Abstract
Objective
Cancer patients and survivors are assuming active roles in decision-making and digital patient support tools are widely used to facilitate patient engagement. As part of Cancer Information Service Research Consortium’s randomized controlled trials focused on the efficacy of eHealth interventions to promote informed treatment decision-making for newly diagnosed prostate and breast cancer patients, and post-treatment breast cancer, we conducted a rigorous process evaluation to examine the actual use of and perceived benefits of two complementary communication channels -- print and eHealth interventions.
Methods
The three Virtual Cancer Information Service (V-CIS) interventions were developed through a rigorous developmental process, guided by self-regulatory theory, informed decision-making frameworks, and health communications best practices. Control arm participants received NCI print materials; experimental arm participants received the additional V-CIS patient support tool. Actual usage data from the web-based V-CIS was also obtained and reported.
Results
Print materials were highly used by all groups. About 60% of the experimental group reported using the V-CIS. Those who did use the V-CIS rated it highly on improvements in knowledge, patient-provider communication and decision-making.
Conclusion
The findings show that how patients actually use eHealth interventions either singularly or within the context of other communication channels is complex.
Practice Implications
Integrating rigorous best practices and theoretical foundations is essential and multiple communication approaches should be considered to support patient preferences.
Keywords: EHealth interventions, cancer patients, decision making, intervention development, utilization, preferences
1.1 INTRODUCTION
1.1.1 Background on Cancer Patient Decision Making and Information Channels
Advances in breast and prostate cancer treatment and supportive care have led to a growing number of care options for patients and survivors (Tiwari and Roy, 2011). Patients with these early stage cancers typically often are presented with a choice of treatment options with similar outcomes. These “preference-sensitive” decisions require knowledge about the treatment alternatives and an understanding of one’s own values to ensure a quality decision (O’Connor et al., 2007, Sepucha et al., 2010). Cancer patients also need to manage long-term disease and treatment effects, cope with the psychological challenges of survivorship, and find support for health promoting behaviors during the “re-entry” phase of their cancer experience (Stanton, 2012). As a result, cancer patients and survivors are increasingly assuming an active role in treatment decisions (Cayton, 2006) and would benefit from well-designed and effective support tools. Access to evidence-based and understandable medical information to increase self-efficacy is foundational to informed decision making and the delivery of this information can be provided in various communication channels and approaches. Although traditional communication approaches, such as printed materials are still widely used, the advances in technology and rising Internet usage (Zickuhr and Smith, 2012) have made eHealth approaches in patient support tools commonplace. These eHealth tools have been shown to facilitate the patient’s role in treatment decision making, communication and survivorship management (Dorfman et al., 2010, Hawn, 2009). With the emerging evidence supporting the positive impact of well-designed and theory-driven eHealth tools and the broad availability of multiple information sources, this paper focuses on the systematic development of eHealth cancer decision tools for the Cancer Information Service Research Consortium’s (CISRC) randomized trials and the utilization of complementary interventions (print and eHealth). Our findings provide insights into the exploration of how patients use complementary information sources (Rains, 2007, Ruppel and Rains, 2012, Dutta-Bergman, 2004, Johnson and Meischke, 1993) in their decision making.
1.1.2 Overview of the Cancer Information Research Consortium Study and Interventions
The NCI-funded Cancer Information Service Research Consortium’s (CISRC) multi-site randomized trial tested three theory-based interactive, multi-media interventions to help newly diagnosed prostate and breast cancer patients make informed treatment decisions (Projects 1 and 2, respectively) and breast cancer patients prepare for life after treatment (Project 3). The study design and implementation are described in detail elsewhere. (Marcus et al., 2013)
Using a theory-guided (Miller and Diefenbach, 1998, Miller et al., 1999) evidence-based approach (Fleisher et al., 2008, Fleisher et al., 2014, Holmes-Rovner, 2007), three separate VCIS eHealth interventions (one per research project ) were designed and evaluated to determine impact on informed decision making and quality of life outcomes. The V-CIS for each project was available in two formats – CD or on the Internet. The 2 versions were identical, just delivered on two formats so participants could choose based on their own preference and access to high-speed Internet (since this was a rich multi-media based site). The interventions were also informed by emerging best practices and standards for development, including: health literacy and cultural relevance, utilization of vetted evidence-based content, and rigorously solicited stakeholder and user input throughout the iterative developmental process. In addition to the impact evaluation, we conducted an extensive process evaluation to determine participants’ perceptions of the value of the intervention as well as their subjective and objective utilization of the intervention which is the focus of this paper.
The application of theory (Miller and Diefenbach, 1998) and intervention development best practices (Fleisher et al., 2014) as well as evaluation of their impact and use, are vital to understanding the value of these tools for addressing the complex issues cancer patients face. Consensus-based standards, such as the International Patient Decision Aid Standards (IPDAS), designed to enhance the quality and effectiveness of patient decision aids using a set of criteria to improve the content, development, implementation, evaluation and systematic development recommendations (Elwyn et al., 2011), have emerged to guide the quality and effectiveness of these tools. However, even when these standards are applied, the picture remains complex as to how patients actually use these support tools, either singularly or within the context of other communication channels (Dorfman et al., 2010, Fleisher et al., 2012, Ryhänen et al., 2010).
This paper describes the iterative, evidence-based and stakeholder driven process used to develop the three eHealth interventions (V-CIS) used in the experimental arm of the studies and a comprehensive process evaluation exploring patients self-reported use and value of both the eHealth and standard print interventions; predictors of V-CIS self-reported use; as well as the actual usage of the web-based version based on data gathered from tracking software. Although not an a priori hypotheses, a stepwise logistic regression was used to identify predictors of V-CIS self-reported use (e.g. age, education, household income, how much control group materials were read, and recruitment source) conducted separately for each project. With the emergence of eHealth tools, often at the replacement of more traditional patient support tools, it is critical that we understand patient preferences and the potential complementary nature of both traditional and new eHealth approaches. Participant’s web usage data also offer rich sources of information that can be used to understand their mechanisms of action and to optimize their effectiveness.
2.1 METHODS & MATERIALS
2.1.1 Development and Description of the Virtual CIS (V-CIS) Interventions
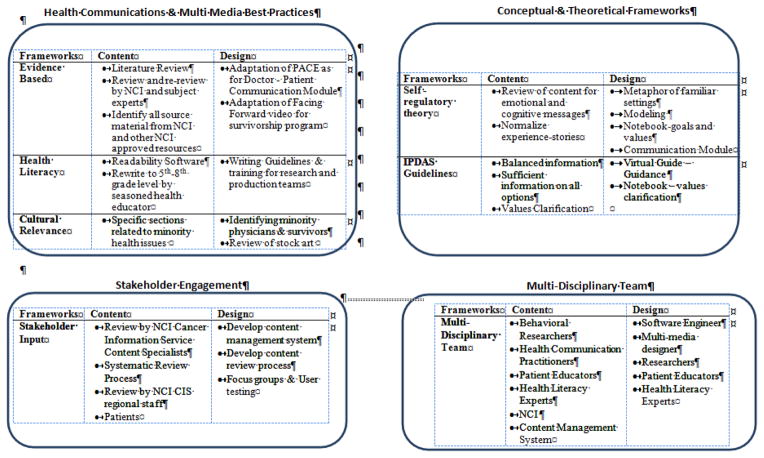
Although the content of each of the three V-CIS software programs varied given their focus on a specific cancer and time in the trajectory of treatment, a common structure and approach was used. This approach included theoretical underpinnings and health communications best practices. As shown in Figure 1, four domains were addressed in the development process, including: 1) health communications and multi-media best practices; 2) integration of conceptual and theoretical frameworks; 3) stakeholder engagement; and 4) use of a multi-disciplinary team.
Figure 1.
Application of Theory & Best Practice Frameworks for the Development of the V-CIS
The structure of the intervention was similar across the projects and consisted of four modules: Library – Text-based information on a variety of relevant topics, (e.g., “what is prostate cancer”, treatment options, side effects, clinical trials, emotions after breast cancer treatment). Patient Stories – Multi-media testimonials with actual patients were used and presented either with video or still photographs with voice-overs (a piece of narration in the video, not accompanied by an image of the speaker) focusing on relevant issues including treatment choices, potential side-effects, emotional reactions, and survivorship. Doctor’s Office – Video-based and text-based information on cancer-specific topics and frequently asked questions as well as video demonstrations of how to communicate with providers using an evidence-based communication approach (Wen et al., 2012). Notebook – Interactive values clarification or action plan. For Project 1 & 2, the notebook served as the values clarification tool where patients could list the pros and cons of each treatment approach and rank them in terms of their personal values. For Project 3, the notebook served as an action plan for the issues that were personally relevant to each woman. Additional details about each of the three interventions are described in previous published articles (Marcus, et al. 2013).
The theoretical constructs of self-regulatory theory (Miller and Diefenbach, 1998) were operationalized in all three V-CIS interventions by normalizing the experience, using familiar settings as a metaphor, modeling self-management through the patient testimonials and communication role play, and the notebook which facilitated users’ identification of their own values and needs. We also addressed the IPDAS standards of providing balanced information and information on all options, including values clarification, and providing navigation in the interactive software through a gender-specific Virtual Guide.
Guided by health communications best practices, the content for each of the three V-CIS programs was based on the literature, adapted from evidence-based resources and was reviewed through a rigorous process with the National Cancer Institute’s (NCI) Cancer Information Service (CIS). It was reviewed and re-written by health literacy experts using plain language (with many sections at 5th–8th grade reading level) and both content and visuals were carefully developed and tested for a multi-cultural population. Stakeholders, such as the NCI’s CIS national and regional staff and cancer patients were involved throughout the process and many changes were made based on this feedback. The CISRC’s multi-disciplinary Intervention Development & Measurement Core (S. Miller PI) oversaw the development and production of the V-CIS interventions, working closely with each of the research teams and the software production company with considerable contribution from each of the Principal Investigators. The development and production of the three eHealth tools required 16 months.
2.1.2 Study Procedures
Callers to the CIS (Cancer Information Service), ACS (American Cancer Society) or CISRC call centers were asked to participate in the study (Stanton, 2012). Those who expressed interest at the end of a usual service call completed a baseline and screening survey with the CIS Information Specialists, and if eligible were randomized to either a control arm receiving NCI materials or an intervention arm including NCI materials, CD of the multi-media patient support tool and a letter with the web address for the multi-media website within a week after their initial call. Eligibility and recruitment are discussed in detail in Marcus, et al and Stanton et al. Patients in the intervention arm had access to the V-CIS through either CD or the internet based on their preference. They also received a reminder letter about using the V-CIS two weeks after enrollment. Project 3 had two experimental arms, one with the V-CIS alone and one with both the V-CIS and a callback from a CIS Information Specialist at 10–14 days after enrollment to address any questions or issues they might be facing. In addition, those enrolled in the call back arm of the study were reminded by the Information Specialist about the software and encouraged to view it.
2.1.3 Data Collection & Measures
Data were collected at three points: at the end of the usual service call to the CIS (baseline) and at two and nine months after baseline. Eligible participants were consented at baseline and completed a short telephone survey to collect demographics, disease-related information, stage of decision making or point in medical treatment, and other psychosocial outcome measures. Telephone follow-up interviews occurred at two and nine months after enrollment. Process data were collected at two months and included all participants self-reported use of the interventions (either print or print and V-CIS) and satisfaction and utility only for those using the V-CIS. These data (including dimensions of impact on knowledge, confidence in decision making, helpful on communication with provider, impact on emotional coping, helpful on managing side effects, or adjusting to life post-treatment) were collected using a 13-item Likert-type survey developed by the research team (Table 2 includes the majority of the items). Those who reported not using the intervention were asked their reasons for nonuse (reason options include: no time/too busy, not needed, computer/technology problem and don’t know how to use it).
Table 2.
Participants’ Self-Reported Satisfaction With the V-CIS at Two Months Follow-Up
| Project 1 | Project 2 | Project 3 | |
|---|---|---|---|
|
| |||
| M (SD) | M (SD) | M (SD) | |
| 1. Increased Knowledge* | 1.69 (.59) | 1.89 (.64) | 2.12 (.67) |
| 2. Helped me talk to my doctor* | 1.80 (.56) | 2.10 (.71) | 2.44 (.67) |
| 3. Helped me with emotional concerns | 2.01 (.63) | 2.06 (.64) | 2.09 (.64) |
| 4. Made me feel more anxious* | 2.98 (.66) | 2.97 (.67) | 3.17 (.50) |
| 5. Made me feel more confident* | 1.84 (.58) | 2.01 (.58) | 2.07 (.55) |
| 6. Helped me make treatment decisions* | 1.87 (.59) | 2.27 (.77) | N/A |
| 7. Information helped me deal with cancer treatment* | 1.76 (.55) | 2.03 (.66) | N/A |
| 8. Information helped me deal with side effects | 1.99 (.63) | 2.22 (.68) | 2.15 (.60) |
| 9. Helped me deal with emotional concerns of recurrence | 2.25 (.66) | 2.34 (.72) | N/A |
| 10. Helped me adjust to life after treatment | 2.18 (.60) | N/A | 2.17 (.59) |
| 11. Helped me understand my follow-up care | 2.06 (.57) | 2.09 (.62) | 2.15 (.60) |
p<.001, ANOVA
2.1.4 Usage Tracking
Objective data regarding the actual use of the website version of the eHealth interventions were collected. Participants who accessed the V-CIS software through the Internet were asked to consent to a sub-study that tracked their use of the software. This was not a primary aim of the study, but rather an exploratory aim to gain insights into what components of the eHealth support tools were used and by whom. This web usage data included total hits per user session on the V-CIS program, as well as hits on each of the program modules (Library, Patient Stories, Doctor’s Office, and Notebook) and pages. Total session time, calculated from time of first hit on the program and each module to time of the last mouse click, was also assessed.
2.1.5. Statistical Approach
Descriptive statistics including age, race, income, education and recruitment source of all study participants were computed. One-way analyses of variance were employed to compare the control and intervention groups on the continuous variables (e.g., age), and χ2 tests were used on the categorical variables (e.g., race, recruitment source) at baseline. Descriptive analyses of participants’ self-reported use of control group materials and intervention obtained from the two-month follow-up interview were also compared between groups using χ2 tests. Reasons for not using the V-CIS intervention were described. Mean scores for the satisfaction items (for those who reported using the V-CIS interventions) were calculated for each item and compared across projects using t tests and analysis of variance, with a required value of p < 0.05. Because we did not pose a priori hypotheses regarding predictors of use, stepwise logistic regression was used to identify predictors of V-CIS self-reported use, conducted separately for each project. The following predictors, common across the trials, were examined: age, education, household income, how much control group materials were read, and recruitment source.
4.1 RESULTS
4.1.1 Description of Subjects
Eligible patients were recruited and randomized (N = 2,134) to each of the three distinct projects (Project 1- Prostate cancer patients = 439; Project 2 – Diagnosed breast cancer patients = 617; Project 3 – Breast cancer patients who have completed primary treatment = 1078). Differences in project sample sizes were related to challenges in recruitment (Project 1) and two experimental groups (Project 3 – V-CIS alone and V-CIS with call back. Recruitment methods and challenges are reported elsewhere (Stanton et al., 2013). Enrolled participants were mainly non-Hispanic White (77% for Project 1, 81% for Project 2, and 93% for Project 3). The mean age of participants was 65 years (SD=9.6) for Project 1, significantly higher (p = <.05) than those for Project 2 (55 years, SD=11.6) and Project 3 (54 years, SD=10.3). All participants had a least a high school education, with a significantly higher percentage reporting a post-graduate degree by Project 3 participants (68%) than Project 1 participants (51%) and Project 2 participants (49%). Seventy-one percent of Project 3 participants reported an income level more than $60K, significantly higher than those reported by Project 1 participants (49%) and Project 2 participants (40%). The majority of Project 1 (73%) and Project 2 (75%) participants were recruited by CIS and American Cancer Society (ACS) call centers, whereas most Project 3 (78%) participants were referred through Dr. Susan Love Research Foundation’s Love/Avon Army of Women (AOW) email recruitment efforts.
4.1.2. Utilization of the Study Interventions
All study participants received the standard NCI print materials and over 90% of participants reported reading them and at least two-thirds stated that they read most to all of those materials (Table 1).
Table 1.
Self-Reported Use of Standard Print and V-CIS* at Two Months Follow-Up
|
Project 1 N = 339 |
Project 2 N = 476 |
Project 3 N = 945 |
|||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Control N (%) |
V-CIS N (%) |
Control N (%) |
V-CIS N (%) |
Control N (%) |
V-CIS N (%) |
V-CIS & Callback N (%) |
|
| How much print read | |||||||
| None | 3 (02) | 7 (04) | 9 (04) | 20 (09) | 12 (04) | 29 (09) | 22 (07) |
| Very little to some | 38 (24) | 36 (21) | 50 (21) | 59 (26) | 74 (23) | 76 (23) | 71 (24) |
| Most to all | 118 (74) | 131 (75) | 180 (75) | 150 (66) | 232 (73) | 208 (67) | 204 (69) |
|
| |||||||
| Self-reported use of V-CIS | NA | NA | NA | ||||
| Yes | 96 (57) | 127 (57) | 206 (66) 1 | 223 (74) 1 | |||
| No | 73 (43) | 96 (43) | 107 (34) | 78 (26) | |||
| Which version | NA | NA | NA | ||||
| Website | 52 (54) | 70 (56) | 138 (67) | 139 (62) | |||
| CD | 23 (24) | 26 (20) | 41 (20) | 39 (17) | |||
| Both | 21 (22) | 31 (24) | 27 (13) | 45 (20) | |||
| How much time | NA | NA | NA | ||||
| 30 min or less | 19 (21) | 28 (23) | 37 (18) | 49 (22) | |||
| About 1 hour | 25 (27) | 50 (40) | 69 (34) | 76 (34) | |||
| more than 1 hour | 48 (52) | 46 (37) | 99 (48) | 97 (44) | |||
| Use of the library | NA | NA | NA | ||||
| Yes | 50 (60) | 78 (70) | 158 (79) | 164 (77) | |||
| No | 34 (40) | 33 (30) | 43 (21) | 50 (23) | |||
| Use of the patient stories | NA | NA | NA | ||||
| Yes | 70 (81) | 97 (79) | 153 (75) | 164 (76) | |||
| No | 16 (19) | 26 (21) | 50 (25) | 52 (24) | |||
| Use of the doctor’s office | NA | NA | NA | ||||
| Yes | 62 (75) | 80 (70) | 137 (69) | 127 (62) | |||
| No | 21 (25) | 34 (30) | 61 (31) | 77 (38) | |||
| Use of the notebook | NA | NA | NA | ||||
| Yes | 33 (38) | 35 (29) | 91 (45) | 83 (39) | |||
| No | 54 (62) | 84 (71) | 111 (55) | 132 (61) | |||
Pearson Chi-square, p=0.026, Comparison between V-CIS and V-CIS and Callback Project 3
Missing data in some variables related to V-CIS use
Over half of the men (57%) in Project 1, 57% of the women in Project 2 and 70% in Project 3 reported using the V-CIS software (both CD and web-based version combined), with significantly higher self-reported usage in Project 3 (p=0.05). Further, women in Project 3 who received the callback as an addition to the V-CIS program were significantly more likely to use the software than those who received the V-CIS program only (66% vs. 74%, p=0.026). Most participants who reported using V-CIS accessed via the Internet, either alone or in combination with the CD version, although some participants used only the CD version (24% for Project 1, 20% for Project 2, 19% for Project 3). Across all projects, a high percentage of users reported using the programs for one or more hours: 79% for Project 1, 77% for Project 2, and 82% (V-CIS only) and 78% (V-CIS + callback) for Project 3. Overall, based on self-report, the Library, Patient Stories and Doctor’s Office were viewed by at 60–81%, while the Notebook (the values clarification component) was used by less than 50% of participants.
4.1.3. Predictors of V-CIS use
Predictors of V-CIS self-reported use were reported using a step-wise selection approach conducted separately for each project. For Project 1 (Cox & Snell R2 = 0.22, Model chi-square = 40.1, p=0.00), having some college (OR=2.68, p=0.01) and had read the print material (OR=12.6, p=0.03) increased the odds of having used the V-CIS. Compared with CIS recruitment, being recruited by ACS decreased the odds of having used the V-CIS (OR=0.42, p=0.05). For project 2 (Cox & Snell R2 = 0.15, Model chi-square = 34.1, p=0.00), having read the print material (OR = 11.9, p = 0.00) and being recruited by AOW (compared with CIS) (OR = 5.2, p=0.00) increased the odds of having used the V-CIS. For project 3 (Cox & Snell R2 = 0.11, Model chi-square = 61.1, p=0.00), only having read the print material (OR=9.9, p=0.00) increased the odds of having used the V-CIS.
4.1.4. Participants’ Reported Perceived Benefit of the V-CIS
As noted above, participants who reported using the software (either web or CD) were also asked a series of questions regarding the perceived benefit of the software using a four-point Likert-type rating scale, with “1” being strongly agree to “4” being strongly disagree. The V-CIS was well received by participants, with an overall mean program satisfaction score ranging from 1.7 to 2.0 (all items combined). However, there were significant differences across projects on five items (Table 2). Participants in Project 3, although still very positive, were less likely to agree that V-CIS increased their knowledge and helped them talk to their doctor, and more likely to say it made them feel more anxious than Project 1 and 2 (ANOVA, p<0.001). Project 1 participants were more likely to state that V-CIS made them more confident and helped them make treatment decisions than Project 2 participants (ANOVA, p=0.007).
4.1.5. Participants’ Reported Reasons for Not Using the V-CIS
Participants who did not report using the V-CIS (n=355) were asked their reasons for not using the software. There were significant differences within and across projects regarding the reasons for nonuse. In Project 1, 21% of men reported that there was “no time or they were too busy”, in comparison to 30% of women in Project 2, and 47% (V-CIS only) and 49% (V-CIS + call back) in Project 3. In the two projects focused on treatment decision making, 25% in Project 1 and 14% in Project 2 stated that V-CIS was “not needed,” whereas those proportions were 11% (V-CIS only) and 13% (V-CIS + callback) in Project 3. Finally, a sizeable proportion of participants stated they had technical problems (e.g., computer problems, problems with the software or didn’t know how to use), ranging from 41% of non-users in Project 1, 25% in Project 2 and 28% (V-CIS only) and 16% (V-CIS + callback) in Project 3. It is of interest that very few participants availed themselves of the publicized Help Line.
4.1.6. Objective Tracking of V-CIS Usage
Participants with baseline data (e.g. Study ID) that could be linked with actual V-CIS use during the two-month post enrollment period were included in the objective usage analysis. This included 32 Project 1 users, 35 Project 2 users, and 282 Project 3 users who consented to take part in the tracking sub-study and accessed the web-based V-CIS. Only one participant across projects declined to give consent for the tracking study. As shown in Table 3, users logged in about 2 times on average across all projects. Project 1 participants spent considerably more time during their first login (38.5 minutes) in comparison to Project 2 (20.7 minutes) and Project 3 (25.2 minutes) and they spent almost double the time overall. Over 90% of all participants accessed the Library and spent almost 20 minutes on average. The Patient Stories and Doctor’s Office were accessed by 50–60% of all users, with Project 1 participants spending more time in these sections as compared to participants in Projects 2 and 3. Finally, the Notebook was accessed by 41% of users in Project 1, 31% in Project 2 and 22% in Project 3 and the time spent was considerably less than the other modules.
Table 3.
Two month post enrollment usage analytics by Project in minutes and percentage of time
| 2-Month | Project 1(n=32) | Project 2 (n=35) | Project 3 (N=283) | |||
|---|---|---|---|---|---|---|
| M (SD) | % of participants | M (SD) | % of participants | M (SD) | % of participants | |
| # of logins | 2.3 (2.1) | 59% logged on more than once | 2.2 (1.5) | 62.9% logged on more than once | 2.0 (1.7) | 49.1% logged on more than once |
| Average time spent during 1st login | 38.5 (25.4) | 20.7 (14.5) | 25.2 (19.5) | |||
| Average overall time spent | 70.9 (67.6) | 35.7 (24.8) | 38.9 (28.9) | |||
| The library time spent among those who accessed | 23.0 (19.8) | 96.4% accessed the library | 17.9 (17.7) | 97.1% accessed the library | 18.4 (19.4) | 90.1% accessed the library |
| The patient stories time spent among those who accessed | 31.3 (21.1) | 50% accessed the patient story | 6.7 (6.3) | 51.4% accessed the patient story | 17.2 (9.5) | 62.9% accessed the patient story |
| The doctor’s office time spent among those who accessed | 25.9 (41.1) | 59.3% accessed the doctor’s office | 5.4 (6.0) | 51.4% accessed the doctor’s office | 6.4 (6.5) | 57.6% accessed the doctor’s office |
| The notebook’s time spent among those who accessed | 13.3 (18.0) | 40.6% accessed the notebook | 10.7 (9.4) | 31.4% accessed the notebook | 2.4 (2.5) | 22.3% accessed the notebook |
5.1 Discussion
A cancer diagnosis is a life-changing event that requires an understanding of sophisticated and complex medical information. This is especially true when multiple options have equal success, and the numerous psychosocial and physical concerns and issues that need to be managed can last for years. The V-CIS eHealth interventions were designed based on a rigorous process (Elwyn et al., 2012) addressing current recommendations and guidelines for the development of decision tools, and careful attention to behavioral theory and health communication best practices. The development required almost 16 months including an extensive amount of time from our multi-disciplinary team including researchers, patient education experts and our technology partner as well as multiple reviews by NCI and CIS management and line staff. However, this labor and expert intensive process was critical to developing a high quality intervention. The feedback from VCIS users indicated that it significantly increased their self-reported knowledge, helped them to talk with their doctor, feel less anxious and more confident, and helped them make treatment decisions.
5.1.1. Use of complementary channels -- print and eHealth tools
One of the key findings, and somewhat unexpected, is that cancer patients value both print and more sophisticated eHealth health interventions. Recent reviews of the literature indicate that many studies comparing multi-media and print materials have shown mixed results regarding the added benefit of multimedia (Wilson et al., 2012), highlighting the complexity of patient actual and perceived needs, variations in the rigor of the development of the materials, access to and preferences of various communication channels, and questions of how these materials were actually used. Moreover, research based on Channel Complementarity Theory (Rains, 2007, Ruppel and Rains, 2012, Dutta-Bergman, 2004) highlight four source characteristics, including 1) access to medical expertise, 2) tailorability; 3) anonymity; and 4) convenience that influence utilization. Both the print materials and eHealth tool in these studies provided access and anonymity, while the print materials may have been more convenient (they were sent directly and required no additional steps) while the eHealth tool was tailored based on initial assessment questions and was self-guided.
More than 90% of participants in all three projects reported reading at least some or a little of the print materials, far surpassing self-reported use of V-CIS. This reminds us to not “throw out the baby with the bath water” in our use of eHealth tools. High quality, comprehensive print materials, such as those distributed by the NCI, are still valued and needed. In addition, these materials may have been more convenient since they were mailed directly and required no additional steps, where the eHealth tool required either installing the CD or logging into a website. Although self-reported use of V-CIS was less than the print materials, the majority of those in the experimental groups did report using the V-CIS and the majority of them reported using either the CD and web versions. Our findings suggest there may be differences as a function of gender, cancer site or where the patient is on the continuum from initial diagnosis to post-treatment survivorship and highlight the importance of understanding the information needs and preferences across the heterogeneous populations of cancer patients. Although the uptake of technology has changed rapidly in the past few years, these findings suggest that we need to understand more deeply why and how patients use a variety of resources in the process of making sense of their disease as well as making treatment and long-term management decisions. In addition, there is a need to more consistently and systematically connect patients to complementary channels of resources navigating them to richer and more comprehensive information.
5.1.3 Usage of V-CIS
The tracking sub-study for those who used the web-based version of the V-CIS was planned in the early stages of the research and was one of the early studies including tracking software to provide objective measures of use. For those who used the web-based V-CIS, the tracking data indicated that they spent between 20 to almost 40 minutes on their first login, and almost double that time in all visits to the site. The most highly accessed components of the V-CIS in all three projects, was the Library, followed by either the Doctor’s Office or Patient Stories. These were the modules with the most content regarding information about the disease, treatment options and supportive care, and they included both patient and provider videos. Both by self-report and actual usage, the Notebook (values clarification & action planning module) was used less. We recognized that a values clarification tool might be challenging; thus, we included a virtual guide in the software to explain the importance and process of using this module as well. However, patients used this module much less and these findings suggest that further research is needed to determine how to design values clarification and action planning tools to be both compelling and easy to use and the value of integrating eHealth tools with human health coaches. In addition, variations in subjective vs. objective use result are difficult to explain and future qualitative research could provide insights into this phenomena.
5.1.4 Limitations
There are limitations to the study. Participants were somewhat older and reported higher SES than the general population, and were information seekers since they were recruited predominately through existing cancer information services. In addition, participants were recruited from various organizations which might confound our results. Further, data collection on actual usage was only available for those participants who accessed the V-CIS on the web since there was no tracking software for the CD version. We only focused on short-term process evaluation using the 2-month data.
6.1 Conclusion
The results suggest that barriers to utilization remain, such as a lack of perceived need and technology issues, reminding us that not everyone will use eHealth tools or use them as intended. It is critical that patient education resources and support are provided through multiple communication channels and approaches and additional research on how the source characteristics (access, tailorability, anonymity and convenience), sequence of sources, and other personal characteristics (use of technology, age, health seeking behavior) impact utilization of information resources. It is also clear that objective usage data can provide insights into how these tools are used and what improvements would be needed for wide-scale dissemination. Although these tracking data can be challenging to collect and analyze, they provide important insights and ideally should be incorporated into all eHealth research (Fleisher et al., 2012).
The integration of traditional communication approaches with more innovative eHealth may be the ideal, especially for cancer patients who need to learn a great deal about their disease, are pressed for time and need to manage complex decisions about treatment choices and symptom management. Moreover, integrating eHealth tools, especially focused on decision making, into clinical practice may increase utilization while fostering opportunities for patient-provider communication. Additional research focused exploring the value and benefits of combining communication tools, especially with the complexity of decision making and self-management, from a patient-centered perspective would provide insights to augment current practice.
Acknowledgments
The project described is supported by NIH Grants 5-PO1-CA057596 and P30 CA006927 from the National Cancer Institute. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the National Cancer Institute, National Institutes of Health. In collaboration with the NCI’s Cancer Information Service (CIS) the research project and core resources support the work reported in this article are:
The Intervention Development and Measurement Core (PI: Suzanne M. Miller, PhD, Associate Director – Linda Fleisher, PhD, MPH, Kuang Yi Wen, PhD, Michael Diefenbach, PhD, and Mary Ropka, PhD), responsible for developing and producing study interventions, including the multimedia education programs, and for ensuring standardization and quality control of the intervention and assessment protocols across projects, as well as taking the lead on designing and producing the communication module reported here. The IDMC collaborated extensively with each of the CISRC Project Teams, CISRC Administrative Core and the National CIS Office.
Project 1 (PI: Michael Diefenbach, PhD) aimed at early stage prostate cancer patients who have not yet started treatment. Diefenbach and his team actively participated in the development of the VCIS through content development and review throughout the entire process.
Project 2 (PI: Peter Raich, MD), aimed at early stage breast cancer patients who have not yet started treatment. Dr. Raich and his team actively participated in the development of the VCIS through content development and review throughout the entire process.
Project 3 (PI: Annette Stanton, PhD), Pathways to Recovery after Breast Cancer Treatment, is aimed at CIS callers who will soon complete or have recently completed their primary treatments for breast cancer. Stanton and her team actively participated in the development of the VCIS through content development and review throughout the entire process.
The Administrative Core (PI: Al Marcus, PhD), responsible for providing scientific leadership and coordinating and facilitating all administrative aspects of the Cancer Information Service Research Consortium (CISRC).
We thank the CIS Project Office and Regional Staff for their commitment to helping patients and their content review and approval, and Fox Chase Cancer Center’s Psychosocial and Biobehavioral Medicine Department, Behavioral Research Core Facility, and Office of Health Communications and Health Disparities’ Resource Education Center for recruitment and assistance in usability testing. We thank Notsoldseparately, our technology partner who took our science and ideas and made it a reality through an exceptional collaborative and creative process, and the patients who shared their insights and stories throughout the development of these eHealth health tools as well as those who participated in the study.
We also want to acknowledge the friendship, leadership, and commitment to excellence that Dr. Alfred Marcus, retired PI of the CIS Research Consortium brought to this research. His collaborative approach among investigators, program leaders and patients served as an exemplar to all of us.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Linda Fleisher, Associate Research Professor - Adjunct, Cancer Prevention and Control, Fox Chase Cancer Center, 333 Cottman Avenue, Philadelphia, PA 19111 USA. Senior Scientist, Children’s Hospital of Philadelphia, USA, 3535 Market Street – Room 1177, Philadelphia, PA 19104 USA.
Kuang Yi Wen, Assistant Professor, Cancer Prevention and Control, Fox Chase Cancer Center, 333 Cottman Avenue, Philadelphia, PA 19111 USA.
Suzanne M. Miller, Director – Psychosocial and Behavioral Medicine Program, Professor – Cancer Prevention and Control Program, Fox Chase Cancer Center, 333 Cottman Avenue, Philadelphia, PA 19111 USA.
Michael Diefenbach, Associate Professor of Urology and Oncological Sciences, Director of Behavioral Research, Department of Urology, Mount Sinai School of Medicine, 1 Gustave L. Levy Place, New York, NY 10029 USA.
Annette L. Stanton, Professor, Departments of Psychology & Psychiatry/Biobehavioral Sciences, UCLA, Member, Jonsson Comprehensive Cancer Center, UCLA Cousins Center for Psychoneuroimmunology, 300 Medical Plaza Driveway, Los Angeles, CA 90095 USA.
Mary Ropka, Professor of Public Health Sciences, UVA School of Medicine, Blake Center · 1224 W. Main St., Suite 400B, P.O. Box 80082, Charlottesville, VA 22908-0821 USA.
Marion Morra, President, Morra Communications, 1 Platt Street, Milford, CT 06460 USA.
Peter C. Raich, Chief, Division of Hematology/Oncology, Denver Health and Hospitals, Professor of Medicine, Adjunct Professor of Psychology, University of Colorado Denver, 777 Bannock Street, MC1925, Denver, CO 80204 USA.
References
- CAYTON H. The flat-pack patient? Creating health together. Patient Educ Couns. 2006;62:288–90. doi: 10.1016/j.pec.2006.06.016. S0738-3991(06)00197-2 [pii] [DOI] [PubMed] [Google Scholar]
- DORFMAN CS, WILLIAMS RM, KASSAN EC, RED SN, DAWSON DL, TUONG W, PARKER ER, OHENE-FREMPONG J, DAVIS KM, KRIST AH, WOOLF SH, SCHWARTZ MD, FISHMAN MB, COLE C, TAYLOR KL. The development of a web- and a print-based decision aid for prostate cancer screening. BMC Med Inform Decis Mak. 2010;10 doi: 10.1186/1472-6947-10-12. 12.1472-6947-10-12 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- DUTTA-BERGMAN MJ. Complementarity in consumption of news types across traditional and new media. Journal of Broadcasting & Electronic Media. 2004;48:41–60. [Google Scholar]
- ELWYN G, FROSCH D, THOMSON R, JOSEPH-WILLIAMS N, LLOYD A, KINNERSLEY P, CORDING E, TOMSON D, DODD C, ROLLNICK S. Shared decision making: a model for clinical practice. Journal of general internal medicine. 2012;27:1361–1367. doi: 10.1007/s11606-012-2077-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ELWYN G, KREUWEL I, DURAND MA, SIVELL S, JOSEPH-WILLIAMS N, EVANS R, EDWARDS A. How to develop web-based decision support interventions for patients: a process map. Patient education and counseling. 2011;82:260–265. doi: 10.1016/j.pec.2010.04.034. [DOI] [PubMed] [Google Scholar]
- FLEISHER L, BUZAGLO J, COLLINS M, MILLARD J, MILLER SM, EGLESTON BL, SOLARINO N, TRINASTIC J, CEGALA DJ, BENSON AB. Using health communication best practices to develop a web-based provider–patient communication aid: The CONNECT™ study. Patient education and counseling. 2008;71:378–387. doi: 10.1016/j.pec.2008.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FLEISHER L, KANDADAI V, KEENAN E, MILLER SM, DEVARAJAN K, RUTH KJ, RODOLETZ M, BIEBER EJ, WEINBERG DS. Build it, and will they come? Unexpected findings from a study on a Web-based intervention to improve colorectal cancer screening. J Health Commun. 2012;17:41–53. doi: 10.1080/10810730.2011.571338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FLEISHER L, RUGGIERI DG, MILLER SM, MANNE S, ALBRECHT T, BUZAGLO J, COLLINS MA, KATZ M, KINZY TG, LIU T. Application of best practice approaches for designing decision support tools: the preparatory education about clinical trials (PRE-ACT) study. Patient education and counseling. 2014;96:63–71. doi: 10.1016/j.pec.2014.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HAWN C. Take two aspirin and tweet me in the morning: how Twitter, Facebook, and other social media are reshaping health care. Health Aff (Millwood) 2009;28:361–8. doi: 10.1377/hlthaff.28.2.361. 28/2/361 [pii] [DOI] [PubMed] [Google Scholar]
- HOLMES-ROVNER M. International Patient Decision Aid Standards (IPDAS): beyond decision aids to usual design of patient education materials. Health Expectations. 2007;10:103–107. doi: 10.1111/j.1369-7625.2007.00445.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- JOHNSON JD, MEISCHKE H. Differences in the evaluations of communication sources by women who have had a mammogram. Journal of Psychosocial Oncology. 1993;11:83–101. [Google Scholar]
- MARCUS AC, DIEFENBACH MA, STANTON AL, MILLER SM, FLEISHER L, RAICH PC, MORRA ME, PEROCCHIA RS, TRAN ZV, BRIGHT MA. Cancer patient and survivor research from the Cancer Information Service Research Consortium: a preview of three large randomized trials and initial lessons learned. Journal of health communication. 2013;18:543–562. doi: 10.1080/10810730.2012.743629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MILLER SM, BUZAGLO JS, SIMMS SL, GREEN V, BALES C, MANGAN CE, SEDLACEK TV. Monitoring styles in women at risk for cervical cancer: Implications for the framing of health-relevant messages. Annals of Behavioral Medicine. 1999;21:27–34. doi: 10.1007/BF02895030. [DOI] [PubMed] [Google Scholar]
- MILLER SM, DIEFENBACH MA. The cognitive-social health information processing (C-SHIP) model: a theoretical framework for research in behavioral oncology. Technology and methods in behavioral medicine. 1998:219–244. [Google Scholar]
- O’CONNOR AM, WENNBERG JE, LEGARE F, LLEWELLYN-THOMAS HA, MOULTON BW, SEPUCHA KR, SODANO AG, KING JS. Toward the ‘tipping point’: decision aids and informed patient choice. Health Aff (Millwood) 2007;26:716–25. doi: 10.1377/hlthaff.26.3.716. 26/3/716 [pii] [DOI] [PubMed] [Google Scholar]
- RAINS SA. Perceptions of traditional information sources and use of the world wide web to seek health information: findings from the health information national trends survey. J Health Commun. 2007;12:667–80. doi: 10.1080/10810730701619992. [DOI] [PubMed] [Google Scholar]
- RUPPEL EK, RAINS SA. Information Sources and the Health Information-Seeking Process: An Application and Extension of Channel Complementarity Theory. Communication Monographs. 2012;79:385–405. doi: 10.1080/03637751.2012.697627. [DOI] [Google Scholar]
- RYHÄNEN AM, SIEKKINEN M, RANKINEN S, KORVENRANTA H, LEINO-KILPI H. The effects of Internet or interactive computer-based patient education in the field of breast cancer: a systematic literature review. Patient education and counseling. 2010;79:5–13. doi: 10.1016/j.pec.2009.08.005. [DOI] [PubMed] [Google Scholar]
- SEPUCHA KR, FAGERLIN A, COUPER MP, LEVIN CA, SINGER E, ZIKMUND-FISHER BJ. How does feeling informed relate to being informed? The DECISIONS survey. Med Decis Making. 2010;30:77S–84S. doi: 10.1177/0272989X10379647. [DOI] [PubMed] [Google Scholar]
- STANTON AL. What happens now? Psychosocial care for cancer survivors after medical treatment completion. J Clin Oncol. 2012;30:1215–20. doi: 10.1200/JCO.2011.39.7406. [DOI] [PubMed] [Google Scholar]
- STANTON AL, MORRA ME, DIEFENBACH MA, MILLER SM, PEROCCHIA RS, RAICH PC, FLEISHER L, WEN KY, TRAN ZV, MOHAMED NE. Responding to a significant recruitment challenge within three nationwide psychoeducational trials for cancer patients. Journal of Cancer Survivorship. 2013;7:392–403. doi: 10.1007/s11764-013-0282-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TIWARI AK, ROY HK. Progress against cancer (1971–2011): how far have we come? J Intern Med. 2011;271:392–9. doi: 10.1111/j.1365-2796.2011.02462.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WEN KY, MILLER SM, STANTON AL, FLEISHER L, MORRA ME, JORGE A, DIEFENBACH MA, ROPKA ME, MARCUS AC. The development and preliminary testing of a multimedia patient–provider survivorship communication module for breast cancer survivors. Patient education and counseling. 2012;88:344–349. doi: 10.1016/j.pec.2012.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WILSON EA, MAKOUL G, BOJARSKI EA, BAILEY SC, WAITE KR, RAPP DN, BAKER DW, WOLF MS. Comparative analysis of print and multimedia health materials: a review of the literature. Patient education and counseling. 2012;89:7–14. doi: 10.1016/j.pec.2012.06.007. [DOI] [PubMed] [Google Scholar]
- ZICKUHR K, SMITH A. Pew Internet and American Life Project: Digital Differences. Pew Research Center; 2012. [Google Scholar]