Abstract
Nasal colonization with antibiotic resistant bacteria represents both a risk factor for the colonized individual and their immediate contacts. Despite the fact that healthcare workers such as orthopedic surgeons are at a critical interface between the healthcare environment and an at-risk patient population, the prevalence of antibiotic resistant bacteria within the surgical profession remains unclear. This study offers a snapshot of the rate of nasal colonization of orthopedic surgeons with multi-resistant staphylococci including methicillin-resistant S. aureus (MRSA) and methicillin-resistant coagulase-negative staphylococci (MRCoNS). We performed a prospective, observational study obtained at a single time point in late 2013. The participants were active orthopedic, spine and head & neck surgeons from 75 countries. The prevalence of nasal carriage of the different bacteria and the corresponding 95% confidence interval were calculated. From a cohort of 1,166 surgeons, we found an average S. aureus nasal colonization rate of 28.0% (CI 25.4;30.6) and MRSA rate of 2.0% (CI 1.3;2.9), although significant regional variations were observed. The highest rates of MRSA colonization were found in Asia (6.1%), Africa (5.1%) and Central America (4.8%). There was no MRSA carriage detected within our population of 79 surgeons working in North America, and a low (0.6%) MRSA rate in 657 surgeons working in Europe. High rates of MRCoNS nasal carriage were also observed (21.4% overall), with a similar geographic distribution. Recent use of systemic antibiotics was associated with higher rates of carriage of resistant staphylococci. In conclusion, orthopedic surgeons are colonized by S. aureus and MRSA at broadly equivalent rates to the general population. Crucially, geographic differences were observed, which may be partially accounted for by varying antimicrobial stewardship practices between the regions. The elevated rates of resistance within the coagulase-negative staphylococci are of concern, due to the increasing awareness of their importance in hospital acquired and device-associated infection.
Introduction
Staphylococcus aureus and coagulase-negative staphylococci (CoNS) are both commensal and opportunistic pathogens, colonizing humans with an estimated prevalence of 30% and 100% respectively [1, 2]. These microorganisms are generally associated with asymptomatic skin and mucosal carriage, yet are paradoxically recognized as amongst the most frequent causative agents of hospital-associated infection (HAI) and device-associated infection (DAI) [3–5].
Antibiotic resistant strains, such as methicillin-resistant S. aureus (MRSA), have emerged as a significant threat in both the hospital and community environment [6]. Recent estimates suggest MRSA causes between 11,000 and 18,000 deaths, and 80,000 invasive infections in the US annually [4, 7]. With limited treatment options, MRSA infections are associated with higher mortality and increased financial costs [8, 9]. Methicillin resistance is also frequently observed within the CoNS (MRCoNS), particularly in surgical site infection (SSI) and DAI, where biofilm formation on implants and on tissue further reduces treatment success [10].
Identifying the source, reservoirs and vectors for the spread of antibiotic resistant bacteria poses significant challenges. The hospital environment, the patient's endogenous microflora, and health care workers (HCWs) may all play a role [11–14]. Evidence seems to indicate that the endogenous microflora of the patient may be critical, since clinical studies have found that S. aureus skin colonization increases the risk of a subsequent infection by three times and up to 80% of cases of staphylococcal bacteremia are caused by strains identical to those in the patient's nasal cavity [15, 16]. Furthermore, patient colonization with S. aureus is associated with a 2-9-fold increased risk of infection [6, 17]. Due to this apparent risk, routine screening of patients for colonization with S. aureus or MRSA upon hospital admission has been introduced into many healthcare settings including all Veterans Affairs hospitals in the US and numerous European countries [18, 19]. Such active surveillance programs have shown benefit in reducing outbreaks of nosocomial MRSA infections [20]. Interestingly, surgical patients have been shown to be at greater risk of developing HAI and surgeons themselves have even been shown, in small-scale studies, to be at an elevated risk of nasal carriage of MRSA in comparison with non-surgical medical doctors [7, 21]. HCWs are exposed to resistant bacteria in their workplace [22], which represents a risk to the HCW themselves, but also a potential factor in the spread of these bacteria within the hospital environment [23–27]. As such, the issue of screening HCWs for colonization with resistant bacteria has been broached, but the topic remains controversial [11, 23, 24, 28, 29]. Particularly since direct link between colonized HCWs and infection rate in their patients has not been established. The controversy centers upon the perceived sensitivity of the data, and the potential implications of colonization for the employer, the employee and the patient [24].
To explore the issue of colonization with antibiotic resistant bacteria within the surgical profession, we have prospectively evaluated the nasal carriage of staphylococci with their antibiotic resistance profiles in a large international cohort of active orthopedic, spine and head & neck surgeons. The primary aim of this study was to identify the prevalence of antibiotic resistant staphylococci present in the nares of active orthopedic surgeons. The secondary aim was to identify risk factors for nasal carriage of staphylococci based on personal and professional parameters.
Materials and Methods
Study design
In total 1,176 orthopedic, spine and head & neck surgeons from 75 different countries attending an international course in Davos, Switzerland, in late 2013 took part in this study. They represented 76% of the 1,200 participants and 350 faculty members present. Enrollment was voluntary, and the collected data was de-identified. All participants gave informed written consent and provided a nasal swab, alongside basic demographic and professional information. Bacterial identification and antibiotic susceptibility data were linked to the personal and professional information with a unique study participant code, which could not be linked with the individual participant in any way. Participants did not receive reimbursement for enrollment in the study.
Surgeon screening and data acquisition
The questionnaire queried years practicing as a surgeon, location of place of work and birth (country and region), personal use of antibiotics within the past six months, treatment of patients with bone and joint infection, and treatment of patients with MRSA infection. No data was recorded on surgeon comorbidities or specific details of antibiotics taken. Data was entered via tablet computers into a REDCap electronic data capture tool, managed by our clinical research statisticians [30].
The surgeon participants circulated a dry swab (MASTASWABTM, Mast Group Ltd., Italy) 5–6 times around the anterior nares of both nasal cavities and immediately placed it in the sterile swab container with protective Amies medium gel. Swabs were stored at 4–6°C at the end of each day and batches were transported to the clinical microbiology laboratory of the Trauma Center Murnau, Germany (maximum transportation time of four hours).
Specimen processing and sample analysis
Bacterial culture and identification was performed according to the standard procedure for our hospital. In order to specifically culture Gram-positive bacteria, the swabs were streaked out on Gram-positive selective Columbia CNA (Colistin-Naladixic Acid) agar with 5% sheep blood (bioMérieux, Hazelwood, MO, USA) and subsequently incubated at 37°C for 48 hours. Morphologically distinct colony types with characteristic visual appearance of a staphylococcal species were identified and antibiotic susceptibility to 28 antibiotics was determined using a Vitek2 machine (bioMérieux Vitek Inc., Hazelwood, MO, USA). The antibiotic susceptibility pattern of all isolates was classified according to the European Centers for Disease Prevention and Control (ECDC) and the US Centers for Disease Control and Prevention (CDC) definition [31]. Using this definition bacteria were classified according to four different criteria: (1) oxacillin resistance; (2) total number of antibiotics to which the bacterium was resistant; (3) number of antibiotic classes to which the bacterium was resistant (out of 14 classes); and (4) multi-drug resistance. Oxacillin resistance is considered definitive for methicillin resistant status, and bacteria displaying oxacillin resistance will henceforth be described as MR (e.g. MRSA, MRSE, MRCoNS).
Statistical analysis
Descriptive statistics were used to analyze surgeon characteristics and the antibiotic resistance patterns of the isolated bacteria. The prevalence of the different bacteria and the corresponding 95% confidence interval (95% CI) were calculated. Differences in the prevalence between subgroups of surgeons as well as differences in multi-drug resistance of bacteria were tested by the Chi-square test, or Fisher's exact test as indicated. Differences in the number of resistances (to 28 antibiotics) were tested by Kruskal-Wallis test. P-values <0.05 were considered significant. Statistical analyses were performed using SAS software (Version 9.2; Cary, NC, USA).
Institutional Review Board approval
Institutional Review Board approval to perform this study was granted by the "Ethik-Kommission der Bayerischen Landesärztekammer", Mühlbauerstrasse 16, 81677 Munich, Germany (Approval number 13090).
Results
Participant demographics
Six of the 1,176 participants enrolled in the study were removed due to incomplete data and four were removed due to missing nasal swabs. Table 1 shows the demographic data of the remaining 1,166 included as study participants. Hospitals from 75 different countries were represented, with the most participants working in Switzerland (n = 178), followed by the Netherlands (n = 86), Germany (n = 56), USA (n = 53), Brazil (n = 50) and China (n = 47). Of the 95 countries of birth, the most participants were born in Germany (n = 101), followed by Switzerland (n = 86), the Netherlands (n = 83), USA (n = 57), Brazil (n = 49) and China (n = 48). The nationality, gender and age profiles were reflective of the course participant profile and included surgeons at all stages of their career.
Table 1. Demographic characteristics of participating surgeons.
| Characteristics | n = 1166 | n (%) |
|---|---|---|
| Age | younger than 36 years | 422 (36.2) |
| 36–45 years | 360 (30.9) | |
| 46–55 years | 272 (23.3) | |
| older than 55 years | 112 (9.6) | |
| Gender | Male | 1026 (88.0) |
| Female | 140 (12.0) | |
| Region of birth, N = 1164 | Africa | 58 (5.0) |
| Asia | 249 (21.4) | |
| Europe | 624 (53.6) | |
| North America | 78 (6.7) | |
| Central America and Caribbean | 22 (1.9) | |
| South America | 113 (9.7) | |
| Oceania | 20 (1.7) | |
| Unknown | 2 (0.2) | |
| Region of work place, N = 1164 | Africa | 39 (3.4) |
| Asia | 231 (19.8) | |
| Europe | 657 (56.4) | |
| North America | 79 (6.8) | |
| Central America and Caribbean | 21 (1.8) | |
| South America | 108 (9.3) | |
| Oceania | 29 (2.5) | |
| Unknown | 2 (0.2) | |
| Years practicing as a surgeon | less than 5 years | 295 (25.3) |
| 5–10 years | 292 (25.0) | |
| 11–25 years | 423 (36.3) | |
| more than 25 years | 156 (13.4) | |
| Type of hospital, N = 1154 | Outpatient department | 0 (0.0) |
| Local hospital | 334 (28.9) | |
| University hospital or level one trauma center | 801 (69.4) | |
| Outpatient department + local hospital | 4 (0.3) | |
| Outpatient department + university hospital or level one trauma center | 3 (0.3) | |
| Local hospital + university hospital or level one Trauma center | 8 (0.7) | |
| All three | 4 (0.3) | |
| Unknown | 12 (1.0) | |
| Treated patients infected with MRSA within the last 6 months? | No | 255 (21.9) |
| Yes | 911 (78.1) | |
| Involved in treatment of bone or Implant infections within last 6 months? | No | 165 (14.2) |
| Yes | 1001 (85.8) | |
| Received antibiotic treatment within last 6 months? | No | 909 (78.0) |
| Yes | 257 (22.0) |
Bacterial growth and antibiotic susceptibility
Overall, 95.3% of all swabs yielded Gram-positive bacterial growth. Two different species were cultured in 162 swabs (148 cases with one S. aureus and one CoNS, 14 cases with 2 different CoNS), resulting in a total number of 1,273 bacterial isolates from the 1,166 enrolled surgeons. The prevalence of each bacterial grouping is shown in Table 2.
Table 2. Prevalence of each bacterial species and grouping, n = 1166 surgeons.
| Prevalence of nasal colonization* | n | % (95% CI) |
|---|---|---|
| No growth of any Gram-positive bacteria | 55 | 4.7 (3.6;6.1) |
| Staphylococcus aureus | 326 | 28.0 (25.4;30.6) |
| MRSA | 23 | 2.0 (1.3;2.9) |
| MSSA | 303 | 26.0 (23.5;28.6) |
| Staphylococcus epidermidis | 591 | 50.7 (47.8;53.6) |
| MRSE | 173 | 14.8 (12.8;17.0) |
| MSSE | 418 | 35.8 (33.1;38.7) |
| Coagulase-negative staphylococci (CoNS) | 933 | 80.0 (77.6;82.3) |
| MRCoNS* * | 250 | 21.4 (19.1;23.9) |
| MSCoNS* * | 681 | 58.4 (55.5;61.3) |
* Prevalence in all 1166 surgeons
** Individual surgeons are included in both MRCoNS and MSCoNS categories, if both microorganisms were cultured from the same swab (n = 2). Four surgeons with a CoNS and missing information on oxacillin resistance were excluded.
Other than S. epidermidis, the CoNS species detected were: Staphylococcus auricularis (n = 8 surgeons, MR = 0%); Staphylococcus capitis (n = 12, MR = 0%); Staphylococcus haemolyticus (n = 46, MR = 28.9%); Staphylococcus hominis (n = 264, MR = 24.8%); Staphylococcus intermedius (n = 2, MR = 0%); Staphylococcus lentus (n = 4, MR = 0%); Staphylococcus lugdunensis (n = 12, MR = 0.1%); Staphylococcus saprophyticus (n = 1, MR = 0%); and Staphylococcus warneri (n = 7, MR = 0%).
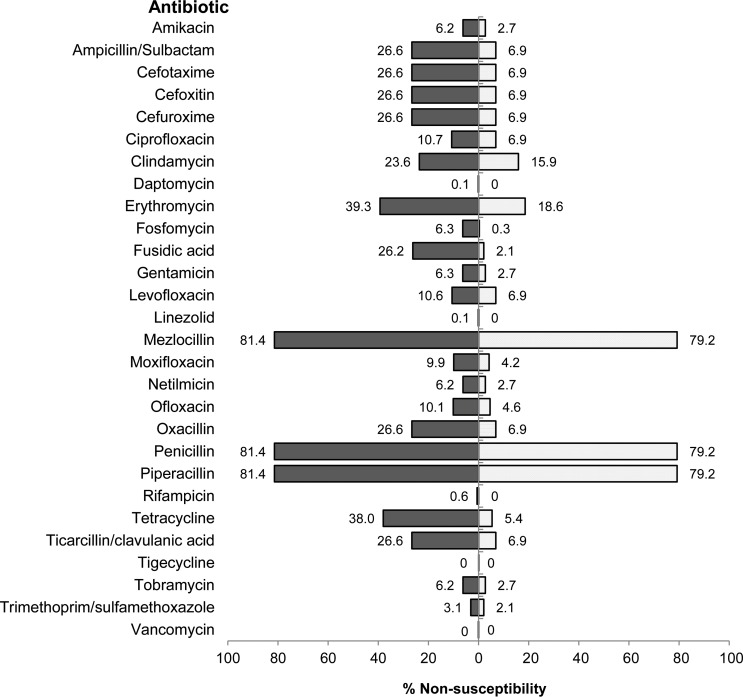
Antibiotic susceptibility testing was complete for all 28 antibiotics in 96.7% of isolates (Fig 1). Few notable resistance pattern were detected within the CoNS group, including strains resistant to rifampicin (1–≥32 μg/ml, n = 6), daptomycin (2 μg/ml, n = 1) and linezolid (≥8 μg/ml, n = 1), whereas Minimum Inhibitory Concentration (MIC) breakpoints defined by EUCAST were utilized [32, 33]. Multi-drug resistance (MDR), according to the ECDC definition [31], was present in 36.0% of all isolates (16.0% of S. aureus, 42.0% of S. epidermidis and 42.9% of all CoNS). No extensively-resistant or pan-drug-resistant isolates were identified [31]. The S. aureus isolates were, on average, non-susceptible (i.e. either intermediate or resistant) to 3.5 antibiotic agents, whilst for the entire CoNS group and the S. epidermidis isolates, it was 6.1 and 6.3 respectively. When grouped into classes, S. aureus isolates were, on average, completely resistant to 0.6 antibiotic classes, while CoNS were completely resistant to an average of 1.8 antibiotic classes.
Fig 1. Non-Susceptibility of CoNS (left) and S. aureus (right), (%).
Risk factors for staphylococcal colonization
The prevalence of S. aureus was found to vary significantly between region of birth and region of work (Table 3). Within Europe, there was no significant intra-regional effect e.g. between Northern and Southern Europe, concerning S. aureus prevalence (Table 4). More than one fifth (22.0%) of the surgeon participants received systemic antibiotic treatment within the six months prior to the study (Table 1). Use of antibiotics did not result in an increase in culture negative swabs (p = 0.088), although significantly lower rates of nasal colonization with S. aureus (p = 0.043) were observed in these participants (Table 3). Nasal colonization with S. aureus was significantly lower in female (18.6%) than in male participants (29.2%, p = 0.008) (Table 3). No other factors were found to influence nasal colonization with S. aureus.
Table 3. Prevalence of S. aureus, MRSA and MRCoNS, n = 1166.
| S. aureus | MRSA | MRCoNS | |||||
|---|---|---|---|---|---|---|---|
| n (%) | P value | n (%) | P value | n (%) | P value | ||
| Region of birth, n = 1164 | Africa | 8 (13.8) | 0.050 | 2 (3.4) | <0.001 | 21 (36.2) | <0.001 |
| Asia | 60 (24.1) | 14 (5.6) | 92 (37.1) | ||||
| Europe | 188 (30.1) | 4 (0.6) | 97 (15.6) | ||||
| North America | 17 (21.8) | 0 (0.0) | 9 (11.5) | ||||
| Central America | 7 (31.8) | 1 (4.5) | 7 (31.8) | ||||
| South America | 38 (33.6) | 2 (1.8) | 19 (17.0) | ||||
| Oceania | 6 (30.0) | 0 (0.0) | 5 (25.0) | ||||
| Region of work place, n = 1164 | Africa | 6 (15.4) | 0.041 | 2 (5.1) | <0.001 | 19 (48.7) | <0.001 |
| Asia | 55 (23.8) | 14 (6.1) | 92 (40.0) | ||||
| Europe | 191 (29.1) | 4 (0.6) | 99 (15.1) | ||||
| North America | 16 (20.3) | 0 (0.0) | 9 (11.4) | ||||
| Central America | 7 (33.3) | 1 (4.8) | 7 (33.3) | ||||
| South America | 40 (37.0) | 2 (1.9) | 17 (15.9) | ||||
| Oceania | 10 (34.5) | 0 (0.0) | 7 (24.1) | ||||
| Received antibiotic treatment within last 6 months | No | 267 (29.4) | 0.043 | 12 (1.3) | 0.003 | 157 (17.3) | <0.001 |
| Yes | 59 (23.0) | 11 (4.3) | 93 (36.3) | ||||
| Age | younger than 36 years | 126 (29.9) | 0.365 | 5 (1.2) | 0.422 | 79 (18.7) | 0.087 |
| 36–45 years | 105 (29.2) | 8 (2.2) | 78 (21.8) | ||||
| 46–55 years | 69 (25.4) | 8 (2.9) | 72 (26.6) | ||||
| older than 55 years | 26 (23.2) | 2 (1.8) | 21 (18.8) | ||||
| Gender | Male | 300 (29.2) | 0.008 | 22 (2.1) | 0.510 | 219 (21.4) | 0.847 |
| Female | 26 (18.6) | 1 (0.7) | 31 (22.1) | ||||
| Years practicing as a surgeon | less than 5 years | 96 (32.5) | 0.207 | 3 (1.0) | 0.258 | 47 (15.9) | 0.027 |
| 5–10 years | 75 (25.7) | 4 (1.4) | 70 (24.0) | ||||
| 11–25 years | 116 (27.4) | 11 (2.6) | 103 (24.5) | ||||
| more than 25 years | 39 (25.0) | 5 (3.2) | 30 (19.4) | ||||
| Type of hospital*, n = 1135 | Local hospital | 101 (30.2) | 0.180 | 5 (1.5) | 0.414 | 76 (22.8) | 0.541 |
| University hospital or level one trauma center | 211 (26.3) | 18 (2.2) | 169 (21.2) | ||||
| Treated patients infected with MRSA within the last 6 months? | No | 72 (28.2) | 0.911 | 5 (2.0) | 0.988 | 50 (19.7) | 0.422 |
| Yes | 254 (27.9) | 18 (2.0) | 200 (22.0) | ||||
| Involved in treatment of bone or implant infections within last 6 months? | No | 37 (22.4) | 0.087 | 1 (0.6) | 0.234 | 35 (21.3) | 0.954 |
| Yes | 289 (28.9) | 22 (2.2) | 215 (21.5) | ||||
* Only surgeons who work in one hospital type exclusively are considered
Table 4. Prevalence of S. aureus and MRCoNS within Europe (workplace), n = 657.
| S. aureus | MRCoNS* | ||||||
|---|---|---|---|---|---|---|---|
| No (%) | Yes (%) | P value | No (%) | Yes (%) | P value | ||
| Region within Europe, n = 657 | Northern | 71 (71.7) | 28 (28.3) | 0.151 | 93 (93.9) | 6 (6.1) | 0.018 |
| Eastern | 37 (82.2) | 8 (17.8) | 33 (75.0) | 11 (25.0) | |||
| Southern | 70 (76.1) | 22 (23.9) | 77 (84.6) | 14 (15.4) | |||
| Western | 288 (68.4) | 133 (31.6) | 353 (83.8) | 68 (16.2) | |||
* Missing data on methicillin resistance in 2 participants with CoNS
Risk factors for antibiotic resistance
The prevalence of MRSA, MRCoNS, and specifically the prevalence of MRSE were found to vary significantly between region of birth and region of work (Tables 3 and 5, Fig 2). Similarly, MDR and the extent of resistances according to our four criteria were all affected by the region of birth and workplace for all bacteria (p<0.001). Within Europe, there was a significant intra-regional effect concerning MRCoNS incidence (Table 4). MRSA colonization was detected in just four participants from Europe, which is too few for inter-regional comparison.
Table 5. Participants with MRSA and MRCoNS by country of workplace.
| Country of workplace* | Number of participants | Number with MRSA | Number with MRCoNS |
|---|---|---|---|
| Argentina | 9 | 1 | 2 |
| Australia | 22 | 0 | 6 |
| Austria | 15 | 0 | 4 |
| Belgium | 33 | 1 | 5 |
| Brazil | 50 | 1 | 8 |
| Canada | 23 | 0 | 2 |
| Chile | 13 | 0 | 3 |
| China | 47 | 3 | 18 |
| Colombia | 19 | 0 | 0 |
| Czech Republic | 7 | 0 | 4 |
| Denmark | 30 | 1 | 1 |
| Egypt | 9 | 2 | 3 |
| Estonia | 7 | 0 | 2 |
| Finland | 12 | 0 | 1 |
| Germany | 56 | 0 | 17 |
| Hungary | 9 | 0 | 3 |
| India | 28 | 3 | 20 |
| Indonesia | 10 | 0 | 4 |
| Ireland | 9 | 0 | 4 |
| Israel | 16 | 0 | 4 |
| Italy | 38 | 0 | 5 |
| Japan | 18 | 2 | 5 |
| Jordan | 8 | 2 | 5 |
| Lebanon | 8 | 0 | 3 |
| Mexico | 16 | 1 | 5 |
| The Netherlands | 86 | 0 | 13 |
| New Zealand | 7 | 0 | 1 |
| Norway | 24 | 0 | 1 |
| Peru | 5 | 0 | 2 |
| Poland | 14 | 0 | 2 |
| Russian Federation | 11 | 0 | 1 |
| Saudi Arabia | 15 | 0 | 6 |
| Singapore | 15 | 2 | 3 |
| Slovenia | 21 | 0 | 5 |
| South Africa | 21 | 0 | 9 |
| South Korea | 5 | 1 | 2 |
| Spain | 21 | 1 | 2 |
| Sri Lanka | 5 | 1 | 4 |
| Sweden | 21 | 0 | 1 |
| Switzerland | 178 | 0 | 20 |
| Thailand | 13 | 0 | 2 |
| Turkey | 8 | 0 | 3 |
| United Arab Emirates | 5 | 0 | 0 |
| United Kingdom | 30 | 1 | 5 |
| United States of America | 53 | 0 | 7 |
| Venezuela | 5 | 0 | 1 |
| Vietnam | 5 | 0 | 4 |
| Others** | 86 | 0 | 22 |
*Only countries with at least 5 participants are listed
**Number of countries with less than 5 participants, n = 28
Fig 2. World map showing surgeon workplace and nasal carriage of MRSA and MRCoNS.
Antibiotic use did result in a significant increase in the prevalence of MRSA, MRSE and MRCoNS and the number of antibiotic non-susceptibilities (p<0.001). The MRSA prevalence in surgeons who had received antibiotic treatment was 4.3%, compared with 1.3% in those who had not received antibiotic treatment. The number of years of practice was found to influence the prevalence of MRCoNS and the extent of non-susceptibilities in CoNS (p = 0.022) but not methicillin resistance in S. aureus. However, no other factor was found to influence antibiotic resistance status of any staphylococcal species (Table 3).
Discussion
The literature is lacking in an international and large-scale assessment of nasal colonization in the surgical profession. Against this background, we provide a global snapshot of nasal colonization with multi-resistant staphylococci in an international cohort of surgeons.
From a total population of 1,166 surgeons, we found an average S. aureus nasal colonization rate of 28.0% (CI 25.4;30.6), which is broadly comparable to previously described colonization rates in the general population: 27% in the UK and 29–32% in the US [34–36]. Studies investigating colonization of HCWs with S. aureus in regional cohorts from São Tomé and Príncipe, Iran, Norway and Thailand has also shown similar rates (20.2–29.7%) [37–40]. Some studies have indicated that HCWs may be colonized at a higher rate, whereby a S. aureus colonization rate of 21.7% was found in non- physicians and a rate of 37.4% in physicians [41], whereas in two West African hospitals, extensive colonization of both inpatients and HCWs by S. aureus (carriage rate 41%) was demonstrated [42]. Only a few studies have specifically analyzed S. aureus nasal colonization in surgeons [43]. Schwarzkopf et al. screened 135 orthopedic surgeons at the New York University Hospital for Joint Diseases and identified a rather high S. aureus colonization rate of 35.7% [43]. Our study of surgeons working in 75 countries, revealed significant differences in S. aureus colonization between the regions, with the lowest colonization rates in surgeons working in Africa and the highest in South America. A prevalence of 21% for S. aureus from 79 North American surgeons, is lower than that described by Schwarzkopf et al. in a smaller cohort of surgeons [43]; although whether this is reflective of a downwards trend in the US is difficult to determine at this point. Previous studies have shown increased prevalence of S. aureus in white males [44, 45]. Although we did not record the ethnicity of participants, we could identify a low S. aureus colonization in our African population. The tendency for increased S. aureus colonization rates in certain regions is likely a multifactorial one involving a significant genetic component [44, 46–48], although this requires further investigation.
The antibiotic resistance profile of these bacteria is an important issue, with the CDC identifying MRSA as a serious threat to public health [4]. MRSA prevalence in our survey averaged 2%, although significant regional variations were observed. The highest rates of MRSA colonization were found in Asia, Central America and Africa. There was no MRSA detected within our population of 79 surgeons working in North America, and a low MRSA rate in 657 surgeons working in Europe. The absence of MRSA in North American surgeons was unexpected. However, given the high positive culture yield, the data strongly indicates a low prevalence in North America. The tendency for higher MRSA rates in Asia and Africa may be expected when one considers the high previously reported MRSA rates (42–73%) in HCWs in regional small-scale studies [49, 50]. MRSA colonization in HCWs has also been described for Norway and Cape Verde (0%), USA, (2%), São Tomé and Príncipe (4.0%) and Iran (5.3%) [37, 39, 40, 42, 51]. Exceedingly high MRSA colonization rates in HCW of 41.9% in Uganda and over 70% in Saudi Arabia [49, 50]. No significant effect of age, gender or type of hospital was found to be significant in relation to MRSA carriage in our study, although our dataset was significantly gender biased. Nevertheless, age has previously been shown to be a factor in S. aureus colonization [52, 53], which could not be repeated within our study.
MRSA colonization rates in the general population are quite consistently below 2%, as shown for large studies in Northern Europe (<1%), with higher levels described in isolated reports from Central/Western-European countries, the US, New Zealand and Australia (6–22%) and higher still in Southern European countries as well as in parts of the US, Asia and Africa (28–63%) [34, 36, 54, 55]. A trend for increasing MRSA prevalence in the US healthcare system has been described in the past, with in two US National Health and Nutrition Examination Surveys (NHANES) showing a significant increase of MRSA colonization within non-institutionalized patients from 0.8% to 1.5% between 2001 and 2004 [56]. Our MRSA prevalence of 0% in North American surgeons reflects a significant reduction in comparison with the earlier New York Study [43]. The annual report 2013 of the European Antimicrobial Resistance Surveillance Network (EARS-Net) has revealed generally lower MRSA percentages in Northern Europe and higher rates in south and southeastern countries [57]. This study could not confirm this trend since MRSA colonization was detected in just four European participants. In addition to a trend of lowering MRSA prevalence across European countries, the improved antimicrobial stewardship practices may also have a side effect of reducing HCW colonization in this region.
Twenty-two percent of participating surgeons received antibiotic treatment in the six months prior to the study. This did not cause an increase in culture negative results in our study, and experimental studies have shown only a short-term reduction in bacterial load secondary to antibiotic usage [58]. We found that antibiotic therapy simultaneously reduced the rate of MSSA colonization, and increased the rate of MRSA and MRCoNS colonization compared with the remaining surgeons. This has not been shown in a surgical population previously, but does mirror patient studies, wherein MRSA prevalence was increased after exposure to antibiotics as revealed in a meta-analysis from 2008 [59]. Therefore, mirroring the calls to rationalize patient antibiotic usage, protocols to ensure antibiotic stewardship for HCWs is a topic also requiring some attention.
In this study, we additionally analyzed MRCoNS carriage, which literature tells us can reach 75% in invasive infections in the hospital setting [10]. Scattered studies report MRCoNS nasal colonization rates of outpatients are much lower, ranging from 11% to 31% [60]. Scant data is available on MRCoNS in surgeon populations. We identified an overall MRCoNS colonization rate of 21.4%, which is quite high, although within the limits of the general population. Geographic differences were again apparent, with North America and Europe again being low, and Asia and Africa with the highest prevalence. Within Europe, methicillin resistance in CoNS ranged from a low of 6.1% in Northern Europe to a high of 25.0% in Eastern Europe. The reasons for a high MRCoNS incidence in Asia and Africa are poorly understood, but a crossover in parameters that lead to high MRSA incidence may be considered likely. With an increasing awareness of MRCoNS as a pathogen and as a source of mobile antibiotic resistance genes, the risk of antibiotic resistance gene transfer to S. aureus should not be underestimated [25, 61]. Some resistant CoNS displayed resistance against rifampicin, daptomycin and linezolid. In infections caused by methicillin resistant staphylococci, these antibiotics may represent the only possible treatment options [62]. Colonization with such strains is a cause for concern and indicates further studies may be required to monitor the scale of colonization with bacteria resistant to important antibiotics.
One of the most discussed topics when it comes to HCW colonization with resistant bacteria is always going to be the impact upon the HCW themselves, their employers and the patients being treated. A proposed solution for colonization with S. aureus and MRSA has been the development of decolonization protocols [63, 64]. Decolonization with MRCoNS is not described and, as universal commensals, decolonization of CoNS is not practical. Decolonization has been shown to be more efficacious in surgical departments, as results have been less promising for other specialties [63, 64], and thus surgeons may represent a special case for more regular screening.
There are a number of limitations to this study. In particular, this study monitors colonization at a single time-point, although colonization is known to be variable over time and it has to be differentiated between persistent and intermitted carriers [2]. Repeat sampling of this diverse and large population of surgeons would require either re-swabbing at each local hospital or recruiting the proportion that return to the same event 12 months later. In any case, storing surgeon data was not permitted according to our IRB approval, rendering repeat sampling impossible. Another potential limitation may be that the detection rate of staphylococci may have been increased if a DNA based evaluation were performed (e.g. PCR). Since the swabs were not moistened, and there was no pre-enrichment step before plating on blood agar, prevalence of S. aureus, MRSA and MRCoNS may, at least in theory, be underestimated. The choice of swab type (MASTASWABTM, Mast Group Ltd., Italy) may influence the MRSA carrier status as shown by Warnke et al. in an in vitro model and may have led to diagnosing false negative MRSA carrier status [65]. Similarly, the swabs were taken at an altitude of 1,400 meters in the Swiss Alps, although previous findings indicate this should not be an issue [45, 66]. Ultimately, our culture positive rate of 95.3% clearly indicates the swab and sample handling techniques were highly successful. An unavoidable limitation of the study is the unequal distribution of participants from each region. The study had a high enrollment rate, and the study profile largely reflected the overall participant profile in all aspects (age, gender, region of work). Finally, a more detailed and expanded questionnaire could have addressed further interesting research questions such as details on treatment with antibiotics, previous decolonization, hospital prescribing practices, length of employment at current institution. However, we minimized the time required for enrollment in an effort to maximize recruitment and so further questions were not asked.
The data presented in this study indicates surgeons are broadly equivalent to the general population in terms of nasal colonization with resistant bacteria. As stated in the recent report (2014) of the World Health Organization on antimicrobial resistance, antibiotic prescribing and infection control practices vary throughout the world [67]. These may affect the significant geographic variation of nasal colonization with resistant strains. Importantly, the surgical profession cares for a vulnerable population, and further studies would be required to elucidate the impact of increased surveillance on the relationship between surgeons and their own health, but also on the role this may play in nosocomial infections.
Conclusions
This study shows that the rate of nasal colonization with S. aureus (26%) and MRSA (2%) in surgeons is similar to the general population. Significant geographic variation was observed, which may be at least partially accounted for by varying antimicrobial stewardship practices in the different regions. Concerted efforts within the USA and Europe to achieve greater antibiotic prescribing restraint, may partially explain the reduced colonization with resistant bacteria in these regions.
Acknowledgments
We acknowledge the contribution of Katrin Rebmann, Janik Hilse and Alexander Joeris of AO Clinical Investigation and Documentation, Dübendorf, Switzerland. Daniela Brandl of the IT department at Trauma Center Murnau and the staff of the Microbiology Laboratory at Trauma Center Murnau, in particular Regina Werle and Ursula Köhler.
Data Availability
All relevant data are within the paper.
Funding Statement
This project was funded by AO Trauma, AO Foundation, Davos Switzerland, https://aotrauma.aofoundation.org (MM). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Grice EA, Segre JA. The skin microbiome. Nat Rev Microbiol. 2011;9(4):244–53. 10.1038/nrmicro2537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kluytmans J, van Belkum A, Verbrugh H. Nasal carriage of Staphylococcus aureus: epidemiology, underlying mechanisms, and associated risks. Clin Microbiol Rev. 1997;10(3):505–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Danzmann L, Gastmeier P, Schwab F, Vonberg RP. Health care workers causing large nosocomial outbreaks: a systematic review. BMC Infect Dis. 2013;13:98 10.1186/1471-2334-13-98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Center for Disease Control and Prevention. Antibiotic resistance threats in the United States, 2013. Atlanta: CDC; 2013. Available: http://www.cdc.gov/drugresistance/threat-report-2013/. Accessed 06 January 2016. [Google Scholar]
- 5.National Nosocomial Infections Surveillance System. National Nosocomial Infections Surveillance (NNIS) System Report, data summary from January 1992 through June 2004, issued October 2004. Am J Infect Control. 2004;32(8):470–85. 10.1016/j.ajic.2004.10.001 . [DOI] [PubMed] [Google Scholar]
- 6.Boucher HW, Corey GR. Epidemiology of methicillin-resistant Staphylococcus aureus. Clin Infect Dis. 2008;46 Suppl 5:S344–9. 10.1086/533590 . [DOI] [PubMed] [Google Scholar]
- 7.Dantes R, Mu Y, Belflower R, Aragon D, Dumyati G, Harrison LH, et al. National burden of invasive methicillin-resistant Staphylococcus aureus infections, United States, 2011. JAMA Intern Med. 2013;173(21):1970–8. 10.1001/jamainternmed.2013.10423 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haddadin AS, Fappiano SA, Lipsett PA. Methicillin resistant Staphylococcus aureus (MRSA) in the intensive care unit. Postgrad Med J. 2002;78(921):385–92. 10.1136/pmj.78.921.385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Klein E, Smith DL, Laxminarayan R. Hospitalizations and deaths caused by methicillin-resistant Staphylococcus aureus, United States, 1999–2005. Emerg Infect Dis. 2007;13(12):1840–6. 10.3201/eid1312.070629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Diekema DJ, Pfaller MA, Schmitz FJ, Smayevsky J, Bell J, Jones RN, et al. Survey of infections due to Staphylococcus species: frequency of occurrence and antimicrobial susceptibility of isolates collected in the United States, Canada, Latin America, Europe, and the Western Pacific region for the SENTRY Antimicrobial Surveillance Program, 1997–1999. Clin Infect Dis. 2001;32 Suppl 2:S114–32. 10.1086/320184 . [DOI] [PubMed] [Google Scholar]
- 11.Vonberg RP, Stamm-Balderjahn S, Hansen S, Zuschneid I, Ruden H, Behnke M, et al. How often do asymptomatic healthcare workers cause methicillin-resistant Staphylococcus aureus outbreaks? A systematic evaluation. Infect Control Hosp Epidemiol. 2006;27(10):1123–7. 10.1086/507922 . [DOI] [PubMed] [Google Scholar]
- 12.von Eiff C, Proctor RA, Peters G. Coagulase-negative staphylococci. Pathogens have major role in nosocomial infections. Postgrad Med. 2001;110(4):63–76. . [PubMed] [Google Scholar]
- 13.Wertheim HF, Melles DC, Vos MC, van Leeuwen W, van Belkum A, Verbrugh HA, et al. The role of nasal carriage in Staphylococcus aureus infections. Lancet Infect Dis. 2005;5(12):751–62. 10.1016/S1473-3099(05)70295-4 . [DOI] [PubMed] [Google Scholar]
- 14.Dalstrom DJ, Venkatarayappa I, Manternach AL, Palcic MS, Heyse BA, Prayson MJ. Time-dependent contamination of opened sterile operating-room trays. J Bone Joint Surg Am. 2008;90(5):1022–5. 10.2106/JBJS.G.00689 . [DOI] [PubMed] [Google Scholar]
- 15.von Eiff C, Becker K, Machka K, Stammer H, Peters G. Nasal carriage as a source of Staphylococcus aureus bacteremia. N Engl J Med. 2001;344(1):11–6. 10.1056/NEJM200101043440102 . [DOI] [PubMed] [Google Scholar]
- 16.Wertheim HF, Vos MC, Ott A, van Belkum A, Voss A, Kluytmans JA, et al. Risk and outcome of nosocomial Staphylococcus aureus bacteraemia in nasal carriers versus non-carriers. Lancet. 2004;364(9435):703–5. 10.1016/S0140-6736(04)16897-9 . [DOI] [PubMed] [Google Scholar]
- 17.Wenzel RP, Perl TM. The significance of nasal carriage of Staphylococcus aureus and the incidence of postoperative wound infection. J Hosp Infect. 1995;31(1):13–24. 10.1016/0195-6701(95)90079-9 . [DOI] [PubMed] [Google Scholar]
- 18.Jain R, Kralovic SM, Evans ME, Ambrose M, Simbartl LA, Obrosky DS, et al. Veterans Affairs initiative to prevent methicillin-resistant Staphylococcus aureus infections. N Engl J Med. 2011;364(15):1419–30. 10.1056/NEJMoa1007474 . [DOI] [PubMed] [Google Scholar]
- 19.Kalenic S, Cookson B, Gallagher R, Popp W, Asensio-Vegas A, Assadian O, et al. Comparison of recommendations in national/regional Guidelines for prevention and control of MRSA in thirteen European countries. Int J Infect Control. 2010;6(2):1–10. 10.3396/ijic.v6i2.5138 [DOI] [Google Scholar]
- 20.Blok HE, Troelstra A, Kamp-Hopmans TE, Gigengack-Baars AC, Vandenbroucke-Grauls CM, Weersink AJ, et al. Role of healthcare workers in outbreaks of methicillin-resistant Staphylococcus aureus: a 10-year evaluation from a Dutch university hospital. Infect Control Hosp Epidemiol. 2003;24(9):679–85. 10.1086/502275 . [DOI] [PubMed] [Google Scholar]
- 21.Brady RR, McDermott C, Graham C, Harrison EM, Eunson G, Fraise AP, et al. A prevalence screen of MRSA nasal colonisation amongst UK doctors in a non-clinical environment. Eur J Clin Microbiol Infect Dis. 2009;28(8):991–5. 10.1007/s10096-009-0718-4 . [DOI] [PubMed] [Google Scholar]
- 22.Cespedes C, Miller M, Quagliarello B, Vavagiakis P, Klein RS, Lowy FD. Differences between Staphylococcus aureus isolates from medical and nonmedical hospital personnel. J Clin Microbiol. 2002;40(7):2594–7. 10.1128/JCM.40.7.2594-2597.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Albrich WC, Harbarth S. Health-care workers: source, vector, or victim of MRSA? Lancet Infect Dis. 2008;8(5):289–301. 10.1016/S1473-3099(08)70097-5 . [DOI] [PubMed] [Google Scholar]
- 24.Hawkins G, Stewart S, Blatchford O, Reilly J. Should healthcare workers be screened routinely for meticillin-resistant Staphylococcus aureus? A review of the evidence. J Hosp Infect. 2011;77(4):285–9. 10.1016/j.jhin.2010.09.038 . [DOI] [PubMed] [Google Scholar]
- 25.Berglund C, Soderquist B. The origin of a methicillin-resistant Staphylococcus aureus isolate at a neonatal ward in Sweden-possible horizontal transfer of a staphylococcal cassette chromosome mec between methicillin-resistant Staphylococcus haemolyticus and Staphylococcus aureus. Clin Microbiol Infect. 2008;14(11):1048–56. 10.1111/j.1469-0691.2008.02090.x . [DOI] [PubMed] [Google Scholar]
- 26.Mulligan ME, Murray-Leisure KA, Ribner BS, Standiford HC, John JF, Korvick JA, et al. Methicillin-resistant Staphylococcus aureus: a consensus review of the microbiology, pathogenesis, and epidemiology with implications for prevention and management. Am J Med. 1993;94(3):313–28. 10.1016/0002-9343(93)90063-U . [DOI] [PubMed] [Google Scholar]
- 27.Solberg CO. Spread of Staphylococcus aureus in hospitals: causes and prevention. Scand J Infect Dis. 2000;32(6):587–95. 10.1080/003655400459478 . [DOI] [PubMed] [Google Scholar]
- 28.Cox RA, Conquest C. Strategies for the management of healthcare staff colonized with epidemic methicillin-resistant Staphylococcus aureus. J Hosp Infect. 1997;35(2):117–27. 10.1016/S0195-6701(97)90100-6 . [DOI] [PubMed] [Google Scholar]
- 29.Dawson S, Barnett J, Perry C, Jones E, MacGowan A, Reeves D. Screening for EMRSA-16 in healthcare workers. J Hosp Infect. 1997;37(1):75–7. 10.1016/S0195-6701(97)90078-5 [DOI] [PubMed] [Google Scholar]
- 30.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18(3):268–81. 10.1111/j.1469-0691.2011.03570.x . [DOI] [PubMed] [Google Scholar]
- 32.Brown DF, Wootton M, Howe RA. Antimicrobial susceptibility testing breakpoints and methods from BSAC to EUCAST. J Antimicrob Chemother. 2016;71(1):3–5. 10.1093/jac/dkv287 . [DOI] [PubMed] [Google Scholar]
- 33.EUCAST. The European Committee on Antimicrobial Susceptibility Testing. Breakpoint tables for interpretation of MICs and zone diameters. Version 6.0, 2016. Available: http://www.eucast.org/clinical_breakpoints/. Accessed 06 January 2016.
- 34.Gamblin J, Jefferies JM, Harris S, Ahmad N, Marsh P, Faust SN, et al. Nasal self-swabbing for estimating the prevalence of Staphylococcus aureus in the community. J Med Microbiol. 2013;62(Pt 3):437–40. 10.1099/jmm.0.051854-0 . [DOI] [PubMed] [Google Scholar]
- 35.Gorwitz RJ, Kruszon-Moran D, McAllister SK, McQuillan G, McDougal LK, Fosheim GE, et al. Changes in the prevalence of nasal colonization with Staphylococcus aureus in the United States, 2001–2004. J Infect Dis. 2008;197(9):1226–34. 10.1086/533494 . [DOI] [PubMed] [Google Scholar]
- 36.Kuehnert MJ, Kruszon-Moran D, Hill HA, McQuillan G, McAllister SK, Fosheim G, et al. Prevalence of Staphylococcus aureus nasal colonization in the United States, 2001–2002. J Infect Dis. 2006;193(2):172–9. 10.1086/499632 . [DOI] [PubMed] [Google Scholar]
- 37.Askarian M, Zeinalzadeh A, Japoni A, Alborzi A, Memish ZA. Prevalence of nasal carriage of methicillin-resistant Staphylococcus aureus and its antibiotic susceptibility pattern in healthcare workers at Namazi Hospital, Shiraz, Iran. Int J Infect Dis. 2009;13(5):e241–7. 10.1016/j.ijid.2008.11.026 . [DOI] [PubMed] [Google Scholar]
- 38.Treesirichod A, Hantagool S, Prommalikit O. Nasal carriage and antimicrobial susceptibility of Staphylococcus aureus among medical students at the HRH Princess Maha Chakri Sirindhorn Medical Center, Thailand: a cross sectional study. J Infect Public Health. 2013;6(3):196–201. 10.1016/j.jiph.2012.12.004 . [DOI] [PubMed] [Google Scholar]
- 39.Olsen K, Sangvik M, Simonsen GS, Sollid JU, Sundsfjord A, Thune I, et al. Prevalence and population structure of Staphylococcus aureus nasal carriage in healthcare workers in a general population. The Tromso Staph and Skin Study. Epidemiol Infect. 2013;141(1):143–52. 10.1017/S0950268812000465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Conceicao T, Santos Silva I, de Lencastre H, Aires-de-Sousa M. Staphylococcus aureus nasal carriage among patients and health care workers in Sao Tome and Principe. Microb Drug Resist. 2014;20(1):57–66. 10.1089/mdr.2013.0136 . [DOI] [PubMed] [Google Scholar]
- 41.Nulens E, Gould I, MacKenzie F, Deplano A, Cookson B, Alp E, et al. Staphylococcus aureus carriage among participants at the 13th European Congress of Clinical Microbiology and Infectious Diseases. Eur J Clin Microbiol Infect Dis. 2005;24(2):145–8. 10.1007/s10096-004-1258-6 . [DOI] [PubMed] [Google Scholar]
- 42.Aires De Sousa M, Santos Sanches I, Ferro ML, De Lencastre H. Epidemiological study of staphylococcal colonization and cross-infection in two West African Hospitals. Microb Drug Resist. 2000;6(2):133–41. 10.1089/107662900419447 . [DOI] [PubMed] [Google Scholar]
- 43.Schwarzkopf R, Takemoto RC, Immerman I, Slover JD, Bosco JA. Prevalence of Staphylococcus aureus colonization in orthopaedic surgeons and their patients: a prospective cohort controlled study. J Bone Joint Surg Am. 2010;92(9):1815–9. 10.2106/JBJS.I.00991 . [DOI] [PubMed] [Google Scholar]
- 44.Cole AM, Tahk S, Oren A, Yoshioka D, Kim YH, Park A, et al. Determinants of Staphylococcus aureus nasal carriage. Clin Diagn Lab Immunol. 2001;8(6):1064–9. 10.1128/CDLI.8.6.1064-1069.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Williams RE. Healthy carriage of Staphylococcus aureus: its prevalence and importance. Bacteriol Rev. 1963;27:56–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Noble WC. Carriage of Staphylococcus aureus and beta haemolytic streptococci in relation to race. Acta Derm Venereol. 1974;54(5):403–5. . [PubMed] [Google Scholar]
- 47.Noble WC, Valkenburg HA, Wolters CH. Carriage of Staphylococcus aureus in random samples of a normal population. J Hyg (Lond). 1967;65(4):567–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.van Belkum A, Melles DC, Nouwen J, van Leeuwen WB, van Wamel W, Vos MC, et al. Co-evolutionary aspects of human colonisation and infection by Staphylococcus aureus. Infect Genet Evol. 2009;9(1):32–47. 10.1016/j.meegid.2008.09.012 . [DOI] [PubMed] [Google Scholar]
- 49.Iyer A, Kumosani T, Azhar E, Barbour E, Harakeh S. High incidence rate of methicillin-resistant Staphylococcus aureus (MRSA) among healthcare workers in Saudi Arabia. J Infect Dev Ctries. 2014;8(3):372–8. 10.3855/jidc.3589 . [DOI] [PubMed] [Google Scholar]
- 50.Kateete DP, Namazzi S, Okee M, Okeng A, Baluku H, Musisi NL, et al. High prevalence of methicillin resistant Staphylococcus aureus in the surgical units of Mulago hospital in Kampala, Uganda. BMC Res Notes. 2011;4:326 10.1186/1756-0500-4-326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Johnston CP, Stokes AK, Ross T, Cai M, Carroll KC, Cosgrove SE, et al. Staphylococcus aureus colonization among healthcare workers at a tertiary care hospital. Infect Control Hosp Epidemiol. 2007;28(12):1404–7. 10.1086/523865 . [DOI] [PubMed] [Google Scholar]
- 52.Armstrong-Esther CA. Carriage patterns of Staphylococcus aureus in a healthy non-hospital population of adults and children. Ann Hum Biol. 1976;3(3):221–7. 10.1080/03014467600001381 . [DOI] [PubMed] [Google Scholar]
- 53.Parnaby RM, O'Dwyer G, Monsey HA, Shafi MS. Carriage of Staphylococcus aureus in the elderly. J Hosp Infect. 1996;33(3):201–6. 10.1016/S0195-6701(96)90003-1 . [DOI] [PubMed] [Google Scholar]
- 54.Zinn CS, Westh H, Rosdahl VT; Sarisa Study Group. An international multicenter study of antimicrobial resistance and typing of hospital Staphylococcus aureus isolates from 21 laboratories in 19 countries or states. Microb Drug Resist. 2004;10(2):160–8. 10.1089/1076629041310055 . [DOI] [PubMed] [Google Scholar]
- 55.Conceicao T, Coelho C, Santos Silva I, de Lencastre H, Aires-de-Sousa M. Staphylococcus aureus in former Portuguese colonies from Africa and the Far East: missing data to help fill the world map. Clin Microbiol Infect. 2015;21(9):842e1-842.e10. 10.1016/j.cmi.2015.05.010 . [DOI] [PubMed] [Google Scholar]
- 56.Tenover FC, McAllister S, Fosheim G, McDougal LK, Carey RB, Limbago B, et al. Characterization of Staphylococcus aureus isolates from nasal cultures collected from individuals in the United States in 2001 to 2004. J Clin Microbiol. 2008;46(9):2837–41. 10.1128/JCM.00480-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.European Centre for Disease Prevention and Control. Antimicrobial resistance surveillance in Europe 2013 Annual Report of the European Antimicrobial Resistance Surveillance Network (EARS-Net). Stockholm: ECDC; 2014. Available: http://ecdc.europa.eu/en/publications/Publications/antimicrobial-resistance-surveillance-europe-2013.pdf. Accessed 06 January 2016. [Google Scholar]
- 58.Aly R, Maibach HI, Strauss WG, Shinefield HR. Effects of a systemic antibiotic on nasal bacterial ecology in man. Appl Microbiol. 1970;20(2):240–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tacconelli E, De Angelis G, Cataldo MA, Pozzi E, Cauda R. Does antibiotic exposure increase the risk of methicillin-resistant Staphylococcus aureus (MRSA) isolation? A systematic review and meta-analysis. J Antimicrob Chemother. 2008;61(1):26–38. 10.1093/jac/dkm416 . [DOI] [PubMed] [Google Scholar]
- 60.Barbier F, Ruppe E, Hernandez D, Lebeaux D, Francois P, Felix B, et al. Methicillin-resistant coagulase-negative staphylococci in the community: high homology of SCCmec IVa between Staphylococcus epidermidis and major clones of methicillin-resistant Staphylococcus aureus. J Infect Dis. 2010;202(2):270–81. 10.1086/653483 . [DOI] [PubMed] [Google Scholar]
- 61.Hanssen AM, Kjeldsen G, Sollid JU. Local variants of Staphylococcal cassette chromosome mec in sporadic methicillin-resistant Staphylococcus aureus and methicillin-resistant coagulase-negative Staphylococci: evidence of horizontal gene transfer? Antimicrob Agents Chemother. 2004;48(1):285–96. 10.1128/AAC.48.1.285-296.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mihailescu R, Furustrand Tafin U, Corvec S, Oliva A, Betrisey B, Borens O, et al. High activity of Fosfomycin and Rifampin against methicillin-resistant Staphylococcus aureus biofilm in vitro and in an experimental foreign-body infection model. Antimicrob Agents Chemother. 2014;58(5):2547–53. 10.1128/AAC.02420-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wertheim HF, Vos MC, Ott A, Voss A, Kluytmans JA, Vandenbroucke-Grauls CM, et al. Mupirocin prophylaxis against nosocomial Staphylococcus aureus infections in nonsurgical patients: a randomized study. Ann Intern Med. 2004;140(6):419–25. 10.7326/0003-4819-140-6-200403160-00007 . [DOI] [PubMed] [Google Scholar]
- 64.Bode LG, Kluytmans JA, Wertheim HF, Bogaers D, Vandenbroucke-Grauls CM, Roosendaal R, et al. Preventing surgical-site infections in nasal carriers of Staphylococcus aureus. N Engl J Med. 2010;362(1):9–17. 10.1056/NEJMoa0808939 . [DOI] [PubMed] [Google Scholar]
- 65.Warnke P, Frickmann H, Ottl P, Podbielski A. Nasal screening for MRSA: different swabs—different results! PLoS One. 2014;9(10):e111627 10.1371/journal.pone.0111627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Noble WC, Williams RE, Jevons MP, Shooter RA. Some aspects of nasal carriage of staphylococci. J Clin Pathol. 1964;17(1):79–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.World Health Organization. Antimicrobial resistance: global report on surveillance 2014. Geneva: WHO 2014. Available: http://www.who.int/drugresistance/en/. Accessed 06 January 2016.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.