Abstract
Objective
The purpose of this study was to compare the effectiveness of three interventions designed to promote hearing protector device (HPD) use.
Design
Randomized controlled trial.
Study Sample
Farm operators (n=491) were randomly assigned to one of 5 intervention groups: 1) interactive Web-based information with mailed assortment of HPDs; 2) Interactive Web-based information only; 3) static Web-based information with mailed assortment of HPDs; 4) Static Web-based information only; or 5) mailed assortment of HPDs only. Data were analyzed using a mixed model approach.
Results
HPD use increased among all participants, and increased more among participants receiving the mailed HPDs (with or without information) compared to participants receiving other interventions. Participants receiving the interactive Web-based information had comparable increased use of HPDs to those receiving the static Web-based information. Participants receiving the mailed HPDs had more positive situational influences scale scores than other participants. Program satisfaction was highest among mailed and Web-based information groups.
Conclusions
A mailed assortment of hearing protectors was more effective than information. Interactive and static information delivered via Web were similarly effective. Programs interested in increasing HPD use among farmers should consider making hearing protectors more available to farmers.
Keywords: Hearing loss prevention, hearing conservation, farmers, randomized controlled trial
Noise-induced hearing loss (NIHL) is highly prevalent among workers, particularly among farmers. Noise-induced hearing loss is among the most common work-related diseases, and the second-most self-reported occupational disease or injury (Conway, Simmons, Talbert 1993). Estimates of prevalence rates for NIHL among farmers vary greatly, and have been reported to be 17% (Thelin et al. 1983), 22% (Gomez et al. 2001), 38% (Stewart, Scherer, Lehman 2003), 65% (Marvel et al. 1991), and 72% (Beckett et al. 2000). In comparison studies, farmers were more likely to have hearing loss than non-farmers (Marvel et al. 1991; Rabinowitz et al. 2005; Thelin et al. 1983).
NIHL is characterized by loss of hearing in higher frequencies. It is permanent, incurable, and progresses insidiously with continued exposure to high levels of noise. Most people are unaware that they are affected until it is already moderately severe (Morata T.C. 1995).
NIHL negatively affects physical and emotional functioning, social life, and employment. It also results in heavy social and economic burdens on families and communities from all ethnic and socioeconomic groups. Most persons with NIHL also experience tinnitus (Hetu, Getty, Quoc 1995). The condition is costly to the individual and society as it includes workers’ compensation (for employees) and medical costs (NIOSH 1996). Importantly, hearing loss has also been associated with increased risk for injury among farmers (Choi et al. 2005).
Unlike workers in general industry, systems to protect workers from NIHL are not present in the farm work setting
Few farmers are protected by the OSHA Hearing Conservation Standard (i.e., noise level monitoring and a hearing conservation program for at-risk employees which includes audiometric testing, training, and provision of hearing protection devices) (Suter 2009). Also, there is no labor advocacy for worker hearing health and work-based health programs because most farms in the US are small, family-run organizations (Murphy 1992). Farmers, unlike most workers, must function as their own safety specialists and industrial hygienists in that they alone determine when to wear, which types are suitable, where to purchase, and how much to pay for HPDs (Suter 2009). Because of this, it is likely that most farmers underestimate their exposure to noise hazards and consequences of noise exposure, and may not be knowledgeable about NIHL prevention techniques. There are few expectations and demands for farmers’ use of hearing protection. Even when the farmer is aware of noise exposure and the hearing health hazard, it is unlikely that he has trialed various types of hearing protection in order to select those most suitable (McCullagh 2011). Further complicating the use of HPDs, farm work is characterized by frequent changes in tasks and noise exposure levels, resulting in intermittent need for use and different types of hearing protection over the course of a workday (McBride, Firth, Herbison 2003). It is, therefore, unlikely that one type of hearing protection will suit any farmer for all of his work tasks.
Although noise elimination would be the most preferred method of prevention of NIHL, this approach is often not technically or economically feasible in the farm work environment (Murphy 1992). However, consistent use of hearing protection devices is effective in preventing NIHL (Hong, Chen, & Conrad 1998; Sataloff & Sataloff 1993; Savell & Toothman 1987). Although there are several types of hearing protectors marketed (e.g., foam plugs, ear muffs), there is no “best” type of hearing protection; the “best” is the one the user prefers and will wear. Selection of type of hearing protection device is highly individualized based on noise exposure, comfort, and convenience (NIOSH 1996; NIOSH 1996).
Several federal agencies have identified NIHL as a priority. These include Healthy People 2020 (DHHS 2010), NIOSH (National Institute for Occupational Safety and Health (NIOSH) 2008), and NIH (NIDCD 2009).
Epidemiological studies show that there is a great need for programs and services to increase hearing protector use among farmers, and that unlike some other worker groups, there is no ceiling effect limiting effectiveness of interventions (Gates and Jones 2007; McCullagh, Lusk, Ronis 2002; McCullagh, Ronis, Lusk 2010). Studies have identified cognitive predictors of hearing protector use among farmers, and have demonstrated that farmers are interested in increasing their use of hearing protectors (McCullagh, Ronis, Lusk 2010). Predictors-based and Internet-based interventions have demonstrated effectiveness in other groups (Alexander, McClure, Calvi 2010; Joseph et al. 2007; Strecher et al. 2008; Ubel et al. In press.; van den Berg, Schoones, Vliet Vlieland 2007). The purpose of this study was to contrast the effects of three alternative NIHL-prevention intervention strategies, delivered in various combinations, on HPD use and use-related attitudes/beliefs. Specifically, the three approaches included: a) an interactive, predictors-based intervention delivered via the Internet; b) a static informational Web site designed to increase farmers’ use of HPDs; and c) a mailed sampler of HPDs, e.g., ear muffs, plugs.
Conceptual Framework
Pender’s (Pender, Murdaugh, & Parsons, 2010) Health Promotion Model guided development of the targeted intervention in this clinical trial. The interventions targeted change in use of hearing protection as well as attitudes and beliefs influencing HPD use. Selected use-related attitudes and beliefs (i.e., barriers to HPD use, situational influences on HPD use, and interpersonal influences on HPD use) were the focus of the interventions. Previous research indicates that HPD use is associated with these attitudes and beliefs (McCullagh, Lusk, Ronis 2002; McCullagh, Ronis, Lusk 2010).
Design and Methods
Sample
Participants were adults aged 18 or older, active in production at least 20 hours per week on average, had the ability to read English, and had computer and Internet access. In order to access farmers, a unique and widely dispersed population, the study team collaborated with a variety of farmer organizations (e.g., American Farm Bureau Federation). Study team members attended selected farmer organization meetings, visiting personally with farmers in group and individual settings to explain the study purpose and procedures, and distribute study information. Recruitment continued until the enrollment quota was met.
Measurements
Outcome measures were taken at 6 and 12 months post-intervention, and included self-reported frequency of HPD use and related attitudes and beliefs. The outcome variables for the study are based on the Predictors of Farmers’ Use of Hearing Protection Model and include cognitive and affective factors that are specific to the behavior of HPD use (i.e., frequency of HPD use, perceived barriers to HPD use, self-efficacy for HPD use, access to HPDs, and interpersonal influences on HPD use).
The HPD Use instruments measuring the concepts from the theoretical model, together with their corresponding alpha reliability coefficients from the current study are described in Table 1. Development of these scales included pretest, revision, and review for construct validity by an expert panel; the process is described elsewhere (McCullagh, Lusk, Ronis 2002). All have alpha coefficients near or above .70.
Table 1.
Summary statistics and Internal consistency measures of six HPD use related Attitudes (N=491)
| Scale Name | Number of items | Range of scores | Mean ± SD | Cronbach’s Alpha |
|---|---|---|---|---|
| Barriers to HPD usea | 11 | 1.27–6.0 | 3.68 ± 0.98 | 0.886 |
| Situational influences on HPD usea | 7 | 1.0–6.0 | 3.69 ± 1.19 | 0.835 |
| Self-efficacy of HPD usea | 3 | 1.0–6.0 | 4.92 ± 1.03 | 0.921 |
| Interpersonal normsb | 5 | 1.0–6.0 | 4.67 ± 0.95 | 0.834 |
| Interpersonal modelingc | 2 | 1.0–6.0 | 3.19 ± 1.24 | 0.683 |
| Interpersonal supportd | 4 | 1.0–6.0 | 3.26 ± 1.13 | 0.827 |
SD=Standard deviation;
Rating scale (1=strongly disagree; 6=strongly agree);
Rating scale (1=not at all; 3=a lot);
Rating scale (1=never; 3=usually);
Rating scale (1=never; 3=often)
Use of Hearing Protection Devices was measured by self-report. The Farmers’ Use of Hearing Protection Scale was developed for use among farmers and consists of four items reporting the percentage of time that workers actually used hearing protection when they were exposed to high noise in specific work settings: in the field, in the shop, with livestock, and at the grain-handling system. The instrument defined high noise as present whenever one had to raise one’s voice to be heard by another person at a distance of three feet or less. In a prior study (McCullagh, Ronis, Lusk 2010), farmers reported a wide range of frequency of use and no difficulty using the instrument. The scale was scored as the average percentage use among settings in which the farmer reported being exposed to high noise. For this study, an additional question assessed subjects’ use of HPDs during noisy recreational activities, as a separate measure of use, and a further assessment of risk for NIHL. In this study, 22.4% of participants reported zero use; 77.6% reported some use.
In studies comparing the validity of observed and self-reported HPD use (Griffin et al. 2009; Lusk, Ronis, Baer 1995), self-report and observations were highly correlated (.89 and .92–.99, respectively), suggesting that self-report is an appropriate measure of HPD use. Further, the low reported use by farmers in previous studies (Carpenter et al. 2002; Gates and Jones 2007; Jenkins et al. 2007; McCullagh, Lusk, Ronis 2002; Stewart, Scherer, Lehman 2003) demonstrates a low social desirability effect. Also, other protocol design features aided in preventing participants’ desire to please investigators: the impersonal mode of data collection, emphasis on request for actual use, and preface stating understanding that it is not easy to always use. In addition, among farmers, self-report can be expected to be at least as valid due to the absence of demand characteristics (such as mandates, policies and regulations for use) found in industrial settings.
Perceived Barriers to HPD Use Scale. The instrument to measure farmers’ barriers to use of hearing protection was derived from one used to measure this concept among factory workers (Lusk, Ronis, Hogan 1997). A sample item from this scale is, “Even though it may be a good idea, I don’t have time to use hearing protection.” The 11-item, 6-point Likert scale was significantly and negatively related to HPD use in a previous sample of farmers (McCullagh, Ronis, Lusk 2010).
Perceived Benefits of HPD Use was measured using the Perceived Benefits of Farmers’ Use of Hearing Protection Scale. The Benefits of Use Scale was derived from one used with factory (Lusk et al. 1994) and construction workers (Lusk, Ronis, Hogan 1997). The 10-point Likert scale consists of 5 items designed to measure the degree of importance of such concepts as “keep out noise” and “protect my hearing.” The scale was significantly and positively related to HPD use in a previous sample of farmers (McCullagh, Ronis, Lusk 2010).
The Perceived Self-Efficacy in Use of Hearing Protection among Farmers Scale consists of a 6-item, 6-point Likert scale derived from one developed by Lusk (Lusk et al. 1994). A sample item from this scale is, “I am not sure I can tell if my hearing protection is working effectively.” In a previous sample of farmers (McCullagh, Ronis, Lusk 2010), perceived self-efficacy was positively related to HPD use.
The Situational Influences on Farmers’ HPD Use Scale was positively related to HPD use in a previous sample of farmers (McCullagh, Ronis, Lusk 2010), but did not achieve significance. A sample item from this Likert scale is, “Ear plugs are available close to high-noise areas.”
Norms, Modeling, and Support were operationalized in three subscales: Perceived Interpersonal (PIP) Norms, PIP Modeling, and PIP Support, modified for use with farmers (McCullagh, Ronis, Lusk 2010). Interpersonal norms for HPD use include the respondents’ beliefs about how much others (e.g., family members, friends, supervisor, and coworkers) think they should wear hearing protection. Interpersonal support for HPD use refers to encouragement or praise from family, friends, coworkers, and supervisors about the respondents’ use of hearing protection. Interpersonal modeling of HPD use is how much respondents believe family members and other farmers use hearing protection when exposed to noise. These scales showed significant and positive relationships to HPD use. A sample item from the interpersonal norms scale is, “Please indicate how much you believe certain people think you should wear hearing protection when you are in a high-noise work environment. The item lists selected roles, e.g., healthcare workers, and response options include not at all, sort of, and a lot.
Demographic characteristics relating to farmers were collected via web-based survey. Items include primary product produced, occupational role, age, race, ethnicity, and gender.
Intervention
In this randomized controlled intervention trial, we delivered three interventions, in various combinations, to study participants. The three interventions consisted of an interactive web-based educational intervention, a static educational web intervention, and a mailed sampler of HPDs. Due to ethical concerns, the study did not include a no-intervention control. Participants were randomly assigned to intervention groups by a computer-generated random allocation sequence at the time of study registration. This project used simple urn randomization (no blocks or stratification) to assign participants to one of five study arms. For each new assignment, the program found the arm(s) with the lowest number of participants and randomly selected one of those arms using the Python RANDOM function (a random number generator). The allocation sequence was implemented in real-time as individuals enrolled in the program, and all steps were completed by the computer algorithm, concealing any sequence from study staff. The algorithm for the allocation sequence was developed by the Center for Health Communications Research (University of Michigan, USA) using input from the study team. Participants enrolled online without any help from study staff, and were assigned to an intervention arm by the computer program. Table 2 displays the intervention assignments by group.
Table 2.
Study Conditions and Observations
| Group | Pretest | Intervention | Post-tests | |||
|---|---|---|---|---|---|---|
| Interactive Web intervention | Static Web intervention | Mailed HPDs | 6 month | 12 month | ||
| 1 | X | X | X | X | X | |
| 2 | X | X | X | X | ||
| 3 | X | X | X | X | X | |
| 4 | X | X | X | X | ||
| 5 | X | X | X | X | ||
Interactive Web-based Information
This targeted intervention included a number of features and techniques designed to promote behavior change, including high interactivity, model-driven approaches, role modeling, and cognitive, demonstration, and persuasion techniques. Rather than passively viewing a programmed linear presentation, participants were free to select the sequence of features they visited, as well as the time spent in each feature and number of visits to the site. The intervention was highly interactive. For example, an interactive sound level meter displayed noise levels (in decibels) and played audio recordings of common work (e.g., farm equipment and livestock) and recreational (e.g., firearms) noises when the user selected the corresponding graphic. Additional interactive activities focused on benefits of each type of HPD, tips for purchasing HPDs, and tips for HPD use in temperature extremes. The intervention was also based on demonstrated predictors of HPD use. These predictors are the factors found to be salient to the behavior, and include perceived barriers to HPD use and situational influences on HPD use. Analysis of individual Barriers and Situational Influences Scale items have revealed precisely which attitudes and beliefs are negatively correlated with HPD use, and drove intervention content. For example, previous research demonstrated that time required to insert and apply hearing protection was negatively correlated with HPD use. (McCullagh, Lusk, Ronis 2002) One intervention activity that focused on this barrier included a farmer testimonial of HPD use not getting in the way of timely completion of farm tasks, and information about selecting types of HPD that are quick to use for intermittent noise exposures common in farming. The intervention also included role modeling techniques, including videotaped, non-scripted interviews with actual farmers who are users of HPDs. These farmers’ comments dispel myths about HPD use on the farm and describe benefits and strategies of HPD use they have developed and found useful in their own farm operations. In a study by Morgan (Morgan et al. 2002), farmers evaluated this narrative approach more favorably than other types of messages (e.g., information and statistics). In addition, the intervention included information highly relevant to the farm and rural environments, such as farm noise hazards, effect of farm noise on hearing, methods of hearing conservation, animated graphic of normal and sound-damaged hearing cells, and video demonstration of proper foam plug insertion technique. Non-scripted video recorded messages of farmers experienced in HPD use offered advice for hearing conservation on the farm.
Static Web-based Information
An alternative intervention was the delivery of standard information promoting HPD use delivered via Internet. This intervention was based on informational brochures previously developed for use by farmers (i.e., Have You Heard? (National Institute for Occupational Safety and Health (NIOSH) 2007a) and They’re Your Ears: Protect Them (National Institute for Occupational Safety and Health (NIOSH) 2007b). These brochures, including color graphics and text, are available on the Internet (as PDF files). Unlike the interactive Web-based intervention, this approach offered no interactivity, animation, explication of farmer-generated tips and techniques for addressing common barriers to hearing protector use, audio, and video, hotlinks, or farmer testimonials, and included minimal use of color.
Mailed Hearing Protection Devices (HPDs)
A sampler of assorted HPDs (i.e., muffs, semi-aurals, roll-down plugs, and pre-molded plugs) was mailed to selected participants, together with manufacturers’ standard written instructions for use. This approach was used alone, as well as in combination with Web-based educational interventions described above.
Data Analysis
Descriptive statistics were calculated for continuous and discrete measures at baseline. A random intercept mixed model was used to explore the fixed effects of the three NIHL prevention interventions over time, adjusting for age and gender. The model includes a random intercept for subjects, to control for subjects’ non-independence of repetitive measurements. Random intercept model selection was done using a Likelihood Ratio (LR) test. A compound symmetric covariance structure was specified in the final model after investigating other candidates using LR (nested model) or Akaike Information Criterion (non-nested model). Each of the attitudes and beliefs was modeled separately in order to investigate the effects of web interventions and mailed hearing protection devices. Paired t-tests were performed on HPD use and six attitudes-related outcomes to compare their means at 6 months and 12 months. The data were analyzed within two research designs. First was the complete factorial 2 (interactive vs static web) × 2 (sent HPDs) × 3 (times: baseline, 6 months, 12 months). This did not include the condition in which participants were simply sent HPDs. The second design included all conditions in an incomplete factorial 3 (interactive web vs static web vs no web) × 2 (sent HPDs) × 3 (times: baseline, 6 months, 12 months). SAS 9.3 (SAS Institute Inc., Cary, NC, USA) and SPSS 22 were used for all analyses. Significance was determined at p <.05.
Results
The initial total sample consisted of 656 respondents who were assessed for eligibility; 159 were excluded (primarily due to declination to participate and inability to verify email addresses), and five participants resigned from the study. Table 3 describes the sample. Of the 491 study participants, the average age was 45 years (SD=15 years). The average time using HPDs when in high noise at baseline was 29.5% (SD=28%), with over one-fifth (22.4%) of subjects reporting no use of HPDs. One-fourth of the study population used HPDs 50% or more of the time. The majority of participants were male (77.2%), non-Hispanic (99%), Caucasian (98%), working as a manager (72%) on the farm and owned/worked on a small sized farm (less than 500 acres, 61%).
Table 3.
Summary statistics for baseline Characteristics of HOTF study (N=491)
| Characteristics | Summary statistics |
|---|---|
|
| |
| HPD use | 29.5 ± 28 |
| No use | 22.4% |
| Less than 50% use | 53.1% |
| 50% or more use | 24.5% |
| Age (years) | 44 ± 15 |
| Years farming | 25 ± 16 |
| Men | 77.2% |
| Hispanic | 1.2% |
| Role | |
| Manager | 71.5% |
| Full time paid | 11.4% |
| Part time paid | 17.1% |
| Size of Farm | |
| Less than 500 acres | 61.3 % |
| 500–999 acres | 15.7% |
| 1000–2000 acres | 10.6 % |
| 2000+ acres | 12.4 % |
Results from mixed model analyses are displayed in Tables 4, 5, and 6. At first, models with three-way interaction (web intervention * HPD * time) were fitted for HPD use and six attitude outcomes. Reduced models were refitted since 3-way interaction terms for each models were non-significant. Table 4 consists of results from reduced model fit of HPD use using both research designs 2×2×3 and incomplete 3×2×3. Table 5 portrays the reduced mixed model results of six HPD use-related attitude outcomes using 2×2×3 study design only. Following results were discussed considering the 2×2×3 design.
Table 4.
Random Intercept Mixed Model results of HPD use using 2×2×3 & incomplete 3×2×3 designs
| 2×2×3 design | Incomplete 3×2×3 design | |||||
|---|---|---|---|---|---|---|
| Effect | DF | F value | p | DF | F value | p |
| Age | (1,383) | 0.14 | .70 | (1,478) | 1.17 | .28 |
| Gender | (1,387) | 2.78 | .10 | (1,484) | 6.77 | .01* |
| HPD | (1,384) | 2.89 | .09 | (1,478) | 3.02 | .08 |
| Web intervention | (1,384) | 0.10 | .76 | (2,480) | 0.09 | .91 |
| Time | (2,721) | 135.97 | <0.001* | (2,895) | 128.21 | <0.001* |
| HPD* Web intervention | (1,384) | 4.48 | .035* | (1,477) | 4.71 | .03* |
| HPD*Time | (2,721) | 4.81 | .008* | (2,893) | 4.92 | .008* |
| Web intervention*Time | (2,721) | 0.30 | .74 | (4,896) | 0.33 | .88 |
Dependent measure: Percentage of HPD use. Statistically significant p-values are indicated by*.
Table 5.
Results from Six Random Intercept Mixed Models Analyses For Barriers, Situational, Self-Efficacy, Interpersonal Norms, Modeling, and Support Considering 2×2×3 Design.
| Barriers | Situational | Self-efficacy | Interpersonal Norms | Interpersonal Modeling | Interpersonal Support | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||||||
| Effect | DF | F value | p | DF | F value | p | DF | F value | p | DF | F | p | DF | F | p | DF | F | p |
|
| ||||||||||||||||||
| Age | (1,388) | 1.36 | .24 | (1,386) | 9.96 | .002* | (1,382) | 3.26 | .07 | (1,384) | 0.28 | .60 | (1,385) | 3.83 | .05* | (1,386) | 0.95 | .33 |
| Gender | (1,389) | 2.47 | .12 | (1,387) | 0.07 | .79 | (1,383) | 2.1 | .14 | (1,385) | 0.11 | .74 | (1,386) | 0.09 | .76 | (1,387) | 0.31 | .58 |
| Web intervention | (1,390) | 0.06 | .81 | (1,388) | 0.10 | .75 | (1,384) | 0.08 | .77 | (1,385) | 0.14 | .71 | (1,385) | 0.97 | .32 | (1,387) | 0.43 | .51 |
|
| ||||||||||||||||||
| HPD | (1,389) | 6.31 | .01* | (1,388) | 4.6 | .03* | (1,384) | 0.06 | .81 | (1,385) | 0.29 | .59 | (1,386) | 0.01 | .92 | (1,387) | 0.01 | .91 |
|
| ||||||||||||||||||
| Time | (2,740) | 38.46 | <.001* | (2,740) | 92.47 | <.001* | (2,743) | 27.26 | <.001* | (2,735) | 11.95 | <.001* | (2,737) | 44.34 | <.001* | (2,737) | 30.74 | <.001* |
|
| ||||||||||||||||||
| Web intervention * time | (2,740) | 1.88 | .15 | (2,740) | 3.34 | .036* | (2,743) | 0.46 | .63 | (2,735) | 0.31 | .74 | (2,737) | 0.82 | .44 | (2,737) | 0.08 | .93 |
|
| ||||||||||||||||||
| HPD * Time | (2,740) | 1.78 | .17 | (2,740) | 5.65 | .004* | (2,743) | 1.12 | .33 | (2,735) | 0.19 | .83 | (2,737) | 0.58 | .56 | (2,737) | 1.47 | .23 |
| HPD * Web intervention | (1,389) | 0.05 | .82 | (1,387) | 0.20 | .66 | (1,384) | 0.09 | .77 | (1,385) | 0.07 | .80 | (1,386) | 0.75 | .39 | (1,387) | 1.16 | .28 |
Statistically significant p-values are indicated by *.
Table 6.
Results from Random Intercept Mixed Model of HPD Use and Attitudes using 2 × 2 × 3 design with Three-way Interaction Term
| Effects | Use of HPDs | Self-efficacy | Barriers | Situational Influences | Inter-personal Norms | Inter-personal Modeling | Inter-personal Support | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F | p | F | p | F | p | F | p | F | p | F | p | F | p | |
| Age | 0.14 | .71 | 3.25 | .07 | 1.37 | .24 | 9.93 | .002* | 0.28 | .60 | 3.86 | .05* | 0.64 | .43 |
| Gender | 2.76 | .10 | 2.15 | .14 | 2.49 | .12 | 0.06 | .80 | 0.11 | .74 | 0.09 | .76 | 1.46 | .23 |
| Web-based intervention | 0.10 | .76 | 0.08 | .77 | 0.06 | .81 | 0.1 | .75 | 0.14 | .71 | 0.98 | .32 | 1.89 | .15 |
| HPD | 2.91 | .09 | 0.06 | .81 | 6.28 | .01* | 4.65 | .03* | 0.29 | .60 | 0.01 | .91 | 0.01 | .92 |
| Time | 135.51 | <0.001* | 27.20 | <0.001* | 38.25 | <0.001* | 92.40 | <0.001* | 11.95 | <0.001* | 44.69 | <0.001* | 31.83 | <0.001* |
| Web-based intervention*Time | 0.30 | .74 | 0.46 | .63 | 1.87 | .15 | 3.35 | .04* | 0.31 | .74 | 0.81 | .44 | 0.33 | .86 |
| HPD*Time | 4.79 | .009* | 1.13 | .32 | 1.79 | .17 | 5.66 | .004* | 0.18 | .84 | 0.55 | .58 | 1.42 | .24 |
| HPD*Web-based intervention | 4.56 | .03* | 0.11 | .74 | 0.04 | .84 | 0.21 | .65 | 0.07 | .79 | 0.72 | .40 | 1.22 | .27 |
| HPD* Web-based intervention*Time | 0.34 | .71 | 1.04 | .35 | 0.64 | .53 | 1.46 | .23 | 0.96 | .38 | 2.58 | .08 | 1.52 | .22 |
Statistically significant p-values are indicated by *.
HPD use increased over time in all groups
Overall, the greatest increase in HPD use occurred at 6 months, with use continuing to increase at a somewhat slower rate at 12 months (Mean use of HPD at Baseline: 29.5 %, 6 months:48.7%, 12 months 49.3%). Mixed model results shown in Table 4 also support this increasing trend of HPD use (F (2,721) =135.97, p=<.001). Paired t-test result reveals the fact that there is statistically significant increase in mean HPD use at 12 months compare to 6 months (t[336]=2.31, p=0.02).
There was no difference in HPD use between participants receiving the interactive Web-based intervention and those receiving the static Web-based intervention (F (1, 384) = 0.10, p=.76). The Web intervention by time interaction was non-significant for use of HPDs (F (2, 721) = 0.30, p=.74) (see Table 4).
Participants receiving mailed HPDs had higher HPD use than participants not receiving mailed HPDs over time
Results were examined for interaction of mailed-HPDs-by-time on HPD use. There was a significant effect of mailed HPDs by time (F (2, 721) = 4.81, p=.008; Table 4). Subjects receiving mailed HPDs increased their use of HPDs more than subjects in other groups.
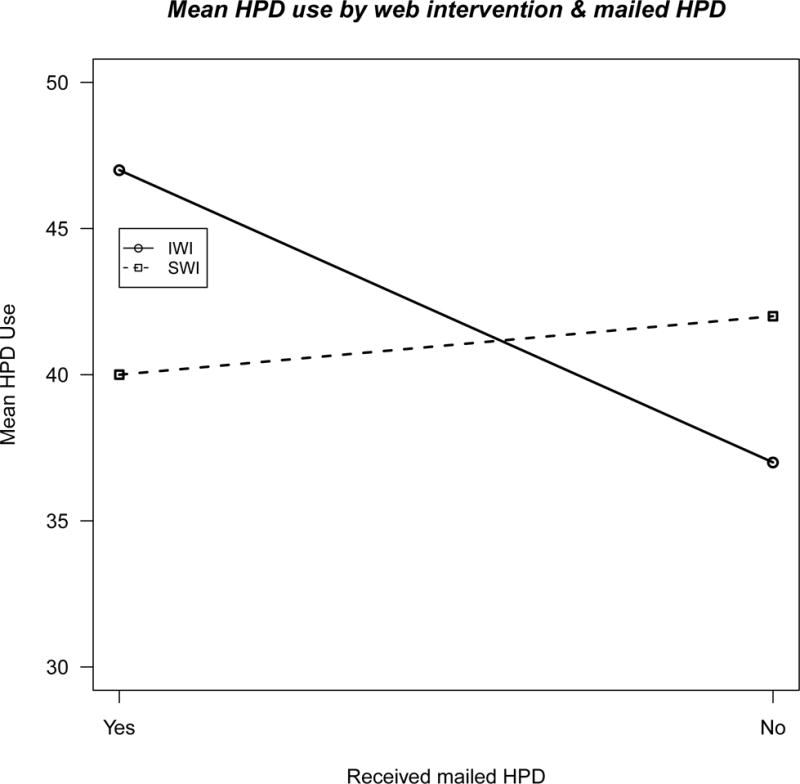
HPD use was higher in the group receiving both the interactive Web-based intervention and mailed HPDs
There was significantly higher HPD use in the interactive Web-based intervention group that had received HPDs compared to the group receiving the static intervention who also received HPDs (F (1, 384) = 4.48, p=.035; Table 4). Figure 1 shows that participants who received the interactive Web-based intervention and also received mailed HPD reported higher use of HPD than others.
Figure 1.
HPD use-related attitudes and beliefs became more positive over time among participants in all groups
The results of the six mixed effect models showed the effect of time was highly significant for each of the six attitudes and beliefs compared to baseline measures (p<.001)(see Table 5). Among six attitudes, the following outcome scores significantly stayed higher at 12 months compared to 6 months according to paired t-tests: situational (t(348)=2.92 & p=0.004), interpersonal modeling (t(350)=4.10 & p=<0.01), and support (t(349)=2.72 & p=0.007).
Participants receiving the interactive Web-based intervention had a different trajectory of situational influences
There was a statistically significant difference present in situational influence scale among participants receiving the Interactive Web-based intervention and those receiving the Static Web-based intervention over time (F (2, 740) = 3.34, p=.036) (see Table 5). The trend was for higher ratings on situational influences at 6 months but not at 12 months. None of the other attitudes have shown any significant effect of Web intervention over time.
Participants receiving mailed HPDs had more positive situational influences scale scores over time than participants not receiving the mailed HPDs
The mailed HPD-by-time interaction effect for situational influences was statistically significant (F (2, 740) = 5.65, p=.004 as shown in Table 5). Although HPD use-related attitudes and beliefs improved in all groups, participants receiving mailed HPDs had more positive situational influences scale scores (e.g., access) than participants in other groups. However there was not an improvement in other HPD-related attitudes/beliefs (i.e., barriers, self-efficacy, or interpersonal attitudes) over participants in other groups (Table 5). In other words, unlike other measures of HPD-related attitudes and beliefs, there was significantly more improvement in situational influences among participants receiving mailed HPDs than among those not receiving HPDs.
Effect of mailed HPDs
Mailed HPDs turned out to be a significant predictor of HPD use-related attitudes barrier and situational influences (Table 5). Average barrier and situational scores were better for the group who had received mailed HPDs than other group.
Effect of Gender
There is a significant gender difference present in the use of HPDs in the incomplete 3×2×3 design (F (1, 484) = 6.77, p=.01; Table 4). Men were more likely than women to self-report their use of HPD in this study cohort. The gender difference was non-significant within the 2×2×3 design (Table 4).
Effect of Age
Age of the participants was a significant predictor for situational influences and interpersonal modeling. Older participants were more likely to report more situational influences and interpersonal modeling on HPD use (Table 5).
There was no relationship between the number of visits to the Interactive or Static Web sites and use of HPDs
The study design required participants to visit the study Web site to enter survey data, and most participants visited only three times (i.e., baseline, 6 months, and 12 months); only a few participants visited more than 3 times (N=86 (22%)). The distribution of the visits to the interactive and Static Web site is shown in Figure 2. The distribution of subjects visiting the interactive and static Web sites more than three times was small for both groups (21% and 23%, respectively).
Figure 2.
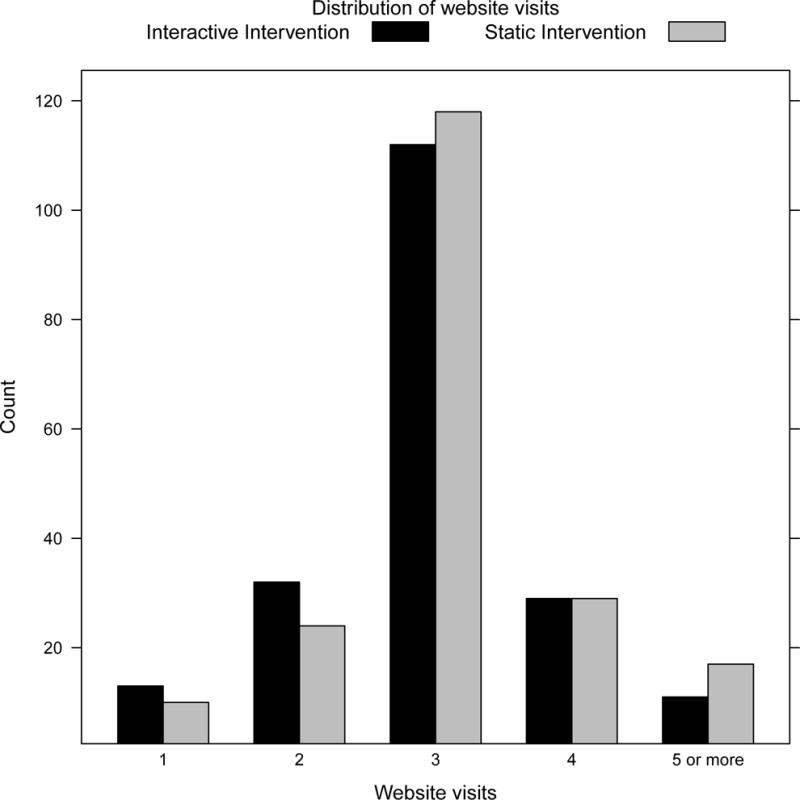
We created two groups for number of visits: had a. 3 visits, b. more than 3 visits. To assess the association between number of visits and use of HPD, we performed t-tests using the information on use of HPD from 12 months. The t-test results suggest that there is no evidence to reject the null hypothesis for either the interactive (t(149)=0.80, p=.43) or static (t(152)=−0.95, p=.34) interventions. Use of HPDs did not differ by the number of visits to either web site.
There was no statistical interaction between intervention delivery mode (Interactive versus Static) and the mailed HPDs on use of HPDs or HPD-related attitudes and beliefs
The three-way interaction web-intervention × mailed-HPDs × time was non-significant for HPD use (F (2, 719) = 0.34, p=. 71, Table 6), as well as attitudes/beliefs. In brief, there was no interaction between Web intervention delivery mode and mailed HPDs in their effects on HPD use or on HPD use-related attitudes and beliefs over time.
Participant satisfaction with the Interactive Web-based program was high
Satisfaction with the programs was very high, with 91% (Interactive), 88% (static), and 97% (HPD only) rating the program as very good or excellent. Nearly all participants using Interactive, Static, and HPD only programs indicated they would recommend the site to others (94%, 95%, and 95%, respectively).
Discussion
Although noise-induced hearing loss is preventable, it is highly prevalent among farm operators, and has been proclaimed a priority among US federal agencies, (National Institute for Occupational Safety and Health (NIOSH) 2008; NIDCD 2009; United States Department of Health and Human Services 2000) there are few programs to protect farm operators from this work hazard. In this study, HPD use improved over time among all groups (i.e., interactive Web-based, static Web-based, and mailed HPDs). However, the greatest increase in use was seen among those who received a mailed assortment of hearing protectors (i.e., muffs, foam plugs, pre-molded plugs, and semi-aurals). One surprising finding was that participants who received informational messages (interactive or static Web-based information) did not use HPDs more frequently than those who did not receive informational messages (i.e., those who received only a mailed assortment of HPDs). Results of this study support the findings of a previous qualitative study with a purposive sample (McCullagh M. C., Robinson C. 2009) showing that obstacles to HPD use among farmers can be overcome. Furthermore, these results also support findings (McCullagh M. C., Robinson C. 2009) indicating that most farmers are interested in increasing their use of HPDs. These results suggest that farmers may have a greater awareness of their work-related noise hazard exposures and interest in adopting HPD use, and that the mailed assortment of HPDs may be addressing their lack of familiarity with the variety of HPDs currently available and/or the low level of convenient access to HPDs on their farms.
Although studies examining the effectiveness of interventions on use of HPDs have been conducted with a variety of groups, including factory workers (Lusk et al. 1999; Lusk et al. 2003; Lusk et al. 2004), motorcyclists (McCombe, Binnington, Nash 1994), high school students (Knobloch and Broste 1998), coal miners (Stephenson et al. 2005), construction workers,(Kerr et al. 2007; Lusk et al. 1999) only one published study has examined effects of interventions on farmers. In a two-group non-randomized study of workers at 22 farms (Gates & Jones 2007), participants in the intervention group received a seminar and brochure together with a farm noise exposure assessment and supply and placement of HPDs, necessitating farm visits by skilled providers. After two months the intervention group had higher frequency of HPD use in comparison to the control group. Although results of this study were favorable, the study used a weaker non-randomized design, and the sustainability of the intervention was not addressed. This study represents, to our knowledge, the first random-controlled trial promoting HPD use among this high-risk population. The greater strength of the random-controlled trial design offers greater confidence in the effects of the intervention on the HPD use behavior of study participants, while the mailed sampler and Internet-based education program may be considered more sustainable by farmer groups and hearing conservation organizations.
The limitations of this study included use of self-report of the outcome variable, HPD use. Although self-report has been criticized as being subject to bias, studies comparing the validity of observed and self-reported HPD use (Griffin et al. 2009; Lusk, Ronis, Baer 1995) showed self-report and observations to be highly correlated (.89 and .92–.99, respectively). Further, the low reported use by farmers demonstrates a low social desirability effect. Also, other study design features serve to prevent participants’ desire to please investigators: the impersonal mode of data collection, emphasis on request for actual use, and preface stating understanding that it is not easy to always use. In addition, among farmers, self-report can be expected to be at least as valid due to the absence of demand characteristics (such as mandates, policies and regulations for use) found in industrial settings. For these reasons, self-report is deemed an appropriate measure of HPD use.
Study participants were largely farm managers, and participation among minority and hired farm workers was low. Further research is needed to examine the needs of these subgroups.
The effects of the mailed HPDs on use were higher at 6 months compared to 12 months. Because the provided supply of HPDs may have dwindled by the 12-month data collection point, it may be worthwhile to consider re-supplying participants every few months to continue to support their increased HPD use.
The study team used a variety of approaches to achieve an exceptionally high retention rate for study participants, with 92% of enrolled participants completing the 12-month study. This is particularly noteworthy, given the difficult-to-reach, highly autonomous, and geographically dispersed nature of the study population. Successes are primarily attributed to partnerships with farm organizations and attention to follow-up contacts.
The comparatively high increase in HPD use among participants receiving the mailed HPDs is of particular theoretical interest. Earlier studies (McCullagh, Ronis, Lusk 2010) suggested that situational influences on HPD use (e.g., access to hearing protectors) were predictive of farmers’ use of HPDs. The mailed sampler of HPDs was designed to address this predictor (McCullagh 2011). Study results confirm that when access to a variety of HPDs (i.e., roll-down plugs, pre-molded plugs, semi-aurals, and ear muffs) was present, then HPD use increased. This finding confirms the earlier predictors work, lending support to the Farmers’ Predictors of Hearing Protector Use Model (McCullagh, Ronis, Lusk 2010).
The comparative effectiveness of Internet-based informational interventions in this study is interesting. In metanalyses of published studies of Internet-based interventions to promote physical activity (Vandelanotte et al. 2007), self-management of chronic health conditions (Murray et al. 2005), and behavior change (Wantland et al. 2004), Internet-based interventions were more successful than comparison groups of participants receiving no intervention. The Internet has also been successful in one-group studies of smoking cessation (Bock et al. 2008), diet change (Norman et al. 2007), weight control (van Wier et al. 2006), and depression and anxiety (Christensen, Griffiths, Korten 2002).
Results from the study provide a model for future behavioral intervention research in a dispersed population. In addition, results of this study suggest new approaches for the prevention of NIHL, a prevalent, serious, preventable impairment among farm operators. Specifically, findings suggest that addressing barriers to access and convenience of use of HPDs may result in greater gains in HPD use among farm operators than the more common educational approaches.
The Internet has been used successfully to achieve changes in a variety of health behaviors, including physical activity, (Vandelanotte et al. 2007) self-management of chronic health conditions (Murray et al. 2005) and smoking cessation,(Bock et al. 2008; Brendryen and Kraft 2008) diet change(Bock et al. 2008; Brendryen and Kraft 2008) weight control,(van Wier et al. 2006) and depression and anxiety (Christensen, Griffiths, Korten 2002; Norman et al. 2007). Although there may be skeptics regarding the use of computers and the Internet among farmers, the Internet is well-suited to reaching members of this geographically dispersed, independent worker group. At least one study found that computers and the Internet were widely used by farmers (Voice of Agriculture 2009). Findings from this study suggest that this group may be receptive to online approaches to learning regarding hearing and other health topics.
Some previous studies aimed at increasing workers’ use of HPDs have employed tailoring of interventions, i.e., measuring individual workers’ beliefs and delivering individualized messages addressing these beliefs from a pre-designed library of messages. In contrast, this study used a targeted approach, i.e., the messages to all users are the same. This approach was selected for this study based on results of previous research showing similarities among farmers in regard to their knowledge, attitudes, and beliefs regarding noise, hearing, and use of hearing protection devices. The targeted approach was thus justified, and resulted in a program that was far more economical to develop, deliver, and maintain.
The findings of this study suggest that increasing the availability of hearing protectors may result in increased use of them. A challenge for the future is to engage the farming community to develop approaches to increase farmers’ awareness of available hearing protector technologies, and to make these devices more readily available in the farm work environment.
Acknowledgments
This research was supported by the National Institute for Deafness and Communication Disorders, National Institutes of Health (grant no. R01-DC010827) and the 3M Corporation, who supplied sample hearing protectors. The author thanks Michael Cohen, PhD for his work in data collection. Trial registration: Clinicaltrials.gov NCT01454895.
Acronyms and abbreviations
- NIHL
noise-induced hearing loss
- HPD
hearing protection device
Footnotes
Declaration of Interest. The results of this study Effects of an RCT of interventions on use of hearing protectors among farm operators were presented at the annual research conference of the National Hearing Conservation Association, New Orleans, LA, February 21, 2015.
References
- Alexander GL, McClure J, Calvi J. A randomized clinical trial evaluating online interventions to improve fruit and vegetable consumption. American Journal of Public Health. 2010;100(2):319–26. doi: 10.2105/AJPH.2008.154468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beckett WS, Chamberlain D, Hallman E, May J, Hwang SA, Gomez M, Eberly S, Cox C, Stark A. Hearing conservation for farmers: Source apportionment of occupational and environmental factors contributing to hearing loss. Journal of Occupational & Environmental Medicine. 2000;42:806–13. doi: 10.1097/00043764-200008000-00008. [DOI] [PubMed] [Google Scholar]
- Bock BC, Graham AL, Whiteley JA, Stoddard JL. A review of web-assisted tobacco interventions (WATIs) J Med Internet Res. 2008;10(5):e39. doi: 10.2196/jmir.989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brendryen H, Kraft P. Happy ending: A randomized controlled trial of a digital multi-media smoking cessation intervention. Addiction. 2008;103(3):478–84. doi: 10.1111/j.1360-0443.2007.02119.x. discussion 485–6. [DOI] [PubMed] [Google Scholar]
- Carpenter WS, Lee BC, Gunderson PD, Stueland DT. Assessment of personal protective equipment use among midwestern farmers. Am J Ind Med. 2002;42(3):236–47. doi: 10.1002/ajim.10103. [DOI] [PubMed] [Google Scholar]
- Choi SW, Peek-Asa C, Sprince NL, Rautiainen RH, Donham KJ, Flamme GA, Whitten PS, Zwerling C. Hearing loss as a risk factor for agricultural injuries. Am J Ind Med. 2005;48(4):293–301. doi: 10.1002/ajim.20214. [DOI] [PubMed] [Google Scholar]
- Christensen H, Griffiths KM, Korten A. Web-based cognitive behavior therapy: Analysis of site usage and changes in depression and anxiety scores. J Med Internet Res. 2002;4(1):e3. doi: 10.2196/jmir.4.1.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conway H, Simmons J, Talbert T. The purposes of occupational medical surveillance in US industry and related health findings. J Occup Med. 1993;35(7):670–86. doi: 10.1097/00043764-199307000-00009. [DOI] [PubMed] [Google Scholar]
- DHHS. Healthy people 2020. Washington DC: DHHS; 2010. [Google Scholar]
- Gates DM, Jones MS. A pilot study to prevent hearing loss in farmers. Public Health Nursing. 2007;24(6):547–553. doi: 10.1111/j.1525-1446.2007.00667.x. [DOI] [PubMed] [Google Scholar]
- Gomez MJ, Hwang SA, Sobotova L, Stark AD, May JJ. A comparison of self-reported hearing loss and audiometry in a cohort of New York farmers. Journal of Speech, Language, and Hearing Research. 2001;44(6):1201–1208. doi: 10.1044/1092-4388(2001/093). [DOI] [PubMed] [Google Scholar]
- Griffin SC, Neitzel R, Daniell WE, Seixas NS. Indicators of hearing protection use: Self-report and researcher observation. Journal of Occupational and Environmental Hygiene. 2009;(10):639–47. doi: 10.1080/15459620903139060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hetu R, Getty L, Quoc HT. Impact of occupational hearing loss on the lives of workers. Occupational Medicine. 1995;10(3):495–512. [PubMed] [Google Scholar]
- Hong OS, Chen SP, Conrad KM. Noise induced hearing loss among male airport workers in korea. Aaohn j. 1998;46(2):67–75. [PubMed] [Google Scholar]
- Jenkins PL, Stack SG, Earle-Richardson GB, Scofield SM, May JJ. Screening events to reduce farmers’ hazardous exposures. J Agric Saf Health. 2007;13:57–64. doi: 10.13031/2013.22312. [DOI] [PubMed] [Google Scholar]
- Joseph CLM, Peterson EL, Havstad S, Johnson CC, Hoerauf S, Stringer S, Gibson-Scipio W, Ownby DR, Elston-Lafata J, Pallonen U, et al. Web-based, tailored asthma management program for urban african-american high school students. American Journal of Respiratory Critical Care Medicine. 2007;175(9):888–895. doi: 10.1164/rccm.200608-1244OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr MJ, Savik K, Monsen KA, Lusk SL. Effectiveness of computer-based tailoring versus targeting to promote use of hearing protection. Can J Nurs Res. 2007;39(1):80–97. [PubMed] [Google Scholar]
- Knobloch MJ, Broste SK. A hearing conservation program for Wisconsin youth working in agriculture. J Sch Health. 1998;68(8):313–8. doi: 10.1111/j.1746-1561.1998.tb00591.x. [DOI] [PubMed] [Google Scholar]
- Lusk SL, Ronis DL, Hogan MM. Test of the health promotion model as a causal model of construction workers’ use of hearing protection. Nursing in Res and Health. 1997;20:183–94. doi: 10.1002/(sici)1098-240x(199706)20:3<183::aid-nur2>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- Lusk SL, Ronis DL, Baer LM. A comparison of multiple indicators–observations, supervisor report, and self-report as measures of workers’ hearing protection use. Eval Health Prof. 1995;18(1):51–63. doi: 10.1177/016327879501800104. [DOI] [PubMed] [Google Scholar]
- Lusk SL, Eakin BL, Kazanis AS, McCullagh MC. Effects of booster interventions on factory workers’ use of hearing protection. Nurs Res. 2004;53(1):53–8. doi: 10.1097/00006199-200401000-00008. [DOI] [PubMed] [Google Scholar]
- Lusk SL, Kerr MJ, Ronis DL, Eakin BL. Applying the health promotion model to development of a worksite intervention. Am J Health Promot. 1999;13(4):219–27. doi: 10.4278/0890-1171-13.4.219. [DOI] [PubMed] [Google Scholar]
- Lusk SL, Ronis DL, Kerr MJ, Atwood JR. Test of the health promotion model as a causal model of workers’ use of hearing protection. Nurs Res. 1994;43(3):151–7. [PubMed] [Google Scholar]
- Lusk SL, Ronis DL, Kazanis AS, Eakin BL, Hong OS, Raymond DM. Effectiveness of a tailored intervention to increase factory workers’ use of hearing protection. Nurs Res. 2003;52(5):289–95. doi: 10.1097/00006199-200309000-00003. [DOI] [PubMed] [Google Scholar]
- Lusk SL, Hong OS, Ronis DL, Eakin BL, Kerr MJ, Early MR. Effectiveness of an intervention to increase construction workers’ use of hearing protection. Hum Factors. 1999;41(3):487–94. doi: 10.1518/001872099779610969. [DOI] [PubMed] [Google Scholar]
- Lusk SL, Ronis DL, Baer LM. A comparison of multiple indicators–observations, supervisor report, and self-report as measures of workers’ hearing protection use. Eval Health Prof. 1995;18(1):51–63. doi: 10.1177/016327879501800104. [DOI] [PubMed] [Google Scholar]
- Marvel ME, Pratt DS, Marvel LH, Regan M, May JJ. Occupational hearing loss in New York dairy farmers. Am J Ind Med. 1991;20(4):517–31. doi: 10.1002/ajim.4700200407. [DOI] [PubMed] [Google Scholar]
- McBride DI, Firth HM, Herbison GP. Noise exposure and hearing loss in agriculture: A survey of farmers and farm workers in the southland region of new zealand. J Occup Environ Med. 2003;45(12):1281–8. doi: 10.1097/01.jom.0000100001.86223.20. [DOI] [PubMed] [Google Scholar]
- McCombe AW, Binnington J, Nash D. Two solutions to the problem of noise exposure for motorcyclists. Occup Med (Lond) 1994;44(5):239–42. doi: 10.1093/occmed/44.5.239. [DOI] [PubMed] [Google Scholar]
- McCullagh MC, Robinson C. Too late smart: Farmers’ adoption of self-protective behavior in response to exposure to hazardous noise. AAOHN Journal. 2009;57(3):99–105. doi: 10.3928/08910162-20090301-06. [DOI] [PubMed] [Google Scholar]
- McCullagh MC. Effects of a low intensity intervention to increase hearing protector use among noise-exposed workers. American Journal of Industrial medicine. 2011;54(3):210–215. doi: 10.1002/ajim.20884. [DOI] [PubMed] [Google Scholar]
- McCullagh MC, Ronis DL, Lusk SL. Predictors of use of hearing protection among a representative sample of farmers. Research in Nursing & Health. 2010;33(6):528–38. doi: 10.1002/nur.20410. [DOI] [PubMed] [Google Scholar]
- McCullagh MC, Lusk SL, Ronis DL. Factors influencing use of hearing protection among farmers: A test of the Pender health promotion model. Nurs Res. 2002;51(1):33–9. doi: 10.1097/00006199-200201000-00006. [DOI] [PubMed] [Google Scholar]
- Morata TC, D DE. Occupational hearing loss. Occupational Medicine. 1995;10(3):495–689. [PubMed] [Google Scholar]
- Morgan SE, Cole HP, Struttmann T, Piercy L. Stories or statistics? farmers’ attitudes toward messages in an agricultural safety campaign. J Agric Saf Health. 2002;8(2):225–39. doi: 10.13031/2013.8427. [DOI] [PubMed] [Google Scholar]
- Murphy D. Safety and health for production agriculture. St. Joseph, MI: American Society of Agricultural Engineers; 1992. [Google Scholar]
- Murray E, Burns J, See TS, Lai R, Nazareth I. Interactive health communication applications for people with chronic disease. Cochrane Database Syst Rev. 2005;(4):CD004274. doi: 10.1002/14651858.CD004274.pub4. (4) [DOI] [PubMed] [Google Scholar]
- National Agriculture, Forestry and Fishing Agenda [Internet] NIOSH; c2008. [cited 2009 05/10]. Available from: http://www.cdc.gov/niosh/nora/comment/agendas/AgForFish/pdfs/AgForFishDec2008.pdf. [Google Scholar]
- They’re your ears: Protect them [Internet] NIOSH; c2007a. [cited 2009 05/10]. Available from: http://www.cdc.gov/niosh/docs/2007-175/ [Google Scholar]
- Have you heard? Hearing loss caused by noise is preventable [Internet] NIOSH; c2007b. [cited 2009 05/10]. Available from: http://www.cdc.gov/niosh/docs/2007-176/ [Google Scholar]
- National Institute on Deafness and Other Communication Disorders Health Disparities Strategic Plan Fiscal Years 2004–2008 [Internet] c2009 [cited 2009 05/09]. Available from: http://www.nidcd.nih.gov/about/plans/strategic/FY2004-08-HDplan.htm.
- NIOSH. Preventing occupational hearing loss: A practical guide (publication 96–110) Washington, DC: NIOSH; 1996. [Google Scholar]
- Norman GJ, Zabinski MF, Adams MA, Rosenberg DE, Yaroch AL, Atienza AA. A review of eHealth interventions for physical activity and dietary behavior change. Am J Prev Med. 2007;33(4):336–45. doi: 10.1016/j.amepre.2007.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pender NJ, Murdaugh CL, Parsons MA. Health promotion in nursing practice. 6th. Upper Saddle River, NJ: Prentice Hall; 2010. [Google Scholar]
- Rabinowitz PM, Sircar KD, Tarabar S, Galusha D, Slade MD. Hearing loss in migrant agricultural workers. J Agromed. 2005;10(4):9–17. doi: 10.1300/J096v10n04_04. [DOI] [PubMed] [Google Scholar]
- Sataloff RT, Sataloff J. Occupational hearing loss. New York: Marcel Deckker; 1993. [Google Scholar]
- Savell JF, Toothman EH. Group mean hearing threshold changes in a noise-exposed industrial population using personal hearing protectors. Am Ind Hyg Assoc J. 1987;48(1):23–7. doi: 10.1080/15298668791384300. [DOI] [PubMed] [Google Scholar]
- Stephenson MT, Witte K, Vaught C, Quick BL, Booth-Butterfield S, Patel D, Zuckerman C. Using persuasive messages to encourage voluntary hearing protection among coal miners. J Safety Res. 2005;36(1):9–17. doi: 10.1016/j.jsr.2004.09.003. [DOI] [PubMed] [Google Scholar]
- Stewart M, Scherer J, Lehman ME. Perceived effects of high frequency hearing loss in a farming population. J Am Acad Audiol. 2003;14:100–8. doi: 10.3766/jaaa.14.2.5. [DOI] [PubMed] [Google Scholar]
- Strecher VJ, McClure J, Alexander G, Nair V, Konkel JM, Greene S, Collins L, Carlier C, Wiese C, Chakroborty B, et al. Web-based smoking cessation components and tailoring depth: Results of A randomized trial. American Journal of Preventive Medicine. 2008;34(5):373–381. doi: 10.1016/j.amepre.2007.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suter AH. The hearing conservation amendment: 25 years later. Noise Health. 2009;11(42):2–7. doi: 10.4103/1463-1741.45306. [DOI] [PubMed] [Google Scholar]
- Thelin JW, Joseph DJ, Davis WE, Baker DE, Hosokawa MC. High-frequency hearing loss in male farmers of Missouri. Public Health Rep. 1983;98(3):268–73. [PMC free article] [PubMed] [Google Scholar]
- Ubel PA, Smith DM, Zikmund-Fisher BJ, Derry HA, McClure J, Stark A, Wiese C, Greene S, Jakovic A, Fagerlin A. Testing whether decision aids introduce cognitive biases:Results of a randomized trial. Patient Education and Counseling. doi: 10.1016/j.pec.2009.10.021. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Department of Health and Human Services. Healthy people 2010. Washington, D.C: United States Department of Health and Human Services; 2000. [Google Scholar]
- van den Berg MH, Schoones JW, Vliet Vlieland TP. Internet-based physical activity interventions: A systematic review of the literature. J Med Internet Res. 2007;9(3):e26. doi: 10.2196/jmir.9.3.e26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Wier MF, Ariens GA, Dekkers JC, Hendriksen IJ, Pronk NP, Smid T, van Mechelen W. ALIFE@Work: A randomised controlled trial of a distance counselling lifestyle programme for weight control among an overweight working population [ISRCTN04265725] BMC Public Health. 2006;6:140. doi: 10.1186/1471-2458-6-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandelanotte C, Spathonis KM, Eakin EG, Owen N. Website-delivered physical activity interventions a review of the literature. Am J Prev Med. 2007;33(1):54–64. doi: 10.1016/j.amepre.2007.02.041. [DOI] [PubMed] [Google Scholar]
- Spirit of optimism buoys young farmers [Internet] American Farm Bureau; c2009. [cited 2009. Available from: http://www.fb.org/index.php?fuseaction=newsroom.newsfocus&year=2009&file=nr0305d.html. [Google Scholar]
- Wantland DJ, Portillo CJ, Holzemer WL, Slaughter R, McGhee EM. The effectiveness of web-based vs. non-web-based interventions: A meta-analysis of behavioral change outcomes. J Med Internet Res. 2004;6(4):e40. doi: 10.2196/jmir.6.4.e40. [DOI] [PMC free article] [PubMed] [Google Scholar]


