Abstract
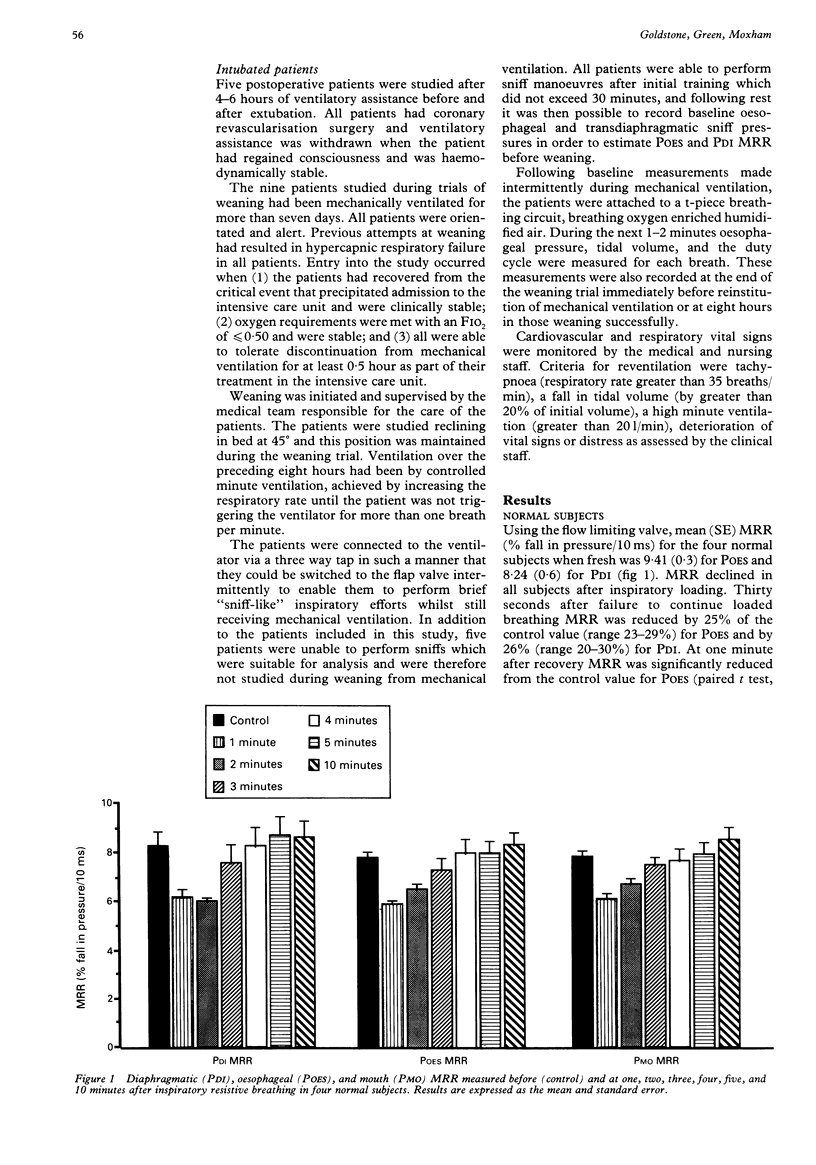
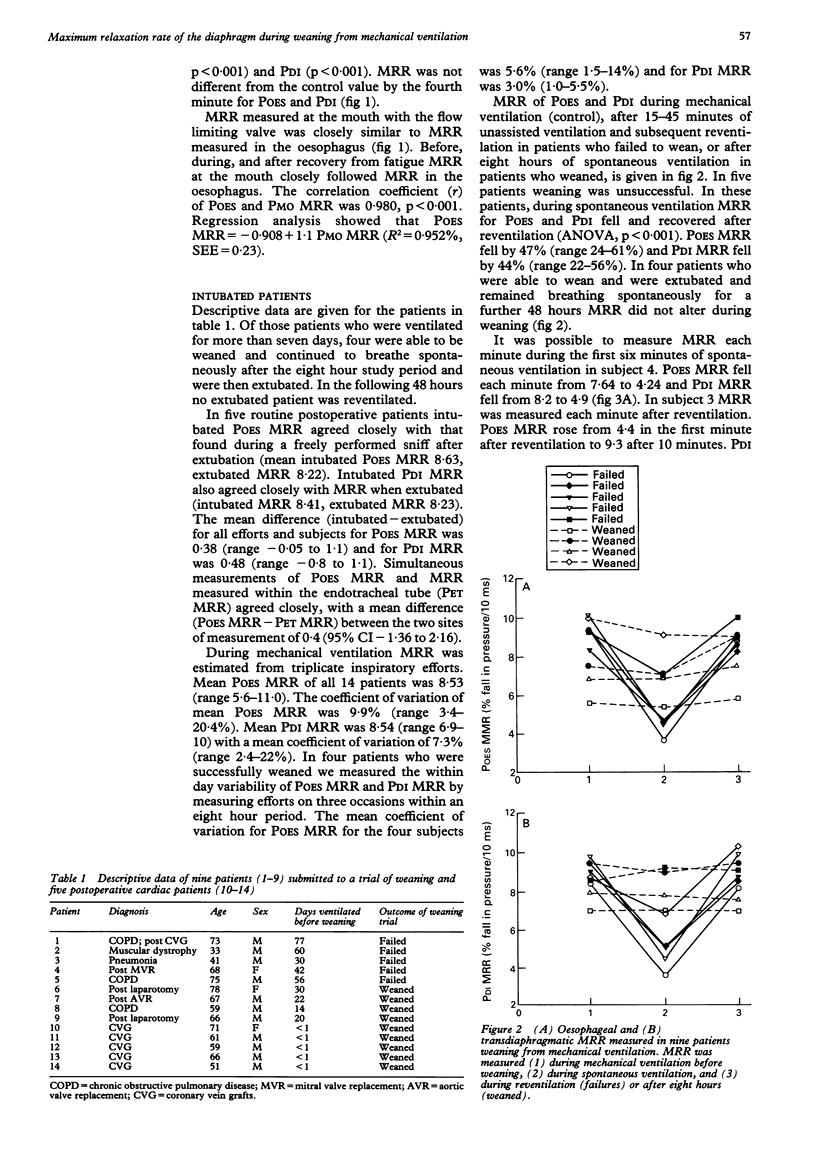
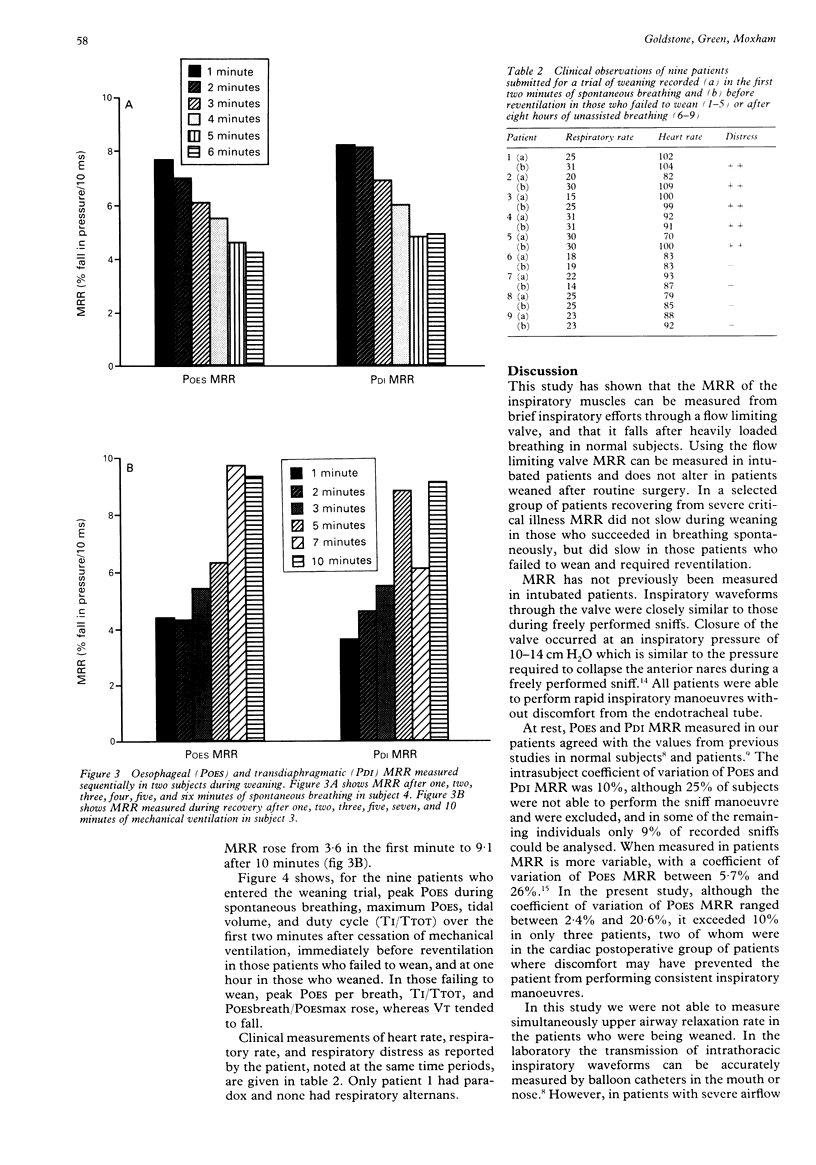
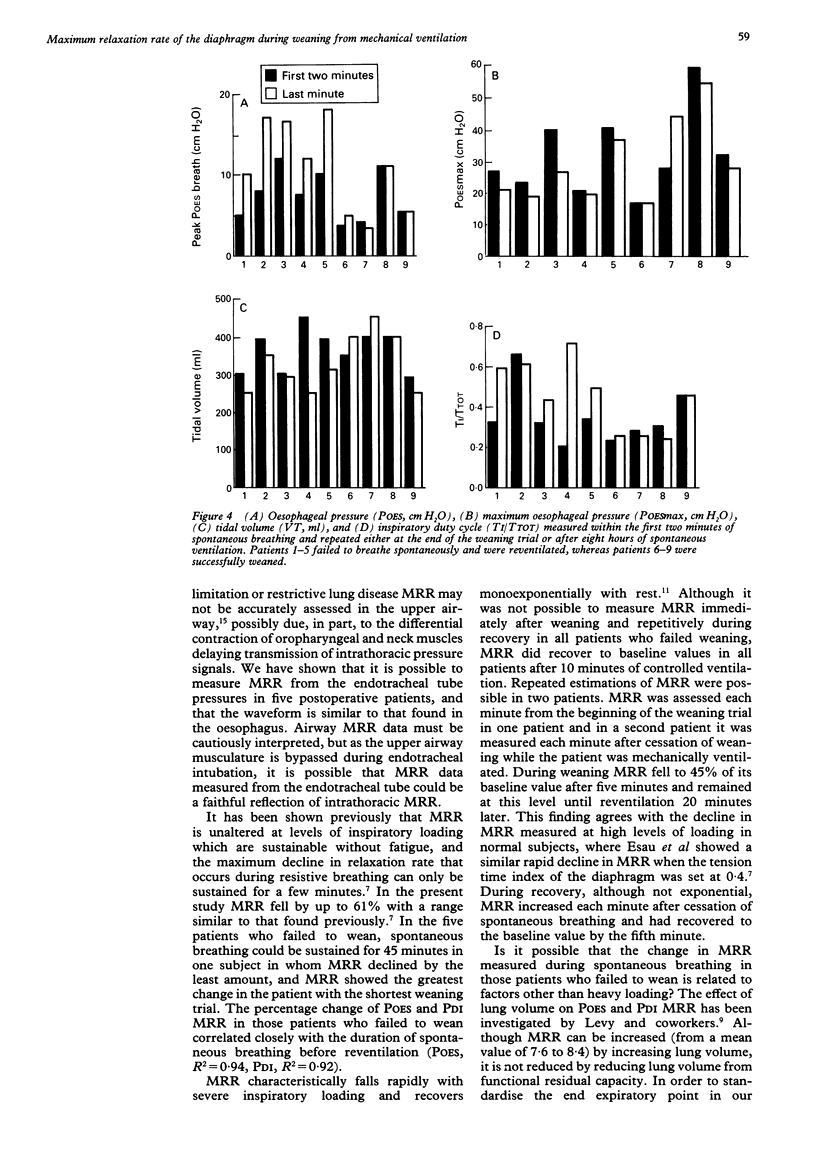
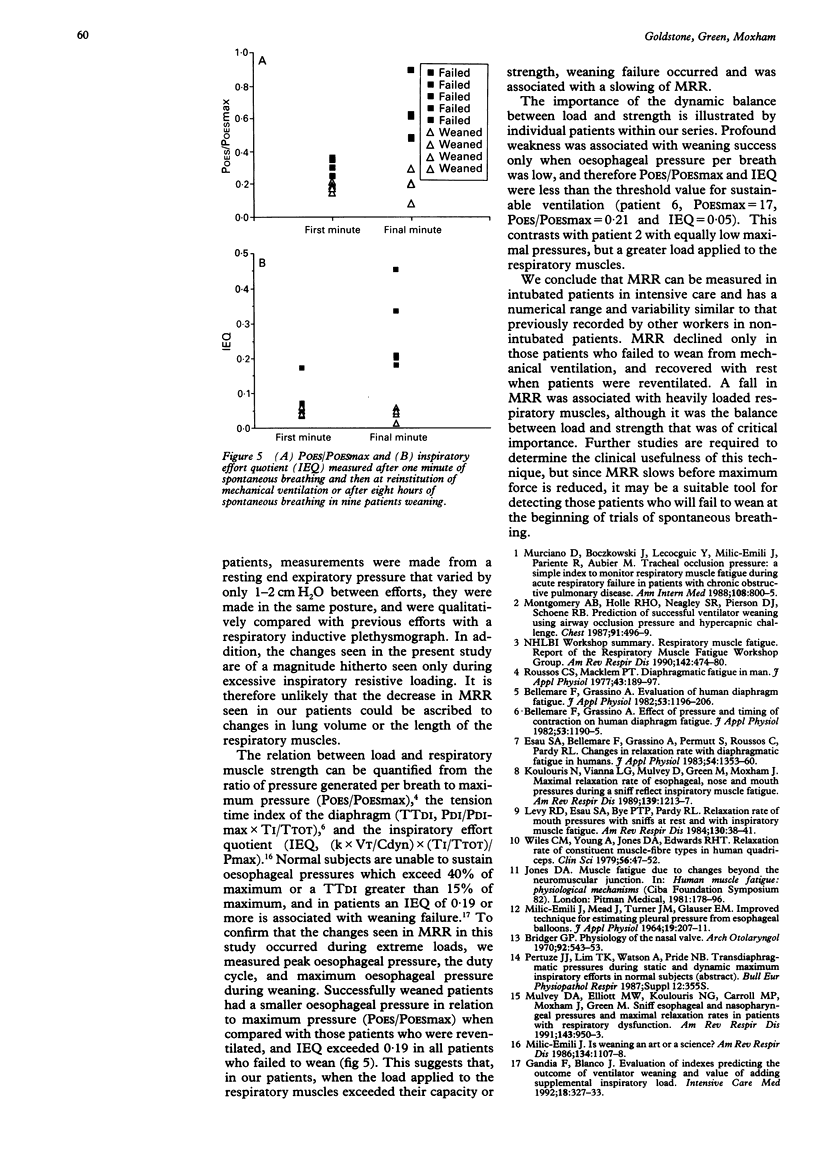
BACKGROUND--The maximum relaxation rate (MRR; percentage fall in pressure/10 ms) of oesophageal (POES) and transdiaphragmatic (PDI) pressure slows under conditions of loaded breathing, and has been measured previously in normal subjects. MRR has not been measured in intubated patients weaning from mechanical ventilation. METHODS--Five postoperative patients who were expected to wean and nine patients who had previously failed were studied. POES and PDI MRR, peak oesophageal pressure during spontaneous breathing, maximum oesophageal pressure, and the inspiratory duty cycle were measured at rest during mechanical ventilation, in the first two minutes of spontaneous breathing, and after reventilation in those patients who failed, or before extubation in those patients who succeeded. RESULTS--At rest POES MRR in intubated patients had a range of 5.6-11 and PDI MRR 6.9-10.0, with a coefficient of variation of 9.9% and 7.3% respectively. POES and PDI MRR were similar before and after extubation in five postoperative patients, and POES MRR was reflected by endotracheal MRR measured at the airway. In five patients who failed to wean POES and PDI MRR slowed by 47% and 44%, and fully recovered after 10 minutes reventilation. In four patients who were successfully weaned MRR was unchanged during spontaneous breathing. At the time when MRR decreased, the respiratory muscles were heavily loaded in relation to their strength. CONCLUSIONS--Weaning failure occurs when the applied load exceeds the capacity of the respiratory muscles, and this is associated with a slowing of respiratory muscle MRR.
Full text
PDF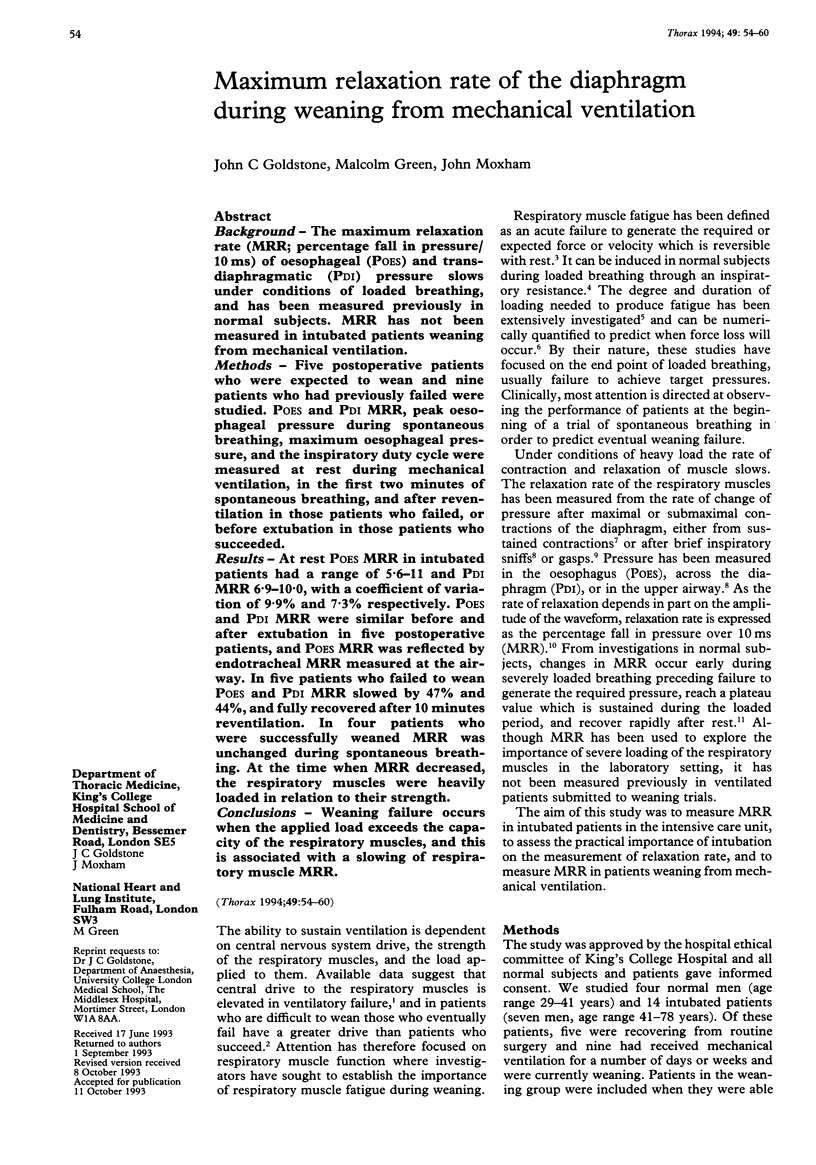
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bellemare F., Grassino A. Effect of pressure and timing of contraction on human diaphragm fatigue. J Appl Physiol Respir Environ Exerc Physiol. 1982 Nov;53(5):1190–1195. doi: 10.1152/jappl.1982.53.5.1190. [DOI] [PubMed] [Google Scholar]
- Bridger G. P. Physiology of the nasal valve. Arch Otolaryngol. 1970 Dec;92(6):543–553. doi: 10.1001/archotol.1970.04310060015005. [DOI] [PubMed] [Google Scholar]
- Esau S. A., Bellemare F., Grassino A., Permutt S., Roussos C., Pardy R. L. Changes in relaxation rate with diaphragmatic fatigue in humans. J Appl Physiol Respir Environ Exerc Physiol. 1983 May;54(5):1353–1360. doi: 10.1152/jappl.1983.54.5.1353. [DOI] [PubMed] [Google Scholar]
- Gandia F., Blanco J. Evaluation of indexes predicting the outcome of ventilator weaning and value of adding supplemental inspiratory load. Intensive Care Med. 1992;18(6):327–333. doi: 10.1007/BF01694360. [DOI] [PubMed] [Google Scholar]
- Jones D. A. Muscle fatigue due to changes beyond the neuromuscular junction. Ciba Found Symp. 1981;82:178–196. doi: 10.1002/9780470715420.ch11. [DOI] [PubMed] [Google Scholar]
- King R. J. Pulmonary surfactant. J Appl Physiol Respir Environ Exerc Physiol. 1982 Jul;53(1):1–8. doi: 10.1152/jappl.1982.53.1.1. [DOI] [PubMed] [Google Scholar]
- Koulouris N., Vianna L. G., Mulvey D. A., Green M., Moxham J. Maximal relaxation rates of esophageal, nose, and mouth pressures during a sniff reflect inspiratory muscle fatigue. Am Rev Respir Dis. 1989 May;139(5):1213–1217. doi: 10.1164/ajrccm/139.5.1213. [DOI] [PubMed] [Google Scholar]
- Levy R. D., Esau S. A., Bye P. T., Pardy R. L. Relaxation rate of mouth pressure with sniffs at rest and with inspiratory muscle fatigue. Am Rev Respir Dis. 1984 Jul;130(1):38–41. doi: 10.1164/arrd.1984.130.1.38. [DOI] [PubMed] [Google Scholar]
- MILIC-EMILI J., MEAD J., TURNER J. M., GLAUSER E. M. IMPROVED TECHNIQUE FOR ESTIMATING PLEURAL PRESSURE FROM ESOPHAGEAL BALLOONS. J Appl Physiol. 1964 Mar;19:207–211. doi: 10.1152/jappl.1964.19.2.207. [DOI] [PubMed] [Google Scholar]
- Montgomery A. B., Holle R. H., Neagley S. R., Pierson D. J., Schoene R. B. Prediction of successful ventilator weaning using airway occlusion pressure and hypercapnic challenge. Chest. 1987 Apr;91(4):496–499. doi: 10.1378/chest.91.4.496. [DOI] [PubMed] [Google Scholar]
- Mostow S. R. Influenza--a preventable disease not being prevented. Am Rev Respir Dis. 1986 Jul;134(1):1–1. doi: 10.1164/arrd.1986.134.1.1. [DOI] [PubMed] [Google Scholar]
- Mulvey D. A., Elliott M. W., Koulouris N. G., Carroll M. P., Moxham J., Green M. Sniff esophageal and nasopharyngeal pressures and maximal relaxation rates in patients with respiratory dysfunction. Am Rev Respir Dis. 1991 May;143(5 Pt 1):950–953. doi: 10.1164/ajrccm/143.5_Pt_1.950. [DOI] [PubMed] [Google Scholar]
- Murciano D., Boczkowski J., Lecocguic Y., Emili J. M., Pariente R., Aubier M. Tracheal occlusion pressure: a simple index to monitor respiratory muscle fatigue during acute respiratory failure in patients with chronic obstructive pulmonary disease. Ann Intern Med. 1988 Jun;108(6):800–805. doi: 10.7326/0003-4819-108-6-800. [DOI] [PubMed] [Google Scholar]
- Roussos C. S., Macklem P. T. Diaphragmatic fatigue in man. J Appl Physiol Respir Environ Exerc Physiol. 1977 Aug;43(2):189–197. doi: 10.1152/jappl.1977.43.2.189. [DOI] [PubMed] [Google Scholar]
- Wiles C. M., Young A., Jones D. A., Edwards R. H. Relaxation rate of constituent muscle-fibre types in human quadriceps. Clin Sci (Lond) 1979 Jan;56(1):47–52. doi: 10.1042/cs0560047. [DOI] [PubMed] [Google Scholar]



