Abstract
Context
The “Appropriate Medical Coverage for Intercollegiate Athletics” (AMCIA) document was created to support assessment and calculation of athletic training personnel requirements. However, little is known regarding disparities between current and recommended staffing practices.
Objective
To identify the staffing and employment characteristics of athletic health care services at Football Bowl Subdivision-level institutions.
Design
Cross-sectional study.
Setting
Web-based survey.
Patients or Other Participants
Head athletic trainers and athletic training staff members who were knowledgeable about budget and staff.
Main Outcome Measure(s)
The survey, Assessment of Staffing Levels at National Collegiate Athletic Association Football Bowl Subdivision-Level Institutions, was used to evaluate personal, university, and staff demographics; staffing and employment topics; and AMCIA variables and use.
Results
The survey was accessed and partially completed by 104 individuals (response rate = 84.6%). A total of 79 athletic trainers (response rate = 76%) completed the entire survey. One-third of the respondents (34.2%, n = 26) met the recommended number of full-time equivalents (FTEs) for football, two-thirds of the respondents (65.7%, n = 50) failed to meet the recommendation, and 26.2% (n = 27) were missing data needed for FTE calculation. Among those who did not meet the recommended FTEs (n = 50), 38.0% (n = 19) were within 1 FTE of being compliant, 26.0% (n = 13) were within 2 FTEs, and 24.0% (n = 12) were within 3 FTEs. About one-third of respondents (35.9%, n = 37) reported not using the AMCIA, citing lack of funding (29.7%, n = 11), lack of administrative support (21.6%, n = 8), and other reasons (37.8%, n = 14).
Conclusions
The majority of institutions that used the AMCIA were able to provide justification for staffing. For most of the institutions that failed to meet their recommendation, adding 1–3 FTE athletic trainers for football would change their compliance status. A uniform definition of the term FTE within collegiate athletics is needed to allow for structured assessment and allocation of staffing and workloads.
Key Words: burnout, work-life balance, staffing, full-time equivalent, medical coverage
Key Points
Most National Collegiate Athletic Association Football Bowl Subdivision-level institutions did not have an adequate number of full-time equivalent (FTE) athletic training personnel for football. Adding 1–3 FTEs would bring many of these institutions into compliance with the “Appropriate Medical Coverage for Intercollegiate Athletics” (AMCIA) recommendations. However, 1 athletic trainer is not equal to 1 FTE.
Institutions used the AMCIA guidelines inconsistently. Financial or administrative constraints were among the reasons cited for not using them.
The majority of those who have used the AMCIA attest that it helped them to justify current or proposed staffing quantities.
The profession needs to promote a standardized definition of FTE and a realistic valuation of the time and effort required to provide athletic training services.
Over the last 2 decades, participation in collegiate sports has consistently increased.1 In the 2012–2013 academic year, collegiate sport participation reached an all-time high, with more than 450 000 student-athletes competing in National Collegiate Athletic Association (NCAA) sports.1 Over 70 000 of those athletes participated in football, making it the largest NCAA sport by total athlete count,1 with 14 367 of those athletes participating in the Football Bowl Subdivision (FBS). The increase in collegiate athletes should be associated with increased medical personnel to ensure delivery of quality services.
In collegiate sports, it is common to have a collaborative health care team that includes athletic trainers (ATs), physical therapists, physicians, and physician assistants. However, these health care professionals are often in short supply in relation to the needs of the institution. Some variables that must be considered in determining an institution's need for athletic medical services are the number of athlete-exposures, number and types of sponsored athletic teams and athletes to be covered, overlap of seasons, length of seasons, and frequency and duration of practices, training sessions, and competitions.2 A mismatch between workload and number of personnel may have detrimental effects on members of the health care team.
Emerging research on the psychological syndrome burnout has identified this problem among ATs3–5 and has shown that too few personnel can cause ATs to develop emotional exhaustion, depersonalization, and a reduced feeling of personal accomplishment, all symptoms of burnout.3 Specifically, ATs who work with multiple sports3,6 and for long hours3,5 may be more prone to developing burnout symptoms, which may compromise the quality of care they provide to athletes.3 Inadequate staffing patterns and long, inflexible hours can also create conflicts when trying to balance professional and personal lives.7–9 Work-life conflict,10,11 role overload,11 and role strain10 have been cited as common reasons ATs leave the profession to pursue other avenues.
The National Athletic Trainers' Association (NATA) recognized the increasing demands on NCAA sports medicine programs and subsequent detrimental effects on the wellbeing of ATs and their ability to deliver a consistent level of care to athletes. This concern prompted the creation of the Task Force to Establish Appropriate Medical Coverage for Intercollegiate Athletics, which developed “Appropriate Medical Coverage for Intercollegiate Athletics” (AMCIA),2 a document that can be used to estimate the personnel resources required to provide appropriate medical care to athletes. The report operationalizes variables such as quantity of athlete-exposures, number and types of sponsored athletic teams and athletes, overlap of seasons, length of seasons, frequency and duration of activities, and ATs' administrative duties to provide “recommended athletic trainer full-time equivalents (FTEs).”2
The NATA noted that numerous athletic training services influence the health and wellbeing of student-athletes and that the provision of appropriate medical care extends beyond emergency care during athletic events.2 Appropriate medical care includes a variety of responsibilities, ranging from day-to-day operations to activities that occur without direct student-athlete contact. The aim of the AMCIA document was to allow institutions to quantify the athletic training personnel required to provide appropriate medical care, in all forms, including event coverage, organization of preparticipation examinations, development and implementation of injury-prevention programs, evaluation and treatment of injuries and illnesses, creation and direction of rehabilitation programs, administrative tasks, nutrition consultation, and maintenance of continuing education.2
Although the original AMCIA document was published more than 10 years ago,2 few researchers have investigated its use or whether institutions typically meet the FTE recommendations. Two dissertations addressing university compliance with the AMCIA recommendations were narrowly focused; 1 looked at universities in Indiana12 and the other at a single conference in the Football Championship Subdivision (FCS).13 Both authors found all institutions (n = 12 and n = 9, respectively) fell short of their minimum FTE recommendation.12,13 These studies had small sample sizes from very specific populations, but the findings establish a discrepancy between the NATA's recommendations for appropriate medical care and current employment characteristics of NCAA sports medicine programs.
The primary purpose of our study was to identify the staffing and employment characteristics of athletic health care services at FBS-level institutions. Specifically, our aim was to capture the FTE assignment practices of universities for football at the highest level within the NCAA and to determine if these FBS institutions met FTE recommendations for football as indicated by the AMCIA method.
METHODS
Instrumentation
Survey Development
The research team, which comprised 6 ATs, created a survey to assess the staffing and employment characteristics of FBS-level institutions. Along with general demographic information, the survey collected data regarding the AMCIA-specified variables to allow for calculation of each institution's recommended FTEs for football. The survey was meant to mimic the AMCIA by operationalizing institutional characteristics to produce a value for recommended AT FTEs. The completed instrument, Assessment of Staffing Levels at National Collegiate Athletic Association FBS-Level Institutions, consisted of 6 subsections: personal demographics, university demographics, staff demographics, staffing and employment, AMCIA variables, and AMCIA use. The survey was developed in Qualtrics Survey Software (Qualtrics Inc, Provo, UT) and included advanced logic and branching techniques that allowed participants to respond to specific questions that depended on their answers to previous questions. The survey structure included a variety of question styles, including binary items, multiple choice questions, Likert-scale items, and open-ended response fields. After development, we administered the survey as a pilot study to the NATA College/University Athletic Trainers' Committee. These individuals assessed the survey for face and content validity. The survey was deemed valid for assessment of FTE assignment and was finalized for national distribution.
Demographics (Personal, Institutional, Staff)
The demographic portion of the survey was divided into personal, institutional, and staff information. The personal demographics section provided a broad sketch of the participant's work experience and responsibilities by asking for years certified as an AT, degree, employment title, and whether the AT held any administrative responsibilities within the athletic department. The university demographics section included questions that determined the institution's general setting via geographic location, conference, and community size. This section also assessed the athletic training budget, number of student-athletes, and types of sports offered at the institution.
The staff demographics portion asked the participant to provide the number of full-time, part-time, graduate-assistant, and intern ATs employed at their institution. The number of ATs in each category assigned to football was also requested. In this section, we asked only how many ATs were assigned to football and did not address FTEs.
Staffing and Employment
In the staffing and employment section, the proportion of FTEs assigned to football at the respective institution was captured. An FTE was defined as the total number of regular straight-time hours (not including overtime or holiday hours) worked by employees, divided by the number of compensable hours in each fiscal year. One FTE is the equivalent of 1 person at full-time status, working 2080 hours per year.14 Participants were provided a standard, operational definition for FTE and asked whether the operational definition reflected what was used at their institution. This definition was used to uniformly identify the proportion of FTEs assigned to football for (a) full-time, (b) part-time, and (c) graduate-assistant/intern ATs, regardless of different institution definitions.
Appropriate Medical Coverage for Intercollegiate Athletics Variables
To calculate the total recommended FTEs for each institution, we asked participants to provide the size of their institution's 2013–2014 football roster, percentage of annual athletic training coverage and services for football, and number of travel days. Respondents were also asked to confirm the number of ATs assigned to football and identify each AT's portion of workload dedicated to administrative tasks and responsibilities outside of direct patient care associated with football.
Appropriate Medical Coverage for Intercollegiate Athletics Use
The last section of the survey assessed the institution's use of the AMCIA document. Participants were asked to indicate their reasoning for or against using the formula to determine staffing arrangements. Those who did not use the AMCIA formula were asked to identify what other resources, calculations, or factors they applied to determine staffing. For participants who did use the AMCIA document, follow-up questions allowed them to share whether the AMCIA was helpful, as well as provide insight into the outcome of its use.
Procedures
A distribution list of head ATs at FBS institutions was obtained from the NATA College/University Athletic Trainers' Committee. We chose FBS-level institutions for participation as this conference is considered the highest level within NCAA Division I athletics, with generally more athletic teams and greater event attendance; seemingly it is also the most likely to have sufficient finances to afford appropriate staffing quantities.15 An initial e-mail, which included the purpose of the study, statement of institutional review board approval, required time commitment, confirmation of participant confidentiality, and a hyperlink to access the survey, was sent to each e-mail address provided. The e-mail emphasized that an appropriate member of the athletic training staff who would have the best understanding of budget and staffing should complete the survey, with the intended respondent being the head AT or director of sports medicine. Participants were given 4 weeks to respond, and consent was implied by submission of the survey. On completion of the survey (indicated by clicking “submit”), an e-mail was sent to the participant to thank him or her for the time and willingness to complete the survey. Three follow-up reminder e-mails were sent weekly to participants who had not yet responded.
Data Analysis
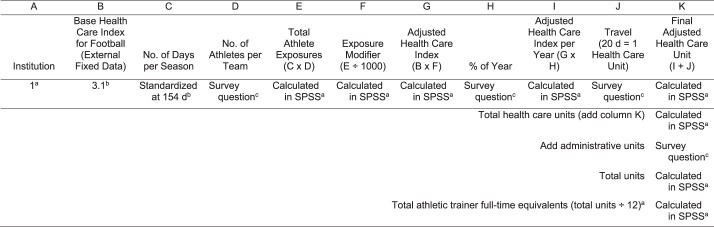
Descriptive statistical analyses were conducted using SPSS statistical software (version 21; IBM Corporation, Armonk, NY). Data are reported as mean ± standard deviation or count (%), as appropriate. To calculate total recommended FTEs for each institution, we coded the AMCIA formula in SPSS. In this equation, external fixed data were calculated with specific survey variables to result in a value for the number of recommended FTEs for football. The AMCIA calculation, with fixed variables, variables captured within the survey, and calculated variables, is depicted in Figure 1.2
Figure 1. .
Appropriate Medical Coverage for Intercollegiate Athletics calculation method. a Variable was calculated by the research team using SPSS (IBM Corporation, Armonk, NY). b Fixed variable. c Variable was captured within the survey.
The primary external fixed datum was the Base Health Care Index (HCI). The Base HCI is a value in the AMCIA document assigned to each sport based on injury-rate surveillance data2,16,17 and treatments per injury18 normalized on a scale of 0–4.2 A zero represents a low-risk/demand sport, and 4 represents a high-risk/demand sport.2 The Base HCI for football is 3.1.
Additional Health Care Units (HCUs) were added to the Base HCI for football to result in the final measurement of total HCUs.2 These HCUs were the number of athletes on the football roster, travel days, administrative duties, and percentage of annual athletic training coverage. Researchers discussed the standardization of the active participation days variable and concluded that due to low variance in active participation days at different institutions, it would be appropriate to standardize the quantity of active participation days per season at 154 days. The AMCIA document stated that it was reasonable for 1 full-time AT to be responsible for 12 HCUs.2 Thus, in the calculation, the aggregate number of HCUs was divided by 12 to calculate the total recommended AT FTEs for each institution, specific to the sport of football at the FBS level. Descriptive analyses are provided for the derived variable, total recommended FTEs. We calculated a Wilcoxon signed rank test to determine if statistical differences existed between recommended and actual FTEs. A cross-tabulation between FBS conference and AMCIA-recommended FTEs was also conducted.
RESULTS
Respondents
A total of 123 ATs were contacted in the initial e-mail distribution. The survey was accessed by 104 individuals, representing 104 separate institutions (response rate = 84.6%). A total of 79 of the 104 ATs (response rate = 76%) completed all parts of the survey. Regardless of partial or full survey completion, 26.0% (n = 27/104) of respondents had missing or invalid data that limited the calculation and comparison of FTEs, and 1 respondent who accessed the survey did not answer any of the questions. Certain data were excluded from the analyses due to incorrect or incomplete entries.
Personal AT Demographics
Male ATs accounted for 90.3% (n = 93) of the respondents, whereas only 9.7% (n = 10) were females. Their average age was 47.6 ± 8.2 years (range, 32–68 years). The majority of participants (93.2%, n = 96) had completed a master's degree, 4.9% (n = 5) had a 4-year college degree, and 2.0% (n = 2) held a clinical (eg, Doctor of Physical Therapy [DPT]) or research (eg, Doctor of Philosophy [PhD]) doctoral degree. Respondents reported being certified as ATs for 25.5 ± 7.8 years (range, 12–43 years) and employed in their current position for 13.8 ± 10.3 years (range, 1–40 years).
Most participants (94.2%, n = 97) held administrative responsibilities within the athletic department at their institutions. The most common job titles for respondents were Director of Athletic Training/Sports Medicine (58%, n = 53), followed by Head Athletic Trainer (43%, n = 40), Associate Athletic Director (20%, n = 18), and Assistant Athletic Director (15%, n = 14). Almost one-third (31.1%, n = 32) reported having multiple job titles. Among these, the most common dual assignments were Director of Athletic Training/Sports Medicine and Head Athletic Trainer (21.9%, n = 7) and a combination role of Director of Athletic Training/Sports Medicine, Head Athletic Trainer, and Associate Athletic Director (21.9%, n = 7).
Institutional Demographics
Participants represented 40 states and all 10 FBS conferences (Table 1). The institution was located in a small to medium city (26 000–300 000) for 43.7% (n = 45) of respondents, a large city (>300 000) for 36.9% (n = 38), and small urban or rural community (<25 000) for 8.7% (n = 9). No institutional demographic information was provided by 10.7% (n = 11) of respondents. A total of 67% (n = 69) indicated that their facility serves as a clinical site for professional athletic training students. The strength coaches at the respondents' institutions most often reported to an assistant or associate athletic director (64.1%, n = 66), followed by the head coach (32%, n = 33), head AT (10.7%, n = 11), athletic director (7.8%, n = 8), and team physician (1.9%, n = 2); 13.6% (n = 14) did not respond. Participants reported 549.5 ± 395.0 student-athletes and 26 800.4 ± 13 117.1 students enrolled at their institutions. The majority of respondents (79.3%, n = 73) indicated their total athletic training and sports medicine budget was greater than $500 000, with 9.7% (n = 9) between $400 000 and $500 000, 6.5% (n = 6) between $300 000 and $400 000; 4.4% (n = 4) reported a budget less than $300 000; and 10% (n = 11) did not answer the question. The percentage of the total budget spent in 5 subbudget categories is presented in Table 2. Of the total budget, staffing decisions were affected primarily by 4 of 6 subbudget categories: staff (51.5%, n = 53), followed by other (19.4%, n = 20), medical (7.8%, n = 8), and operational (6.8%, n = 7).
Table 1. .
Conference Affiliations of Respondents
| Conference |
Respondents |
| Frequency (%) | |
| American Athletic | 9 (8.7) |
| Atlantic Coast | 12 (11.7) |
| Big 12 | 9 (8.7) |
| Big 10 | 11 (10.7) |
| Conference USA | 11 (10.7) |
| Mid-American | 9 (8.7) |
| Mountain West | 10 (9.7) |
| Pacific 12 | 8 (7.8) |
| Southeastern | 7 (6.8) |
| Sun Belt | 6 (5.8) |
| No response | 11 (10.7) |
Table 2. .
Budget Subcategories Expressed as a Percentage of the Total Budget (n = 92)
| Subbudget Category |
Mean ± SD |
Range |
| Insurance | 13.9 ± 14.0 | 0–55 |
| Medical | 18.6 ± 13.5 | 0–66 |
| Operational | 12.3 ± 9.4 | 0–50 |
| Staff | 39.0 ± 17.6 | 0–82 |
| Supplies | 16.2 ± 8.8 | 5–60 |
Staffing Demographics
On average, athletic training staffs consisted of 9.4 ± 3.7 full-time (nongraduate assistant/nonintern) ATs (range, 3–20), ranging in age from 23–68 years old (average age = 34.6 ± 7.4 years). Collectively, a higher proportion of male full-time ATs (60.5%, n = 470) were on staff than female full-time ATs (39.5%, n = 307). The majority of full-time ATs on staff had completed a master's degree (91%, n = 709), whereas 6% (n = 46) held a doctoral degree, and 3% (n = 24) held a bachelor's degree. There were 2.4 ± 0.9 full-time ATs, 0.2 ± 0.5 part-time ATs, 1.2 ± 1.0 graduate-assistant ATs, 0.3 ± 0.5 intern ATs, and 7.4 ± 3.9 undergraduate athletic training students working football per season. The number of total athletic training staff and the number assigned to football by job title are provided in Table 3.
Table 3. .
Overall Staffing Data for Athletic Trainers (ATs), No.
| Position Type |
Mean ± SD |
Range |
| On staff | ||
| Full-time ATs | 9.4 ± 3.7 | 3–20 |
| Part-time ATs | 0.7 ± 1.6 | 0–9 |
| Graduate-assistant ATs | 5.1 ± 3.4 | 0–16 |
| Paid intern ATs | 0.9 ± 1.8 | 0–8 |
| Full-time equipment managers | 5.3 ± 6.4 | 0–58 |
| Full-time strength coaches | 6.2 ± 2.8 | 2–14 |
| Physicians | 2.9 ± 3.6 | 0–22 |
| Persons assigned to football | ||
| Full-time ATs | 2.4 ± 0.9 | 0–5 |
| Part-time ATs | 0.2 ± 0.5 | 0–3 |
| Graduate assistant ATs | 1.2 ± 1.0 | 0–5 |
| Paid intern ATs | 0.3 ± 0.5 | 0–3 |
| Athletic training students | 7.4 ± 3.9 | 0–20 |
Appropriate Medical Care
A large proportion of respondents (41.7%, n = 43) agreed that the standard definition of an FTE accurately reflected the way in which their university requires the athletic training staff to determine FTEs, with 27.1% (n = 28) disagreeing, 17.5% (n = 18) not knowing, and 13.6% (n = 14) not responding.
The AMCIA Calculations for Football
Participants reported an average of 114.9 ± 13.8 athletes on the football roster at the beginning of the 2013–2014 season. Only 36% of respondents (n = 29) agreed with the AMCIA document assumption that ATs provide coverage for a given sport for 50% of the year.2 The majority of respondents disagreed; 59.4% (n = 47) stated the coverage percentage was greater than 50%. Of those indicating coverage of greater than 50% of the year, nearly all noted that ATs provided coverage and services for football for more than 80% of the year (91.5%, n = 43). Participants estimated that the football team travelled 15.7 ± 5.5 days during the 2013–2014 season (range, 5–32 days) and 14.7 ± 5.0 days in the 2012–2013 season (range, 0–30 days). Typically, 4.1 ± 1.4 (range, 2–9) ATs accompanied the football team on a regular season trip, and 4.4 ± 1.5 (range, 2–10) accompanied the football team on a postseason trip.
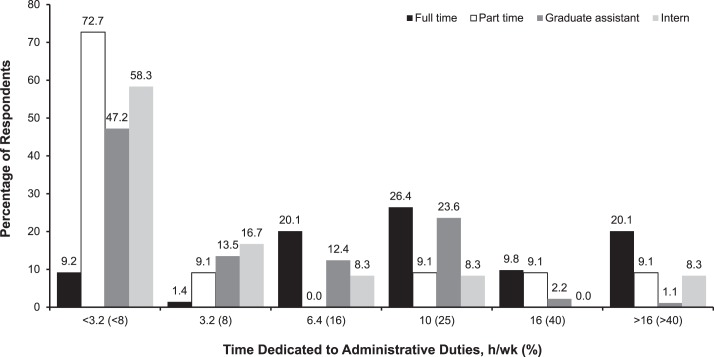
Respondents were asked to report administrative tasks and responsibilities (outside of direct patient care associated with football) for all ATs (Figure 2). The percentage of administrative duties was converted to HCUs. For the majority of full-time ATs (26.4%, n = 46), administrative duties accounted for 25% of their workload, equating to 3 HCUs. Respondents reported that 20.1% (n = 35) of full-time staff had administrative duties that exceeded 40% of the AT's workload (>5 HCUs) and that 20.1% (n = 35) of full-time staff had administrative workloads of 16% (2 HCUs). For part-time athletic training staff, administrative duties most commonly accounted for less than 8% (<1 HCU) of the AT's workload (72.7%, n = 8). Many graduate assistants (47.2%, n = 42) had administrative duties that accounted for less than 8% (<1 HCU) of their total workload. Almost one-quarter of graduate assistants (23.6%, n = 21) had administrative duties that accounted for 25% (3 HCUs) of their workload. Interns typically had the smallest portion of administrative duties, with 58.3% (n = 14) having less than 8% (<1 HCU).
Figure 2. .
Staff administrative duties.
Regarding recommended FTEs versus actual FTEs specific to football, 76 respondents provided the data to allow calculation and comparison. In assessing the number of personnel, regardless of their FTE assignment, we found that an average of 4.0 ± 1.1 ATs were assigned to football (range, 1.5–7.0 ATs). Calculation of AMCIA variables revealed that the average number of FTEs recommended for football was 4.1 ± 1.2 (range, 2.2–7.8 FTEs). The average number of FTEs assigned to football was 3.4 ± 1.3 (range, 0.0–6.8 FTEs), less than what was recommended. These differences were significant (P = .001, 2 tailed). Only one-third of respondents (34.2%, n = 26) met or exceeded the AMCIA-recommended number of FTEs for football. Close to two-thirds (65.8%, n = 50) fell short or failed to meet the recommendation, and 26.0% (n = 27) were missing data to calculate compliance. Among those who did not meet the minimum recommended FTEs for football (n = 50), 38.0% (n = 19) were within 1 FTE of being compliant, 26.0% (n = 13) were within 2 FTEs, and 24.0% (n = 12) were within 3 FTEs. A small percentage of respondents had larger deficits, with 8.0% (n = 4) needing 4 FTEs for compliance and 4.0% (n = 2) needing 5 FTEs. The cross-tabulations of FBS conference with FTE compliance are presented in Table 4.
Table 4. .
Compliance With Appropriate Medical Coverage for Intercollegiate Athletics (AMCIA) by Football Bowl Subdivision Conference
| Football Bowl Subdivision Conference |
No. of Respondents |
Schools Not Meeting AMCIA Full-Time Equivalent Requirements, No. (%) |
| American Athletic | 9 | 6 (66.7) |
| Atlantic Coast | 8 | 4 (50.0) |
| Big 12 | 8 | 2 (25.0) |
| Big 10 | 9 | 6 (66.7) |
| Conference USA | 9 | 5 (55.6) |
| Mid-American | 9 | 9 (100.0) |
| Mountain West | 9 | 7 (77.8) |
| Pacific 12 | 6 | 6 (100.0) |
| Southeastern | 5 | 2 (40.0) |
| Sun Belt | 4 | 3 (75.0) |
| Total | 76 | 50 (65.8) |
Use of the AMCIA Document
Just over 40% (n = 42) of respondents had used the AMCIA document to determine athletic training staff size. Participants who used the AMCIA did so to increase staffing (88.1%, n = 37), as an internal audit (38.1%, n = 16), out of curiosity (64.3%, n = 27), to enhance facilities (14.3%, n = 6), or for other reasons (11.9%, n = 5). When asked if they were successful in using AMCIA, 62% (n = 26) of participants agreed. Of those who had not used the AMCIA (35.9%, n = 37), 10 (27.0%) indicated that they were not familiar with the document (27.0%, n = 10), that the effort would be futile due to lack of funding (21.6%, n = 8), that the effort would be futile due to lack of administrative support (21.6%, n = 8), or other reasons (37.8%, n = 14). A smaller proportion replied that they either did not understand the AMCIA or found the methods too difficult to use (8.1%, n = 3) or that they lacked time to complete it (8.1%, n = 3).
DISCUSSION
Our findings suggest that, in comparison with the recommendations of the current version of the AMCIA document,2 only one-third of the NCAA FBS institutions that provided enough information in the survey to calculate AMCIA recommendations had adequate AT staffing for football, and about two-thirds did not. Those without adequate staffing to provide appropriate medical coverage and athletic training services, given the AMCIA guidelines, were typically short 1–3 FTEs by these criteria, although a small percentage fell short by 4–5 FTEs.
Full-Time Equivalent
Because the standard definition for and characteristics of the term FTE vary among responding institutions, the resulting variability and, in some cases, considerable confusion can make the use of a standardized tool such as the AMCIA challenging. The AMCIA document uses full-time AT equivalents for its calculations and assumes that institutions apply a common metric to that descriptor.2 Although many survey respondents agreed with the standard definition, several disagreed or did not know how their institution defined FTE.
Some participants may have used the designation of AT interchangeably with the term FTE. This is problematic, especially when an AT has an assignment outside of athletics. As an example, if one full-time AT worked half time in student health and half time in athletics with football, it would not be accurate to equate this individual to 1 AT assigned to football. More accurately, this individual was 0.5 FTE assigned to football. Understanding this difference may improve the effectiveness of the AMCIA document in proposals for increased staffing.
Even if users are able to discriminate between an AT and an FTE, defining an FTE within the field of athletic training can be difficult. In our survey, we defined an FTE as 1 individual working full time, 2080 hours annually; that is, working 8 hours per day, 5 days per week, 52 weeks per year. Historically for athletic training, administrators have not emphasized or been motivated to calculate FTEs. However, beginning to do so is critical in adequately capturing workloads and schedule fluctuations across the year to ensure consistency with other university employees. Long hours and long workweeks are not foreign to those working in the field of athletic training,3,7,11,19–22 and unfortunately, neither is a work environment in which AT responsibilities extend beyond the standard definition of 1 FTE.7,11,19–22 For an AT working in the NCAA Division I setting, an average weekly workload may range from 45 hours during off-season,7,20 to 60+ hours in-season.7,11,20,22 The use of FTEs needs to be emphasized, and we should explore the interpretation and allocation of FTEs in the field of athletic training.
To address the increased demands on athletic training staffs, we must focus on the multitude of duties an AT has and how an FTE is distributed. Collegiate ATs can experience overload when faced with the difficulties of meeting the obligations for multiple work roles.23,24 With directives beyond sport assignment, ATs may be responsible for a workload beyond that of 1 FTE. It is imperative to assess and frame responsibilities in terms of FTEs to identify imbalances and increase the likelihood of gaining administrator understanding and support for staffing changes.
Currently, it may be commonplace to assume that the workload of 1 AT assigned to a sport consists only of event coverage, evaluation, diagnosis, and immediate and emergency care. However, both the NATA and NCAA note that, in addition to customary medical services, ATs are responsible for numerous duties relating to risk minimization, organization and administration, and academics.2,25 In providing athletic training services for a football team, an AT may be reasonably expected to create injury-prevention programs, inspect facilities, review preparticipation examinations, review and rehearse emergency action plans, conduct functional movement assessments, provide nutrition consultations, select and fit protective equipment, search and appraise evidence-based research, educate athletes and coaches on relevant sports medicine information, and document all of these. Even if these responsibilities fall under the health care services workload captured by the AMCIA, the list of responsibilities is significant.
Outside of routine sport assignment duties, an AT's FTE may be further divided to allow him or her to teach, instruct athletic training students, or attend to administrative duties. Athletic trainers with a large proportion of administrative duties may need to spend some of their time hosting department meetings, scheduling staff members, managing insurance claims, ensuring facility safety and adherence to regulations, managing the facility's inventory, monitoring the renewal of staff credentials, drug testing, or budgeting. Many ATs serving as clinical preceptors face role strain.24 In addition to their regular work assignments, they must also allocate time to supervise students, assess proficiencies, and provide guidance and education.
Effect of the AMCIA Document
The AMCIA document was established more than a decade ago2 and has been used as a tool by institutions seeking to increase AT staffing in recent years.26 Among the institutions that have used it, most have successfully provided justification for current staffing numbers or the need to increase staff. However, those that have not used it argue that they are unfamiliar with the tool or lack funding or administrative support.
Currently, the NATA maintains a Web page (http://www.nata.org/appropriate-medical-coverage-intercollegiate-athletics/) that provides a link to not only the AMCIA document but also access to an online worksheet, answers to frequently asked questions, and contact information for almost 2 dozen mentors who will provide assistance to those wanting to use the AMCIA.27 The Web site supplies sufficient information to introduce the AMCIA to ATs who are unfamiliar with the document.
To overcome the lack of funding needed for staffing increases, modifications may be made to the way a sports medicine or general athletic department budget is allocated or prioritized. However, if an athletic training department does not have influence over its staffing budget (staffing being covered by the general athletic or administrative budget), making adjustments may be difficult. In his assessment of AMCIA compliance within a single FCS conference, Obray13 suggested that third-party reimbursement should be explored as a way of generating revenue to fund adequate athletic training staff. With the recent push for ATs to apply for a National Provider Identifier, recognizing ATs as reimbursable entities may become a viable option.
To determine if lack of funding is an obstacle to meeting AMCIA recommendations, it will be necessary to assess the correlation between respondent budgets and AMCIA compliance. Unfortunately, the upper budget limits in this survey were not set high enough to detect disparities among institutions. The budget category greater than 500k was the highest financial bracket provided, so we were unable to capture upper-limit budget differences. A better breakdown of total athletic training budgets might have demonstrated if and how budget size may affect AMCIA compliance.
Addressing the failure to understand the AMCIA as an impediment may require focused, integrative education aimed at administrative groups. It is possible that the only time administrators hear about AMCIA calculations and recommendations is when an AT introduces those concepts, likely in conjunction with a request for increased staffing, resources, or finances. Introducing administrative groups to the AMCIA and its components requires not only information dissemination but also reiteration of AMCIA endorsement by the NATA and the NCAA. In its 2013–14 NCAA Sports Medicine Handbook,25 the NCAA recommended a systematic approach to assessing an institution's medical staffing needs. To gain administrative “buy-in,” it may be advantageous to seek support from the university risk management department and well-known groups such as the US Department of Labor or athletic conference offices.
According to our findings, some respondents perceived administrative opposition to increasing athletic training staffing. However, if administrators or institutions were provided with a reasonable staffing goal increase and a reasonable timeline, they might be more supportive of proposed changes. Most institutions that fell short were within 1–3 FTEs of being compliant with AMCIA recommendations. Proposing to offset a deficit of 1 FTE by hiring additional staff might be attainable within 1 year for some institutions. However, for the institutions that were short 2–3 FTEs and for the small percentage short by 4–5 FTEs, hiring additional staff may be a long-term process, to be completed over several years. For these institutions, it may be beneficial to evaluate and redistribute workload within the athletic department, perhaps even by decreasing the number of coaches or administrators to allow for the hiring of an AT to meet the appropriate number of FTEs.
Limitations and Future Research
We specifically targeted the NCAA Division I FBS, as we believed that this level of competition would most likely have the resources available to support adequate staffing of athletic training personnel. Although we compared actual and recommended FTEs for institutions within the NCAA FBS, the data were specific to football. In a similar study, Obray13 found that all sports in 9 institutions were below their recommendation by an average of 3.6 ATs. If we had evaluated institutions as a whole, even more might have fallen short and by a larger FTE deficit. A greater amount of time and effort would be required to assess each sport, but the resulting data would more clearly depict the extent of staffing and care or coverage discrepancies in collegiate sports medicine.
One benefit of assessing institutions within the FBS is that the subdivision is considered the highest level of competition within the NCAA.15 By looking at schools that offer more sports and have higher event attendance, we hoped to assess staffing among institutions that would have ample finances to afford an appropriate number of athletic training FTEs. However, assessing only FBS institutions produced results that are generalizable only to that group. Future authors should compare institutions within the FCS, Division II, or Division III to truly represent the scale of staffing concerns within the NCAA and with modifications to the AMCIA formula to account for the current practice and training climate of FBS football.
Additionally, researchers should evaluate how AMCIA mentors are used. Currently, mentors are listed on the NATA Web site, but not much is known about whether mentors are given standardized training in how to guide those who request their advice or in what capacity mentors serve users. If mentors are found to clarify calculation accuracy, the AMCIA might need to be updated with more clear or interactive instructions, eg, Web-based video. If users ask mentors for advice on how to speak to administrators with a request for increased staffing, that may support the need to host role-playing opportunities or provide sample scripts or video scenarios for ATs.
Lastly, future investigators should focus on assessing the effect of the AMCIA on different factors. Evaluating attrition or burnout in ATs at institutions that meet or do not meet their recommended FTEs may help to support staffing needs. Additionally, comparing economic estimates of athletic training services before and after using the AMCIA may provide ATs with quantifiable examples to aid in conversations with administrators about whether having the appropriate number of FTEs results in better medical care and patient outcomes.
CONCLUSIONS
The majority of institutions in the FBS did not have an adequate number of FTEs allotted to football. To further determine the adequacy of AT staffing, all sports need to be incorporated into the AMCIA calculation. Unfortunately, the AMCIA document is used only marginally, mostly because ATs feel resistance from financial or administrative constraints. Efforts need to be made to ease resistance, starting with equipping ATs with accurate definitions for terms such as FTE and instilling knowledge and confidence so that ATs can successfully discuss staffing issues. Individually, and as a profession, we need to realistically assess the time and effort required to provide athletic training services. By recognizing how and where an AT's energies are spent, we can better illustrate our profession's worth and gain support from administrators when seeking to raise the bar for appropriate medical care.
REFERENCES
- 1.1981–1982—2012–13: NCAA sports sponsorship and participation rates report. National Collegiate Athletic Association Web site 2015 . http://www.ncaapublications.com/productdownloads/PR2014.pdf. Accessed August 7, [Google Scholar]
- 2.Recommendations and guidelines for appropriate medical coverage of intercollegiate athletics. The National Athletic Trainers' Association Web site 2015 . http://www.nata.org/sites/default/files/AMCIA-Revised-2010.pdf. Accessed August 7, [Google Scholar]
- 3.Kania ML, Meyer BB, Ebersole KT. Personal and environmental characteristics predicting burnout among certified athletic trainers at National Collegiate Athletic Association institutions. J Athl Train. 2009;44(1):58–66. doi: 10.4085/1062-6050-44.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Giacobbi PR. Low burnout and high engagement levels in athletic trainers: results of a nationwide random sample. J Athl Train. 2009;44(4):370–377. doi: 10.4085/1062-6050-44.4.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mazerolle SM, Monsma E, Dixon C, Mensch J. An assessment of burnout in graduate assistant certified athletic trainers. J Athl Train. 2012;47(3):320–328. doi: 10.4085/1062-6050-47.3.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hendrix AE, Acevedo EO, Hebert E. An examination of stress and burnout in certified athletic trainers at Division I-A universities. J Athl Train. 2000;35(2):139–144. [PMC free article] [PubMed] [Google Scholar]
- 7.Mazerolle SM, Bruening JE, Casa DJ. Work-family conflict, part I: antecedents of work-family conflict in National Collegiate Athletic Association Division I-A certified athletic trainers. J Athl Train. 2008;43(5):505–512. doi: 10.4085/1062-6050-43.5.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mazerolle SM, Bruening JE, Casa DJ, Burton LJ. Work-family conflict, part II: job and life satisfaction in National Collegiate Athletic Association Division I-A certified athletic trainers. J Athl Train. 2008;43(5):513–522. doi: 10.4085/1062-6050-43.5.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mazerolle SM, Bruening JE. Sources of work-family conflict among certified athletic trainers, part 1. Athl Ther Today. 2006;11(5):33–35. [Google Scholar]
- 10.Goodman A, Mensch JM, Jay M, French KE, Mitchell MF, Fritz SL. Retention and attrition factors for female certified athletic trainers in the National Collegiate Athletic Association Division I Football Bowl Subdivision setting. J Athl Train. 2010;45(3):287–298. doi: 10.4085/1062-6050-45.3.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mazerolle SM, Pitney WA, Goodman A, Caswell S. Factors influencing the decisions of male athletic trainers to leave the NCAA Division-I practice setting. Int J Athl Ther Train. 2013;18(6):7–12. [Google Scholar]
- 12.Hackman K. Determination of Compliance with NATA Recommendations for Care of Intercollegiate Athletes Among Higher Education Institutions in the State of Indiana [dissertation] Muncie, IN: Ball State University;; 2007. [Google Scholar]
- 13.Obray G. Compliance with the National Athletic Trainers' Association's Recommendations and Guidelines for Appropriate Medical Coverage of Intercollegiate Athletics in a Football Championship Subdivision Conference [dissertation] Pocatello: Idaho State University;; 2010. [Google Scholar]
- 14.Circular No. A-11. Section 85: estimating employment levels and the employment summary (Schedule Q) Executive Office of the President—Office of Management and Budget Web site 2015 . https://www.whitehouse.gov/sites/default/files/omb/assets/a11_current_year/a11_2013.pdf. Accessed August 7, [Google Scholar]
- 15.Divisional differences and the history of multidivision classification. National Collegiate Athletic Association Web site. 2015 http://www.ncaa.org/about/who-we-are/membership/divisional-differences-and-history-multidivision-classification. Accessed August 7. [Google Scholar]
- 16.Dick R, Ferrara MS, Agel J, et al. Descriptive epidemiology of collegiate men's football injuries: National Collegiate Athletic Association Injury Surveillance System, 1988–1989 through 2003–2004. J Athl Train. 2007;42(2):221–233. [PMC free article] [PubMed] [Google Scholar]
- 17.Albright JP, Powell JW, Martindale A, et al. Injury patterns in big ten conference football. Am J Sports Med. 2004;32(6):1394–1404. doi: 10.1177/0363546504264159. [DOI] [PubMed] [Google Scholar]
- 18.Powell JW, Dompier TP. Analysis of injury rates and treatment patterns for time-loss and non-time-loss injuries among collegiate student-athletes. J Athl Train. 2004;39(1):56–70. [PMC free article] [PubMed] [Google Scholar]
- 19.Naugle KE, Behar-Horenstein LS, Dodd VJ, Tillman MD, Borsa PA. Perceptions of wellness and burnout among certified athletic trainers: sex differences. J Athl Train. 2013;48(3):424–430. doi: 10.4085/1062-6050-48.2.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mazerolle SM, Faghri P, Marcinick M, Milazzo S. Athletic trainers' workload in NCAA Division I athletic programs. Athl Ther Today. 2010;15(3):34–37. [Google Scholar]
- 21.Pitney WA, Mazerolle SM, Pagnotta KD. Work-family conflict among athletic trainers in the secondary school setting. J Athl Train. 2011;46(2):185–193. doi: 10.4085/1062-6050-46.2.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mazerolle SM, Goodman A, Pitney WA. Factors influencing retention of male athletic trainers in the NCAA Division I setting. Int J Athl Ther Train. 2013;18(5):6–9. [Google Scholar]
- 23.Brumels K, Beach A. Professional role complexity and job satisfaction of collegiate certified athletic trainers. J Athl Train. 2008;43(4):373–378. doi: 10.4085/1062-6050-43.4.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Henning JM, Weidner T. Role strain in collegiate athletic training approved clinical instructors. J Athl Train. 2008;43(3):275–283. doi: 10.4085/1062-6050-43.3.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.2013–14 NCAA sports medicine handbook. National Collegiate Athletic Association Web site 2015 . http://www.ncaapublications.com/productdownloads/MD14.pdf. Accessed August 7, [Google Scholar]
- 26.AMCIA Mentors. The National Athletic Trainers' Association Web site. 2015 http://www.nata.org/appropriate-medical-coverage-intercollegiate-athletics/mentors. Accessed August 7. [Google Scholar]
- 27.Appropriate medical coverage of intercollegiate athletics. The National Athletic Trainers' Association Web site 2015 . http://www.nata.org/appropriate-medical-coverage-intercollegiate-athletics. Accessed August 7, [Google Scholar]