
| COPD | −0.04 (0.10) | .68 | ||
| Etiology | ||||
| Dysvascular | REF | |||
| Trauma | 0.10 (0.06) | .11 | ||
| Other | 0.08 (0.08) | .29 | ||
| BKA vs AKA/Knee | 0.16 (0.06) | .01 | 0.17 (0.05) | .01 |
| Pre-operative Ambulatory Status | 0.14 (0.08) | .07 | ||
| Time from Amputation | ||||
| 3-12 mos | REF | |||
| 1-4 years | −0.10 (0.07) | .14 | ||
| > 5 years | 0.08 (0.06) | .21 | ||
| Employment | ||||
| Working | REF | |||
| Unemployed | −0.12 (0.11) | .31 | ||
| Retired | −0.12 (0.08) | .13 | ||
| On Disability | −0.17 (0.07) | .03 | ||
| Insurance (footnote) | −0.10 (0.06) | .07 | ||
| Graduated High School | 0.18 (0.07) | .01 | 0.10 (0.06) | .10 |
| Married | 0.07 (0.05) | .24 | ||
BMI Body Mass Index; COPD Chronic Obstructive Pulmonary Disease; CVA Cerebral Vascular Accident; BKA Below the Knee Amputation; AKA Above the Knee Amputation.
Systemic Social Support
Demographic
For the systemic social support analysis, we compared a population with perceived high systemic social support (Boston, United States) with a low systemic social support population (Moshi, Tanzania). Thirty-nine patients were recruited from the general and orthopedic surgery clinics at the Kilimanjaro Christian Medical Center in Moshi, Tanzania. In comparing the Boston cohort with the Tanzanian cohort, there were clear differences between the two populations (Table V). The Tanzanian cohort was overall healthier, having lower incidence of obesity, diabetes, stroke, and COPD. The Tanzanian group also had trauma as their main etiology of amputation and had a higher rate of knee or AKA amputation.
Table V.
Patient Demographics, Select Comorbidities, and Functional Outcome by Site.
| Boston (n=63) | Tanzania (n=39) | P | |
|---|---|---|---|
| Age, mean (range), years | 58.0 (21.9-92.7) | 43.4 (18.2-80.1) | <.001 |
| Gender | .79 | ||
| Male | 42/63 (67) | 25/39 (64) | |
| Female | 21/63 (33) | 14/39 (36) | |
| Obese (BMI > 30) | 14/63 (22) | 1/39 (3) | .006 |
| Comorbidities | |||
| Smoke | 11/63 (17) | 3/39 (8) | .16 |
| Diabetes | 32/63 (59) | 8/39 (20) | .002 |
| CVA | 11/63 (17) | 0/39 (0) | .006 |
| COPD | 5/63 (8) | 0/39 (0) | .07 |
| Etiology | .001 | ||
| Dysvascular | 36/63 (57) | 8/39 (20) | |
| Trauma | 18/63 (29) | 23/39 (59) | |
| Other | 9/63 (14) | 8/39 (20) | |
| Type | .04 | ||
| BKA | 49/63 (78) | 23/39 (59) | |
| Knee/AKA | 14/63 (22) | 16/39 (41) | |
| Pre-operative Ambulatory Status | .003 | ||
| Ambulatory | 54/61 (88) | 25/39 (64) | |
| Non-ambulatory | 7/61 (11) | 14/39 (36) | |
| Time from Amputation | .37 | ||
| 3-12 mos | 21/63 (33) | 8/39 (20) | |
| 1-4 years | 19/63 (30) | 14/39 (36) | |
| > 5 years | 23/63 (36) | 17/39 (44) | |
| Graduated High School | 53/63 (84) | 23/39 (59) | .004 |
| Marital Status | |||
| Married | 26/63 (41) | 26/39 (67) | .01 |
| Single | 37/63 (59) | 13/39 (33) | |
| Social Integration, median (IQR) | 100 (64-100) | 100 (61-100) | .93 |
| 6MWT | .35 | ||
| No Walk | 10/63 (16) | 3/39 (8) | |
| Slow Walk | 22/63 (35) | 12/39 (31) | |
| Fast Walk | 31/63 (49) | 24/39 (61) |
P values are from the Chi-square test, except for age which is from a t-test.
BMI Body Mass Index; COPD Chronic Obstructive Pulmonary Disease; CVA Cerebral Vascular Accident; BKA Below the Knee Amputation; AKA Above the Knee Amputation; 6MWT Six Minute Walk Test.
Function
There was no significant difference in functional outcome (Table V) between the two populations (Fast Walkers: Boston 49% vs. Tanzania 61%: P=.35). A multivariable analysis was not conducted, as there was no difference between the two groups in the bivariate analysis.
Quality of Life
In the bivariate analysis, the Boston cohort was associated with lower QoL score when compared to the Tanzanian cohort (β -.08; SE .04; P = .03). However, this did not persist in the multivariable analysis.
Discussion
Amputation results in a profound change in a patient's life. The patient's environment has a strong influence on how they will adapt to the new situation. This study demonstrates that patients who have higher levels of social integration are more likely to have better functional and QoL outcomes. In a multivariable model, patients with high levels of social integration had 44 times the odds of having high scores on the 6MWT as patients with low level of social integration. Similarly, increasing social integration scores were positively associated with increasing quality of life scores. There was no association identified between systemic social support and post amputation outcomes.
Improving outcomes after lower extremity amputation is a multifactorial process. Many different features have been identified as impacting how amputees adapt to life after their amputations. These include specialized rehabilitation,22,23 age, comorbidities,24,25 level of amputation, 26 employment status and use of a prosthesis.3 In terms of the role social factors play, data are mixed. Helm et al and Nissen et al did not find a relationship between the amputee's social situation and his and her functional results.27,28 Schoppen et al looked at 46 patients over the age of 60 who underwent unilateral lower extremity amputations and found no association in functional scores between either having a living partner or receiving higher scores on a social support questionnaire (SSL12-I).29 Williams et al studied 89 patients over two years and found that higher scores on a questionnaire of perceived social support (MSPSS) predicted life satisfaction and mobility.30 Scores also predicted mobility and occupational functioning six months post amputation, but outcomes were assessed via a phone interview rather than directly measured. This study adds to this literature in that it links social integration to directly measured outcomes of quality of life and function.
There are a number of reasons why outcomes may be superior in patients with higher levels of social integration. A number of prospective studies in the literature document the significant association between social relationships and all-cause and disease-specific morbidity and mortality.8,9 In particular, epidemiologic data suggest that people who have larger and more integrated social networks are at reduced risk for depression31, ischemic heart disease10 and stroke11 and have better prognoses following myocardial infarction13 as compared to their more socially isolated counterparts. In patients with end stage renal disease on dialysis, perceiving a discrepancy between expected and received social support was associated with increased mortality. Social companionship, daily emotional support and total support were all associated with decreased mortality.12 House describes three theories to explain the link between social isolation and inferior outcomes.7 First, isolation from others is anxiety provoking and stressful in and of itself and can produce physiologic arousal and changes.32-34 Second, social relationships beneficially affect health because of the social control that others exercise over a person, especially by encouraging health-promoting behaviors such as adequate sleep, diet, exercise, and compliance with medical regimes or by discouraging health damaging behavior such as smoking, excessive eating, alcohol consumption or drug abuse.8,35 It stands to reason that the social network must be a positive one as some social interactions can instead support poor behavior. Finally, there is the theory that social ties link people with diffuse social networks that facilitate access to a wide range of resources supportive of health, such as medical referral networks, access to peer visitation and support groups, life skills training and education, or opportunities to acquire needed resources.
Understanding the role that social integration plays in outcomes after MLE can guide future intervention. Should this study's preliminary data be confirmed with further, prospective study, patients at risk for low social integration should be identified early, even preoperatively. Table I indicates unequal distribution of a number of factors between social integration groups. We demonstrate that patients with diabetes, history of stroke, dysvascular etiology for their amputation and public insurance are associated with low levels of social integration. Interventions aimed at increasing social integration might be helpful if implemented in the acute tertiary hospital, rehabilitation facility and outpatient settings.36 These patients should also have closer clinical follow up to make sure their function improves as it should. Telephone based counseling has also been shown to improve coping skills and community integration.37 Changes need to be seen on the policy level as well, with more coordination and allocation of resources to those with low social integration. Expansion of the Family and Medical Leave Act could guarantee more long-term assistance. Finally, the authors hope to call attention to the need for further research into outcomes following amputation to ensure that this unique and important population receives the best care possible.
This study is not without limitations and the conclusions drawn must take them into account. This was not a longitudinal study and baseline levels of social integration or function were not recorded. This calls into question whether it is low social integration that causes poor outcomes, or if it is the poor outcomes themselves that lead to social isolation. Nevertheless, the observed association between the two suggests that the healthcare system need to address social integration. While this study identifies a number of associations at the bivariate level, the sample size did not allow for detailed risk stratification via a large multivariable analysis. As patients were recruited from outpatient clinics, there is potential for selection bias, which affects the generalizability of the study. Not included in the study are patients who do not follow up after their amputation. However, these patients would be more likely to have low social integration and their inclusion would only strengthen the findings. Finally, the 6MWT does not accurately measure true mobility as many patients in the study had mechanical devices that allowed them impressive mobility that was not reflected in their 6MWT scores.
Even viewed with these limitations, this study has several important strengths. It identifies a clear association between social integration and outcomes after MLE amputation. The tools used to measure social integration, quality of life and function are well validated, reliable and objective. A wide range of patients across ages, gender, and comorbidities were evaluated. Finally, the statistical methods used allowed us to control for known confounders and come closer to understanding the true relationships between social integration and outcomes.
This study attempted to describe an association between systemic social support and outcomes by comparing US and Tanzanian cohorts. This is a difficult comparison as using mere nationality as a surrogate for systemic social support fails to capture important differences such as cultural differences, differences in family structure, differences in the density of the population, density of hospitals, density of physicians, and access to care. The authors hypothesized that established systems such as the ADA in the US would lead to better outcomes through the mechanism of greater baseline social support. However, no association was identified. This could be due to a number of reasons. The sample size in the Tanzanian population was small, so the issue could be one of statistical power. As in the above critique, a weakness of the single observation nature of the study is that there were no preoperative baseline data on the patients. The cohorts could have looked different preoperatively and could have undergone different levels of change. Finally, there is the possibility that no association exists and that systemic social support does not play a role in outcomes after MLE amputation. Additional studies looking at larger populations in Tanzania and other developing countries should be done before one can confidently make any conclusions about the impact of systemic social support.
Care of the patient with end stage PVD does not end with the amputation. Life goes on for these patients and it is incumbent upon the clinicians who care for them to understand the factors that dictate success or failure post operatively. This study provides important insight into the role that social integration plays into outcomes for amputees. Beyond the ethical imperative to do the right thing for our patients, the movement toward tying reimbursement to outcomes makes this subject matter even more germane. Though not perfect, the strengths of this study allow for important conclusions to be made. Patients with low social support must be identified early and interventions enacted even prior to their surgery. Assistance should be focused both on improving social integration and improving functional and QoL outcomes. The stage is set for the next step in this investigation, namely a prospective, longitudinal trial to assess the effect of improving social integration among MLE amputees.
Conclusion
In the US population, increased social integration is associated with both improved function and QoL outcomes among MLE amputees. A significant difference in function and QoL was not seen between US and Tanzanian cohorts. Steps should be taken to identify and aid amputees with poor social integration.
Acknowledgement
The authors would like to acknowledge Rachel Rifkin, MPH and Amanda Shanner, BA from the Brigham and Women's hospital for their assistance in acquisition of data.
Support
Dr. Hawkins is supported by the NIH NHLBI T32 (HL007734) Harvard/Longwood Vascular Surgery Training Program and a grant from the Partners Center of Expertise in Global and Humanitarian Health. Drs. Hawkins and Smith are supported by the Brigham & Women's Center for Surgery and Public Health Arthur Tracy Cabot Fellowship. Dr. Smith is also supported by the Lea du Pont Research and Education Endowment.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
*Presented at the 2013 Vascular Annual Meeting, San Francisco, CA, June 1, 2013.
Disclosures
None
References
- 1.Dillingham TR, Pezzin LE, MacKenzie EJ. Limb amputation and limb deficiency: Epidemiology and recent trends in the united states. South Med J. 2002;95(8):875–883. doi: 10.1097/00007611-200208000-00018. [DOI] [PubMed] [Google Scholar]
- 2.Ziegler-Graham K, MacKenzie EJ, Ephraim PL, Travison TG, Brookmeyer R. Estimating the prevalence of limb loss in the united states: 2005 to 2050. Arch Phys Med Rehabil. 2008;89(3):422–429. doi: 10.1016/j.apmr.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 3.Sinha R, van den Heuvel WJ, Arokiasamy P. Factors affecting quality of life in lower limb amputees. Prosthet Orthot Int. 2011;35(1):90–96. doi: 10.1177/0309364610397087. [DOI] [PubMed] [Google Scholar]
- 4.Bhangu S, Devlin M, Pauley T. Outcomes of individuals with transfemoral and contralateral transtibial amputation due to dysvascular etiologies. Prosthet Orthot Int. 2009;33(1):33–40. doi: 10.1080/03093640802492434. [DOI] [PubMed] [Google Scholar]
- 5.Henry AJ, Hevelone ND, Belkin M, Nguyen LL. Socioeconomic and hospital-related predictors of amputation for critical limb ischemia. J Vasc Surg. 2011;53(2):330–9. e1. doi: 10.1016/j.jvs.2010.08.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.GovTrack.us. H.R. 3590, 111th cong.: Patient protection and affordable care act. 2009 [Google Scholar]
- 7.House JS. Social isolation kills, but how and why? Psychosom Med. 2001;63(2):273–274. doi: 10.1097/00006842-200103000-00011. [DOI] [PubMed] [Google Scholar]
- 8.House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241(4865):540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- 9.Seeman TE. Health promoting effects of friends and family on health outcomes in older adults. Am J Health Promot. 2000;14(6):362–370. doi: 10.4278/0890-1171-14.6.362. [DOI] [PubMed] [Google Scholar]
- 10.Barefoot JC, Gronbaek M, Jensen G, Schnohr P, Prescott E. Social network diversity and risks of ischemic heart disease and total mortality: Findings from the copenhagen city heart study. Am J Epidemiol. 2005;161(10):960–967. doi: 10.1093/aje/kwi128. [DOI] [PubMed] [Google Scholar]
- 11.Rutledge T, Linke SE, Olson MB, et al. Social networks and incident stroke among women with suspected myocardial ischemia. Psychosom Med. 2008;70(3):282–287. doi: 10.1097/PSY.0b013e3181656e09. [DOI] [PubMed] [Google Scholar]
- 12.Thong MS, Kaptein AA, Krediet RT, Boeschoten EW, Dekker FW. Social support predicts survival in dialysis patients. Nephrol Dial Transplant. 2007;22(3):845–850. doi: 10.1093/ndt/gfl700. [DOI] [PubMed] [Google Scholar]
- 13.Case RB, Moss AJ, Case N, McDermott M, Eberly S. Living alone after myocardial infarction. impact on prognosis. JAMA. 1992;267(4):515–519. [PubMed] [Google Scholar]
- 14.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) - A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. Apr. 2009;42(2):377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories ATS statement: Guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166(1):111–117. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 16.Datta D, Ariyararatnam R, Hilton S. Timed walking test- an all-ambracing outcome measure for lower-limb amputees? Clin.Rehabil. 1996;10:227. [Google Scholar]
- 17.EuroQol--a new facility for the measurement of health-related quality of life. the EuroQol group. Health Policy. 1990;16(3):199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- 18.Walker N, Mellick D, Brooks CA, Whiteneck GG. Measuring participation across impairment groups using the craig handicap assessment reporting technique. Am J Phys Med Rehabil. 2003;82(12):936–941. doi: 10.1097/01.PHM.0000098041.42394.9A. [DOI] [PubMed] [Google Scholar]
- 19.Walker JL, Knapp D, Minter C, et al. Adult outcomes following amputation or lengthening for fibular deficiency. J Bone Joint Surg Am. 2009;91(4):797–804. doi: 10.2106/JBJS.G.01297. [DOI] [PubMed] [Google Scholar]
- 20.Aldersey H. Disability and work: The united republic of tanzania's workplace policies in the persons with disabilities act of 2010. Disability Studies Quarterly. 2012;32(3) [Google Scholar]
- 21.Jelsma J, Hansen K, De Weerdt W, De Cock P, Kind P. How do Zimbabweans value health states? Popul Health Metr. 2003;1(1):11. doi: 10.1186/1478-7954-1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stineman MG, Kwong PL, Kurichi JE, et al. The effectiveness of inpatient rehabilitation in the acute postoperative phase of care after transtibial or transfemoral amputation: Study of an integrated health care delivery system. Arch Phys Med Rehabil. 2008;89(10):1863–1872. doi: 10.1016/j.apmr.2008.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sauter CN, Pezzin LE, Dillingham TR. Functional outcomes of persons who underwent dysvascular lower extremity amputations: Effect of postacute rehabilitation setting. Am J Phys Med Rehabil. 2013;92(4):287–296. doi: 10.1097/PHM.0b013e31827d620d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Norvell DC, Turner AP, Williams RM, Hakimi KN, Czerniecki JM. Defining successful mobility after lower extremity amputation for complications of peripheral vascular disease and diabetes. J Vasc Surg. 2011;54(2):412–419. doi: 10.1016/j.jvs.2011.01.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Belmont PJ, Jr, Davey S, Orr JD, Ochoa LM, Bader JO, Schoenfeld AJ. Risk factors for 30-day postoperative complications and mortality after below-knee amputation: A study of 2,911 patients from the national surgical quality improvement program. J Am Coll Surg. 2011;213(3):370–378. doi: 10.1016/j.jamcollsurg.2011.05.019. [DOI] [PubMed] [Google Scholar]
- 26.MacKenzie EJ, Bosse MJ, Castillo RC, et al. Functional outcomes following trauma-related lower-extremity amputation. J Bone Joint Surg Am. 2004;86-A(8):1636–1645. doi: 10.2106/00004623-200408000-00006. [DOI] [PubMed] [Google Scholar]
- 27.Helm P, Engel T, Holm A, Kristiansen VB, Rosendahl S. Function after lower limb amputation. Acta Orthop Scand. 1986;57(2):154–157. doi: 10.3109/17453678609000891. [DOI] [PubMed] [Google Scholar]
- 28.Nissen SJ, Newman WP. Factors influencing reintegration to normal living after amputation. Arch Phys Med Rehabil. 1992;73(6):548–551. [PubMed] [Google Scholar]
- 29.Schoppen T, Boonstra A, Groothoff JW, de Vries J, Goeken LN, Eisma WH. Physical, mental, and social predictors of functional outcome in unilateral lower-limb amputees. Arch Phys Med Rehabil. 2003;84(6):803–811. doi: 10.1016/s0003-9993(02)04952-3. [DOI] [PubMed] [Google Scholar]
- 30.Williams RM, Ehde DM, Smith DG, Czerniecki JM, Hoffman AJ, Robinson LR. A two-year longitudinal study of social support following amputation. Disabil Rehabil. 2004;26(14-15):862–874. doi: 10.1080/09638280410001708878. [DOI] [PubMed] [Google Scholar]
- 31.Tsai AC, Lucas M, Sania A, Kim D, Kawachi I. Social integration and suicide mortality among men: 24-year cohort study of u.s. health professionals. Ann Intern Med. 2014;161(2):85–95. doi: 10.7326/M13-1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Piferi RL, Lawler KA. Social support and ambulatory blood pressure: An examination of both receiving and giving. Int J Psychophysiol. 2006;62(2):328–336. doi: 10.1016/j.ijpsycho.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 33.Steptoe A. Stress, social support and cardiovascular activity over the working day. Int J Psychophysiol. 2000;37(3):299–308. doi: 10.1016/s0167-8760(00)00109-4. [DOI] [PubMed] [Google Scholar]
- 34.Kiecolt-Glaser JK, McGuire L, Robles TF, Glaser R. Psychoneuroimmunology: Psychological influences on immune function and health. J Consult Clin Psychol. 2002;70(3):537–547. doi: 10.1037//0022-006x.70.3.537. [DOI] [PubMed] [Google Scholar]
- 35.Umberson D. Family status and health behaviors: Social control as a dimension of social integration. J Health Soc Behav. 1987;28(3):306–319. [PubMed] [Google Scholar]
- 36.Haring TG, Breen CG. A peer-mediated social network intervention to enhance the social integration of persons with moderate and severe disabilities. J Appl Behav Anal. 1992;25(2):319–333. doi: 10.1901/jaba.1992.25-319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dorstyn DS, Mathias JL, Denson LA. Psychosocial outcomes of telephone-based counseling for adults with an acquired physical disability: A meta-analysis. Rehabil Psychol. 2011;56(1):1–14. doi: 10.1037/a0022249. [DOI] [PubMed] [Google Scholar]