Abstract
The Centers for Medicare and Medicaid Services' Open Payments program implements Section 6002 of the Affordable Care Act requiring medical product manufacturers to report payments made to physicians or teaching hospitals, as well as ownership or investment interests held by physicians in the manufacturer. To determine the characteristics and distribution of these industry payments by specialty, we analyzed physician payments made between August 1, 2013 and December 31, 2013 that were publicly disclosed by Open Payments. We compared payments between specialty type (grouped as medical, surgical, and other specialties) and across specialties within each type, using Pearson's chi square test and the Kruskal-Wallis test. The number of physicians receiving payments was compared to the total number of active physicians in each specialty in 2012. We also analyzed physician ownership interests. There were 2.7 million identified payments to recipient physicians totaling $527 million. Allopathic and osteopathic physicians received 2.43 million payments totaling $475 million. General payments represented 90% ($430 million) of payments by total value (per-physician median:$100, IQR:$31-$273, mean:$1,407, SD:$23,766) with the remaining 10% ($45 million) as research payments (median:$2,365, IQR:$592-$8,550; mean:$12,880, SD:$66,743). Physicians most likely to receive general payments were cardiovascular specialists (78%) and neurosurgeons (77%); those least likely were pathologists (9%). Reports of ownership interest in reporting entities included $310 million in dollar amount invested and $447 million in value of interest held by 2,093 physicians. In conclusion, the distribution and characteristics of industry payments to physicians varied widely by specialty during the first half-year of Open Payments reporting.
The recently debuted Centers for Medicare and Medicaid Services' (CMS) Open Payments transparency program establishes a national database of industry payments to physicians and teaching hospitals1. Financial relationships between medical product manufacturers and physicians have long been a source of concern to patients and policymakers alike. These concerns have grown in recent years as research continues to show the ways in which these widely prevalent relationships2 may affect treatment decisions and may drive healthcare costs due to inappropriate utilization3,4. In their report calling for broad transparency of industry-physician relationships, the Institute of Medicine “defines a conflict of interest as existing when an individual or institution has a secondary interest (…) that creates a risk of undue influence on decisions or actions affecting a primary interest (e.g., the conduct of objective and trustworthy medical research). This definition frames a conflict of interest in terms of the risk of such undue influence and not the actual occurrence of bias3.” In many cases, industry-physician financial relationships, from transfers of value as small as a meal or gift to those for royalties and licensing fees, create a conflict of interest3,4,5.
As a result of concerns about these financial conflicts of interest, several legislative efforts have been made over the years to increase transparency with respect to industry-physician relationships. Prior to Open Payments implementation, several states enacted laws requiring various levels of disclosure of industry payments to physicians6, including full transparency, disclosure to the state, compliance with professional guidelines7, and limits on gifts. However, only 8 states had such laws prior to Open Payments implementation6. In addition to these laws, several pharmaceutical and device manufacturers publicly disclosed payments, though with varying detail8. Kesselheim et al., in their evaluation of Massachusetts physician payment transparency data, found wide variation among specialties9. They speculated that there may be differences in industry incentive to engage in such relationships or that specialties may have differences in the acceptance of these relationships.
Federal policymakers have attempted to increase transparency of industry-physician financial relationships, though attempts between 2002 and 2009 failed to gain enough support for the bills to pass10-12. Finally, in 2010, the Physician Payment Sunshine Act was signed into law as Section 6002 of President Obama's Patient Protection and Affordable Care Act13, leading to the establishment of the Open Payments program. The stated goal of the Sunshine Act and Open Payments is to “shed light on the nature and extent of [industry-physician] relationships and […] hopefully discourage the development of inappropriate relationships and help prevent the increased and potentially unnecessary health care costs that can arise from such conflicts13.” The Open Payments data release was updated in December 2014 and includes 4.5 million records of $3.7 billion in total value for payments occurring between August 1, 2013 and December 31, 2013. These data, despite representing only five months of 2013, are the most comprehensive to date describing physician-industry relationships in the United States. Physician payments reported to Open Payments include payments of greater than $10 or $100 in aggregate annually (adjusted based on the consumer price index) with notable exceptions that include product samples, discounts, charity care, and patient educational materials1.
Much of the existing literature on the Open Payments program is speculative, published prior to the availability of the data, but provide important insight into the possible uses and impact of the data. For example, Rosenthal and Mello14 speculated on the use of Open Payments data by attorneys, insurance carriers, researchers, policymakers, and patients14. The debate on the influence of conflicts of interest on physician decision-making is ongoing14-16, with researchers acknowledging that there is little evidence to answer such questions. Analysis of these newly available data may bring better understanding of the differences and commonalities between specialties in their relationships with industry. Such knowledge may help to determine how to assess the appropriateness of these relationships and their effects on clinical practice, as well as help inform evidence-based advocacy efforts as ongoing federal transparency efforts shift the landscape of disclosure for physicians.
The purpose of our study was to characterize Open Payments program records of industry payments to physicians and determine how these payments vary by specialty. We hypothesized that there would be differences in the characteristics and distribution of payments by physician specialty.
Methods
The Open Payments database allows for physician-level industry payment calculations and aggregation for analysis of broader characteristics by specialty. We performed a retrospective analysis of the most recent (December 2014) publicly available release of Open Payments data on industry payments (>$10 or $100 in aggregate annually) to identified physicians made between August 1, 2013 and December 31, 2013. CMS excludes resident and manufacturer employee physicians. The data released also include payments to teaching hospitals, but these are beyond the scope of this article. Payments to recipient physicians were available in both identified and de-identified databases. Identified physician payments included records of payments or other transfer of value (‘physician payments’) to a specific physician and included physician specialty designation. ‘Recipient physicians’ include both allopathic and osteopathic specialties as well as other practitioners designated as physicians by CMS. We further limited our analysis to allopathic and osteopathic physician specialties that could be matched with the AMA masterfile count of active physicians17. Data were aggregated by physician specialty type (medical, surgical, and other) and by specialty:
medical specialties: allergy & immunology, dermatology, family medicine & general practice, cardiovascular disease, gastroenterology, internal medicine, pediatrics, and pediatric cardiology;
surgical specialties: colorectal surgery, neurosurgery, obstetrics & gynecology, ophthalmology, oral and maxillofacial surgery, orthopedic surgery, otolaryngology, plastic surgery, surgery (general), thoracic surgery, and urology; and,
other specialties: anesthesiology, emergency medicine, neurology, pathology, psychiatry, radiology, and other.
A listing of the specialty groupings is provided to delineate specialty taxonomy used for this analysis (see eTable 1). Records include information on reporting manufacturers, physicians, payments, associated drug or device, and ownership interests.
We characterized payments by ‘type’ (general or research). General payments include all forms of payment other than for research activities, which are classified under research payments (defined below). General payments were also characterized by ‘form’ of payment or the modality used to transfer payment, including: cash or cash equivalent (‘cash’); in-kind items and services (‘in-kind’); dividend, profit or other return on investment (‘ROI’); or stock, stock option or other ownership interest (‘ownership interest’). General payments are further classified by ‘nature’ of payment or the reason the general payment was made. CMS provides descriptive titles for each nature of payment classification and has examples of payment types that were developed with stakeholder input available on their website (available at: https://www.cms.gov/OpenPayments/About/Natures-of-Payment.html, accessed June 15, 2015). We have provided an adapted version of the CMS descriptions in eTable 2.
Research payments include any direct compensation, funding for coordination or implementation, or study participant expense payment associated with research activities1. Research is defined in the regulations as “a systematic investigation designed to develop or contribute to generalizable knowledge relating broadly to public health, including behavioral and social-sciences research. This term encompasses basic and applied research and product development1.” Research-related payments are reported separately from general payments due to the complexity of research programs1. In addition, certain research payments qualify for delayed publication if they are related to new, additional applications of, or clinical investigations regarding a drug, biologic, device or medical supply1. Research payments are not required to report an expenditure category (similar to nature of payment for general payments) because there are often multiple, although the option to report such a category is available. 91% of research payment records did not specify an expenditure category; therefore we did not further explore this classification. We present summarized aggregate data, data by specialty type, and data by physician specialty (organized by specialty type). Payment characteristics analyzed included number of payment reports, value of payments, and the per-physician median and mean payment amount.
Lastly, we characterized physician and immediate family member ownership interests in manufacturers. ‘Ownership interests’ include any ownership or investment interests of physicians or immediate family members in a reporting entity (applicable manufacturer or group purchasing organization) required to report payments1. Ownership interest include stocks, stock options, partnership shares, limited liability company membership(s), loans, bond or other financial instruments secured by the reporting entity; notable exclusions include ownership interest received as compensation (until exercised), as part of a retirement plan, or interest in a publicly traded security or mutual fund1. Unless listed under general payments, ownership interests must be held within the defined reporting period but are not necessarily transferred. To characterize ownership and investment interest data, we utilized CMS terms “amount invested” and “value of interest” to delineate the original amount of the interest holding or transfer of value and the “cumulative value” of that ownership interest in the reporting entity at the end of the reporting period, respectively18. Ownership interest characteristics analyzed included number of ownership interests held, and the total and per-physician median dollar amount invested and value of interest.
We analyzed how payment and ownership interest characteristics vary between specialty types and across physician specialties within each type using Pearson Chi-square test and the Kruskal-Wallis test where applicable. We compared the number of physicians receiving payments to the total number of active physicians in each specialty in 201217 to estimate the proportion of physicians receiving payment and holding ownership interest.
Results
From August 1, 2013 to December 31, 2013, there were 4.4 million payments totaling $2.6 billion reported to Open Payments with 2.7 million of these payments ($869 million) disclosed in an identified manner. General payments represented 4.2 million ($1.0 billion) of all payments, and 2.7 million ($693 million) of the identified payments. Recipient physicians received 4.2 million ($761 million) of all general payments, and identified recipient physicians received 2.6 million payments totaling $476 million. The nature of all general payments to recipient physicians and the subset of identified payments are presented in Table 1. Nature of identified general payments to recipient physicians by total value was primarily compensation for services [$113 million (24%)], royalty/license [$107 million (22%)], and consulting fees [$94 million (20%)]; by number of records, they were primarily food/beverage [2.2 million (84%)].
Table 1. Nature of general paymentsb to recipient physicians, August 1, 2013 to December 31, 2013.
| All general payments | Identified general payments | |||
|---|---|---|---|---|
|
| ||||
| Nature of payment or transfer of value | General payments, No. (% of total) | Total value, USD (% of total) | General payments, No. (% of total) | Total value, USD (% of total) |
| Charitable contribution | 317 (<1%) | $270,769 (<1%) | 232 (<1%) | $149,089 (<1%) |
| Compensation for services other than consulting, including serving as faculty/speaker at a non-CME program | 118,274 (3%) | $189,211,910 (25%) | 75,514 (3%) | $112,549,967 (24%) |
| Compensation for serving as faculty/speaker for a non-accredited and non-certified CME program | 7,152 (<1%) | $15,021,864 (2%) | 4,411 (<1%) | $9,773,642 (2%) |
| Compensation for serving as faculty/speaker for an accredited or certified CME program | 927 (<1%) | $4,375,863 (<1%) | 399 (<1%) | $1,233,613 (<1%) |
| Consulting fee | 67,297 (2%) | $147,813,521 (19%) | 45,989 (2%) | $94,005,913 (20%) |
| Current or prospective ownership or investment interest | 2,047 (<1%) | $14,975,459 (2%) | 1,587 (<1%) | $8,524,147 (2%) |
| Education | 187,436 (4%) | $20,559,345 (3%) | 128,044 (5%) | $12,772,469 (3%) |
All identified payments includes payments to an identified recipient physician, regardless of the type of payment (research or general). All identified general payments include the subset of payments made for any reason other than for research.
Allopathic and osteopathic physicians received 2.4 million payments totaling $475 million (Table 2). Figure 1 shows the distribution of payments among allopathic and osteopathic specialties. Internal medicine and orthopedic surgery had the greatest total value ($111 million each), Figure 1a; however, payments were distributed to a greater number of internal medicine physicians vs. orthopedic surgeons (77,515 vs. 15,459, respectively). Medical specialties that received the greatest number of payments were cardiovascular disease and gastroenterology (78% and 68%, respectively). The proportion of physicians receiving payment was significantly different between specialty types and by specialty within each type (P < .001 for all tests). Form of payments (Figure 1) was primarily cash [$367 million (77%) by value, 469,557 (19%) by number] or in-kind [$103 million (22%) by value, 2.0 million (81%) by number], with the remaining payments as ROI [$421,769 (0.1%) by value, 48 (<0.1%) by number) and ownership interest [$4.8 million (1%) by value, 66 (<0.1%) by number].
Table 2. Industry payments to allopathic and osteopathic physicians by specialty type and by specialty, August 1, 2013 to December 31, 2013.
| All identified paymentsb | Identified general paymentsb | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Specialty | Total payment records, No. | Total value, USD | Active physiciansc, No. | Physicians receiving paymentd, No. (%) | Total general payment records, No. | Total value of general paymentse, USD | Per-physician median value of general payments, USD (IQR) | Per-physician mean value of general payments, USD (SD) | Largest general payment, USD |
| All allopathic and osteopathic specialtiesf | 2,428,437 | $474,676,057 | 813,123 | 324,523 (40%) | 2,415,449 | $429,889,790 | $100 ($31-$273) | $1,407 ($23,766) | $7,356,000 |
| Specialty typef | |||||||||
| Medical specialties | 1,646,144 | $206,179,711 | 417,130 | 187,354 (45%) | 1,636,765 | $176,013,917 | $100 ($31-$268) | $976 ($9,797) | $2,150,000 |
| Surgical specialties | 428,475 | $197,131,503 | 167,314 | 81,444 (49%) | 426,497 | $188,814,432 | $99 ($32-$286) | $2,383 ($43,742) | $7,356,000 |
| Other specialties | 353,818 | $71,364,843 | 228,679 | 55,725 (24%) | 352,187 | $65,061,441 | $83 ($25-$216) | $1,195 ($7,953) | $687,600 |
| Medical specialties | |||||||||
| Allergy & immunology | 17,394 | $3,947,834 | 4,413 | 2,426 (55%) | 17,170 | $2,885,335 | $107 ($39-$259) | $1,194 ($5,074) | $88,000 |
| Cardiovascular disease | 208,107 | $35,606,531 | 23,085 | 18,114 (78%) | 205,392 | $33,755,702 | $175 ($61-$519) | $1,866 ($8,489) | $445,000 |
| Dermatology | 54,295 | $8,130,678 | 11,772 | 7,441 (63%) | 54,143 | $7,294,757 | $106 ($32-$283) | $980 ($4,624) | $93,930 |
| Family medicine & general practice | 468,331 | $21,408,772 | 98,365 | 53,781 (55%) | 467,216 | $18,064,870 | $80 ($25-$206) | $336 ($6,099) | $734,600 |
| Gastroenterology | 93,205 | $15,623,526 | 13,826 | 9,406 (68%) | 92,737 | $14,732,864 | $149 ($56-$373) | $1,569 ($19,167) | $1,716,000 |
| Internal medicine | 748,420 | $111,148,259 | 182,540 | 77,515 (42%) | 744,183 | $92,322,945 | $103 ($32-$280) | $1,152 ($11,148) | $2,150,000 |
| Pediatrics | 55,283 | $9,843,206 | 80,822 | 18,324 (23%) | 54,838 | $6,585,667 | $38 ($17-$91) | $358 ($3,553) | $232,300 |
| Pediatric cardiology | 1,109 | $470,905 | 2,307 | 347 (15%) | 1,086 | $371,777 | $76 ($23-$196) | $1,087 ($4,402) | $51,320 |
| Surgical specialties | |||||||||
| Colorectal surgery | 5,330 | $1,529,758 | 1,568 | 857 (55%) | 5,324 | $1,501,093 | $141 ($47-$618) | $1,754 ($5,886) | $86,000 |
| Neurosurgery | 26,382 | $17,871,297 | 6,041 | 4,632 (77%) | 26,327 | $17,406,424 | $88 ($30-$391) | $3,763 ($30,761) | $1,253,000 |
| Obstetrics & gynecology | 82,349 | $10,241,341 | 43,527 | 18,621 (43%) | 82,042 | $9,070,036 | $62 ($24-$138) | $488 ($4,383) | $337,300 |
| Ophthalmology | 56,874 | $14,218,156 | 18,805 | 9,894 (53%) | 56,121 | $10,970,900 | $113 ($36-$250) | $1,111 ($8,111) | $397,800 |
| Oral/maxillofacial surgery | 655 | $268,380 | 455 | 277 (61%) | 654 | $264,455 | $64 ($23-$146) | $955 ($6,252) | $80,020 |
| Orthopedic surgery | 80,951 | $110,704,56 | 25,670 | 15,459 (60%) | 80,784 | $109,885,624 | $120 ($35-$612) | $7,114 ($94,658) | $7,356,000 |
| Otolaryngology | 15,732 | $2,990,801 | 10,466 | 4,625 (44%) | 15,708 | $2,611,438 | $71 ($26-$160) | $565 ($2,770) | $60,680 |
| Plastic surgery | 12,207 | $4,330,005 | 7,726 | 2,865 (37%) | 11,877 | $3,880,534 | $114 ($34-$326) | $1,363 ($8,848) | $341,400 |
| Surgery (general) | 70,603 | $21,811,190 | 37,739 | 15,387 (41%) | 70,396 | $20,342,511 | $99 ($30-$306) | $1,324 ($20,713) | $2,305,000 |
| Thoracic surgery | 15,259 | $4,562,545 | 4,544 | 2,499 (55%) | 15,204 | $4,417,545 | $181 ($60-$840) | $1,771 ($7,664) | $159,400 |
| Urology | 62,133 | $8,603,467 | 10,773 | 6,328 (59%) | 62,060 | $8,463,872 | $169 ($59-$503) | $1,339 ($6,449) | $250,900 |
| Other specialties | |||||||||
| Anesthesiology | 37,252 | $6,297,362 | 44,555 | 9,855 (22%) | 37,208 | $6,089,848 | $43 ($16-$123) | $618 ($4,508) | $202,100 |
| Emergency medicine | 13,780 | $2,904,024 | 35,937 | 6,271 (17%) | 13,732 | $2,679,681 | $28 ($14-$100) | $428 ($4,324) | $191,800 |
| Neurology | 101,371 | $20,609,422 | 16,810 | 8,282 (49%) | 100,995 | $19,335,051 | $147 ($51-$508) | $2,342 ($9,800) | $278,700 |
| Pathology | 3,731 | $2,219,969 | 18,922 | 1,614 (9%) | 3,701 | $2,030,903 | $60 ($20-$125) | $1,264 ($8,220) | $193,200 |
| Psychiatry | 136,358 | $22,018,887 | 47,833 | 16,399 (34%) | 135,421 | $21,077,442 | $110 ($57-$260) | $1,288 ($7,478) | $212,000 |
| Radiology | 22,428 | $9,947,863 | 40,922 | 7,034 (17%) | 22,273 | $7,022,774 | $66 ($22-$180) | $1,003 ($10,933) | $687,600 |
| Other | 38,898 | $7,367,316 | 23,700 | 6,270 (26%) | 38,857 | $6,825,742 | $75 ($24-$197) | $1,091 ($8,316) | $286,300 |
abbreviations: IQR=Interquartile range, No.= Number, SD=Standard Deviation, USD=2013 United States Dollars
All identified payments includes payments to an identified recipient physician, regardless of the type of payment (research or general). All identified general payments include the subset of payments made for any reason other than for research.
Calculated using the number of active physicians for each specialty in 2012 obtained from AMA masterfile data (American Medical Association,17 2013).
The proportion of physicians paid differed significantly between specialty types and across specialties within each type (Pearson's chi-squared test, P < .001 for all comparisons)
The value of general payments differed significantly between specialty types and across specialties within each type (Kruskal-Wallis test, P < .001 for all comparisons)
Due to rounding, some of the totals may not correspond to the sum of the subtotals.
Figure 1.
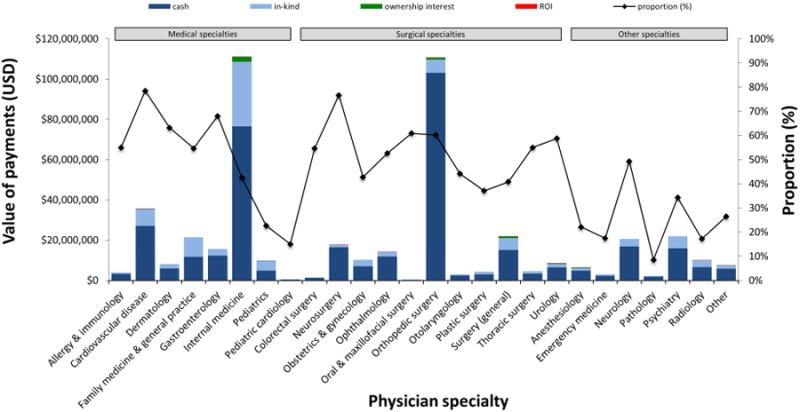
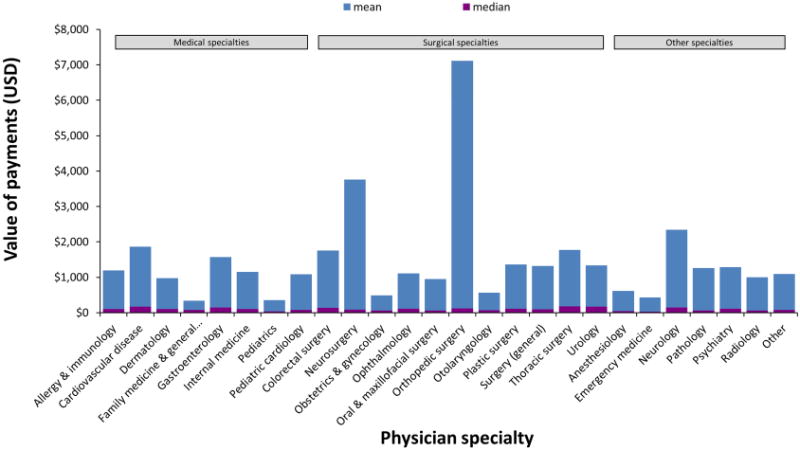
Industry payments to allopathic and osteopathic physicians by specialty, August 1, 2013 to December 31, 2013
a. Total value of payments by form of payment* and proportion of physicians receiving payments†
b. Mean and median per-physician value# of general industry payments
Abbreviations: USD=2013 United States Dollars; ROI=Return on investment
Data include payments to identified physicians in allopathic and osteopathic specialties. Form of payment is the modality used to transfer payment, including: cash or cash equivalent (‘cash’); in-kind items and services (‘in-kind’); dividend, profit or other return on investment (‘ROI’); or stock, stock option or other ownership interest (‘ownership interest’)
*The proportion of payments in each form of payment category was significantly different across specialties within each type (Pearson's chi-square test, all P < .001).
†The proportion of physicians receiving payment was significantly different across specialties within each type (Pearson's chi-squared test, all P < .001).
#The per-physician value of general payments was significantly different across specialties within each type (Kruskal-Wallis test, all P < .001).
General payments represented $430 million (90%) of the total value of payments to allopathic and osteopathic physicians (per-physician median:$100, IQR:$31-$273, mean:$1,407, SD: $23,766) and 2.4 million (99%) of the number of records. The remaining $45 million (10%) of the total value were research payments (median:$2,365, IQR:$592-$8,550; mean:$12,880,SD:$66,743). Thoracic surgery, cardiovascular disease, and urology had the highest median general payments; and, orthopedic surgery, neurosurgery and neurology had the highest mean value of general payments per-physician (Figure 1b). The value of general payments was significantly different between specialty types and by specialty within each type (P < .001 for all tests). The distribution of the nature of payments by specialty type can be found in Figure 2a, Figure 2b, and eTable 3. Surgical specialties had the greatest proportion of general payments for royalty/license [$89 million (47%) in value, 2,431 (<1%) by number]. Royalty/license payments to surgical specialties encompassed 89% of the $100 million total royalty/license payments made for all specialty types. The proportion of general payments in each nature of payment category differed significantly between specialty types and by specialty within each type (P < .001 for all tests).
Figure 2.
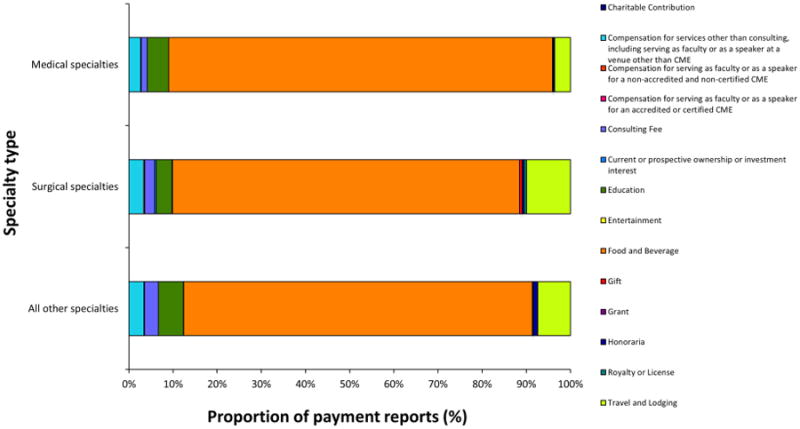
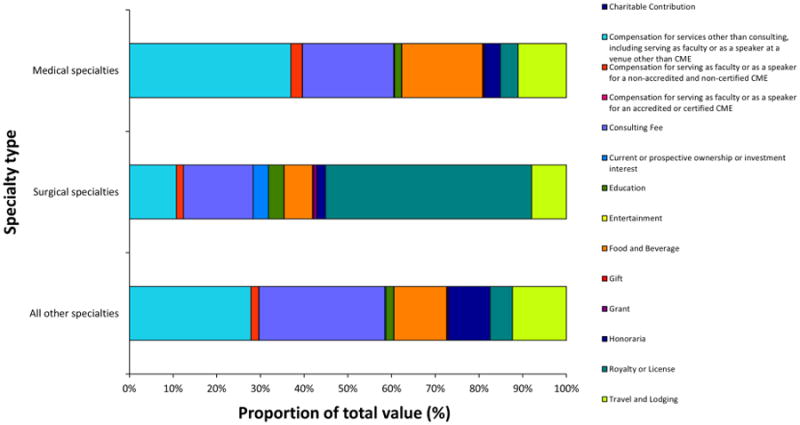
Nature* of identified general payment(s) to allopathic and osteopathic physicians by specialty type as the proportion of payment reports† (a) and of total value (b), August 1, 2013 to December 31, 2013
*Nature of payment is the reason general payment was made
†The proportion of general payments in each nature of payment category was significantly different when compared between specialty types (Pearson's chi-squared test, all P < .001).
Manufacturers also disclosed 3,296 reports of 2,093 individual physicians (0.3% of all physicians) with ownership interest (Table 3) totaling $310 million in total dollar amount invested (median:$12,520, IQR:$3,114-$50,050) and $447 million in total value of interest (median:$15,640, IQR:$4,747-$72,880). We found significant differences in the total dollar amount invested between specialty types and by specialty within each type (Kruskal-Wallis test, P < .001 between specialty types, and by specialty within medical and surgical specialties; P =.001 by specialty within other specialties). We also found that total value of interest between specialty types and by specialty within each type were significantly different for each comparison (P < .001 between specialty types, and by specialty within medical and surgical specialties), except for by specialty within other specialties (P = .11). Specialties most likely to have ownership interests were urology [583 of 10,773 (5%)], neurosurgery [117 of 6,041 (2%)], and orthopedic surgery [385 of 25,670 (2%)]. All other specialties had <1% of physicians with ownership interest. We found significant differences in the proportion of physicians with ownership interest by specialty type and by specialty within each specialty type (P < .001 for all tests).
Table 3. Allopathic and osteopathic physicians' ownership interest in entities reporting to Open Payments by specialty type and specialty, January 1, 2013 to December 31, 2013.
| Physician specialty | Total records, No. | Total dollar amount investedb, USD | Per-physician median dollar amount invested, USD (IQR) | Total value of interestc, USD | Per-physician median value of interest, USD (IQR) | Active physicians, No. | Physicians with ownership interestd, No. (% of total) |
|---|---|---|---|---|---|---|---|
| All allopathic and osteopathic specialties | 3,296 | $309,732,657 | $12,520 ($3,114-$50,050) | $446,722,819 | $15,640 ($4,747-$72,880) | 813,123 | 2,093 (0.26%) |
| Specialty types | |||||||
| Medical specialties | 668 | $109,759,857 | $11,250 ($100-$45,380) | $122,893,860 | $9,961 ($1,000-$50,000) | 417,130 | 613 (0.15%) |
| Surgical specialties | 2,412 | $150,829,819 | $10,690 ($4,297-$50,000) | $252,470,807 | $13,990 ($6,903-$68,440) | 167,314 | 1,303 (0.78%) |
| Other specialties | 216 | $49,142,981 | $50,000 ($10,190-$110,300) | $71,358,152 | $55,310 ($15,500-$150,000) | 228,679 | 177 (0.08%) |
| Medical specialties | |||||||
| Allergy & immunology | 6 | $273,545 | $20,250 ($2,418-$78,980) | $236,597 | $899 ($191-$72,840) | 4,413 | 6 (0.14%) |
| Cardiovascular disease | 103 | $45,401,145 | $72,500 ($20,430-$219,300) | $47,115,102 | $57,490 ($9,029-$200,000) | 23,085 | 82 (0.36%) |
| Dermatology | 11 | $1,135,718 | $30,000 ($25,000-$150,000) | $827,181 | $58,000 ($7,456-$150,000) | 11,772 | 9 (0.08%) |
| Family medicine & general practice | 101 | $2,049,440 | $13 ($10-$285) | $2,808,674 | $252 ($114-$892) | 98,365 | 97 (0.10%) |
| Gastroenterology | 21 | $44,407,718 | $34,430 ($2,682-$64,930) | $41,910,224 | $27,850 ($11,700-$57,410) | 13,826 | 20 (0.14%) |
| Internal medicine | 370 | $15,942,875 | $13,140 ($1,000-$30,000) | $29,198,748 | $16,610 ($1,000-$42,770) | 182,540 | 351 (0.19%) |
| Pediatrics | 56 | $549,416 | $50 ($20-$100) | $797,334 | $1,359 ($406-$2,024) | 80,822 | 48 (0.06%) |
| Pediatric cardiology | 0 | NA | NA | NA | NA | 2,307 | 0 (0.00%) |
| Surgical specialties | |||||||
| Colorectal surgery | 9 | $77,600 | $5,950 ($0-$12,520) | $138,822 | $9,675 ($3,993-$28,460) | 1,568 | 8 (0.51%) |
| Neurosurgery | 139 | $18,113,613 | $50,000 ($20,000-$136,900) | $28,948,119 | $80,380 ($25,760-$209,200) | 6,041 | 117 (1.94%) |
| Obstetrics & gynecology | 49 | $45,177,593 | $10 ($8-$27,090) | $43,410,134 | $398 ($147-$53,520) | 43,527 | 44 (0.10%) |
| Ophthalmology | 72 | $8,408,084 | $49,980 ($24,250-$139,200) | $31,160,165 | $96,900 ($49,950-$248,700) | 18,805 | 66 (0.35%) |
| Oral/maxillofacial surgery | 0 | NA | NA | NA | NA | 455 | 0 (0.00%) |
| Orthopedic surgery | 511 | $60,377,284 | $50,000 ($11,500-$109,600) | $88,029,175 | $50,000 ($13,500-$143,200) | 25,670 | 385 (1.50%) |
| Otolaryngology | 25 | $3,416,882 | $9,533 ($9,533-$69,960) | $8,534,038 | $9,686 ($9,686-$112,500) | 10,466 | 24 (0.23%) |
| Plastic surgery | 8 | $1,528,715 | $30,000 ($26,550-$110,700) | $1,646,186 | $99,600 ($26,380-$134,800) | 7,726 | 7 (0.09%) |
| Surgery (general) | 64 | $4,395,325 | $28,880 ($2,067-$78,720) | $29,773,281 | $42,820 ($7,025-$142,700) | 37,739 | 55 (0.15%) |
| Thoracic surgery | 21 | $1,099,408 | $12,800 ($126-$176,900) | $4,518,110 | $75,680 ($11,560-$265,500) | 4,544 | 14 (0.31%) |
| Urology | 1,514 | $8,235,315 | $6,937 ($3,955-$10,690) | $16,312,777 | $7,542 ($5,275-$12,500) | 10,773 | 583 (5.41%) |
| Other specialties | |||||||
| Anesthesiology | 39 | $4,786,711 | $67,330 ($17,250-$165,800) | $14,454,518 | $79,870 ($25,480-$257,000) | 44,555 | 34 (0.08%) |
| Emergency medicine | 17 | $3,197,682 | $49,980 ($24,250-$146,500) | $3,292,858 | $79,370 ($17,220-$150,000) | 35,937 | 14 (0.04%) |
| Neurology | 12 | $424,982 | $27,500 ($7,083-$50,000) | $1,185,354 | $43,750 ($15,770-$142,300) | 16,810 | 11 (0.07%) |
| Pathology | 7 | $339,064 | $9,197 ($0-$79,600) | $2,339,510 | $103,000 ($38,800-$336,800) | 18,922 | 6 (0.03%) |
| Psychiatry | 9 | $869,191 | $73,580 ($64,190-$125,000) | $1,221,293 | $71,910 ($40,490-$107,600) | 47,833 | 8 (0.02%) |
| Radiology | 116 | $37,705,465 | $33,850 ($6,274-$81,820) | $47,311,353 | $50,000 ($11,100-$90,640) | 40,922 | 91 (0.22%) |
| Other | 16 | $1,819,886 | $101,000 ($50,000-$163,900) | $1,553,266 | $112,200 ($51,010-$190,900) | 23,700 | 13 (0.05%) |
Abbreviations: IQR=Interquartile range; NA=Not applicable; No.= Number; USD=2013 United States Dollars
The proportion of physicians with ownership interest differed significantly between specialty types, and across specialties within each type (Pearson's chi-square test, P < .001 for all comparisons).
The total dollar amount invested differed significantly between specialty types, and across specialties within each type (Kruskal-Wallis test, P < .001 for all comparisons except for across specialties within other specialties (P = .001))
The total value of interest differed significantly between specialty types and across specialties within each type using (Kruskal-Wallis test, P < .001 for all comparisons except for across specialties within other specialties (P = .11)).
Discussion
Our analysis of this unprecedented volume of physician-specific data on industry-related financial conflicts of interest shows wide variability in the prevalence and characteristics of industry payments to physicians by specialty. While important analyses of Open Payments manufacturer and product data exist19,20, little attention has been paid to characteristics of physician data. A report by Jarvies et al.20 gave an initial account of the first release of Open Payments data in September 2014, focusing largely on manufacturer and product data. However, the data provided regarding physician specialties were limited to 5 specialties and provided aggregates that included ownership and investment interests in the totals, despite the difference in reporting of these records. Useful aggregation and analyses of Open Payments manufacturer and product data are also available from ProPublica19 and from CMS in their recent report to Congress21, although little attention has been paid to characteristics of physician data. Prior to the enactment of Open Payments, ProPublica also assembled a separate important database of industry-physician financial relatinships22 containing $4 billion in payments disclosed by 17 pharmaceutical companies between 2009 and 2013. In comparison to the 4 year period evaluated by ProPublica, the Open Payments data presented herein reports on a 5 month period that contains data on nearly the same total value of payments ($3.7 billion in total).
Our findings are also important because the specialty variation in our analysis demonstrates that further interpretation of the impact of industry payments on physician decision-making, healthcare costs and utilization must incorporate the specialty-specific context of these data. We found significant differences in the distribution and median values of payments by specialty type as well as by specialty within each type. We found that general medical specialties (internal medicine and family medicine/general practice,) were the target of a large proportion of industry payments (1.2 million (50%) of 2.4 million total) though the value of these payments tended to be lower than other specialties [$133 million (28%) of $475 million paid to allopathic and osteopathic specialties in our analysis]. In addition, the medical specialties that involve a greater amount of intervention (cardiovascular disease, gastroenterology and dermatology) had the highest proportion of physicians receiving industry payments. Our data are consistent with prior evidence showing wide variation among specialties in an early evaluation of Massachusetts physician payment transparency data9 as well as in physician self-reports2,23. These evaluations also found a high prevalence of payments with specialty variability, as well as high values of payments attributed to cardiology and orthopedic surgery. In addition, our data differ from the Massachusetts data in the nature of payments by providing additional detail to the distribution of payments, where a large proportion of Massachusetts payments fell under the broad category of “compensation for bona fide services9.” Other analyses of Open Payments data also found similar variation amongst a limited number of surgical specialties24-26, although a comprehensive analysis of medical and other specialties is absent. Certain specialties may have greater research and development involvement resulting in royalty and licensing payments27. Comparisons between surgical, medical and other specialties in our findings show distinct payment distributions and characteristics in each specialty type, with greater royalty and licensing payments in surgical specialties compared to medical and other specialties. In addition, our findings are consistent with an analysis showing the broad extent of financial interaction between orthopedic surgery and industry26, a field with long-standing financial relationships28 and a history of recent problematic relationships with device manufacturers influencing the dissemination of research results29,27.
Whether transparency will impede valuable collaborations and the pace of innovation also requires ongoing evaluation, as does further investigation into the appropriateness of these financial relationships. For example, the influence of payments of greater value (orthopedic surgery received 80,951 (3%) of payments by number and $111 million (23%) of $475 million by value) cannot necessarily be interpreted under the same criteria as payments to other specialties. However, implications of these payments are complex; and, the prevalence and magnitude of payments seen in these data increase the need for further research into the effect of these payments, both beneficial and problematic. Research has shown that physician payment laws may deter physician-industry relationships that create conflicts of interest6,15. Physicians may be less likely to accept industry payments15, and manufacturers may be less likely to pay physicians and shift these expenditures towards direct-to-consumer advertising and towards payers30. But there is also some debate as to whether an unintended consequence of transparency of physician payments may result in allowing such payments to be more rather than less influential because they have been disclosed31 due to discounting by informed patients or a feeling of moral license after having disclosed such a relationship. Moreover, others16 have found that the effects of transparency are small in deterring utilization of higher priced drugs, for example. Many have expressed concern with the limitations of the Open Payments program, citing the inaccuracies of the database32, the short review period33, and the value assigned to research payments due to the high price of drugs34. Additionally, others are concerned that payment transparency, if not properly contextualized, will deter physicians from entering even those relationships that are beneficial, out of concern that such payments will be misconstrued as problematic32.
Our study adds to the current literature by providing a comprehensive analysis of Open Payments physician-level data with specialty-specific analyses to evaluate differences in the distribution and characteristics of payments. Now that Open Payments data are publicly available, despite criticisms of the data released thus far35, physicians must understand what is being reported, how to engage efficiently and effectively with Open Payments, and how to manage questions from patients and other interested parties. Manufacturers are not required to inform physicians that certain payments must be reported, nor is physician participation in the program required; thus, educating physicians on transparency data is critical to physician awareness. CMS estimates that 50% of physicians will have a reported financial relationship with industry1. We estimate that 40% (324,523) of all allopathic and osteopathic physicians (813,123) received identified payments, nearly meeting CMS estimates, though we expect that the actual proportion is greater. The remaining 1.7 million de-identified records may include up to 546,000 total physicians (68% of physicians by our estimates), but the actual number is unclear due to provider identifier inconsistencies1. CMS also excluded 190,000 records due to delay in publication requests. In addition, manufacturers must now report payments for accredited CME activities made in 2016 and beyond. Moreover, if payers incorporate Open Payments data into certain quality and utilization measures used for reimbursement14, more physicians are likely to review their reports. Acknowledging the potential for an increase in physicians engaging with Open Payments will ensure that the proper support and resources are available.
While CMS suggests that Open Payments data be combined with quality and utilization data to improve understanding of these relationships1, no unique physician identifier is publicly available to facilitate comparison to other quality and utilization, research publication, or funding databases to facilitate effective analysis. Industry reporting of payments must include a National Provider Identifier (NPI), however the law itself prohibits publication of NPIs with Open Payments data. CMS implemented a search tool to help identify payments by physician or manufacturer name, but does not enable broader aggregation and analysis. However, searching for payments to an individual physician still provides organizations the opportunity to verify conflicts of interest and make more informed decisions on physician participation in influential decision making and developing guidelines. There is also ongoing debate into whether or not some payments deserve exclusion36, with recent federal efforts to allow payments related to accredited CME activities to be excluded from reporting requirements based on the recent changes made by CMS discussed above for the 2016 reporting year.
The extent to which patients' knowledge of industry-physician relationships will impact their decision making is unclear3. Research into the opinion of patients regarding industry-physician financial conflicts of interest has shown that patients in clinical trials largely (90%) expressed little to no concern about the financial ties, although many wanted disclosure of these interests (31%)37. In addition, a survey or orthopedic surgery patients found that they largely viewed financial relationships for surgeons acting as consultants for device manufacturers as beneficial38. Nevertheless, proper contextualization of payments is an ongoing concern for physicians and specialty societies, given the potential for misinterpretation by patients or the media, and the potential for use in liability claims. Industry collaborations in research are increasingly important as a result of stagnating government-funded support28,29,39. In a commentary on the potential unintended effects of Open Payments on oncology care, one author suggests that given the assignment of industry publication expenses being attributed to a physician, that important research findings may be delayed and that researchers may be reluctant to engage in industry-supported research40. Our data establish important elements of payment context that may help to mitigate such reluctance, and ongoing assessment of the appropriateness of industry-physician relationships may help ensure that disclosure does not adversely affect beneficial relationships that are becoming more common, and will deter those that are inappropriate. Furthermore, such payments for publication expenses, if reported correctly, would be included in a research payment if subject to an agreement, contract or research protocol, and the separate reporting of research payments should mitigate certain concerns, especially as the program and reporting entity experience with the Open Payment system matures and physicians become more involved.
Our study has limitations. First, our study is limited by restricting our analysis to identified physician payments–payments linked to a physician with total confidence–excluding 1.7 million records. Accordingly, we likely underestimated the proportion of physicians receiving industry payments and as such, the generalizability of our data is limited. Also, we were unable to assess specialty-level systematic differences in the excluded data. However, the distribution of de-identified general payments by nature was similar to identified payments (Table 1), and we do not expect that errors leading to provider identification introduce large systematic bias, though it cannot be ruled out. Ongoing analyses of upcoming data releases will be an important step in verifying our findings and analyzing how they change over time. CMS also excluded 190,000 records due to delay in publication requests, many of which may have been for proprietary drugs or devices. Accordingly, incidence of physician payments may be underestimated and we could not account for potential systematic differences in excluded records or inaccuracies inherent to the database. CMS does not publish NPIs in the public use dataset, therefore incorporation of demographic and other data of interest is limited.
The Open Payments data and our analyses, while important, demonstrate the need to test the effects of financial conflicts of interest on physician behavior and those of transparency itself in prospective interventional studies. In addition, the variability of our data between specialties demonstrate a potential need for specialty-specific advocacy as federal transparency programs and their broad availability evolve.
Conclusion
Our analysis provides important insights into the specialty differences in industry-related conflicts of interest as the nation's physician workforce enters an era of transparency for industry-physician relationships. These data can inform transparency policy-making and advocacy efforts by specialty organizations and guide further research efforts to measure the effect of transparency on physician and patient decision-making and how industry-physician relationships change over time.
Supplementary Material
Acknowledgments
None
Financial support and disclosure: The authors are partially supported by the National Institutes of Health, Grants TL1TR00098 (DM), 5T35HL007491 (MJ), UL1TR000100 (JHG), and KL2TR00099 (JHG). The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
List of abbreviations
- CME
Continuing medical education
- CMS
Centers for Medicare and Medicaid Services
- IQR
Interquartile range
- NPI
National Provider Identifier
- ROI
Return on investment
- SD
Standard deviation
Footnotes
Supplemental Online Material: Supplemental material can be found online at: http://www.mayoclinicproceedings.org. Supplemental material attached to journal articles has not been edited, and the authors take responsibility for the accuracy of all data.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Medicare, Medicaid, Children's Health Insurance Programs: transparency reports and reporting of physician ownership or investment interest. Vol. 78. Centers for Medicare and Medicaid Services; 2013. [PubMed] [Google Scholar]
- 2.Campbell EG, Rao SR, DesRoches CM, et al. Physician professionalism and changes in physician-industry relationships from 2004 to 2009. Arch Intern Med. 2010;170(20):1820–1826. doi: 10.1001/archinternmed.2010.383. [DOI] [PubMed] [Google Scholar]
- 3.Conflict of interest in medical research, education, and practice. Washington, D.C.: Institute of Medicine: National Academies Press; 2009. [PubMed] [Google Scholar]
- 4.Wazana A. Physicians and the pharmaceutical industry: is a gift ever just a gift? JAMA. 2000;283(3):373–380. doi: 10.1001/jama.283.3.373. [DOI] [PubMed] [Google Scholar]
- 5.Dana J, Loewenstein G. A social science perspective on gifts to physicians from industry. JAMA. 2003;290(2):252–255. doi: 10.1001/jama.290.2.252. [DOI] [PubMed] [Google Scholar]
- 6.Chimonas S, Rozario NM, Rothman DJ. Show us the money: lessons in transparency from state pharmaceutical marketing disclosure laws. Health Serv Res. 2010;45(1):98–114. doi: 10.1111/j.1475-6773.2009.01048.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Department of Health and Human Services (DHHS), Office of the Inspector General. OIG compliance program guidelines for pharmaceutical manufacturers. Fed Regist. 2003;68:23731. [Google Scholar]
- 8.Hwong AR, Qaragholi N, Carpenter D, Joffe S, Campbell EG, Soleymani Lehmann L. A systematic review of state and manufacturer physician payment disclosure websites: implications for implementation of the Sunshine Act. J Law Med Ethics. 2014;42(2):208–219. doi: 10.1111/jlme.12136. [DOI] [PubMed] [Google Scholar]
- 9.Kesselheim AS, Robertson CT, Siri K, Batra P, Franklin JM. Distributions of industry payments to Massachusetts physicians. N Engl J Med. 2013;368(22):2049–2052. doi: 10.1056/NEJMp1302723. [DOI] [PubMed] [Google Scholar]
- 10.Drug Company Gift Disclosure Act of 2002, HR 5037, 107th Cong, 2nd Sess (2002).
- 11.Physician Payments Sunshine Act of 2007, S 2029, 110th Cong, 1st Sess (2007).
- 12.Physician Payments Sunshine Act of 2009, S 301, 111th Cong, 1st Sess (2009).
- 13.Patient Protection and Affordable Care Act, Public Law 111-148, USC HR 3590. 2010 [Google Scholar]
- 14.Rosenthal MB, Mello MM. Sunlight as disinfectant--new rules on disclosure of industry payments to physicians. N Engl J Med. 2013;368(22):2052–2054. doi: 10.1056/NEJMp1305090. [DOI] [PubMed] [Google Scholar]
- 15.Sah S, Loewenstein G. Nothing to declare: mandatory and voluntary disclosure leads advisors to avoid conflicts of interest. Psychol Sci. 2014;25(2):575–584. doi: 10.1177/0956797613511824. [DOI] [PubMed] [Google Scholar]
- 16.Pham-Kanter G, Alexander GC, Nair K. Effect of physician payment disclosure laws on prescribing. Arch Intern Med. 2012;172(10):819–821. doi: 10.1001/archinternmed.2012.1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Survey & Data Resources. American Medical Association; 2013. Physician Characteristics and Distribution in the United States. [Google Scholar]
- 18. [Accessed June 15, 2015];Frequently asked questions, FAQ 8376 2015. 2015 https://questions.cms.gov/faq.php?id=5005&faqId=8376.
- 19.Dollars for Docs: Open Payments Explorer. [Accessed February 1, 2015];ProPublica. Available at: http://projects.propublica.org/open-payments/
- 20.Jarvies D, Coombes R, Stahl-Timmins W. Open Payments goes live with pharma to doctor fee data: first analysis. BMJ. 2014;349:g6003. doi: 10.1136/bmj.g6003. [DOI] [PubMed] [Google Scholar]
- 21.Department of Health and Human Services, Centers for Medicare and Medicaid Services. Annual Report to Congress on the Open Payments Program for Fiscal Year 2014. 2015. [Google Scholar]
- 22.Dollars for Docs: How industry dollars reach your doctors. [Accessed June 15, 2015];ProPublica. Available at: https://projects.propublica.org/docdollars/
- 23.Campbell EG, Gruen RL, Mountford J, Miller LG, Cleary PD, Blumenthal D. A national survey of physician-industry relationships. N Engl J Med. 2007;356(17):1742–1750. doi: 10.1056/NEJMsa064508. [DOI] [PubMed] [Google Scholar]
- 24.Chang JS. The Physician Payments Sunshine Act: data evaluation regarding payments to ophthalmologists. Ophthalmology. 2015;122(4):656–661. doi: 10.1016/j.ophtha.2014.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rathi VK, Samuel AM, Mehra S. Industry ties in otolaryngology: initial insights from the physician payment sunshine act. Otolaryngol Head Neck Surg. 2015;152(6):993–999. doi: 10.1177/0194599815573718. [DOI] [PubMed] [Google Scholar]
- 26.Samuel AM, Webb ML, Lukasiewicz AM, et al. Orthopaedic Surgeons Receive the Most Industry Payments to Physicians but Large Disparities are Seen in Sunshine Act Data. Clin Orthop Relat Res. 2015 doi: 10.1007/s11999-015-4413-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chatterji AK, Fabrizio KR, Mitchell W, Schulman KA. Physician-industry cooperation in the medical device industry. Health Aff (Millwood) 2008;27(6):1532–1543. doi: 10.1377/hlthaff.27.6.1532. [DOI] [PubMed] [Google Scholar]
- 28.Zuckerman JD, Prasarn M, Kubiak EN, Koval KJ. Conflict of interest in orthopaedic research. J Bone Joint Surg Am. 2004;86-A(2):423–428. doi: 10.2106/00004623-200402000-00030. [DOI] [PubMed] [Google Scholar]
- 29.Gelberman RH, Samson D, Mirza SK, Callaghan JJ, Pellegrini VD., Jr Orthopaedic surgeons and the medical device industry: the threat to scientific integrity and the public trust. J Bone Joint Surg Am. 2010;92(3):765–777. doi: 10.2106/JBJS.I.01164. [DOI] [PubMed] [Google Scholar]
- 30.Mackey TK, Liang BA. Physician payment disclosure under health care reform: will the sun shine? J Am Board Fam Med. 2013;26(3):327–331. doi: 10.3122/jabfm.2013.03.120264. [DOI] [PubMed] [Google Scholar]
- 31.Loewenstein G, Sah S, Cain DM. The unintended consequences of conflict of interest disclosure. JAMA. 2012;307(7):669–670. doi: 10.1001/jama.2012.154. [DOI] [PubMed] [Google Scholar]
- 32.Moy B, Jagsi R, Gaynor RB, Ratain MJ. The impact of industry on oncology research and practice. Am Soc Clin Oncol Educ Book. 2015;35:130–137. doi: 10.14694/EdBook_AM.2015.35.130. [DOI] [PubMed] [Google Scholar]
- 33.Kirschner NM, Sulmasy LS, Kesselheim AS. Health policy basics: the Physician Payment Sunshine Act and the Open Payments program. Ann Intern Med. 2014;161(7):519–521. doi: 10.7326/M14-1303. [DOI] [PubMed] [Google Scholar]
- 34.Morain SR, Flexner C, Kass NE, Sugarman J. Forecast for the Physician Payment Sunshine Act: partly to mostly cloudy? Ann Intern Med. 2014;161(12):915–916. doi: 10.7326/M14-1683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Santhakumar S, Adashi EY. The Physician Payment Sunshine Act: testing the value of transparency. JAMA. 2015;313(1):23–24. doi: 10.1001/jama.2014.15472. [DOI] [PubMed] [Google Scholar]
- 36.Richardson EC, A, Saver R, Lott R, Gnadinger T. Health Policy Brief: The Physician Payments Sunshine Act. 2014 [Google Scholar]
- 37.Hampson LA, Agrawal M, Joffe S, Gross CP, Verter J, Emanuel EJ. Patients' views on financial conflicts of interest in cancer research trials. N Engl J Med. 2006;355(22):2330–2337. doi: 10.1056/NEJMsa064160. [DOI] [PubMed] [Google Scholar]
- 38.Khan MH, Lee JY, Rihn JA, et al. The surgeon as a consultant for medical device manufacturers: what do our patients think? Spine (Phila Pa 1976) 2007;32(23):2616–2618. doi: 10.1097/BRS.0b013e318158cc3a. discussion 2619. [DOI] [PubMed] [Google Scholar]
- 39.Moses H, 3rd, Matheson DH, Cairns-Smith S, George BP, Palisch C, Dorsey ER. The anatomy of medical research: US and international comparisons. JAMA. 2015;313(2):174–189. doi: 10.1001/jama.2014.15939. [DOI] [PubMed] [Google Scholar]
- 40.Ratain MJ. Forecasting unanticipated consequences of “The Sunshine Act”: mostly cloudy. J Clin Oncol. 2014;32(22):2293–2295. doi: 10.1200/JCO.2014.55.4592. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


