Abstract
Ultrasound visual feedback of the tongue is one treatment option for individuals with persisting speech sound errors. This study evaluated children's performance during acquisition and generalisation of American English rhotics using ultrasound feedback. Three children aged 10–13 with persisting speech sound errors associated with childhood apraxia of speech (CAS) were treated for 14 one-hour sessions. Two of the participants increased the accuracy of their rhotic production during practice trials within treatment sessions, but none demonstrated generalisation to untreated words. Lack of generalisation may be due to a failure to acquire the target with sufficient accuracy during treatment, or to co-existing linguistic weaknesses that are not addressed in a motor-based treatment. Results suggest a need to refine the intervention procedures for CAS and/or a need to identify appropriate candidates for intervention to optimise learning.
Phonetically accurate productions of American English rhotics (the /ɹ/ family of sounds) require complex articulatory control of the tongue. Rhotics are the most common residual speech sound errors (Shriberg, 2009) and can impact both intelligibility and naturalness of speech. Such errors are also frequently observed in school-age children with motor speech impairments including childhood apraxia of speech (CAS) (Preston, Brick, & Landi, 2013). Moreover, rhotic errors are commonly described as difficult to treat with traditional methods (McAllister Byun & Hitchcock, 2012). Ultrasound imaging of the tongue has been used to provide visual feedback on tongue positioning in speech treatment for children with /ɹ/ errors (e.g., Adler-Bock, Bernhardt, Gick, & Bacsfalvi, 2007; McAllister Byun, Hitchcock, & Swartz, 2014; Modha, Bernhardt, Church, & Bacsfalvi, 2008) including children with CAS (Preston et al., 2013). The present study evaluates acquisition and generalisation of rhotic production in the context of an intervention using ultrasound visual feedback in three children with CAS.
CAS is characterised by impaired production of speech sounds, difficulty transitioning between sounds and syllables, impaired prosody, and inconsistent token-to-token phonetic productions of words (ASHA, 2007). Thus, producing accurate speech sounds together with appropriate suprasegmental elements of speech should be a primary goal for CAS intervention. The core deficit in CAS is in planning and programming speech movements, resulting in increased reliance on external and internal feedback (Iuzzini-Seigel, Hogan, Guarino, & Green, 2015; Preston, Molfese et al., 2014; Terband, Maassen, Guenther, & Brumberg, 2009). Preston et al. (2013) hypothesised that enhancing feedback during speech production through the visual domain with ultrasound imaging may enhance error detection and thus allow children with CAS to establish and update the motor commands necessary for proper feed-forward control of speech.
To treat errors on articulatorily complex sounds such as /ɹ/ in children with CAS, approaches that focus on lingual control may be beneficial (Preston et al., 2013). By holding an ultrasound transducer beneath the chin to obtain real-time images of the tongue, feedback of tongue posture can be used to teach complex articulatory requirement for sounds including /ɹ/ (Adler-Bock et al., 2007; McAllister Byun et al., 2014; Preston et al., 2013; Preston, McCabe, et al., 2014). These images are used to cue the desired articulatory movements by showing the client which parts of the tongue should be raised, lowered, or moved forward or back. The focus of cueing with an ultrasound is typically on achieving a complex tongue shape that results in an acoustically acceptable production. Articulatory features for /ɹ/ that may be cued include elevation of the anterior tongue (tip or blade), lowering of the posterior tongue dorsum, retraction of the tongue root into the pharynx, and lateral bracing of the tongue (Adler-Bock et al., 2007; Bacsfalvi, 2010; McAllister Byun et al., 2014). Treating /ɹ/ may aid in improving speech intelligibility and naturalness.
Motor-based intervention for CAS
In the context of motor speech interventions, it is important to distinguish between performance during acquisition and learning. Performance during acquisition describes accuracy on a task during training, while learning requires generalisation to untrained stimuli as well as retention over time (Maas et al., 2008; Schmidt & Lee, 2011). For example, children may demonstrate increased performance during treatment when producing rhotics but they may fail to sufficiently integrate this information to achieve improved accuracy at later times or in new contexts. Thus, the ultimate goal of speech intervention is to facilitate motor learning (retention and generalisation to untrained contexts). However, some level of acquisition during training is a necessary precursor to learning; that is, generalisation of a skill cannot be observed until there is sufficient success in acquiring the skill (Hitchcock & McAllister Byun, 2015).
Within the framework of schema-based motor learning, a number of practice and feedback conditions may influence acquisition and learning (Maas et al., 2008). For example, feedback can take the form of knowledge of performance (KP, information about the movement) or knowledge of results (KR, information about accuracy). KP may facilitate increased accuracy during practice, particularly when the target movement is unknown (Newell, Carlton, & Antoniou, 1990). Ultrasound visual feedback of the tongue provides KP feedback and therefore is expected to enhance acquisition of target lingual movements. However, in non-speech motor tasks, too much KP may impede motor learning (Hodges & Franks, 2001). Thus, while ultrasound feedback may facilitate acquisition of sounds for individuals, it might not necessarily facilitate learning. Alternatively, learning and acquisition are enhanced when the focus of attention is external (on the effects of the movement) rather than internal (on the muscles completing the movement) (Freedman, Maas, Caligiuri, Wulf, & Robin, 2007; Wulf & McNevin, 2003). A visual display of the tongue such as that provided by ultrasound may provide sufficient external focus to enhance generalisation.
With respect to practice conditions, schema-based motor learning theory predicts that learning will be enhanced when movements are practised variably. Practice variability refers to practising the same generalised motor plan many different ways (cf. Adams & Page, 2000). In the present study, practice variability is incorporated by cueing the child to practise segmental targets (i.e., /ɹ/) in various phonetic contexts (cf. Ballard, Maas, & Robin, 2007) and under various prosodic conditions. Although the pairing of segmental and prosodic goals is embedded in some treatment approaches for CAS (e.g., Ballard et al., 2010; Strand & Debertine, 2000), the specific effect of prosodic cueing to achieve practice variability has not been tested in CAS.
Preston et al. (2013) demonstrated that using ultrasound with children with CAS could lead to improved speech sound accuracy in about 5–7 sessions for most treated sound sequences (including sequences with and without /ɹ/). All six participants demonstrated improved accuracy on at least two treated sound sequences, and five of the six participants demonstrated improvement on at least one sound sequence that included /ɹ/. In that study, each treatment session included practice both with and without the ultrasound feedback. In addition, target words and phrases were practised variably with different prosodic demands. For example, the phrase “A blue car” could be practised with varying intonation as a statement, question or command, or with varying rate (fast, slow). This allowed for cueing of tongue movements for the /aɹ/ in “car” but with variable practice. Thus, learning may have been facilitated through this practice variability, although no comparison was made between practice with and without prosodic variation. The present study sought to replicate the findings from Preston et al. (2013) while directly comparing targets treated with and without prosodic cues.
Preston, McCabe et al. (2014) used a single-subject design to compare sound targets treated with and without prosodic cues in eight individuals with residual speech sound errors who did not have CAS; that study found that prosodic cueing neither facilitated nor hindered generalisation and retention. However, given the prosodic impairments often observed in children with CAS, these children may specifically benefit from practice that requires the integration of both lingual control for segmental accuracy and the respiratory and phonatory demands of varying prosody; thus, the present study also explores whether children with speech sound errors associated with CAS can achieve greater generalisation of rhotics when prosodic variation is included with ultrasound treatment than when it is not.
Purpose and hypotheses
The goal of the present study was to extend previous findings which demonstrated improved speech sound accuracy in school-age children with CAS. We sought to evaluate whether ultrasound biofeedback of the tongue could (1) facilitate acquisition of /ɹ/ during treatment sessions, (2) lead to generalisation to untrained /ɹ/ words, and (3) be enhanced with cues for practicing words and phrases with varied prosody.
It was hypothesized that ultrasound training could lead to perceptually accurate productions of /ɹ/ during treatment for children with CAS1. Furthermore, it was hypothesized that generalisation to untrained words would be observed. Finally, it was hypothesized that prosodic cues, which enable variable practice, would facilitate generalisation to a greater extent than practice without prosodic cueing.
Methods
Participants
Three males aged 10–13 participated in this study. Participants were referred from local speech-language clinicians as part of a larger study evaluating ultrasound feedback for children with and without CAS. Results of treatment of children with residual articulation errors without CAS have been previously reported (Preston et al., 2014), thus the present results include only participants with CAS.
All three participants passed a hearing screening (20 dB at 1000, 2000, 4000 Hz bilaterally) and a vision screening (Snellen eye chart). Participants were from monolingual English-speaking homes and had persisting errors on /ɹ/ in both onset and coda positions (see Table 1).
Table 1.
Sample errors on words containing rhotics
| Task | Word | 094 | 097 | 103 |
|---|---|---|---|---|
| GFTA | ring | [wʊn] | [wɪŋ] | [wεn] |
| rabbit | ['wӕbɪn] | ['wӕbɪt] | ['wӕbɪt] | |
| carrot | ['kεwɪɁ] | ['kεwɪt] | ['kεwɪt] | |
| girl | [ɡn] | [ɡ] | [gol] | |
| zipper | ['zɪp] | ['zɪp] | ['zɪ'pu] | |
| scissors | ['sɪzʊz] | ['sɪzəs] | ['sɪ'zus] | |
| car | [kɔ] | [kɔ] | [k] | |
| finger | ['θɪŋɡʊ] | ['fɪŋɡʊ] | ['fɪŋɡuɫ] | |
| tree | [twi] | [ʃi] | [dʒi] | |
| brush | [bwʌs] | [bwʌʃ] | [bwʌs] | |
| frog | [fwɑk] | [fwɑɡ] | [fwɔk] | |
| green | [ɡin] | [ɡwin] | [ɡwɪn] | |
| Multisyllabic Word Repetition | practitioner | bæ'tɪstɪk | pæɁ'tɪʃən | pwæk'tɪ'ʃɪn |
Note: [] represents a derhoticized /ɹ/ (cf. Shriberg & Kent 2013).
Pre-Treatment Assessments
The assessment battery took place over 3 visits prior to treatment, during which time pre-treatment probes were administered to obtain baseline data (see below). All assessment tasks were administered and scored by a certified speech-language pathologist. Performance on standardised and researcher-developed measures is presented in Table 2.
Table 2.
Descriptive data for three participants with CAS
| Participant | |||
|---|---|---|---|
|
|
|||
| #094 | #097 | #103 | |
|
|
|||
| Age (years) | 13 | 10 | 10 |
| Intervention History | Age 2.5-present | Age 2.5-present | Age 5-present* |
| Speech Production Measures | |||
| GFTA-2 Raw score/Standard Score/Percentile | 20/<40/<1 | 20/43/<1 | 22/<40/<1 |
| GFTA-2 Percent Consonants Correct / Percent Rhotics Correct | 75 / 0 | 79 / 0 | 79 / 0 |
| Multisyllabic Word Repetition Percent Consonants Correct | 71 | 80 | 77 |
| Multisyllabic Word Repetition Percent Correct Lexical Stress | 55 | 80 | 60 |
| Inconsistency Task (range 1= always consistent, 8= always inconsistent) | 3.9 | 1.9 | 1.9 |
| Emphatic Stress Score (Max = 24) | 17 | 23 | 3 |
| Maximum Performance Task Apraxia Score | 2 | 2 | 2 |
| Maximum Performance Task Dysarthria Score | 1 | 0 | 1 |
| Oral Language Measures | |||
| PPVT-4 Standard Score | 19 | 116 | 87 |
| EVT-2 Standard Score | 14 | 104 | 89 |
| CELF-4-Recalling Sentences Scaled Score | 2 | 7 | 4 |
| CELF-4-Formulated Sentences Scaled Score | 4 | 7 | 6 |
| Phonological Processing | |||
| CTOPP-2 Elision Scaled Score | 1 | 6 | 8 |
| CTOPP-2 Blending Scaled Score | 4 | 6 | 4 |
| CTOPP-2 Phoneme Isolation Scaled Score | 4 | 4 | 3 |
| CTOPP-2 Phonological Awareness Standard Score | 56 | 71 | 69 |
| SAILS Number Correct (of 100) | 16 | 77 | 54 |
| SAILS ɹ Correct (of 20) | 13 | 15 | 9 |
| Nonword Repetition Percent Phonemes Correct (of 100) | 69 | 58 | 75 |
| Nonverbal | |||
| WASI-2 Block Design T-score | 25 | 37 | 37 |
| WASI-2 Matrix Reasoning T-score | 26 | 52 | 56 |
Note: Standard scores are normed with a mean of 100 and SD of 15. Scaled scores are normed with a mean of 10 and SD of 3. T-scores have a mean of 50 and SD of 10. Percentages are out of 100. See text for descriptions of tasks and scoring for non-standardised measures.
Due to an adoption, speech therapy history before age 5 is unknown for participant 103
Speech production measures
To confirm that participants had a speech sound disorder, the Goldman-Fristoe Test of Articulation-2 (GFTA-2, Goldman & Fristoe, 2000) was administered. Percent consonants correct (PCC) and percent rhotics correct (PRC) were calculated. Additional measures were used to evaluate speech production skills and to diagnose CAS. CAS diagnosis was reported by the referring clinicians, and was independently confirmed by two certified speech-language pathologists on the research team. The diagnosis of CAS was based on the ASHA (2007) criteria: token-to-token inconsistency, prosodic impairments, and difficulty transitioning between sounds/syllables. Specific tasks used to evaluate these criteria are outlined below. No specific threshold was used on any one task to make the diagnosis of CAS.
A Multisyllabic Word Repetition Task (Preston & Edwards, 2007) required children to repeat 20 challenging words of 3–6 syllables (e.g., “specificity”). Percent Consonants Correct (PCC) was computed. Additionally, a lexical stress score was assigned for each word: stress shift, excess/equal stress, or pauses within the word were scored as 0, and appropriate stress was scored 1.
A researcher-developed Inconsistency Task was administered. Participants repeated consecutive productions of phonetically challenging words which elicited a variety of lexical stress patterns (e.g., rectangle, computer). Eight pictures were copied on a page 8 times in a row and the participant was instructed, “Name each picture as quickly as you can. This one is a rectangle. Ready? Go!” For each word, phonetic transcription of the initial production was taken. Subsequent tokens that varied from the initial production were also phonetically transcribed, and the total number of variations of each word was recorded (cf. Marquardt, Jacks, & Davis, 2004; Preston & Koenig, 2011). Thus, if a child produced “rectangle” 5 different ways in 8 renditions of the word, the score would be 5 for that word. A variability score for each word was computed and averaged; 1 represented completely consistent productions and 8 represented inconsistent productions on every token of every word.
An Emphatic Stress Task based on Shriberg et al. (2010) was administered. Three different four-word sentences were recorded by a male speaker with contrastive stress on one word (Dan hates red shoes; Dan hates red shoes; Dan hates red shoes; Dan hates red shoes). This resulted in 12 items which were then randomized. Following two practice items with feedback, sentences were played to the participant who was asked to repeat the sentences exactly the way he heard them. Participants' productions were scored from audio recordings as follows: 0 = Poor prosody, very poor distinction between stressed/unstressed words; 1 = Subtle (mild or moderate) disturbance in prosody; perhaps some differentiation between stressed and unstressed, but not a good imitation of the sentence; 2 = Good imitation of the overall prosody of the sentence, clear distinction of the stressed word. Thus, the maximum score on was 24.
A motor speech assessment was administered that evaluated maximum duration of /ɑ/, /mɑmɑ/, /f, s, z/, maximum repetition rate for single syllables /pʌ/, /tʌ/, and /kʌ/, and rapid sequences of /pʌtʌkʌ/ (Thoonen, Maassen, Gabreëls, & Schreuder, 1999). Durations were obtained from acoustic waveforms in Praat (Boersma & Weeninck, 2013). Separate scores for dysarthria and CAS are obtained based on maximum phonation duration, maximum repetition rate, and sequencing. On the dysarthria scale 0 represents “not dysarthric”, 1 represents “undefined” and 2 represents “dysarthric.” On the CAS scale, 0 represents “not CAS”, 1 represents “undefined” and 2 represents “CAS.” All three participants scored 2 on the CAS scale (cf. Rvachew, Ohberg & Savage, 2006).
Oral Language
Measures of oral language were administered for descriptive purposes. The Peabody Picture Vocabulary Test-4 (Dunn & Dunn, 2007) was used to assess receptive vocabulary. The Expressive Vocabulary Test-2 (Williams, 2007) assessed expressive vocabulary. Two subtests of the Clinical Evaluation of Language Fundamentals-4 (Semel, Wiig, & Secord, 2003) were administered: Recalling Sentences, and Formulated Sentences.
Phonological processing
Phonological processing skills were also evaluated. From the Comprehensive Test of Phonological Processing-2 (Wagner, Torgesen, Rashotte, & Pearson, 2013), Phonological Awareness subtests included Elision, Blending Words, and Phoneme Isolation.
In addition, Speech Assessment and Interactive Learning System (SAILS) (Rvachew, 1994) was administered to evaluate participants' ability to judge correct and incorrect productions of phonemes. Twenty tokens each of /ɹ, s, θ, f, ʃ/ were presented for a total of 100 trials; for each phoneme category, the highest level of difficulty available in the software was presented.
To assess phonological working memory, a nonword repetition task by Dollaghan and Campbell (1998) was administered. Responses were phonetically transcribed and Percent Phonemes Correct (PPC) was computed from the 96 phonemes.
Non-verbal ability
The Block Design and Matrix Reasoning subtests of Wechsler Abbreviated Scales of Intelligence-2 (Wechsler, 2011) were administered to assess nonverbal visual spatial perception and reasoning.
Descriptive data from assessments
Based on this testing, participant 94 had weaknesses in receptive and expressive language, phonological processing, and visual spatial reasoning. He was externally diagnosed with attention deficit disorder and learning disability. He had both CAS and flaccid dysarthria (low tone, poor breath support, low speaking volume, monopitch, slightly weakened articulation of pressure consonants). Participant 97 demonstrated CAS with significant impairments in transitioning between sounds and syllables; his expressive language skills were low average and he had poor phonological processing. Participant 103 had significantly impaired prosody, frequent vowel distortions, weak phonological processing, and mild expressive language delays.
Probes for assessing baseline performance and treatment progress
To confirm that there were errors on /ɹ/ and to aid in identifying intervention targets, word-level probes were developed: word-initial singleton (e.g. “red”, 25 items), word-initial cluster (e.g., “brown”, 50 items) and word-final (e.g., “star”, 25 items). Participants read the probe words which were scored 0 (incorrect) and 1 (correct) for the perceived accuracy of the rhotic sound. Probes were administered before treatment and again at the beginning of intervention sessions to assess short-term retention and generalization of the target behaviours.
Design
A multiple-baselines-across-behaviours design was utilized with two behaviours (syllable positions) addressed per participant. Prior studies have shown that onset /ɹ/ and coda /ɹ/ emerge independently in typical development (McGowan, Nittrouer, & Manning, 2004) and during treatment (McAllister Byun & Hitchcock, 2012; McAllister Byun et al., 2014; Preston, McCabe, et al., 2014), highlighting the need to treat these contexts independently. Each participant was evaluated during three baseline visits prior to the onset of therapy. Based on the assessment tasks, two behaviors were selected for intervention. Treatment consisted of two phases. During Phase I of treatment (sessions 1 – 7), one syllable position was addressed in therapy (/ɹ/ in onset or coda position) and was assigned to either Prosodic Cueing or No Prosody conditions. The other treatment target was monitored but was untreated until Phase II (sessions 8 – 14). This second target sequence was then addressed in Phase II under the remaining condition. The order for the first treatment target (/ɹ/ in onset or coda position) and treatment condition (Prosodic Cueing nor No Prosody) was randomly determined for the first participant and was counterbalanced with the subsequent participants to ensure that condition order was not the same. Between Phases, midpoint probes were administered over approximately one week in which no treatment occurred. Finally, post-therapy probes were administered (over approximately one week) following completion of Phase II. To monitor retention, probes were repeated two months after the post-therapy probes.
Intervention Procedures
All three participants were treated by the same ASHA certified speech-language pathologist familiar with ultrasound treatment procedures. Intervention procedures were identical to those reported in Preston, McCabe et al. (2014); however, in that study, none of the participants had CAS. All participants had errors on /ɹ/ in all word positions.Within each Phase of treatment, two phonetic contexts were selected for practice. For /ɹ/ singleton targets, treatment addressed syllables and words with /ɹ/ plus two vowels (e.g., training syllables and words with /ɹe/ and /ɹo/). For /ɹ/ cluster targets, treatment addressed syllables and words with /ɹ/ following two consonants (e.g., /θɹ/ and /bɹ/).2 For /ɹ/ coda targets, participants practised syllables and words with two different preceding vowels (e.g., /ɑɹ/ and /ɪɹ/).
Session structure
Each session was divided into four 13-minute time periods. Periods A and C included practice with the ultrasound; Periods B and D did not. A timer was used to monitor these time requirements and to ensure fidelity. This time structure was followed regardless of whether in the Elicitation or the Structured Practice phase of the session (see below). The time criterion for ultrasound feedback was independent of the performance criterion for advancing to more challenging stimuli.
All sessions began with an Elicitation (pre-practice) phase designed to teach a perceptually acceptable production for rhotics by providing facilitative cues. During Elicitation, any clinical strategy was allowable to encourage correct production, including modeling, facilitative contexts (e.g., [dɹ:], [ɹæ]), shaping (e.g., [l] → [ɹ], [ɑ] → [ɹ]) and phonetic cues (e.g., “lift the front of your tongue off the floor of your mouth”, “pull your whole tongue back in your throat”). Once the participant achieved 6 correct productions of /ɹ/ in each of two phonetic contexts (e.g., 6 correct /ɑɹ/ and 6 correct /ɪɹ/) the session switched to Structured Practice. If the child did not meet the criteria to move to Structured Practice, then the entire session would be spent in Elicitation.
Structured Practice included blocked practice of 6 consecutive trials of the same target with gradual increases in complexity of the utterance if the child was successful. The participant began with 6 trials at the syllable level (e.g., /ɑɹ/). Structured Practice could progress to monosyllabic words (words with at least one additional consonant), multisyllabic words (which contained the monosyllabic words), set phrases, and phrase generation (child makes up a sentence with the target word). If the child achieved at least 5 of 6 correct productions at any level, he advanced to the next level for the next block of 6 trials. Chains were developed that progressed from syllables through phrases, such as “are”, “tar”, “guitar”, “loud guitar”, and “____ guitar”. Failure to meet the 5 of 6 criterion at any level meant the child returned to practise at the syllable level of another chain, such as “ear”, “tear”, “frontier”, “the wild frontier”, and “___ frontier”. The goal of this chaining procedure was to gradually increase complexity of the utterances.
As the complexity of the utterance increased, frequency of verbal feedback decreased. Knowledge of Results (KR) verbal feedback required that the clinician indicate the acoustic acceptability of the production (e.g., “that sounded clear” or “not quite”). Knowledge of Performance (KP) verbal feedback included verbal feedback by the clinician about the articulators (e.g., “your tongue tip was too low”, “keep the back of your tongue low”, “you didn't move your tongue into the back of your throat”). During Periods A & C, verbal KP feedback by the clinician referenced the visual display and drew the client's attention to elements of the desired tongue position; during trials without ultrasound, verbal KP feedback was provided on lip/jaw aperture and tongue position based on the clinician's best estimate (as in traditional speech therapy). KP and KR were provided on 5 of 6 trials at the syllable level. At the monosyllabic word level, feedback was provided on 5 of 6 trials (2 KR only and 3 with both KP and KR). At the multisyllabic word level, feedback was provided on 4 of 6 trials (2 KR only and 2 with both KP and KR). At the set phrase and phrase generation levels, feedback was provided on 3 of 6 trials (1 with KR only and 2 with KP and KR).
Prosodic Cues
Prosodic cueing was included in one randomly-selected phase for each participant. Prosodic Cueing involved pairing the target utterance with one of three punctuation cues (question mark, exclamation point, and period) during Structured Practice as the participant produced monosyllabic words, multisyllabic words, set phrases, and generated phrases (therefore, Prosodic Cueing did not occur during Elicitation in which the target sequences were being established). Prosodic Cues simply required the participant to practise the target utterance 3 times with one punctuation cue and 3 times with a different cue (e.g., “Race! Race! Race! Race? Race? Race?”). A model was provided with the punctuation cue but no feedback was given on prosody, as all KP and KR feedback was directed toward accuracy of the rhotic. Table 3 shows the treatment targets and assigned conditions for Phase I and Phase II.
Table 3.
Intervention targets, treatment condition, and change in accuracy
| Participant | Phase | Treatment Target | Condition | Pretreatment % Accuracy | Post-treatment % Accuracy |
|---|---|---|---|---|---|
| 94 | I | Initial /ɹ/ | (Prosodic Cues) | 3 | 4 |
| II | Final /ɹ/ | (No Prosodic Cues) | 0 | 2 | |
| 97 | I | Final /ɹ/ | (No Prosodic Cues) | 0 | 7 |
| II | Initial /ɹ/ clusters | Prosodic Cues | 9 | 17 | |
| 103 | I | Initial /ɹ/ | No Prosodic Cues | 2 | 1 |
| II | Final /ɹ/ | (Prosodic Cues) | 0 | 0 |
Note: Prosodic cueing was implemented only in Structured Practice, not in Elicitation. Parentheses indicate that the participant did not advance past Elicitation to Structured practice and therefore there was no opportunity to implement the intended prosodic cueing condition. Accuracy was based on average of two independent listeners' scores on 3–4 generalisation probes immediately before and after the treatment phase.
Use of ultrasound in treatment
A SeeMore PI 7.5 MHz ultrasound probe was used to provide feedback (in Periods A and C). For all participants, the ultrasound probe was initially held by the clinician at the beginning of the first session but over the course of the session the probe was given to the client with instructions on positioning. For participant 94, who had difficulty with fine motor control, the probe was eventually stabilized (clamped on a microphone stand) and he leaned forward to rest his chin on the ultrasound probe. Cueing with the ultrasound focused on several elements of tongue positioning such as posterior movement of the tongue into the pharynx to form a pharyngeal constriction, elevation of tongue tip, blade, or mid-dorsum to achieve an oral constriction, lowering the posterior tongue dorsum to avoid a constriction at the velum, or elevation of the lateral margins of the tongue to achieve lateral bracing (cf. Bacsfalvi, 2010). Both “bunched” and “retroflex” tongue shapes were cued at various times to try to establish a tongue shape that resulted in an acoustically acceptable production of /ɹ/ (cf. McAllister Byun et al., 2014). Visual targets were traced on a transparent overlay placed over the screen; these provided marks for the child to try to “hit” to encourage raising, lowering, or retracting of the tongue. Both sagittal and coronal views were used at the clinician's discretion, although the majority of training involved a sagittal view. Once a tongue shape was identified that resulted in an acoustically acceptable production, the tongue shape was traced on the screen offering a template for the child to match on subsequent trials. Variation in tongue shape in different phonetic contexts was allowed, as the goal was to achieve a perceptually acceptable production. Ultrasound visual feedback was presented in real time, although occasionally static images were used to describe desirable/undesirable tongue shapes.
To illustrate tongue shapes, Figure 1 displays (unstabilised) sagittal images of distorted vocalic /ɹ/ productions from all three participants, along with correct productions produced during treatment for participants 97 (in “broom”) and 103 (in “rain”). As can be seen in the images, the distortions were primarily characterized by a posterior peak of the tongue dorsum, whereas a more anterior peak is observed in the correct productions.
Figure 1.
Example tongue shapes for distorted and correct productions of rhotics
Note: All three distorted productions came from vocalic /ɹ/ productions whereas the correct productions occurred in onsets (“broom” for participant 97 and “rain” for 103).
Reliability and fidelity
Generalisation probes were scored via recordings by the treating clinician and a second listener who was blind to treatment targets. All probes differed by less than 20% between the two listeners, suggesting acceptable levels of agreement. The two listeners disagreed on 3% of the tokens. Data presented for the generalisation probes are an average of the two listeners.
Fidelity monitoring of the sessions involved ensuring adherence to the feedback structure. Each block of 6 trials in Structured Practice had a specified KP and KR feedback schedule as described above. A research assistant reviewed recordings of the Structured Practice for two sessions for each participant. The intended verbal feedback was provided on 96% of trials (cf. Maas, Butalla, & Farinella, 2012). The research assistant also compared her judgments of accuracy with the clinician's KR feedback to ensure the clinician was reinforcing accurate productions and diminishing errors. Reliability of the accuracy of KR feedback between the treating clinician and the research assistant's judgments was 86%.
Data analysis
Graphical displays of the data were used to evaluate trends, and mean changes coinciding with intervention were computed to evaluate treatment effects (Beeson & Robey, 2006; Kratochwill et al., 2010; Tate et al., 2008).3 When comparing pre- and post-treatment probe scores, improvements of 20% or greater were considered clinically important (cf. Preston et al., 2014).
Results
Within-session performance
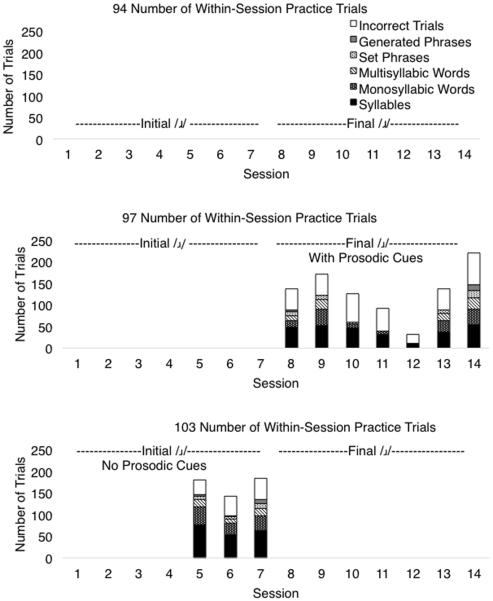
Sessions progressed from Elicitation to Structured Practice in syllables, monosyllabic words, multisyllabic words, set phrases, and generated phrases. Figure 2 displays the number of correct trials and the total attempted trials within each session for the given participant. For sessions in which the participant advanced from Elicitation to Structured Practice, the average number of trials per session was 142 (SD 53). Because advancing to the next level was dependent upon the clinician's judgment of success in the preceding level, the number of correct trials is based on the treating clinician's judgment. It can be seen that participant 94 did not achieve any successful practice trials even at the syllable level (i.e., he never progressed past Elicitation) in either phase. Participant 97 did not achieve any correct productions in Phase I when practising final /ɹ/, but in Phase II when practising /ɹ/ clusters he achieved at least 50 correct trials per session in 6 of 7 sessions. Participant 103 advanced to Structured Practice only in 3 sessions during Phase I when targeting initial /ɹ/ singletons but he did not advance past Elicitation in Phase II when targeting final /ɹ/. Thus, some level of accuracy was observed with the ultrasound treatment programme but it was not successful in facilitating correct productions for all participants nor with all treatment targets.
Figure 2.
Performance during acquisition by participant
Note: Participant 94 did not achieve criteria to advance past Elicitation into Structured Practice so no correct trials were observed. Participant 97 advanced to Structured Practice during the final 7 sessions, and Participant 103 advanced to Structured Practice only for sessions 5, 6, and 7. Top of bar represents total number of Structured Practice trials for the session.
Generalisation
Figure 3 displays performance on /ɹ/ generalisation probes used for progress monitoring, and Table 3 presents average probe scores from before and after each treatment phase. Improvements across all phases were under 10%, suggesting minimal generalisation. If we consider improvement of approximately 20% on the generalisation probe to reflect clinically significant treatment effect (cf. Preston et al., 2014), no clinically significant generalisation was observed for either of the two treated targets for any of the three participants.
Figure 3.
Performance on generalisation probes by participant
Note: Shaded boxes represent sessions in which treatment occurred. Probe data were collected at the beginning of each session; therefore, probes at the first session of the treatment phase are considered pre-treatment datapoints. B=Baseline pre-treatment, M= Midpoint between Phase I and Phase II, P=Post-treatment, 2M=2 month follow-up.
Prosodic Cues
Prosodic cueing was contingent upon the participants practicing word and phrase level items. However, of the six total treatment phases, only two involved sessions that reached practice at the word or phases level: Phase II for participant 97 and Phase I for participant 103. Thus, there were no data for within-subject comparison of generalisation for conditions with and without prosodic cueing.
Discussion
This study used an intervention approach that has been shown to be effective in prior studies addressing /ɹ/ production in individuals with residual speech sound errors, CAS, and acquired apraxia (Preston et al., 2013; Preston & Leaman, 2014; Preston, McCabe et al., 2014). In the present study, two children (participants 97 and 103) showed context-specific acquisition within treatment sessions. However, none showed significant generalisation in 14 treatment sessions or during post-treatment probes. Thus, the learning effects observed in prior studies were not replicated with these three participants.
Prosodic cueing, which was implemented only when practising words and phrases, was only introduced in Phase II for participant 97. Therefore, there is not enough information to determine if prosodic cueing facilitated motor learning. For participant 97, limited generalisation to untrained words was observed. Further research on the role of prosodic variation to facilitate generalisation in CAS is needed.
Participant 94 clearly failed to respond to the intervention. He never passed the Elicitation phase of treatment despite 14 sessions. This participant had symptoms not only of CAS but also a range of concomitant communication and cognitive difficulties. His attention during treatment varied and he required frequent breaks. It is possible that he was not able to sufficiently integrate the visual feedback to modify his motor plan when attempting production of rhotics. A higher treatment dose or alternate treatment strategies might be necessary to facilitate acquisition and learning.
For the two participants who achieved some accurate productions during Structured Practice (participants 97 and 103), generalisation to untrained words was not observed. This may indicate that there was insufficient acquisition of the target and that more successful attempts may be required before generalisation occurs. A limited ability to acquire, retain, and generalise motor plans may be at the core of CAS. Difficulty in generalisation has been observed in other CAS treatment studies but the threshold for generalisation is as yet unknown (e.g., Ballard et al., 2010; Maas et al., 2012). A greater dosage of treatment may be necessary to facilitate the transition from acquisition to learning (cf. Maas, Gildersleeve-Neumann, Jakielski, & Stoeckel, 2014). Alternatively, it may be the case that the extensive visual (and verbal) KP feedback aided acquisition for these two participants but inhibited generalisation (cf. Hodges & Franks, 2001). That is, the participants may have become dependent upon the KP feedback and may not have developed a stable internal model for production.
Rhotics may be particularly challenging for individuals with complex motor speech impairments due to the gestural complexity of the target, which requires simultaneous coordinated movements of anterior and posterior aspects of the tongue (Gick et al., 2007). These complex movements may be easier to achieve in some contexts than in others. For example, participants 97 and 103 were able to achieve perceptually correct rhotics when practising onsets but not when practising codas. Differential response in onset and coda positions has been previously reported (McAllister Byun et al., 2014; Preston & Leaman, 2014); this may be due to the fact that tongue configurations used by typical speakers of English sometimes vary between syllable/word positions (Delattre & Freeman, 1968; Guenther et al., 1999). Additionally, the timing and magnitude requirements for the anterior and posterior constrictions of the tongue during production of rhotics may differ in onset and coda positions (Campbell, Gick, Wilson, & Vatikiotis-Bateson, 2010). The two participants in this study who showed some acquisition did so only in onset position, suggesting that the inherent timing and/or magnitude of movements for onsets were easier for them.
Generalisation may have been limited in this study because these individuals were not appropriate candidates for this intervention. The three participants were relatively complex cases with a variety of comorbid impairments. As has been reported in adults with acquired apraxia of speech, some individuals may be less capable of integrating visual feedback to modify feed-forward control of movements in order to increase accuracy (Ballard & Robin, 2007). Moreover, several prior studies have shown that not all individuals generalise to untrained items when rhotic sounds are treated with ultrasound feedback (McAllister Byun et al., 2014; Preston et al., 2013; Preston, McCabe et al., 2014). Thus, future studies should explore pre-treatment factors that predict responders and non-responders to this type of intervention.
In particular, the role of phonological processing warrants consideration. Motor impairments notwithstanding, all participants in this study demonstrated weaknesses on multiple phonological processing tasks (phonological awareness tasks on the CTOPP, perception of rhotics and other sounds on SAILS, nonword repetition tasks). This observation is in line with prior studies that have reported phonological processing differences in children with CAS (Froud & Khamis-Dakwar, 2012; Lewis et al., 2004). The treatment programme implemented here included no explicit attempts to address perception of correct or incorrect productions. Therefore, the strong emphasis on articulatory goals in this visual feedback intervention may lead to insufficient focus on training the proper acoustic target for rhotics. It is possible that a focus on the acoustic target would elicit a more external focus of attention, which might have facilitated acquisition and learning (cf. Lisman & Sadagopan, 2013). Prior studies have shown that including a perceptual training component in speech sound therapy may facilitate acquisition of sounds, including sounds that are not stimulable (Rvachew, Nowak, & Cloutier, 2004; Rvachew, Rafaat, & Martin, 1999). Some studies have also included metaphonological training and have observed increased speech sound accuracy (McNeill et al., 2009). Future studies should explore combined effects of phonological processing training and ultrasound visual feedback for children with CAS, particularly when pre-treatment production accuracy is near 0%. Additionally, despite the success of ultrasound visual feedback training for some children with CAS (Preston et al., 2013), ultrasound visual feedback is not a “one size fits all” approach, and further consideration should be given to other linguistic and motoric strategies to facilitate improved speech sound accuracy in individuals with concomitant impairments.
In sum, the limited acquisition and generalisation observed in the present study indicates that ultrasound biofeedback may not facilitate rapid acquisition or generalisation for rhotics in some children with CAS. It will be important to continue to develop intervention protocols such that even individuals with complex motor speech impairments and comorbid weaknesses would benefit. It may be necessary to identify alternative strategies to facilitate learning of complex speech targets such as /ɹ/.
Acknowledgments
The authors declare that funding was provided by NIH grant R03DC012152.
Footnotes
Declaration of Interest The authors have no other relevant financial or nonfinancial interests to disclose.
Although some studies also evaluate tongue shape changes over the course of treatment, the aim of this study was to evaluate ecologically valid outcomes related to listeners' judgments of correct and incorrect /ɹ/.
Multiple vowel contexts were used with the cluster targets to ensure a sufficiently large number of items that could be trained and extended into longer words and phrases (see Session Structure below).
Inferential statistics are not reported as this study was not designed to meet the assumptions of such analyses (cf. Kratochwill et al., 2010)
References
- Adams SG, Page AD. Effects of selected practice and feedback variables on speech motor learning. Journal of Medical Speech-Language Pathology. 2000;8(4):215–220. [Google Scholar]
- Adler-Bock M, Bernhardt B, Gick B, Bacsfalvi P. The use of ultrasound in remediation of North American English /ɹ/ in 2 adolescents. American Journal of Speech-Language Pathology. 2007;16(2):128–139. doi: 10.1044/1058-0360(2007/017). [DOI] [PubMed] [Google Scholar]
- American Speech-Language-Hearing Association Childhood apraxia of speech. 2007 [Technical Report]. Available from www.asha.org/policy.
- Bacsfalvi P. Attaining the lingual components of /ɹ/ with ultrasound for three adolescents with cochlear implants. Journal of Speech-Language Pathology and Audiology. 2010;34(3):206–217. [Google Scholar]
- Ballard KJ, Maas E, Robin DA. Treating control of voicing in apraxia of speech with variable practice. Aphasiology. 2007;21:1195–1217. [Google Scholar]
- Ballard KJ, Robin DA. Influence of continual biofeedback on jaw pursuit-tracking in healthy adults and in adults with apraxia plus aphasia. Journal of Motor Behavior. 2007;39(1):19–28. doi: 10.3200/JMBR.39.1.19-28. [DOI] [PubMed] [Google Scholar]
- Ballard KJ, Robin DA, McCabe P, McDonald J. A treatment for dysprosody in childhood apraxia of speech. Journal of Speech, Language, and Hearing Research. 2010;53(5):1227–1245. doi: 10.1044/1092-4388(2010/09-0130). [DOI] [PubMed] [Google Scholar]
- Beeson PM, Robey RR. Evaluating single-subject treatment research: Lessons learned from the aphasia literature. Neuropsychology review. 2006;16(4):161–169. doi: 10.1007/s11065-006-9013-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernhardt B, Gick B, Bacsfalvi P, Ashdown J. Speech habilitation of hard of hearing adolescents using electropalatography and ultrasound as evaluated by trained listeners. Clinical Linguistics & Phonetics. 2003;17(3):199–216. doi: 10.1080/0269920031000071451. [DOI] [PubMed] [Google Scholar]
- Boersma P, Weeninck D. Praat v 5.3.49. 2013 Available from www.praat.org.
- Campbell F, Gick B, Wilson I, Vatikiotis-Bateson E. Spatial and temporal properties of gestures in North American English /ɹ/ Language and Speech. 2010;53(1):49–69. doi: 10.1177/0023830909351209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delattre P, Freeman DC. A dialect study of American r's by x-ray motion picture. Linguistics. 1968;6(44):29–68. [Google Scholar]
- Dollaghan CA, Campbell TF. Nonword repetition and child language impairment. Journal of Speech, Language, and Hearing Research. 1998;41:1136–1146. doi: 10.1044/jslhr.4105.1136. [DOI] [PubMed] [Google Scholar]
- Dunn LM, Dunn DM. Peabody picture vocabulary test. 4 ed. Pearson; Minneapolis, MN: 2007. [Google Scholar]
- Freedman SE, Maas E, Caligiuri MP, Wulf G, Robin DA. Internal versus external: Oral-motor performance as a function of attentional focus. Journal of Speech, Language, and Hearing Research. 2007;50(1):131–136. doi: 10.1044/1092-4388(2007/011). [DOI] [PubMed] [Google Scholar]
- Froud K, Khamis-Dakwar R. Mismatch negativity responses in children with a diagnosis of childhood apraxia of speech (CAS) American Journal of Speech-Language Pathology. 2012;21(4):302–312. doi: 10.1044/1058-0360(2012/11-0003). [DOI] [PubMed] [Google Scholar]
- Gick B, Bacsfalvi P, Bernhardt BM, Oh S, Stolar S, Wilson I. A motor differentiation model for liquid substitutions in children's speech. Proceedings of Meetings on Acoustics. 2007;1(1):060003. [Google Scholar]
- Goldman R, Fristoe M. Goldman Fristoe test of articulation. 2 ed. AGS; Circle Pines, MN: 2000. [Google Scholar]
- Guenther FH, Espy-Wilson CY, Boyce SE, Matthies ML, Zandipour M, Perkell JS. Articulatory tradeoffs reduce acoustic variability during American English /r/ production. The Journal of the Acoustical Society of America. 1999;105(5):2854–2865. doi: 10.1121/1.426900. [DOI] [PubMed] [Google Scholar]
- Hitchcock ER, McAllister Byun T. Enhancing generalisation in biofeedback intervention using the challenge point framework: A case study. Clinical Linguistics & Phonetics. 2015;29(1):59–75. doi: 10.3109/02699206.2014.956232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodges NJ, Franks IM. Learning a coordination skill: Interactive effects of instruction and feedback. Research Quarterly for Exercise and Sport. 2001;72(2):132–142. doi: 10.1080/02701367.2001.10608943. [DOI] [PubMed] [Google Scholar]
- Iuzzini-Seigel J, Hogan TP, Guarino AJ, Green JR. Reliance on auditory feedback in children with Childhood Apraxia of Speech. Journal of Communication Disorders. doi: 10.1016/j.jcomdis.2015.01.002. in press. [DOI] [PubMed] [Google Scholar]
- Kratochwill TR, Hitchcock J, Horner RH, Levin JR, Odom SL, Rindskopf DM, Shadish WR. Single-case designs technical documentation. 2010 Retrieved from What Works Clearinghouse website: http://ies.ed.gov/ncee/wwc/pdf/wwc_scd.pdf.
- Lewis BA, Freebairn LA, Hansen AJ, Iyengar SK, Taylor HG. School-age follow-up of children with childhood apraxia of speech. Language, Speech, and Hearing Services in Schools. 2004;35:122–140. doi: 10.1044/0161-1461(2004/014). [DOI] [PubMed] [Google Scholar]
- Lisman AL, Sadagopan N. Focus of attention and speech motor performance. Journal of Communication Disorders. 2013;46:281–293. doi: 10.1016/j.jcomdis.2013.02.002. [DOI] [PubMed] [Google Scholar]
- Maas E, Butalla CE, Farinella KA. Feedback frequency in treatment for childhood apraxia of speech. American Journal of Speech-Language Pathology. 2012;21:239–257. doi: 10.1044/1058-0360(2012/11-0119). [DOI] [PubMed] [Google Scholar]
- Maas E, Farinella KA. Random versus blocked practise in treatment for childhood apraxia of speech. Journal of Speech, Language, and Hearing Research. 2012;55:561–578. doi: 10.1044/1092-4388(2011/11-0120). [DOI] [PubMed] [Google Scholar]
- Maas E, Gildersleeve-Neumann CE, Jakielski KJ, Stoeckel R. Motor-based intervention protocols in treatment of childhood apraxia of speech (CAS) Current Developmental Disorders Reports. 2014;1:197–206. doi: 10.1007/s40474-014-0016-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maas E, Robin DA, Austermann Hula SN, Freedman SE, Wulf G, Ballard KJ, Schmidt RA. Principles of motor learning in treatment of motor speech disorders. American Journal of Speech-Language Pathology. 2008;17(3):277–298. doi: 10.1044/1058-0360(2008/025). [DOI] [PubMed] [Google Scholar]
- Marquardt TP, Jacks A, Davis BL. Token-to-token variability in developmental apraxia of speech: Three longitudinal case studies. Clinical Linguistics & Phonetics. 2004;18(2):127–144. doi: 10.1080/02699200310001615050. [DOI] [PubMed] [Google Scholar]
- McAllister Byun T, Hitchcock ER. Investigating the use of traditional and spectral biofeedback approaches to intervention for /r/ misarticulation. American Journal of Speech-Language Pathology. 2012;21(3):207–221. doi: 10.1044/1058-0360(2012/11-0083). [DOI] [PubMed] [Google Scholar]
- McAllister Byun T, Hitchcock ER, Swartz MT. Retroflex versus bunched in treatment for rhotic misarticulation: Evidence from ultrasound biofeedback intervention. Journal of Speech, Language, and Hearing Research. 2014;57(6):2116–2130. doi: 10.1044/2014_JSLHR-S-14-0034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGowan RS, Nittrouer S, Manning CJ. Development of /r/ in young, Midwestern, American children. Journal of the Acoustical Society of America. 2004;115(2):871–884. doi: 10.1121/1.1642624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeill BC, Gillon GT, Dodd B. Effectiveness of an integrated phonological awareness approach for children with childhood apraxia of speech (CAS) Child Language Teaching and Therapy. 2009a;25(3):341–366. [Google Scholar]
- Modha G, Bernhardt B, Church R, Bacsfalvi P. Ultrasound in treatment of /r/: A case study. International Journal of Language & Communication Disorders, 43 (3) 2008;43(3):323–329. doi: 10.1080/13682820701449943. [DOI] [PubMed] [Google Scholar]
- Murray E, McCabe P, Ballard KJ. A systematic review of treatment outcomes for children with childhood apraxia of speech. American Journal of Speech-Language Pathology. 2014;23(3):486–504. doi: 10.1044/2014_AJSLP-13-0035. [DOI] [PubMed] [Google Scholar]
- Newell K, Carlton M, Antoniou A. The interaction of criterion and feedback information in learning a drawing task. Journal of Motor Behavior. 1990;22(4):536–552. doi: 10.1080/00222895.1990.10735527. [DOI] [PubMed] [Google Scholar]
- Preston JL, Brick N, Landi N. Ultrasound biofeedback treatment for persisting childhood apraxia of speech. American Journal of Speech-Language Pathology. 2013;22(4):627–643. doi: 10.1044/1058-0360(2013/12-0139). [DOI] [PubMed] [Google Scholar]
- Preston JL, Edwards ML. Phonological processing skills of adolescents with residual speech sound errors. Language, Speech and Hearing Services in Schools. 2007;38:297–308. doi: 10.1044/0161-1461(2007/032). [DOI] [PubMed] [Google Scholar]
- Preston JL, Koenig LL. Phonetic variability in residual speech sound disorders: Exploration of subtypes. Topics in Language Disorders. 2011;31(2):168–184. doi: 10.1097/TLD.0b013e318217b875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preston JL, Leaman M. Ultrasound visual feedback for acquired apraxia of speech: A case report. Aphasiology. 2014;28(3):278–295. [Google Scholar]
- Preston JL, McCabe P, Rivera-Campos A, Whittle JL, Landry E, Maas E. Ultrasound visual feedback treatment and practise variability for residual speech sound errors. Journal of Speech, Language, and Hearing Research. 2014;57(6):2102–2115. doi: 10.1044/2014_JSLHR-S-14-0031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preston JL, Molfese PJ, Gumkowski N, Sorcinelli A, Harwood V, Irwin JR, Landi N. Neurophysiology of speech differences in childhood apraxia of speech. Developmental Neuropsychology. 2014;39(5):385–403. doi: 10.1080/87565641.2014.939181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rvachew S. Speech perception training can facilitate sound production learning. Journal of Speech & Hearing Research. 1994;37:347–357. doi: 10.1044/jshr.3702.347. [DOI] [PubMed] [Google Scholar]
- Rvachew S, Nowak M, Cloutier G. Effect of phonemic perception training on the speech production and phonological awareness skills of children with expressive phonological delay. American Journal of Speech-Language Pathology. 2004;13(3):250–263. doi: 10.1044/1058-0360(2004/026). [DOI] [PubMed] [Google Scholar]
- Rvachew S, Ohberg A, Savage R. Young children's responses to maximum performance tasks: Preliminary data and recommendations. Journal of Speech-Language Pathology and Audiology. 2006;30(1):6–13. [Google Scholar]
- Rvachew S, Rafaat S, Martin M. Stimulability, speech perception skills, and the treatment of phonological disorders. American Journal of Speech-Language Pathology. 1999;8(1):33–43. [Google Scholar]
- Schmidt RA, Lee TD. Motor control and learning: A behavioural emphasis. 2nd ed. Human Kinetics; 2011. [Google Scholar]
- Secord WA, Boyce SE, Donohue JS, Fox RA, Shine RE. Eliciting sounds: Techniques and strategies for clinicians. 2nd ed. Thomson Delmar Learning; Clifton Park, NY: 2007. [Google Scholar]
- Semel E, Wiig EH, Secord WA. Clinical evaluation of language fundamentals. 4th ed. Harcourt Assessment, Inc.; 2003. [Google Scholar]
- Shriberg LD. A response evocation programme for /ɝ/ Journal of Speech & Hearing Disorders. 1975;40(1):92–105. doi: 10.1044/jshd.4001.92. [DOI] [PubMed] [Google Scholar]
- Shriberg LD. Childhood speech sound disorders: From postbehaviourism to the postgenomic era. In: Paul R, Flipsen P, editors. Speech sound disorders in children. Plural Publishing; San Diego: 2009. [Google Scholar]
- Shriberg LD, Fourakis M, Hall SD, Karlsson HB, Lohmeier HL, McSweeny JL, Wilson DL. Extensions to the speech disorders classification system (SDCD) Clinical Linguistics & Phonetics. 2010;24(10):795–824. doi: 10.3109/02699206.2010.503006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shriberg LD, Kent RD. Clinical phonetics. 4 ed. Pearson Education; 2013. [Google Scholar]
- Strand EA, Debertine P. The efficacy of integral stimulation intervention with developmental apraxia of speech. Journal of Medical Speech Language Pathology. 2000;8(4):295–300. [Google Scholar]
- Tate RL, McDonald S, Perdices M, Togher L, Schultz R, Savage S. Rating the methodological quality of single-subject designs and n-of-1 trials: Introducing the Single-Case Experimental Design (SCED) scale. Neuropsychological Rehabilitation. 2008;18(4):385–401. doi: 10.1080/09602010802009201. [DOI] [PubMed] [Google Scholar]
- Terband H, Maassen B, Guenther FH, Brumberg J. Computational neural modeling of speech motor control in childhood apraxia of speech (CAS) Journal of Speech, Language, and Hearing Research. 2009;52(6):1595–1609. doi: 10.1044/1092-4388(2009/07-0283). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thoonen G, Maassen B, Gabreëls F, Schreuder R. Validity of maximum performance tasks to diagnose motor speech disorders in children. Clinical Linguistics & Phonetics. 1999;13(1):1–23. [Google Scholar]
- Wagner RK, Torgesen JK, Rashotte CA, Pearson NR. Comprehensive test of phonological processing. 2nd ed. Pro-Ed; Austin, TX: 2013. [Google Scholar]
- Wechsler D. Wechsler abbreviated scales of intelligence. 2nd ed. Pearson; San Antonio, TX: 2011. [Google Scholar]
- Williams KT. Expressive vocabulary test. 2nd ed. Pearson; Minneapolis, MN: 2007. [Google Scholar]
- Wulf G, McNevin N. Simply distracting learners is not enough: More evidence for the learning benefits of an external focus of attention. European Journal of Sport Science. 2003;3:1–13. [Google Scholar]