Abstract
Background
This study examined poly-drug use involving the use of cannabis with nonmedical prescription pain reliever use (NMPR) and alcohol use.
Methods
Computer-assisted survey data from the National Survey on Drug Use and Health were examined. The NSDUH is an annual, cross-sectional survey of non-institutionalized citizens in the United States (ages 12+). Replicate analyses were conducted using the 2013 and 2003 survey waves.
Results
Higher levels of cannabis use were consistently associated with more frequent consumption of prescription pain relievers, with findings replicating in both 2013 and 2003. While the prevalence of dual users declined from 2003 (2.5%) to 2013 (2.3%), the average number of days used among dual users increased by an average of 20 days over that period. These changes largely occurred among those aged 35 or older, males, whites, and non-illicit drug users. Past-year marijuana use increased by 16% (10.8–12.6%, p-value < .001) whereas NMPR decreased by 15% (4.9–4.2%, p-value < .001). The largest changes occurred after 2011. Persons using the most cannabis generally had higher levels of alcohol use relative to those using the least amount of cannabis. There was a significant increase in the prevalence of dual use between 2003 (10.2%) and 2013 (11.6%), while the prevalence of past-year alcohol use remained relatively stable.
Conclusions
Clinical efforts and public health interventions should consider the possible co-ingestion of cannabis with NMPR and alcohol, as concomitant use may portend negative health effects in the short and long-term.
Keywords: Epidemiology, Marijuana, Cannabis, Alcohol, Opioids, Prescription drug misuse
1. Introduction
Cannabis is one of the most commonly used drugs in the United States. Despite recent state legislation that permits use for medical and even recreational use in some states, cannabis remains classified as an illegal substance at the federal level (SAMHSA, 2014). Motivations for use include the self-medication of pain, reduced anxiety and tension, intoxication, and even increased sociability (Hayaki et al., 2010). It is not surprising that users report different motivations for consumption, as over 400 different pharmaceutical agents have been isolated in the cannabis plant (Kogan and Mechoulam, 2007). The two primary pharmacological agents in cannabis are cannabidiol (CBD) and Δ9-tetrahydrocannabinol (THC). CBD is responsible for its anxiolytic and anti-inflammatory properties. Because of its efficacy as a pain reliever, some users may prefer cannabis over opioids as a frontline treatment for pain (Lucas, 2012). Laboratory studies provide evidence that users may be drawn to cannabis as a result of its strong intoxicating effect, primarily due to its THC content (Watson and Benson, 2001). This underscores the possibility that cannabis may be used as a substitute for alcohol as well, likely because it produces feelings of tension reduction that are similar to alcohol.
There are several possible relationships that can be used to describe patterns of dual use involving cannabis and other licit and illicit drugs. The term “substitution” effect has been used to describe the behavioral phenomena in which an individual freely chooses to consume one substance as a replacement for another substance. In contrast to substitution, use may also occur in a complementary fashion, such as using a second drug as a way to augment the effects of a primary drug. For example, a case study of pain clinic patients reported that promethazine can augment the feelings of euphoria among those using prescription pain reliever products (Lynch et al., 2015). Substances that are ingested by the same person can have markedly different effects depending upon their pharmacokinetics, absorption and distribution throughout the body (FDA, 2015). Understanding the pattern of dual use has important clinical and public health implications in terms of short-term (e.g., overdose) and long-term (e.g., hepatic functioning) health effects.
A first step to determining the nature of the relationship between one or more substances is to first examine their consumption practices more broadly. Typically, self-report data are used to indicate whether use has occurred in a given period. Prior studies have shown using binary indicators that the likelihood of alcohol use and prescription pain reliever misuse is higher among cannabis users compared to non-cannabis users (Compton et al., 2004). Others have examined use of one substance during periods of abstinence involving another substance. For example, Allsop et al. (2015) found increases in tobacco and alcohol use during periods of abstinence from cannabis (Allsop et al., 2015).
A limitation to the indicator approach is that persons using more frequently are coded the same as those using just once or twice. Examining levels of use overcomes this limitation by establishing whether a user favors one substance relative to another based on quantity measures. A study by Kral et al. (2015) examined the possibility that cannabis may be used as a substitute for opioids by comparing the frequency of use as reported for both substances. The authors found a negative relationship between cannabis use and opioid use, and drew upon those findings to support a substitution hypotheses. One limitation of this approach is that the relationship is established only by the number of days each substance was used. The quantitative measures of consumption do not provide direct evidence for a causal relationship because it is not possible to establish the actual number of days the substances were actually used together. However, this correlational exposure approach does have utility, as the number of days a product was used can help identify preferences for one product relative to another. The number of days a substance was used in a month is also a fairly simple measure to report, so it is widely available on most surveys of drug use. Data on concomitant use are lacking on many surveys, likely because it is a complicated behavioral pattern to measure. The current study draws on the correlational approach, but conducts a series of sensitivity analyses by examining the stability of the findings across different observational periods, as well as examining whether the relationships are similar across related substances.
The goal of the current study was to examine the dual use of cannabis with prescription pain relievers and alcohol. As much of the prior studies used small, community-based samples that were largely cross-sectional, the current study overcomes those previous limitations in using data from the 2003 to 2013 National Survey on Drug Use and Health. The NSUDH is only available for public use through the year 2013, prior to the first statewide retail legalization of cannabis in 2014. To provide an understanding of the stability of the relationships, the analyses were replicated using 2013 and 2003 NSDUH data. There was a major NSDUH redesign in 2003, which precluded comparisons to previous years. Therefore, the data available for analyses were only between the years from 2003 to 2013.
It is important to note that this study is not meant to estimate the impact of policy changes that may have occurred during this 10-year period on substance use behaviors. Yet, it is important to recognize the larger cultural environment during this time. Before 2003, three states legalized cannabis for medicinal purposes only. Between 2003 and 2013, seventeen additional states legalized medical cannabis. In 2014, cannabis was legalized for retail purposes in Colorado and Washington, and later in the District of Colombia, Oregon and Alaska. While access to cannabis certainly increased during this period, numerous policies were also implemented to restrict access to prescription pain relievers, such as prescription drug monitoring programs and medication take-back programs (Gugelmann and Perrone, 2011; Manchikanti, 2006). Inspection of the data over time can provide a sensitivity analyses that controls for the influence of environmental factors on usage. In light of this, the goal of the current work is to evaluate the dual use of cannabis with NMPR and alcohol using nationally representative data collected over multiple years.
2. Methods
The National Survey on Drug Use and Health (NSDUH) is an annual computer-aided, interviewer-assisted survey of non-institutionalized U.S. civilians aged 12 years or older. Additional sample details are available elsewhere (SAMHSA, 2014). The yearly data from 2003 to 2013 were used to test for trends in substance use over time. The 2003 and 2013 data sets were used for the rest of the analyses presented in this study. The unweighted sample sizes were approximately 55,000 per year. Past-year nonmedical pain reliever (NMPR) use was defined as use in the past 12 months without a doctor’s prescription or for the experience or subjective feelings it causes. Past-year cannabis use was defined as use of cannabis or hashish in any form (e.g., smoked or edible) in the past 12 months. Alcohol use was defined as any alcoholic beverage/distilled spirits, including beer, wine, and “hard” liquor (e.g., bourbon, tequila, specialty beverages). Respondents were asked to report the number of days each substance was used in the past 12 months. Those who reported past-year NMPR and cannabis use in the past 12 months were classified as dual users of cannabis-NMPR. This approach was also used to classify dual users of cannabis-alcohol as well.
Among dual users, the frequency of past-year cannabis use was categorized into separate quartiles for each year (i.e., 2003 and 2013) based on the number of days used. Separate cut-points were used for 2003 and 2013 rather than using the same cut-points across years. This method aligned with the goal to examine changes in the relative position of use from 2003 to 2013. This method of standardization allows for the comparison of those using in the same quartile (e.g., 1–25th percentile) over time, accounting for population changes in use over time. Initial sensitivity analyses were conducted by using the same cutpoints for both years. The results did not change appreciably whether the 2003 or 2013 quartiles were used, so the separate cut-points were used, essentially controlling for study year. For 2003, marijuana quartiles were defined as: quartile 1: 1–4 days, quartile 2: 5–43 days, quartile 3: 44–155 days, and quartile 4: 156–365 days. For 2013, the marijuana quartiles were defined as: quartile 1: 1–5 days, quartile 2: 6–51 days, quartile 3: 52–207 days, and Quartile 4: 208–365 days.
A Generalized Estimating Equation (GEE) modeling approach was first used to test for a linear statistical trend between 2003 and 2013 using a single continuously distributed variable representing survey year. Separate models were estimated for cannabis, NMPR, and alcohol. The next set of analyses examined the relationship between cannabis and the use of either NMPR or alcohol. A set of analyses were estimated for 2013, the most recent year of NSDUH data and also the year prior to the legalization of marijuana for retail sales. The proportions were tested using the generalized linear model, with the model-based chi-squared derived from either a 2-level (e.g., use/no use) or 4-level (e.g., no use, NMPR only, cannabis only, both) variable. All statistical tests were computed with SUDAAN (Release 11.1) to account for the complex sampling design and the sampling weights. This method also transforms the results so that they are generalize to the non-instituitonalized population in the U.S. The weights are also calculated such that they control for changes in demographic composition in the U.S. over time.
3. Results
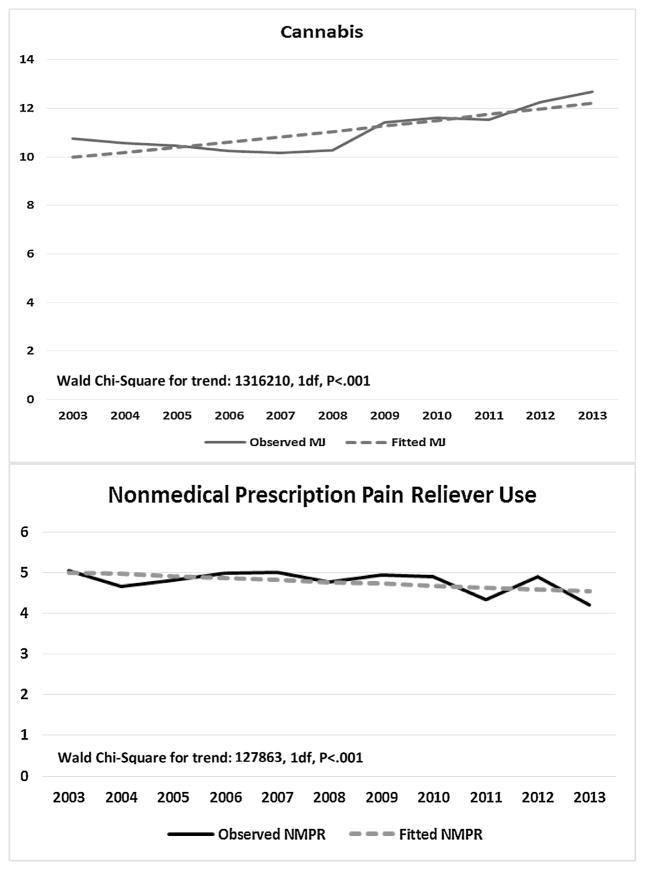
Fig. 1 shows the linear trend between 2003 and 2013, and specifically that the prevalence of cannabis users aged 12 or older in the United States increased from 10.8% to 12.6%. The fitted predicted probability trend line showing the positive change is also presented (Chi-Square 1316210, 1df, P < .001). In contrast, the prevalence of NMPR decreased from 4.9% to 4.2% over that same 10-year period. The linear trend showing a decline (Chi-square = 127863, 1df, P < .001) is also presented. Note that there was no significant change in the prevalence of alcohol use between 2003 and 2013 (65.3% in 2003 and 66.2% in 2013), so we did not include a separate figure. These data are also shown in Fig. 2, Panel 1.
Fig. 1. Trends in the past-year cannabis and nonmedical prescription pain reliever use: 2003–2013, NSDUH.
Note: Analyses conducted within SUDAAN, release 11.0. P-values reflect longitudinal trend between 2003 and 2013. Alcohol use is not presented, as it did not statistically change between 2003 and 2013. (Sample size for 2003 = 55,230 and 2013 = 55,160).
Source: 2003 and 2013 National Survey on Drug Use and Health (NSDUH, 2003–2013).
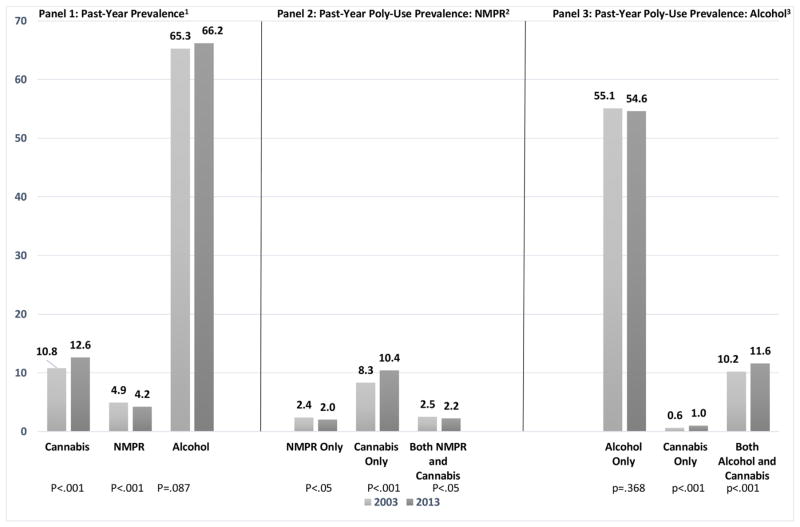
Fig. 2. Past-year prevalence of cannabis, nonmedical pain reliever use and alcohol, and co-occurring use: 2003 and 2013 NSDUH.
(1) Among entire NSDUH sample; (2) represents NMPR/no cannabis, cannabis/no NMPR, both NMPR/cannabis, or no use of either (not shown); (3) represents alcohol only/no cannabis, cannabis only/no alcohol, both alcohol/cannabis, or no use of either (not shown). Estimates are weighted, and therefore adjust for population-level demographic changes.
Source: 2003 and 2013 National Survey on Drug Use and Health (NSDUH, 2003 and 2013).
Fig. 2, Panel 2 categorized past-year users into four categories: NMPR only/No Cannabis, Cannabis only/No NMPR, Both, and none (not shown). It is important to note that only a small percentage of the population reported past-year use of both cannabis and NMPR, and this population declined from 2003 to 2013 (2.5% to 2.2%). Fig. 2, Panel 3 shows the same analysis, except it focuses on the combined use of cannabis with alcohol. The prevalence of dual use of cannabis and alcohol increased between 2003 and 2013 (10.2% to 11.6%).
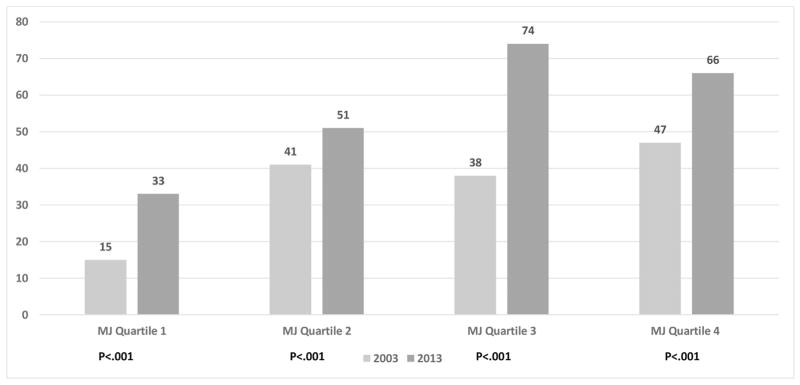
The next analyses, shown in Fig. 3 is subset to those dual users of cannabis and NMPR for 2003 (2.5%, unweighted sample n = 2,565) and 2013 (2.2%, unweighted sample n = 1,915). There was a statistically significant and positive association between the number of days of cannabis use and days of NMPR use in 2003 (Chi-Square: 9.2, 3df, P < .001) and in 2013 (Chi-square: 3.7, 3df, P = .010). To illustrate for 2013, those consuming the most amount of cannabis by percentile (quartile 4: 76th percentile or higher) reported 33 more days of NMPR use (66 days versus 33 days) than those in the lowest percentile (quartile 1: 1 to 25 percentile). This relationship also held for 2003, where respondents in the 4th quartile reported 47 days of NMPR compared to 15 days for the lowest quartile. Within each quartile, there were also increases in the number of NMPR days between 2003 and 2013. To illustrate, there was an 18 day increase (15 days to 33 days, P < .001) between 2003 and 2013 for those in the lowest quartile (1–4 days in 20003 and 1–5 days in 2013).
Fig. 3. Number of days of nonmedical pain reliever misuse (nmpr) in past-year among levels (quartiles) of cannabis use: 2003 and 2013 NSDUH.
To examine how the relative quartiles changed over time, cannabis use was standardized for 2003 and 2013 based on the observed cut-points in each year. For 2003, the marijuana use quartiles (based on number of days used per year), the quartiles for 2013 were Q1 (1–4 days), Q2 (5–43 days), Q3 (44–155 days) and Q4 (156–365 days). The quartiles for 2013 were Q1 (1–5 days), Q2 (6–51 days), Q3 (52–207 days), and Q4 (208–365 days). Two sets of statistical tests are presented, a test between 2003 and 2013 within each quartile that represents changes over time in the number of days of either NMPR or alcohol within each quartile. An overall chi-square test for 2003 and 2013 represents differences for NMPR and alcohol between the four quartiles within each separate year.
Source: 2003 and 2013 National Survey on Drug Use and Health (NSDUH, 2003 and 2013).
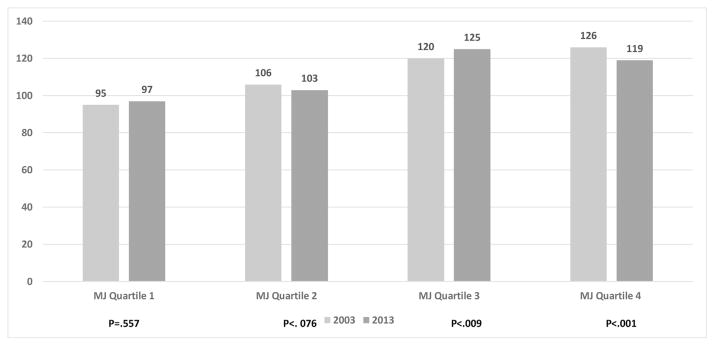
Fig. 4 also shows that as the days of cannabis use increased, the days of alcohol use also increased, and this finding held for 2003 (Chi-Square 23.5, 3df, P < .001) and 2013 (Chi-Square 4.1, 3df, P = .007). In 2013, persons engaging in the 4th quartile of cannabis use (76th or higher percentile of marijuana days) reported approximately 22 more days using alcohol compared to those using the lowest amount of cannabis in the 1st quartile (119 versus 97 days). This positive association was largely consistent for 2003, except that the 4th quartile reported 6 fewer days of alcohol use than those in the 3rd quartile (119 versus 125). This difference, however, was non-significant. Within each quartile, there were largely non-significant changes (quartile 1: P = .557, quartile 2: P = .076), or relatively small changes that were statistically significant (quartile 3: increase from 120 days to 125 days; quartile 4: decrease from 126 days to 119 days) in the number of days using alcohol between 2003 and 2013.
Fig. 4. Number of days of alcohol use in past-year among levels (quartiles) of cannabis use: 2003 and 2013 NSDUH.
To examine how the relative quartiles changed over time, cannabis use was standardized for 2003 and 2013 based on the observed cut-points in each year. For 2003, the marijuana use quartiles (based on number of days used per year), the quartiles for 2013 were Q1 (1–4 days), Q2 (5–43 days), Q3 (44–155 days) and Q4 (156–365 days). The quartiles for 2013 were Q1 (1–5 days), Q2 (6–51 days), Q3 (52–207 days), and Q4 (208–365 days). Two sets of statistical tests are presented, a test between 2003 and 2013 within each quartile that represents changes over time in the number of days of either NMPR or alcohol within each quartile. An overall chi-square test for 2003 and 2013 represents differences for NMPR and alcohol between the four quartiles within each separate year.
Source: 2003 and 2013 National Survey on Drug Use and Health (NSDUH, 2003 and 2013).
The last set of analyses sought to examine changes in the number of days using either NMPR or alcohol with cannabis over the 10 year study period, and whether changes varied by demographic characteristics. Table 1 shows that the largest increases in the number of days using NMPR were concentrated among those using cannabis the heaviest. More specifically, the increases were largest for those aged 35 or older. For example, those using the highest amount of cannabis and who were also aged 50 or older increased their use of prescription pain relievers by 67 days between the years of 2003 and 2013. In contrast, the younger age groups only increased their use of NMPR at most 20 days. Across all types of cannabis users, males typically increased their NMPR from 10 to 48 days. Females only increased their use over the 10-year period from 9 to 18 days. Among the heaviest cannabis users, those who were Hispanic and Black racial/ethnic groups had the largest increases in NMPR (about 45 days averaged across all groups). Finally, the biggest increases in use of NMPR occurred among those with no other co-occurring illicit drug use, mostly in the range of 8–50 days.
Table 1.
Average number of alcohol days in past year by levels (quartiles) of cannabis use: 2003 and 2013 NSDUH.
| MJ quartile 1
|
MJ quartile 2
|
MJ quartile 3
|
MJ quartile 4
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2003 | 2013 | Diff | 2003 | 2013 | Diff | 2003 | 2013 | Diff | 2003 | 2013 | Diff | |
| Age | ||||||||||||
| 12–17 | 13 | 33 | 20 | 23 | 20 | −3 | 53 | 52 | −1 | 49 | 44 | −5 |
| 18–25 | 25 | 28 | 3 | 25 | 43 | 18 | 33 | 52 | 19 | 47 | 48 | 1 |
| 26–34 | 9 | 42 | 33 | 72 | 62 | 10 | 43 | 59 | 16 | 39 | 84 | 45 |
| 35–49 | 5 | 26 | 21 | 24 | 59 | 35 | 28 | 177 | 149 | 56 | 105 | 49 |
| ≥50 | 30 | 36 | 6 | 156 | 58 | −98 | 48 | 105 | 57 | 15 | 82 | 67 |
| Sex | ||||||||||||
| Male | 18 | 41 | 23 | 49 | 59 | 10 | 34 | 82 | 48 | 50 | 75 | 25 |
| Female | 13 | 25 | 12 | 33 | 43 | 10 | 45 | 62 | 18 | 42 | 51 | 9 |
| Race | ||||||||||||
| White | 15 | 34 | 19 | 42 | 52 | 10 | 40 | 85 | 45 | 47 | 66 | 19 |
| Black | 12 | 23 | 11 | 42 | 73 | 21 | 39 | 57 | 18 | 40 | 96 | 56 |
| Hispanic | 21 | 34 | 13 | 29 | 57 | 28 | 23 | 66 | 43 | 39 | 96 | 57 |
| Other | 5 | 25 | 20 | 39 | 23 | −16 | 41 | 30 | −11 | 38 | 30 | −8 |
| Illicit drug, PYR | ||||||||||||
| Yes | 9 | 30 | 21 | 53 | 69 | 16 | 38 | 57 | 19 | 51 | 65 | 14 |
| No | 18 | 33 | 25 | 32 | 40 | 8 | 38 | 88 | 50 | 40 | 68 | 28 |
Note: Analyses conducted within SUDAAN, release 11.0. Source: 2003 and 2013 National Survey on Drug Use and Health (NSDUH, 2003 and 2013). To examine how the relative quartiles changed over time, cannabis use was standardized for 2003 and 2013 based on the observed cut-points in each year. For 2003, the marijuana use quartiles (based on number of days used per year), the quartiles for 2013 were Q1 (1–4 days), Q2 (5–43 days), Q3 (44–155 days) and Q4 (156–365 days). The quartiles for 2013 were Q1 (1–5 days), Q2 (6–51 days), Q3 (52–207 days), and Q4 (208–365 days).
Estimates in BOLD represent statistically significant change between 2003 and 2013.
The average number of days that alcohol was used in the past year was also examined within the same quartiles of cannabis users (Table 2). With the exception of age, there were no statistically significant changes between 2003 and 2013 based on biological sex, race/ethnicity, and illicit drug use status. With regard to age, the largest shifts in alcohol use occurred among those using cannabis the least. There was an average increase of 24 days for those aged 26 to 34 in the lowest quartile of cannabis use. Otherwise, there were significant declines by about 16 fewer days of alcohol consumption on average for those ages 12–17 in the past decade, averaging across all categories of use.
Table 2.
Average number of alcohol days in past year by levels (quartiles) of cannabis use: 2003 and 2013 NSDUH.
| MJ quartile 1
|
MJ quartile 2
|
MJ quartile 3
|
MJ quartile 4
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2003 | 2013 | Diff | 2003 | 2013 | Diff | 2003 | 2013 | Diff | 2003 | 2013 | Diff | |
| Age | ||||||||||||
| 12–17 | 35 | 23 | −12 | 51 | 34 | −17 | 71 | 55 | −16 | 87 | 72 | −15 |
| 18–25 | 84 | 82 | 2 | 104 | 90 | −14 | 110 | 104 | −6 | 125 | 103 | −22 |
| 26–34 | 102 | 126 | 24 | 132 | 121 | −9 | 135 | 144 | 9 | 121 | 132 | 11 |
| 35–49 | 146 | 116 | −30 | 104 | 121 | 117 | 146 | 132 | −14 | 142 | 141 | −1 |
| ≥50 | 95 | 96 | 1 | 150 | 122 | 28 | 114 | 172 | 58 | 193 | 128 | −65 |
| Sex | ||||||||||||
| Male | 111 | 104 | −7 | 121 | 111 | −10 | 130 | 127 | −3 | 135 | 122 | −12 |
| Female | 80 | 90 | 10 | 85 | 91 | 6 | 103 | 120 | 17 | 111 | 111 | 0 |
| Race | ||||||||||||
| White | 101 | 105 | 4 | 109 | 110 | 1 | 121 | 129 | 8 | 127 | 123 | −5 |
| Black | 94 | 73 | −21 | 110 | 87 | −23 | 110 | 112 | 2 | 127 | 106 | −21 |
| Hispanic | 61 | 82 | 21 | 96 | 77 | −19 | 118 | 125 | 7 | 131 | 102 | −29 |
| Other | 69 | 68 | −1 | 63 | 89 | 26 | 147 | 110 | −37 | 124 | 123 | −1 |
| Illicit drug, PY | ||||||||||||
| Yes | 127 | 126 | 1 | 116 | 131 | 15 | 125 | 120 | −5 | 137 | 129 | −8 |
| No | 90 | 93 | 3 | 103 | 95 | −8 | 117 | 126 | 9 | 120 | 113 | −7 |
Note: Analyses conducted within SUDAAN, release 11.0. Source: 2003 and 2013 National Survey on Drug Use and Health (NSDUH, 2003 and 2013). To examine how the relative quartiles changed over time, cannabis use was standardized for 2003 and 2013 based on the observed cut-points in each year. For 2003, the marijuana use quartiles (based on number of days used per year), the quartiles for 2013 were Q1 (1–4 days), Q2 (5–43 days), Q3 (44–155 days) and Q4 (156–365 days). The quartiles for 2013 were Q1 (1–5 days), Q2 (6–51 days), Q3 (52–207 days), and Q4 (208–365 days).
Estimates in BOLD represent statistically significant change between 2003 and 2013.
4. Discussion
This study investigated the nature of the relationship between the dual use of cannabis and NMPR as well as cannabis and alcohol use. We observed that more frequent use of cannabis was associated with more frequent use of NMPR, with findings replicating in 2013 and 2003. Kral et al. (2015) reported data somewhat counter to our findings, showing an inverse relationship between the number of times cannabis was used in relation to the proportion of opioid users in each category of marijuana use. Several methodological differences between the two studies may shed light on the sources of these differences. The Kral study combined all opioids together, with most of the sample using heroin, and all reporting being a person who injects drugs (PWID).
These two studies may not necessarily yield entirely contradictory findings once the methodological differences are taken into account. It is important to note that these findings are drawn from a current general population-based study, and the positive associations can be used to support conclusions of a synergistic relationship. But these types of frequency measures do not lend themselves to a definitive test of the causal relationship. The reason is that the NSDUH does not ask about concomitant use of both substances on the same occasion. Rather, the data show that persons who use cannabis more frequently also use prescription pain relievers more frequently as well. However, it is certainly possible that at the event level, a substitution effect may also occur such that dual users may opt for prescription-type pain relievers as a substitution for cannabis. However, a positive association is more consistent with the notion that greater use increases the probability that use of both substances occurs on the same day, especially for those who are regular cannabis users, such as those using more than 200 or so days a year.
A second notable finding was that the number of NMPR days within each quartile of cannabis use increased over the 10 year period. The replication of the findings in 2013 and 2003 are provided for a comparative purpose, but we also thought it important to examine how use was changing over time. As noted in the introduction, the primary focus of this paper is not to conduct a trend analyses. Rather, the two time points are essentially used as a snapshot to describe how the climate has changed between 2013 and a decade prior. The longitudinal analyses are to be regarded as preliminary, but some interesting findings emerged and they deserve some comment.
The population comparison between 2003 and 2013 indicates that as the number of dual users was slightly declining over the 10 year period, the number of days in which prescription pain relievers were used nonmedically actually increased. Increase occurred across all levels of cannabis use. Additional analyses were conducted to isolate the subgroups in which use may have been increasing the most. Surprisingly, it appears that the increases were largely concentrated in groups typically at lower risk for substance use, such as those aged 35 or older and persons who did not use illicit drugs in the past year. During this 10-year timeframe, there was an expansion of states adopting medical marijuana legislation. Medical marijuana patients typically are older and are not currently engaged in illicit drug use because prescribers are unwilling to write for high-risk patients (Reinarman et al., 2011). While this artifact may explain how the composition of users has changed over time, it doesn’t explain differences in usage patterns over time. Future studies are needed to understand how different age groups may have altered their consumption practices over time.
The decline in the prevalence of NMPR users, combined with the corresponding increases in the prevalence of cannabis users between 2003 and 2013 also deserve mention. These findings may suggest that public health interventions to limit access to opioid pain relievers may have had an effect on population-wide consumption, as evidenced by the declining use of NMPR. In contrast, the expansion of marijuana through increased medicalization may be leading to increased use. These findings may be regarded as preliminary, and provide direction for future studies to more carefully isolate confounding to statistically test for a causal pathway linking environmental policies and individual-level consumption. Additional discussions are also needed to resolve whether the magnitude of the changes over time are to be regarded as a positive or negative consequence of the increased availability of cannabis over time.
In terms of alcohol use, the pattern of consumption among dual users was less clear than it was for cannabis and NMPR. Those using the most amounts of cannabis were observed to have also used alcohol more frequently, relative to those using lower amounts of cannabis. While the number of dual users increased over the 10 year period, the number of days that alcohol was used did not appear to change.
Other than the lack of detailed information on concomitant use highlighted earlier in this paper, perhaps the most important limitation to highlight here is that this study did not stratify by states that had legalized cannabis use for medical purposes. The NSDUH only allows researchers to access the state-level estimates in a file that combines the raw data into two-year intervals. While this method increases the precision of the state-level estimates, particularly for the smallest states, it also precludes a more refined analyses of the yearly trends between adjacent years. Several studies investigating yearly trends in cannabis use and their relationship to state-wide legislation have used data sources that permit the linking of respondents within states (Cerda et al., 2012; Hasin et al., 2015). These sources are limited because they contain a small range of study years or narrow populations. Researchers have also published using the restricted NSDUH data, but the estimates are aggregated to the state-level, and only a limited number of state-level variables are available for analysis (Wall et al., 2011). There are also well-acknowledged limitations to self-report data. For this study, there may also be additional response bias related to changes in stigma and the social desirability as cannabis has become more normalized over the past decade.
The observed increases in the average number of days of dual use has some important implications for public health, largely due to the greater opportunities for harmful side-effect interactions. Alcohol and prescription pain relievers are known to cause significant depression on key biological systems (e.g., respiratory, neurological), so combining these substances with cannabis may have deleterious side-effects. While the effects of cannabis on respiratory and neurological systems are under study, all three substances act to interfere with higher order decision-making under even small doses, thereby placing an individual at risk for unintentional injury. Data from the former Drug Abuse Warning Network (DAWN) support potential dangers of combing substances with cannabis, as there was an 125% increase in the Emergency Department visits involving cannabis combined with prescription pain relievers in the 5-year period from 2004 to 2009 (SAMHSA, 2010). Studies have shown the positive benefits of medical marijuana. For instance, medical marijuana laws have been associated with lower rates of opioid-related fatal overdoses (Bachhuber et al., 2014). These results may not necessarily be inconsistent with data in this study, as the laws may have differential effects on various user groups, such as recreational NMPR versus persons who inject opioids. These findings do signal a need to specifically investigate the mechanisms linking policy changes to individual behaviors as a means to help resolve ecological biases in these national studies. Taken together, the findings from this study may help inform future prospective case-control studies as new legislation and policies are enacted. They may also inform behaviorally-based studies that utilize designs that can capture intensive longitudinal data. Such data could ultimately better describe consumption practices and associated motivations at a situational level each day.
Acknowledgments
Funding
Support for the writing of this paper was conducted with funding from the National Institute on Drug Abuse (NIDA, R01DA030427) and the Substance Abuse and Mental Health Services Administration.
Footnotes
Conflicts of interest
The authors have none to declare.
Contributors
SPN conceptualized the study and drafted the paper. NCP conducted the analyses and wrote the methods and results section. SN, NCP, and GAZ conceptualized the analysis of the paper. All authors reviewed and approved changes to the final manuscript.
References
- Allsop DJ, Dunlop A, Sadler C, Rivas G, Copeland J. Changes in cigarette and alcohol use during cannabis abstinence. Drug Alcohol Depend. 2015;146:e207. doi: 10.1016/j.drugalcdep.2014.01.022. [DOI] [PubMed] [Google Scholar]
- Bachhuber MA, Saloner B, Cunningham CO, Barry CL. Medical cannabis laws and opioid analgesic overdose mortality in the United States, 1999–2010. JAMA Int Med. 2014;174:1668–1673. doi: 10.1001/jamainternmed.2014.4005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerda M, Wall M, Keyes KM, Galea S, Hasin D. Medical marijuana laws in 50 states: investigating the relationship between state legalization of medical marijuana and marijuana use, abuse and dependence. Drug Alcohol Depend. 2012;120:22–27. doi: 10.1016/j.drugalcdep.2011.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton WM, Grant BF, Colliver JD, Glantz MD, Stinson FS. Prevalence of marijuana use disorders in the United States: 1991–1992 and 2001–2002. JAMA. 2004;291:2114–2121. doi: 10.1001/jama.291.17.2114. [DOI] [PubMed] [Google Scholar]
- FDA. [accessed 28.09.15];2015 http://www.fdanews.com/articles/173063-fda-advisory-panels-rejects-purdues-avridi?v=preview.
- Gugelmann HM, Perrone J. Can prescription drug monitoring programs help limit opioid abuse? JAMA. 2011;306:2258–2259. doi: 10.1001/jama.2011.1712. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Wall M, Keyes KM, Cerdá M, Schulenberg J, O’Malley PM, Galea S, Pacula R, Feng T. Medical marijuana laws and adolescent marijuana use in the USA from 1991 to 2014: results from annual, repeated cross-sectional surveys. Lancet Psychiatry. 2015;2:601–608. doi: 10.1016/S2215-0366(15)00217-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayaki J, Hagerty CE, Herman DS, de Dios MA, Anderson BJ, Stein MD. Expectancies and marijuana use frequency and severity among young females. Addict Behav. 2010;35:995–1000. doi: 10.1016/j.addbeh.2010.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kogan NM, Mechoulam R. Cannabinoids in health and disease. Dialogues Clin Neurosci. 2007;9:413–430. doi: 10.31887/DCNS.2007.9.4/nkogan. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kral AH, Wenger L, Novak SP, Chu D, Corsi K, Coffa D, Shapiro B. Is marijuana use associated with less opioid use among people who inject drugs. Drug Alcohol Depend. 2015;153:236–241. doi: 10.1016/j.drugalcdep.2015.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas P. Cannabis as an adjunct to or substitute for opiates in the treatment of chronic pain. J Psychoactive Drugs. 2012;44:125–133. doi: 10.1080/02791072.2012.684624. [DOI] [PubMed] [Google Scholar]
- Lynch KL, Shapiro BJ, Coffa D, Novak SP, Kral AH. Promethazine use among chronic pain patients. Drug Alcohol Depend. 2015;150:92–97. doi: 10.1016/j.drugalcdep.2015.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manchikanti L. Prescription drug abuse: what is being done to address this new drug epidemic? Testimony before the Subcommittee on Criminal Justice, Drug Policy and Human Resources. Pain Physician. 2006;9:287–321. [PubMed] [Google Scholar]
- Reinarman C, Nunberg H, Lanthier F, Heddleston T. Who are medical marijuana patients? Population characteristics from nine California assessment clinics. J Psychoactive Drugs. 2011;43:128–135. doi: 10.1080/02791072.2011.587700. [DOI] [PubMed] [Google Scholar]
- SAMHSA. [accessed 5.06.2015];Drug Abuse Warning Network: Detailed Tables: National Estimates, Drug-Related Emergency Department Visits for 2004–2009. 2010 http://www.samhsa.gov/data/DAWN.aspx.
- SAMHSA. Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2014. [Google Scholar]
- Wall MM, Poh E, Cerda M, Keyes KM, Galea S, Hasin DS. Adolescent marijuana use from 2002 to 2008: higher in states with medical marijuana laws, cause still unclear. Ann Epidemiol. 2011;21:714–716. doi: 10.1016/j.annepidem.2011.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson S, Benson J. Marijuana and medicine: assessing the science base: a summary of the 1999 institute of medicine report. Arch Gen Psychiatry. 2001;57:547–552. doi: 10.1001/archpsyc.57.6.547. [DOI] [PubMed] [Google Scholar]