Abstract
Synaptic dysfunction is a hallmark of many neurodegenerative and psychiatric brain disorders, yet we know remarkably little about the mechanisms that underlie synaptic vulnerability. Although neuroinflammation and reactive gliosis are prominent in virtually every CNS disease, glia are largely viewed as passive responders to neuronal damage rather than drivers of synaptic dysfunction. This perspective is changing with the growing realization that glia actively signal with neurons and influence synaptic development, transmission, and plasticity through an array of secreted and contact-dependent signals. We propose that disruptions in neuron-glia signaling contribute to synaptic and cognitive impairment in disease. Illuminating the mechanisms by which glia influence synapse function may lead to the development of novel therapies and biomarkers for synaptic dysfunction.
Introduction
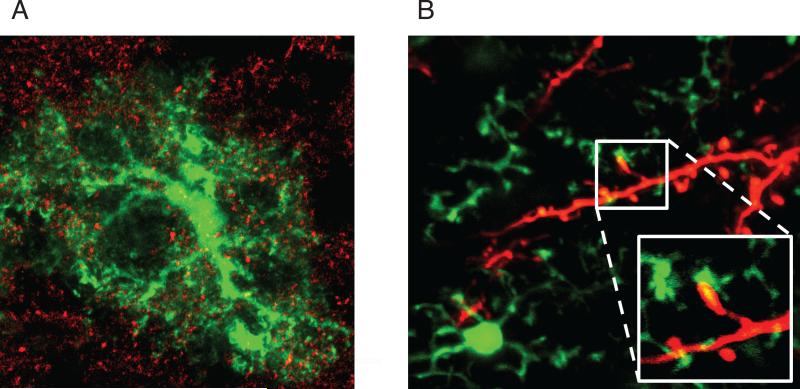
It is becoming increasingly clear that glial cells influence major aspects of synapse development, plasticity, and function. The fine processes of astrocytes and microglia intimately associate with pre- and postsynaptic elements and impact synaptic functions long thought to be intrinsic to neurons (Fig 1). In the developing and healthy brain, glia secrete soluble factors that induce synapse formation and modulation of synaptic transmission and plasticity (Fig 2A, C). Astrocytes and microglia also refine and sculpt synaptic circuits by removing excess synaptic connections (Fig. 2B). At the same time, synaptic signals influence glia by activating cell surface receptors and ion channels (Fig 2B-C). Perisynaptic astrocytes and microglia are thus well positioned to both sense early disruptions in synaptic activity and to potentially contribute to synaptic demise. It is well documented that glia are affected in late stages of nervous system pathologies1,2, but synapse dysfunction and loss can occur long before signs of neuropathology and cognitive impairment in disease3,4. The recent discoveries of astrocyte and microglia modulation of synapse function in the healthy brain suggest that glia are capable of contributing to early stages of disease, and that they perhaps may even be required for disease symptoms to develop. Understanding which neuron-glia signaling pathways are disrupted could lead to the development of new therapies as well as novel biomarkers for synaptopathies.
Figure 1.
Astrocytes and microglia interacting with synapses. A: 3-D projection view of a GFP-expressing astrocyte associating with SV2 positive synaptic terminals in red. Image courtesy of Lu Sun in Ben Barres’ Lab. B: GFP-expressing microglia in close proximity to dendrites and spines fluorescently labeled in red. Image courtesy of Jenelle Wallce in Beth Stevens’ lab.
Figure 2.
Astrocyte and microglia regulation of synaptic formation, function, and elimination, and potential implications for disease. A) Astrocytes (blue) and microglia (green) release soluble factors that regulate excitatory synapse formation and function. Aberrations in these processes may be relevant for epilepsy and schizophrenia. B) Glia refine synaptic circuits by engulfing synapses. MEGF10 and MERTK are astrocytic receptors required for synapse phagocytosis. MEGF10 and MERTK may detect synapses for elimination through bridging molecules such as Gas6 and Pros1 for Mertk that bind “eat me signals” on less active synapses. The identities of “synaptic eat me signals” for both receptors and bridging molecules for Megf10 are unknown. Microglia synapse pruning is dependent on the receptors CX3CR1 and CR3. The ligand of CX3CR1 is the neuronal CX3CL1 (fractalkine), which can either be membrane targeted or secreted. CR3 binds to C3, which may tag less active synapses and target them for elimination. Glial synapse elimination may be dysregulated in AD, ASD, schizophrenia, or other neuropsychiatric diseases. C) Astrocyes and microglia regulate synaptic transmission and plasticity. Astrocytes buffer K+ mostly through Na+/K+ ATPase and uptake glutamate through GLT1 and GLAST. Astrocytes also secrete D-serine and mediate synaptic plasticity. Microglia can impact synaptic plasticity through release of ROS, IL-1β, IL-6, and TNF. Microglia receptors required for proper synaptic function include CX3CR1 (with its ligand CX3CL1/fractalkine), as well as TREM2 and its downstream effector DAP12. These mechanisms may be important for ASD and schizophrenia.
New discoveries and new tools by which to study glia-synapse interactions are generating important mechanistic insight into neuron-glia signaling in the healthy brain. Here we will highlight recent research in this area, with focus on those pathways that may be most relevant to CNS neurodegenerative and neuropsychiatric disorders. We will then discuss how these pathways could be implicated in disease.
Astrocytes are active participants in synaptic connectivity and function
Astrocytes constitute the most abundant cell type in the CNS and play essential roles in regulating brain function. Through their close physical association with synapses, astrocytes are in the optimal position to sense and modulate synaptic activity. Moreover, recent findings implicate astrocytes in synapse formation and elimination, as well as in synaptic plasticity. It is thus likely that astrocyte dysfunction contributes to the initiation and progression of many neurological disorders.
Astrocytes have numerous processes and interact with various cellular structures including synapses and blood vessels. It is estimated that one cortical astrocyte in the mouse brain can ensheath multiple neuronal cell somas, 300-600 dendrites, and more than 100,000 synapses. More than 90% of spines in the mouse barrel cortex are in contact with astrocytic processes5, and similar synaptic ensheathment by astrocytes is also present in the human brain6. This close physical association between synapses and astrocytic processes enables astrocytes to function as the first cellular responders to various changes in synaptic activity during development and adulthood. Furthermore, fine astrocytic processes are highly dynamic, constantly modulating their association with synapses over the course of minutes7 with the degree of dynamics dependent on physiological conditions5. Astrocytes can thus continuously regulate their physical contacts with synapses.
Astrocytes are required for structural and functional maturation of synapses
Synapse formation and maturation occur in parallel with the differentiation and maturation of astrocytes. This temporal overlap is not a coincidence: the addition of astrocytes, or astrocyte-conditioned media, to purified cultures of retinal ganglion cells (RGCs) results in a significant increase in the number of functional excitatory synapses8. This initial discovery has been reproduced in many other rodent and human neuron types, and several astrocyte-secreted factors have been identified that regulate pre- and postsynaptic development and function9. Cholesterol with apolipoprotein E (APOE) from astrocytes increases the presynaptic release probability and induces synaptic transmission in vitro10. Astrocyte-derived Thrombospondins 1-5 (TSP1-5)11 and Hevin12 induce the formation of structural excitatory synapses that are postsynaptically silent. Astrocytes also release SPARC, which antagonizes the synaptogenic function of Hevin12. Glypican 4 and 6 are additional astrocyte-secreted molecules that are sufficient to induce the formation of structural excitatory synapses but also induce postsynaptic membrane insertion of GluA1-containing AMPARs13. Through unknown mechanisms, astrocytes furthermore mediate the formation of inhibitory synapses14. As mice deficient in astrocyte-derived synaptogenic molecules have reduced synapse numbers11,12, astrocytes can play a significant long-term role in regulating synaptic connectivity. Astrocytes are not only required for synapse formation and function, but also for synaptic maintenance: when astrocytes or astrocyte-secreted signals are removed from neurons in culture, synapses rapidly disappear. Thus, the formation of mature functional synapses is not an autonomous property of neurons but requires multiple astrocyte-secreted signals in vitro and in vivo.
Astrocytes mediate synapse elimination through phagocytosis
During development, neurons produce excessive numbers of synapses, and subsequent synapse elimination is required for the mature brain circuit to form. Astrocytes were recently found to express a plethora of genes that have been implicated in phagocytosis, and to physically eliminate synapses through the MEGF10 and MERTK pathways15. In developing mice deficient in the Megf10 and Mertk phagocytic receptors, RGCs show a failure of normal refinement of connections and retain excess functionally weak but intact synapses onto neurons in the lateral geniculate nucleus of the thalamus. Astrocytes thus actively participate in eliminating live synapses rather than simply cleaning up dead synaptic debris. Remarkably, synaptic engulfment by astrocytes is strongly regulated by neighboring neuronal activity. Bilateral blocking of retinal activity led to fewer synapses being pruned by astrocytes in the thalamus; unilateral blocking of retinal activity led to preferential pruning of the silenced synapses. Astrocytes were found to engulf synapses throughout adulthood, suggesting that astrocytes may be active participants in the synaptic refinement process underlying critical period plasticity as well as other forms of learning and memory.
The continued astrocyte-mediated pruning of synapses in adult rodent brains is consistent not only with a role in synaptic remodeling underlying learning but suggests the possibility of an important role in synapse turnover. Given that most neurons throughout the brain are not replaced during adulthood, special mechanisms that turnover heavily used synaptic membranes that may undergo biochemical degradation with use and age may be especially important in the brain. Interestingly, the rate of synapse pruning by astrocytes progressively decreases with age15, raising important questions about whether the declining rate of this engulfment may contribute to cognitive decline, and whether drugs that speed up synapse removal by astrocytes may enhance cognition in the elderly. It may also help explain the timing of the striking decrease in synapse number occurring in human brains during puberty and adolescence that then stabilizes by adulthood.
Astrocytes modulate synaptic transmission and plasticity
Astrocytes actively participate in synaptic transmission and contribute to synaptic plasticity. The best-studied functions of astrocytes include potassium buffering during neuronal activity and uptake of the neurotransmitters glutamate (by GLT-1 and GLAST) and GABA (by GAT-1). These fundamental functions of astrocytes are absolutely essential for maintaining synaptic activity, and dysregulation of these processes leads to pathological conditions such as seizures and neurological dysfunction16,17. Recent studies additionally demonstrate that astrocyte-secreted glutamine is critical for sustained glutamate release by neurons indicating that astrocytes are active participants in the production of the neurotransmitters used by neurons18.
Several secreted astrocytic factors are capable of regulating synaptic plasticity. Sparc knockout mice show an increase in excitatory synapse function and impaired LTP19, possibly due to the effects of altered Hevin-SPARC antagonism on AMPAR recruitment to the postsynaptic surface. Recent studies have also shown that D-serine secreted from astrocytes is involved in synaptic plasticity by functioning as a coagonist of NMDARs20. Along with D-serine, large numbers of studies have suggested that ATP and glutamate may be secreted from astrocytes via Ca2+-dependent vesicular exocytosis and contribute to synaptic strength and plasticity21. However, recent studies cast serious doubt on those conclusions. The previous in vitro model of cultured astrocytes displays non-physiological properties and contains a significant number of contaminating neurons. In addition, the transgenic mouse lines used to provide genetic evidence of vesicular mediated neurotransmitter release from astrocytes turned out not to specifically target astrocytes22.
Whatever the mechanisms, evidence of astrocytes actively controlling synaptic plasticity is increasing. A recent study suggests that human astrocytes may even be better than rodent astrocytes in controlling synaptic plasticity events underlying learning23.
Microglia Survey and Sculpt Developing Synapses
Many diseases of the CNS are characterized by neuroinflammation, especially in late stages of the disease. As the resident macrophages and phagocytes of the CNS, microglia have been studied in depth in this context1,2. It is now appreciated that microglia also play important roles in structurally shaping and functionally modulating the connectivity of the developing and healthy brain. Understanding microglia functions in healthy settings can provide new insight into their potential contributions to synapse loss and dysfunction at early stages of pathology, prior to overt neurodegeneration and neuroinflammation.
Microglia are well positioned to impact synaptic function (Fig 1B). Their processes constantly extend and retract as they survey their local environment. In the adult mouse cortex, the speed is approximately 1 μm/min, so that microglia are estimated to scan the entire brain volume over the course of a few hours24. Microglia processes transiently interact with boutons and spines, and direct contacts between microglia and synaptic elements have been confirmed by EM25. Each microglial cell can thus affect many synapses, as well as quickly change the motility of its processes in response to extracellular stimuli24.
Microglia contribute to synapse elimination and formation
Microglia can promote both structural synapse elimination and formation. Phagocytic microglia prune synaptic connections during development by engulfing pre- and postsynaptic elements in the hippocampus and retinogeniculate system during the first weeks after birth26,27. Although primarily an early developmental process, synapse engulfment in visual cortex can be observed during the critical period in response to changing visual experience25. In contrast, loss of microglia reduces spine formation in the adult and juvenile mouse motor cortex during motor learning. Microglia mediate this spine formation through BDNF, but as microglia express low levels of BDNF compared to neurons, further work is needed to understand the underlying mechanisms28.
The early postnatal pruning process is dependent on the receptors CX3CR1 and complement receptor 3 (CR3) in the hippocampus and thalamus, respectively. These receptors, which in the brain parenchyma are microglia-specific, mediate pruning using signals from neurons. The only known CX3CR1 ligand CX3CL1 (fractalkine) is primarily neuronal, and regulates microglia phagocytosis of synapses through an unknown mechanism26,29. C1q, the initiator of the classical complement cascade, is produced by presynaptic retinal neurons in the thalamus during the peak of pruning and is, along with downstream C3, required for synapse elimination30. It is hypothesized that C1q induces deposition of the CR3 ligand C3 onto synapses, thereby tagging them for elimination by microglia27. Activity may be involved in regulating C1q and C3 deposition. Microglia-mediated pruning in the thalamus is an activity-dependent process, as microglia preferentially engulf less active presynaptic inputs over more active ones. The C3 tag could therefore specifically mark weak synapses for removal. Significantly, microglia engulfment influences adult circuitry: in the absence of CR3, synapse densities remain elevated in the thalamus into adulthood, and CX3CR1 knockout mice have aberrant long-range functional connectivity27,31.
Microglia promote functional synaptic maturation
Microglia regulate functional synaptic maturation. Synapses in mice lacking CX3CR1 show a delayed establishment of normal electrophysiological characteristics during development26. Although impaired synaptic pruning could contribute to these deficits, CX3CR1 may also be required for regulating the release of soluble factors that mediate synaptic maturation. In accordance with the latter idea, developmental phenotypes are observed in mice expressing a truncated form of DAP1232. DAP12 is a transmembrane protein that signals downstream of multiple receptors expressed on myeloid cells, including TREM2 (see below)33. Animals with truncated DAP12 show impaired synaptic maturation, and cultured microglia derived from these mice express higher levels of the enzyme iNOS, required for nitric oxide production, as well as of IL-6 and IL-1β32. Secretion of one or a combination of these three factors may thus mediate the aberrant development of synaptic properties.
Microglia can regulate synaptic plasticity
Microglia-secreted factors can regulate synaptic function in the juvenile and mature brain, after the establishment of proper synaptic connections. IL-1β, which is primarily expressed by microglia, is implicated in regulating LTP in the hippocampus34,35. Aberrant IL-1β signaling furthermore underlies deficits in hippocampal LTP in animals lacking CX3CR136. Under stress from LPS and hypoxia, microglia release reactive oxygen species (ROS) that cause hippocampal LTD37. Microglia may also be contributing to homeostatic plasticity. TNF-α released by glia is required for the synaptic scaling following a long-term reduction in activity38. As TNF-α expression is highly enriched in microglia compared to other cells in the brain, microglia may mediate this effect35.
The ability of microglia to create and remove synapses, as well as change the strength of existing ones, appears to be crucial for proper behavior. Global CX3CR1 knockout animals have deficits in social behavior, which could be due to impaired developmental synaptic pruning and maturation, or to continuous deficits in plasticity31. By an unknown mechanism, the loss of microglia BDNF furthermore reduces motor learning in mice only a few days after recombination28. These and other studies thus reveal microglia-synapse interactions as potential key regulators of overall nervous system function.
Do Microglia and Astrocytes Mediate Synaptic Dysfunction in Disease?
Synapse dysfunction is a hallmark of many neurological diseases and disorders. The growing realization that glia critically influence synaptic development and function in the healthy brain suggests that disruption in neuron-glia signaling may contribute to synaptic and cognitive impairment in the diseased CNS. In support of this idea, human genetic studies have identified a number of glial genes that increase the risk of diseases that feature cognitive dysfunction39-43. Here we review recent findings suggesting that glia are important contributors to development of neurological disease, and discuss possible mechanisms through which astrocytes and microglia could mediate synaptic and cognitive dysfunction.
Neurodevelopmental and Neuropsychiatric Disorders
Alterations in Microglia and Immune Pathways in Autism Spectrum Disorder and Schizophrenia
The majority of microglial cells derive from myeloid-lineage cells in the yolk sac and migrate into the brain very early in embryonic development44-46. Microglia are therefore present from early steps of nervous system development, potentially allowing them to contribute to synaptic deficits and the pathobiology of autism spectrum disorder (ASD) or schizophrenia. In support of a connection between microglia and these disorders, RNA-sequencing reveals a strong association between ASD and a module of co-expressed genes related to microglia activation47. The transcriptional data is supported by PET imaging of live patients, which suggests increased microglia activation in the brains of individuals with schizophrenia48. Although the potential link between microglia and ASD/schizophrenia is intriguing, it is not yet clear what changes in microglia ‘activation’ tell us about the pathobiology of these disorders. Do microglia contribute to synaptic and cognitive deficits in these diseases? Intriguingly, epidemiological studies suggest that infections in pregnant women increase the risk of ASD and schizophrenia in the offspring. These results can be replicated in animal models, where immune activation in the pregnant mother is sufficient to induce behavioral deficits in the offspring49. Immune changes are thus, at least in animals, sufficient to initiate symptoms reminiscent of neurodevelopmental and neuropsychiatric disease.
Although it is not clear whether microglia mediate the consequences of infection during pregnancy, known mechanisms of microglia-synapse interactions give insight into how microglia could contribute to neurodevelopmental and neuropsychiatric disease. One possibility is that genetic or environmental perturbations dysregulate microglia-mediated synapse elimination. ASD and schizophrenia both feature synaptic and connectivity defects50, and altered pruning of cortical synapses is suggested to underlie schizophrenia51. This idea is supported in the CX3CR1 knockout mice, which have impaired synaptic pruning, social behavior, and functional long-range connectivity31. Alterations to synapses and dendritic spines have also been reported in several mouse models of ASD50. Rett Syndrome mice are among these mouse models, and disease progression in these animals appears to be affected by microglia52. The involvement of microglia in mouse models of this disease is, however, controversial53. Alternatively, or concurrently, microglia may be modulating the maturation or function of synapses. Microglial release of inflammatory molecules such as interleukins, TNF-α, or ROS regulates synaptic maturation and plasticity (see above). These factors could induce disease by both impairing synaptic maturation early in development, and by being aberrantly released in the adult.
Disruptions in Astrocyte-Synapse Signaling
A recent genome wide association study (GWAS) has found genetic evidence for important roles of astrocytes in schizophrenia54. Many of the associated genes are implicated in various aspects of astrocyte-synapse interactions, suggesting that schizophrenia may arise from dysregulation of normal functions of astrocytes at synapses. One of the important features of astrocyte-synapse interactions that may be disrupted in here is glutamate uptake. Astrocyte glutamate uptake directly couples astrocytes to synaptic transmission, and dysregulation of this process constitutes a strong insult to synaptic and behavioral function. In accordance, expression of GLT-1 and glutamine synthetase is altered in patients with schizophrenia and ASD55. Deleting GLT-1 from astrocytes in adolescent mice results in pathological repetitive behaviors in affected animals, such as excessive grooming with increased seizure sensitivity, reminiscent of humans with ASD56. Furthermore, human mutations in enzymes involved in the production, stability, and degradation of D-serine have been genetically linked to schizophrenia57. Mice with decreased D-serine displays behavior abnormalities consistent with hypofunction of NMDA neurotransmission, similar to NMDA-related alteration in schizophrenia patients58.
The ability of astrocytes to induce synapse formation may be detrimental when not appropriately regulated. The neuronal receptor for the synaptogenic TSPs was found to be the calcium channel subunit α2δ1 (Cacna2d1) and the TSPs-α2δ1binding is blocked by the antiepileptic drug gabapentin59. Blocking the formation of a hyperexcitable network after injury with gabapentin prevents posttraumatic epilepsy60 suggesting that an abnormal increase in excitatory synapse formation by astrocytes is involved in neuropathic pain and epilepsy.
A disruption of the proper balance between synapse formation and elimination is a feature of the pathophysiology of neuropsychiatric disorders. In particular, the recent identification of a novel and highly activity-dependent role for astrocytes in constantly phagocytosing synapses15 suggests the possibility that astrocyte dysfunction in synapse elimination might contribute to the pathogenesis of major depressive disorder, bipolar disorder, ASD and schizophrenia. For schizophrenia in particular, this hypothesis has strong genetic support, as schizophrenia-associated SNPs have been identified in the TSP1 gene as well as in the MEGF10 phagocytic pathway (MEGF10, GLUP1 and ABCA1)61. Might the well-established effectiveness of electroconvulsive therapy to stimulate improvement in many psychiatric disorders be explained by the stimulation or rebooting of astrocyte mediated synapse engulfment, given its strong activity dependence? Although it is difficult to use postmortem studies to answer this type of questions, the recent development of methods to generate human astrocytes from induced pluripotent stem cells (iPSCs)62 makes it possible to directly determine whether astrocytes from patients with various psychiatric and neurological disorders have a genetically altered ability to engulf synapses and to develop drugs that alter this rate.
Alzheimer's disease and Neurodegenerative disease
Microglial activation and reactive astrogliosis are cardinal features of Alzheimer's disease (AD) and other neurodegenerative diseases (NDD) including Huntington's disease, Parkinson's disease, and glaucoma2. Although reactive gliosis and neuroinflammation have long been considered to be secondary events caused by neurodegeneration, recent GWAS and other integrated network studies find microglia- and astrocyte-related pathways to be central to AD pathogenesis41,42,63,64 Synapse loss and dysfunction is an early hallmark of AD, where synapse loss is the strongest correlate of cognitive decline3,4; however, mechanisms by which CNS synapses are aberrantly eliminated in the AD brain are not yet clear. The emerging role of astrocytes and microglia in synaptic homeostasis and pruning in the healthy brain therefore suggests the intriguing hypothesis that glia may also play a pivotal role in the dysfunction of synapses early in AD and other NDDs. Below we review emerging evidence on the potential contribution of microglia and astrocytes to synapse dysfunction and loss in AD.
Microglia and Synapse Dysfunction in AD: Emerging data and paths forward
Recent studies reveal associations in genes related to immune signaling in AD and other NDDs, raising questions about the biological significance of these associations. One gene of particular interest is TREM2, an innate immune receptor expressed on microglia and cells of the monocyte lineage. Human genetic studies identified rare mutations in TREM2 as a risk factor for AD and other NDDs41-43; however, the effects of AD- and NDD-associated TREM2 mutations on TREM2 biology remain elusive. Studies in the peripheral immune system indicate that TREM2 can act as a negative regulator of inflammatory cytokine and Toll like receptor (TLR) responses, as well as of phagocytosis, by pairing with the signaling adapter DAP1233. Thus, mutations in TREM2 signaling could potentially promote AD pathogenesis by affecting phagocytosis and neuroinflammation. In the AD brain, activated microglia often surround amyloid plaques, where they may have a double-edged role of clearing amyloid β (Aβ) and contributing to neurotoxicity through excessive cytokine release2. Several studies using AD transgenic mice in which TREM2 was deleted have found fewer microglia and monocytes surrounding Aβ plaques with varying impacts on plaque burden65-67; impact of TREM2 deletion on tau pathology still needs to be explored. Interestingly, TREM2 or DAP12 mutations alone causes progressive cognitive impairment in Nasu-Hakola disease39,40, suggesting that microglial TREM2 may play a major role in synaptic health. Important questions that still need to be addressed are the potential role of TREM2 in microglia-synapse interactions in the healthy brain, and how TREM2 deficiency or mutations contributes to synaptic and cognitive impairment in the AD brain.
Several genes associated with the classical complement cascade have emerged as susceptibility genes in AD including ApoJ/Clusterin, and complement receptor 1 (CR1)2. As discussed previously, complement is a key mechanism underlying synaptic pruning and microglia mediated engulfment of synapses in the developing brain27,30, raising the question of whether this pathway could drive aberrant engulfment of synapses in AD and other NDDs. Indeed, complement cascade proteins are profoundly upregulated in late stage AD brain68. A C1q-deficient mouse model of AD had less neuropathology, astrogliosis and plaque deposition, suggesting a potential detrimental role of the classical complement pathway69. Interestingly, Aβ and tau aggregates have been shown to induce microglial and complement activation70,71. Given their major roles in eliminating synapses in development, we hypothesize that microglia and complement are reactivated in the AD brain to aberrantly mediate synaptic dysfunction and loss. It will be important to address the functional role of microglia and complement on synaptic health early in disease and independent of plaques and tangles.
Do Astrocytes Drive Early Synaptic Dysfunction in AD?
Similar to microglia, reactive astrocytes surround the sites of Aβ deposits in human AD brains and in animal models of AD where they may play either beneficial or deleterious roles in disease progression. Astrocytes can help clear Aβ through degradation and phagocytosis, thus contributing to reduced Aβ-mediated neurotoxicity; conversely, reactive astrocytes can contribute to AD progression through releasing pro-inflammatory factors and inducing microglial activation2.
Recent studies have shown that astrocytes in AD alter their gene expression patterns, and induce synaptic dysfunction and behavioral deficits at early stages of AD pathophysiology. Adenosine receptor A2A is highly upregulated in reactive astrocytes and contributes to long-term memory loss, potentially by affecting astrocyte-synapse interactions72. Monoamine oxidase-B mediated GABA production was also increased in reactive astrocytes in AD model mice and human patients. Inhibiting tonic release of GABA rescued impaired synaptic plasticity and memory loss in these AD mice73.
Among many genes associated with AD, APOE genotype is by far the strongest genetic risk factor for late onset AD, and astrocytes are the major source of APOE in the brain. In humans, there are three common APOE variants, which differ by a single amino acid change: E2, E3, and E4. The presence of two copies of APOE4 increases the risk of developing AD by ~12 fold, whereas the E2 variant is associated with a ~2-fold decreased risk for developing AD. Individuals with APOE4 also show reduced brain glucose metabolism, altered neural activity and early deposition of Aβ even before developing any cognitive symptoms74; however, how APOE4 contributes to AD pathogenesis is unclear. APOE4 may contribute to Aβ aggregation by decreasing rate of its clearance75. Moreover, mice that express the human APOE4 variant show fewer dendritic spines and reduced branching in cortical neurons with decreased production of glutamate from the presynaptic compartment76. It is interesting to note that these ApoE4 knock-in mice do not develop Aβ plaques, suggesting that APOE4 can impair synaptic plasticity and homeostasis independently of plaque formation. Whether such synaptic dysfunction originates from impaired function of APOE4-expressing astrocytes at synapses, and whether correcting those functions of astrocytes can improve AD pathophysiology, would be intriguing questions to address.
Given the steep age-dependent decline of the rate of synapse eating by astrocytes, an important question for future work is whether a slower rate of synapse turnover in the aged brain leads to an ever-increasing accumulation of “senescent” synapses. This possibility is strongly suggested by the recent discovery of an exponential elevation of complement component C1q during aging in both mouse and human brains77. As C1q is a lectin-like protein that can recognize and bind to aging, dying, and altered membranes, we hypothesize that its accumulation at synapses reflects the build-up of aging senescent synapses. As these C1q-binding synapses are thus much more vulnerable to attack by the classical complement cascade, it would be important to determine whether drugs that promote astrocyte engulfment of synapses, and thus improve synaptic turnover, might not only help prevent cognitive decline but also the greater vulnerability to AD that is associated with normal brain aging.
CONCLUSIONS & PERSPECTIVES
The recent findings that glial cells, both astrocytes and microglia, profoundly control synapse formation, function, plasticity, and elimination, represent a paradigm shift in neurobiology. It is unlikely that important neurobiological processes in development, adulthood or disease can be understood by a sole focus on understanding neurons. This has been the repeated lesson in biomedical research in many other fields outside of neurobiology as well. It was long dogma in the cancer field that cancer could be understood by a sole focus on understanding genetic alterations in the cancer cells themselves. Recent studies, however, demonstrate that many important properties of tumors can only be understood by elucidating how these cancer cells interact with non-malignant cells in their environment. One suspects that the same principle will turn out to be true in diseases of other tissues, for instance the pancreas where the cause of beta cell death in the islets in Type 2 diabetes is still unexplained. Most likely this gap in knowledge is caused by our limited understanding of what the surrounding cell types are or how they interact with the beta cells.
The findings that rodent glial cells powerfully control synapses raise profound questions for further research. First, how do the properties of human glial cells, both astrocytes and microglia, compare to those of rodent cells? Might human glia have altered or even more profound abilities to control synapse formation, function, and elimination? Second, to what extent are brain disorders long thought to be caused by purely neuronal defects, actually be disorders of glial cells or of neuron-glial interactions? The development of methods to generate human glia from iPSCs offers a powerful tool to address these questions in future studies. Finally, as synapse loss is the strongest correlate of cognitive decline in AD, what is the role of glia in early synaptic dysfunction and elimination? Answering these questions will greatly increase our understanding of nervous system function, and may help guide the development of novel treatments for CNS diseases.
Acknowledgements
We thank Lu Sun, Jenelle Wallace and Venkatesh Murthy for providing images used in Figure 1. We also thank Soyon Hong and Emily Lehrman for helpful discussions and critical reading of the manuscript.
Footnotes
Competing financial interests
The authors declare competing financial interests: Ben Barres is a co-founder of Annexon Biosciences, Inc., a company making new drugs to treat neurological disorders, and Beth Stevens is on the scientific advisory board of Annexon Biosciences.
References
- 1.Ransohoff RM, Perry VH. Annu. Rev. Immunol. 2009;27:119–145. doi: 10.1146/annurev.immunol.021908.132528. [DOI] [PubMed] [Google Scholar]
- 2.Wyss-Coray T, Rogers J. Inflammation in Alzheimer Disease—A Brief Review of the Basic Science and Clinical Literature. Cold Spring Harbor Perspectives in Medicine. 2012;2 doi: 10.1101/cshperspect.a006346. doi:10.1101/cshperspect.a006346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Terry RD, et al. Physical basis of cognitive alterations in alzheimer's disease: Synapse loss is the major correlate of cognitive impairment. Annals of Neurology. 1991;30:572–580. doi: 10.1002/ana.410300410. doi:10.1002/ana.410300410. [DOI] [PubMed] [Google Scholar]
- 4.DeKosky ST, S. S. W., Styren SD. Structural correlates of cognition in dementia: quantification and assessment of synapse change. Neurodegeneration. 1996;5:5. doi: 10.1006/neur.1996.0056. [DOI] [PubMed] [Google Scholar]
- 5.Genoud C, et al. Plasticity of astrocytic coverage and glutamate transporter expression in adult mouse cortex. PLoS biology. 2006;4:e343. doi: 10.1371/journal.pbio.0040343. doi:10.1371/journal.pbio.0040343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Witcher MR, et al. Three-dimensional relationships between perisynaptic astroglia and human hippocampal synapses. Glia. 2010;58:572–587. doi: 10.1002/glia.20946. doi:10.1002/glia.20946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Haber M, Zhou L, Murai KK. Cooperative astrocyte and dendritic spine dynamics at hippocampal excitatory synapses. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2006;26:8881–8891. doi: 10.1523/JNEUROSCI.1302-06.2006. doi:10.1523/JNEUROSCI.1302-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ullian EM, Sapperstein SK, Christopherson KS, Barres BA. Control of synapse number by glia. Science. 2001;291:657–661. doi: 10.1126/science.291.5504.657. doi:10.1126/science.291.5504.657. [DOI] [PubMed] [Google Scholar]
- 9.Clarke LE, Barres BA. Emerging roles of astrocytes in neural circuit development. Nat Rev Neurosci. 2013;14:311–321. doi: 10.1038/nrn3484. doi:10.1038/nrn3484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mauch DH, et al. CNS synaptogenesis promoted by glia-derived cholesterol. Science. 2001;294:1354–1357. doi: 10.1126/science.294.5545.1354. doi:10.1126/science.294.5545.1354. [DOI] [PubMed] [Google Scholar]
- 11.Christopherson KS, et al. Thrombospondins are astrocyte-secreted proteins that promote CNS synaptogenesis. Cell. 2005;120:421–433. doi: 10.1016/j.cell.2004.12.020. doi:10.1016/j.cell.2004.12.020. [DOI] [PubMed] [Google Scholar]
- 12.Kucukdereli H, et al. Control of excitatory CNS synaptogenesis by astrocyte-secreted proteins Hevin and SPARC. Proceedings of the National Academy of Sciences of the United States of America. 2011;108:E440–449. doi: 10.1073/pnas.1104977108. doi:10.1073/pnas.1104977108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Allen NJ, et al. Astrocyte glypicans 4 and 6 promote formation of excitatory synapses via GluA1 AMPA receptors. Nature. 2012;486:410–414. doi: 10.1038/nature11059. doi:10.1038/nature11059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hughes EG, Elmariah SB, Balice-Gordon RJ. Astrocyte secreted proteins selectively increase hippocampal GABAergic axon length, branching, and synaptogenesis. Molecular and cellular neurosciences. 2010;43:136–145. doi: 10.1016/j.mcn.2009.10.004. doi:10.1016/j.mcn.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chung WS, et al. Astrocytes mediate synapse elimination through MEGF10 and MERTK pathways. Nature. 2013;504:394–400. doi: 10.1038/nature12776. doi:10.1038/nature12776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rangroo Thrane V, et al. Ammonia triggers neuronal disinhibition and seizures by impairing astrocyte potassium buffering. Nat Med. 2013;19:1643–1648. doi: 10.1038/nm.3400. doi:10.1038/nm.3400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tanaka K, et al. Epilepsy and exacerbation of brain injury in mice lacking the glutamate transporter GLT-1. Science. 1997;276:1699–1702. doi: 10.1126/science.276.5319.1699. [DOI] [PubMed] [Google Scholar]
- 18.Tani H, et al. A local glutamate-glutamine cycle sustains synaptic excitatory transmitter release. Neuron. 2014;81:888–900. doi: 10.1016/j.neuron.2013.12.026. doi:10.1016/j.neuron.2013.12.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jones EV, et al. Astrocytes control glutamate receptor levels at developing synapses through SPARC-beta-integrin interactions. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2011;31:4154–4165. doi: 10.1523/JNEUROSCI.4757-10.2011. doi:10.1523/JNEUROSCI.4757-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Henneberger C, Papouin T, Oliet SH, Rusakov DA. Long-term potentiation depends on release of D-serine from astrocytes. Nature. 2010;463:232–236. doi: 10.1038/nature08673. doi:10.1038/nature08673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Halassa MM, Haydon PG. Integrated Brain Circuits: Astrocytic Networks Modulate Neuronal Activity and Behavior. Annual Review of Physiology. 2010;72:335–355. doi: 10.1146/annurev-physiol-021909-135843. doi:doi:10.1146/annurev-physiol-021909-135843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fujita T, et al. Neuronal transgene expression in dominant-negative SNARE mice. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2014;34:16594–16604. doi: 10.1523/JNEUROSCI.2585-14.2014. doi:10.1523/JNEUROSCI.2585-14.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Han X, et al. Forebrain engraftment by human glial progenitor cells enhances synaptic plasticity and learning in adult mice. Cell stem cell. 2013;12:342–353. doi: 10.1016/j.stem.2012.12.015. doi:10.1016/j.stem.2012.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nimmerjahn A, Kirchhoff F, Helmchen F. Resting Microglial Cells Are Highly Dynamic Surveillants of Brain Parenchyma in Vivo. Science. 2005;308:1314–1318. doi: 10.1126/science.1110647. [DOI] [PubMed] [Google Scholar]
- 25.Tremblay M-È, Lowery RL, Majewska AK. PLoS Biol. 2010;8:e1000527. doi: 10.1371/journal.pbio.1000527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Paolicelli RC, et al. Science. 2011;333:1456–1458. doi: 10.1126/science.1202529. [DOI] [PubMed] [Google Scholar]
- 27.Schafer DP, et al. Neuron. 2012;74:691–705. doi: 10.1016/j.neuron.2012.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Parkhurst CN, et al. Cell. Vol. 155. Elsevier Inc.; 2013. pp. 1596–1609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Harrison JK, et al. Role for neuronally derived fractalkine in mediating interactions between neurons and CX3CR1-expressing microglia. Proceedings of the National Academy of Sciences. 1998;95:10896–10901. doi: 10.1073/pnas.95.18.10896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stevens B, et al. Cell. 2007;131:1164–1178. doi: 10.1016/j.cell.2007.10.036. [DOI] [PubMed] [Google Scholar]
- 31.Zhan Y, et al. Nature Publishing Group. Vol. 17. Nature Publishing Group; 2014. pp. 400–406. [Google Scholar]
- 32.Roumier A, et al. Prenatal Activation of Microglia Induces Delayed Impairment of Glutamatergic Synaptic Function. PLoS ONE. 2008;3:e2595. doi: 10.1371/journal.pone.0002595. doi:10.1371/journal.pone.0002595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Colonna M. TREMs in the immune system and beyond. Nat Rev Immunol. 2003;3:445–453. doi: 10.1038/nri1106. [DOI] [PubMed] [Google Scholar]
- 34.Williamson LL, Bilbo SD. Brain Behavior and Immunity. Vol. 30. Elsevier Inc.; 2013. pp. 186–194. [DOI] [PubMed] [Google Scholar]
- 35.Zhang Y, et al. An RNA-Sequencing Transcriptome and Splicing Database of Glia, Neurons, and Vascular Cells of the Cerebral Cortex. The Journal of Neuroscience. 2014;34:11929–11947. doi: 10.1523/JNEUROSCI.1860-14.2014. doi:10.1523/jneurosci.1860-14.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rogers JT, et al. Journal of Neuroscience. 2011;31:16241–16250. doi: 10.1523/JNEUROSCI.3667-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang J, et al. Neuron. Vol. 82. Elsevier Inc.; 2014. pp. 195–207. [DOI] [PubMed] [Google Scholar]
- 38.Stellwagen D, Malenka RC. Nature. 2006;440:1054–1059. doi: 10.1038/nature04671. [DOI] [PubMed] [Google Scholar]
- 39.Paloneva J, et al. Loss-of-function mutations in TYROBP (DAP12) result in a presenile dementia with bone cysts. Nat Genet. 2000;25:357–361. doi: 10.1038/77153. [DOI] [PubMed] [Google Scholar]
- 40.Paloneva J, et al. Mutations in Two Genes Encoding Different Subunits of a Receptor Signaling Complex Result in an Identical Disease Phenotype. The American Journal of Human Genetics. 2002;71:656–662. doi: 10.1086/342259. doi: http://dx.doi.org/10.1086/342259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Guerreiro R, et al. TREM2 variants in Alzheimer's disease. N Engl J Med. 2013;368:117–127. doi: 10.1056/NEJMoa1211851. doi:10.1056/NEJMoa1211851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jonsson T, et al. N Engl J Med. 2013;368:107–116. doi: 10.1056/NEJMoa1211103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rayaprolu S, et al. TREM2 in neurodegeneration: evidence for association of the p.R47H variant with frontotemporal dementia and Parkinson's disease. Molecular Neurodegeneration. 2013;8:19–19. doi: 10.1186/1750-1326-8-19. doi:10.1186/1750-1326-8-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ginhoux F, et al. Science. 2010;330:841–845. doi: 10.1126/science.1194637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schulz C, et al. A Lineage of Myeloid Cells Independent of Myb and Hematopoietic Stem Cells. Science. 2012;336:86–90. doi: 10.1126/science.1219179. doi:10.1126/science.1219179. [DOI] [PubMed] [Google Scholar]
- 46.Kierdorf K, et al. Microglia emerge from erythromyeloid precursors via Pu.1- and Irf8-dependent pathways. Nat Neurosci. 2013;16:273–280. doi: 10.1038/nn.3318. doi: http://www.nature.com/neuro/journal/v16/n3/abs/nn.3318.html#supplementary-information. [DOI] [PubMed] [Google Scholar]
- 47.Voineagu I, et al. Nature. Vol. 474. Nature Publishing Group; 2011. pp. 380–384. [Google Scholar]
- 48.van Berckel BN, et al. Microglia Activation in Recent-Onset Schizophrenia: A Quantitative (R)-[11C]PK11195 Positron Emission Tomography Study. Biological Psychiatry. 2008;64:820–822. doi: 10.1016/j.biopsych.2008.04.025. doi: http://dx.doi.org/10.1016/j.biopsych.2008.04.025. [DOI] [PubMed] [Google Scholar]
- 49.Patterson PH. Maternal infection and immune involvement in autism. Trends in Molecular Medicine. 2011;17:389–394. doi: 10.1016/j.molmed.2011.03.001. doi: http://dx.doi.org/10.1016/j.molmed.2011.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Penzes P, Cahill ME, Jones KA, VanLeeuwen J-E, Woolfrey KM. Nature Publishing Group. Vol. 14. Nature Publishing Group; 2011. pp. 285–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Feinberg I. Schizophrenia: caused by a fault in programmed synaptic elimination during adolescence? J Psychiatr Res. 1982-1983;17:319–334. doi: 10.1016/0022-3956(82)90038-3. [DOI] [PubMed] [Google Scholar]
- 52.Derecki NC, et al. Nature. Vol. 483. Nature Publishing Group; 2012. pp. 105–109. [Google Scholar]
- 53.Wang J, et al. Wild-type microglia do not reverse pathology in mouse models of Rett syndrome. Nature. 2015;521:E1–E4. doi: 10.1038/nature14444. doi:10.1038/nature14444 http://www.nature.com/nature/journal/v521/n7552/abs/nature14444.html#supplementary-information. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Goudriaan A, et al. Specific glial functions contribute to schizophrenia susceptibility. Schizophr Bull. 2014;40:925–935. doi: 10.1093/schbul/sbt109. doi:10.1093/schbul/sbt109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Matute C, Melone M, Vallejo-Illarramendi A, Conti F. Increased expression of the astrocytic glutamate transporter GLT-1 in the prefrontal cortex of schizophrenics. Glia. 2005;49:451–455. doi: 10.1002/glia.20119. doi:10.1002/glia.20119. [DOI] [PubMed] [Google Scholar]
- 56.Aida T, et al. Astroglial Glutamate Transporter Deficiency Increases Synaptic Excitability and Leads to Pathological Repetitive Behaviors in Mice. Neuropsychopharmacology : official publication of the American College of Neuropsychopharmacology. 2015 doi: 10.1038/npp.2015.26. doi:10.1038/npp.2015.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ma TM, et al. Pathogenic disruption of DISC1-serine racemase binding elicits schizophrenia-like behavior via D-serine depletion. Mol Psychiatry. 2013;18:557–567. doi: 10.1038/mp.2012.97. doi:10.1038/mp.2012.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Matsuno H, et al. A Naturally Occurring Null Variant of the NMDA Type Glutamate Receptor NR3B Subunit Is a Risk Factor of Schizophrenia. PLoS One. 2015;10:e0116319. doi: 10.1371/journal.pone.0116319. doi:10.1371/journal.pone.0116319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Eroglu C, et al. Gabapentin receptor alpha2delta-1 is a neuronal thrombospondin receptor responsible for excitatory CNS synaptogenesis. Cell. 2009;139:380–392. doi: 10.1016/j.cell.2009.09.025. doi:10.1016/j.cell.2009.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Li H, et al. Gabapentin decreases epileptiform discharges in a chronic model of neocortical trauma. Neurobiol Dis. 2012;48:429–438. doi: 10.1016/j.nbd.2012.06.019. doi:10.1016/j.nbd.2012.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Chen X, et al. Apoptotic engulfment pathway and schizophrenia. PloS one. 2009;4:e6875. doi: 10.1371/journal.pone.0006875. doi:10.1371/journal.pone.0006875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pasca SP, Panagiotakos G, Dolmetsch RE. Generating human neurons in vitro and using them to understand neuropsychiatric disease. Annual review of neuroscience. 2014;37:479–501. doi: 10.1146/annurev-neuro-062012-170328. doi:10.1146/annurev-neuro-062012-170328. [DOI] [PubMed] [Google Scholar]
- 63.Lambert J-C, et al. Meta-analysis of 74,046 individuals identifies 11 new susceptibility loci for Alzheimer's disease. Nat Genet. 2013;45:1452–1458. doi: 10.1038/ng.2802. doi:10.1038/ng.2802 http://www.nature.com/ng/journal/v45/n12/abs/ng.2802.html#supplementary-information. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhang B, et al. Integrated Systems Approach Identifies Genetic Nodes and Networks in Late-Onset Alzheimer's Disease. Cell. 2013;153:707–720. doi: 10.1016/j.cell.2013.03.030. doi: http://dx.doi.org/10.1016/j.cell.2013.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ulrich JD, et al. Altered microglial response to A β plaques in APPPS1-21 mice heterozygous for TREM2. Molecular Neurodegeneration. 2014;9:20–20. doi: 10.1186/1750-1326-9-20. doi:10.1186/1750-1326-9-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Jay TR, et al. TREM2 deficiency eliminates TREM2+ inflammatory macrophages and ameliorates pathology in Alzheimer's disease mouse models. The Journal of Experimental Medicine. 2015;212:287–295. doi: 10.1084/jem.20142322. doi:10.1084/jem.20142322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wang Y, et al. TREM2 Lipid Sensing Sustains the Microglial Response in an Alzheimer's Disease Model. Cell. 2015;160:1061–1071. doi: 10.1016/j.cell.2015.01.049. doi: http://dx.doi.org/10.1016/j.cell.2015.01.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Stephan AH, Barres BA, Stevens B. Annu. Rev. Neurosci. 2012;35:369–389. doi: 10.1146/annurev-neuro-061010-113810. [DOI] [PubMed] [Google Scholar]
- 69.Fonseca MI, Zhou J, Botto M, Tenner AJ. Absence of C1q Leads to Less Neuropathology in Transgenic Mouse Models of Alzheimer's Disease. The Journal of Neuroscience. 2004;24:6457–6465. doi: 10.1523/JNEUROSCI.0901-04.2004. doi:10.1523/jneurosci.0901-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rogers J, S. J., Brachova L, Lue LF, Webster S, Bradt B, Cooper NR, Moss DE. Complement activation and beta-amyloid-mediated neurotoxicity in Alzheimer's disease. Res Immunol. 1992;143:7. doi: 10.1016/0923-2494(92)80046-n. [DOI] [PubMed] [Google Scholar]
- 71.Shen Y, et al. Complement activation by neurofibrillary tangles in Alzheimer's disease. Neuroscience Letters. 2001;305:165–168. doi: 10.1016/s0304-3940(01)01842-0. doi: http://dx.doi.org/10.1016/S0304-3940(01)01842-0. [DOI] [PubMed] [Google Scholar]
- 72.Orr AG, et al. Astrocytic adenosine receptor A2A and Gs-coupled signaling regulate memory. Nat Neurosci. 2015;18:423–434. doi: 10.1038/nn.3930. doi:10.1038/nn.3930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Jo S, et al. GABA from reactive astrocytes impairs memory in mouse models of Alzheimer's disease. Nat Med. 2014;20:886–896. doi: 10.1038/nm.3639. doi:10.1038/nm.3639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lian H, et al. NFkappaB-activated astroglial release of complement C3 compromises neuronal morphology and function associated with Alzheimer's disease. Neuron. 2015;85:101–115. doi: 10.1016/j.neuron.2014.11.018. doi:10.1016/j.neuron.2014.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Castellano JM, et al. Human apoE isoforms differentially regulate brain amyloid-beta peptide clearance. Science translational medicine. 2011;3:89ra57. doi: 10.1126/scitranslmed.3002156. doi:10.1126/scitranslmed.3002156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Dumanis SB, DiBattista AM, Miessau M, Moussa CE, Rebeck GW. APOE genotype affects the pre-synaptic compartment of glutamatergic nerve terminals. J Neurochem. 2013;124:4–14. doi: 10.1111/j.1471-4159.2012.07908.x. doi:10.1111/j.1471-4159.2012.07908.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Stephan AH, et al. A dramatic increase of C1q protein in the CNS during normal aging. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2013;33:13460–13474. doi: 10.1523/JNEUROSCI.1333-13.2013. doi:10.1523/JNEUROSCI.1333-13.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]