Abstract
Allergic rhinitis is a global illness with a well-recognised impact on quality of life and work performance. Comparatively little is known about the extent of its economic impact on society. The TOTALL study estimates the total cost of allergic rhinitis using a sample representing the entire Swedish population of working age. A questionnaire focused on allergic rhinitis was mailed out to a random population of Swedish residents, aged 18–65 years. Health-care contacts, medications, absenteeism (absence from work) and presenteeism (reduced working capacity at work) were assessed, and the direct and indirect costs of allergic rhinitis were calculated. Medication use was evaluated in relation to the ARIA guidelines. In all, 3,501 of 8,001 (44%) answered the questionnaire, and 855 (24%) of these reported allergic rhinitis. The mean annual direct and indirect costs because of allergic rhinitis were €210.3 and €750.8, respectively, resulting in a total cost of €961.1 per individual/year. Presenteeism represented 70% of the total cost. Antihistamines appear to be used in excess in relation to topical steroids, and the use of nasal decongestants was alarmingly high. The total cost of allergic rhinitis in Sweden, with a population of 9.5 million, was estimated at €1.3 billion annually. These unexpectedly high costs could be related to the high prevalence of disease, in combination with the previously often underestimated indirect costs. Improved adherence to guidelines might ease the economic burden on society.
Introduction
Allergic rhinitis is a global health problem that causes major disability worldwide, characterised by nasal obstruction, secretion and itching. It is often associated with eye symptoms, fatigue and asthma.1 The impact of allergic rhinitis on quality of life, work and school performances is well recognised. Its economic effects are therefore potentially substantial. Attempts to estimate the costs of allergic rhinitis were made 20–30 years ago in the USA,2,3 but more comprehensive endeavours in the area are still lacking.4,5 The societal costs of a disease are commonly described as direct and indirect costs. The former are instigated by health-care visits, use of medication and hospitalisation, whereas the latter are related to absence from work (absenteeism) and reduced working capacity at work (presenteeism). We have recently estimated the annual indirect cost of all forms of rhinitis, allergic, non-allergic and infectious (common cold) in Sweden at €2.7 billion a year.6 The aim of the present study, TOTALL (TOTal costs of ALLergic rhinitis in Sweden), was to calculate both the direct and the indirect costs of allergic rhinitis in the Swedish working population. In addition, the reported use of pharmacological treatment was contrasted with the current international ARIA guidelines.1
Results
Sample characteristics
The response rate was 44% (3,501 of 8,001). The respondents were slightly older than the study population, 47±12.7 vs. 43±13.2 years, and the response rate was somewhat higher among women than in men (49% vs. 39%). Baseline data including age, gender, smoking habits and employment are presented in Table 1. Eight hundred and fifty-five participants were classified as suffering from self-reported allergic rhinitis, giving a prevalence of 24%. Doctor-diagnosed asthma was reported by 9% of the whole target population and by 22% of the participants with self-reported allergic rhinitis. Additional eye symptoms interpreted as rhinoconjunctivitis were reported by 19% of the total responding population.
Table 1. Baseline characteristics for the study population and the sub-population with self-reported allergic rhinitis.
|
Total population
|
Self-reported allergic rhinitis
|
|||
|---|---|---|---|---|
| N | % | N | % | |
| Female | 1,898 | 54.2 | 481 | 56.3 |
| Male | 1,592 | 45.5 | 371 | 43.4 |
| Missing or no answer | 11 | 0.3 | 3 | 0.4 |
| Total | 3,501 | 100 | 855 | 100 |
|
Present employment
a
| ||||
| Full-time employment | 2,150 | 61 | 554 | 64.8 |
| Part-time employment | 616 | 18 | 144 | 16.8 |
| Full-time student | 174 | 5 | 49 | 5.7 |
| Part-time student | 42 | 1 | 11 | 1.3 |
| Other working situation | 621 | 18 | 135 | 15.8 |
| Missing or no answer | 35 | 1 | 2 | 0.2 |
|
Smoking/day
| ||||
| Yes, daily, >1 package | 24 | 0.7 | 3 | 0.4 |
| Yes, daily, ~1 package | 78 | 2 | 16 | 1.9 |
| Yes, daily, <1 package | 286 | 8 | 46 | 5.4 |
| Former smoker | 1,002 | 29 | 222 | 26.0 |
| Never smoked | 2,093 | 60 | 561 | 65.6 |
| Missing or no answer | 18 | 0.5 | 7 | 0.8 |
| Total | 3,501 | 100 | 855 | 100 |
|
Diagnosis by doctor
a
| ||||
| Allergic nasal and/or eye problems | 629 | 18 | 516 | 60.4 |
| Non-allergic nasal problems | 72 | 2 | 33 | 3.9 |
| Asthma | 318 | 9 | 187 | 21.9 |
| Eczema | 401 | 11.5 | 146 | 17.1 |
| COPD | 35 | 1 | 8 | 0.9 |
| None of these diagnoses | 2,388 | 68 | 251 | 29.4 |
| Missing or no answer | 35 | 1 | 8 | 0.9 |
Abbreviation: COPD, chronic obstructive pulmonary disease.
Any value for the total population includes the group with self-reported allergic rhinitis.
Several alternatives could be specified.
Pharmacological treatment and health-care contacts
The self-reported use of pharmacological treatment is presented in Table 2. Among persons with self-reported allergic rhinitis, oral antihistamines were by far the most frequently used drug (72%), followed by nasal steroids (44%) and decongestant nasal spray (41%). Together, these drugs accounted for 70% of the total pharmaceutical costs of €106.5 per individual with allergic rhinitis. The corresponding cost of health-care contacts was about the same (€103.8 per individual with allergic rhinitis). Physician visits accounted for a mean cost/person of €77.2, nurse visits €11.5, telephone consultations €3.8 and other consultations €11.3.
Table 2. Use of pharmacological treatments and mean cost/person in 855 participants with self-reported allergic rhinitis.
| Pharmacological treatments | N | % | Mean costs, € |
|---|---|---|---|
| Any drug for nasal and/or eye problems | 690 | 80.7 | |
| Nasal spray with steroids | 380 | 44.4 | 32.4 |
| Antihistamine, oral | 612 | 71.6 | 35.4 |
| Nasal spray with antihistamine | 198 | 23.2 | 11.8 |
| Decongestant nasal spray | 353 | 41.3 | 7.3 |
| Decongestant tablets | 59 | 6.9 | 1.3 |
| Allergy vaccination, oral | 6 | 0.7 | 4.0 |
| Allergy vaccination, injection | 12 | 1.4 | 5.6 |
| Steroids, oral or injection | 63 | 7.4 | 1.8 |
| Alternative medicine | 80 | 9.4 | 6.8 |
Several alternatives possible.
Direct and indirect costs
The annual direct cost of medication and health-care contacts amounted to €210.3/individual and the indirect cost caused by productivity loss because of absenteeism and presenteeism was €750.8/individual, resulting in a total cost of €961.1 per individual/year with allergic rhinitis. The distribution of direct and indirect costs is illustrated in Figure 1. The cost per patient varied with the ARIA classification of the symptoms. For persons with moderate to severe persistent allergic rhinitis, the cost was €1756.6 per individual/year, whereas the cost of patients with mild persistent disease was only a quarter of this (€464.4 per individual/year). The costs for different subgroups of participants with allergic rhinitis are shown in Table 3. On the basis of the prevalence of 24% allergic rhinitis, the total cost to Swedish society because of allergic rhinitis was estimated at €1.3 billion annually. Of this, €0.4 billion (31%) could be related to allergic rhinitis in combination with asthma.
Figure 1.
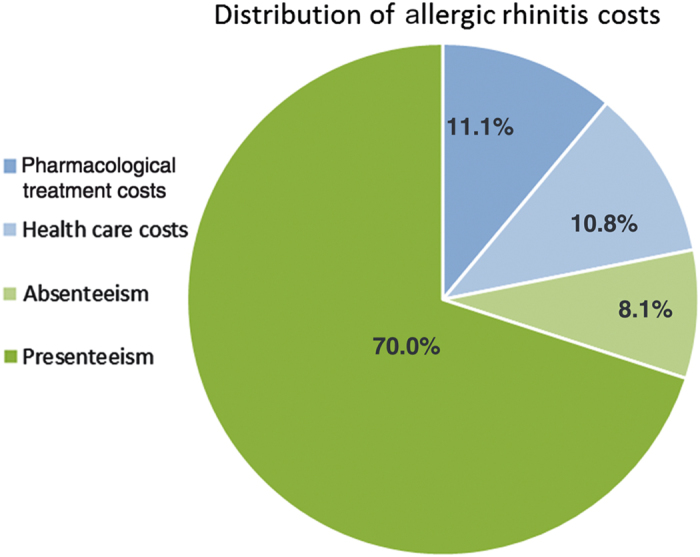
Distribution of direct and indirect costs in participants with allergic rhinitis. Total cost/individual with allergic rhinitis/year: €961.1.
Table 3. Subgroup analyses of participants with self-reported allergic rhinitis, mean costs per individual/year in € (n=855).
| N | Direct costs | Indirect costs absenteeism | Indirect costs presenteeism | Total costs | |
|---|---|---|---|---|---|
| All | 855 | 210.3 | 78.0 | 672.8 | 961.1 |
|
Age groups
| |||||
| 18–29 years | 122 | 266.5 | 102.3 | 895.0 | 1,263.7 |
| 30–44 years | 305 | 184.8 | 74.1 | 574.9 | 833.6 |
| 45–65 years | 423 | 203.8 | 74.6 | 686.9 | 965.5 |
|
Gender
| |||||
| Male | 371 | 166.3 | 91.2 | 648.3 | 905.6 |
| Female | 481 | 236.8 | 68.4 | 695.6 | 1,000.7 |
|
Working situation
| |||||
| Full-time employment | 554 | 174.2 | 99.3 | 840.6 | 1,114.2 |
| Part-time employment | 144 | 244.1 | 80.8 | 766.9 | 1,091.8 |
| Full-time student | 49 | 284.4 | 3.4 | 60.3 | 348.0 |
| Part-time student | 11 | 169.7 | 23.8 | 1,508.3 | 1,701.8 |
| Other working situation | 135 | 303.6 | 4.2 | 134.4 | 442.3 |
|
Smoking habits
| |||||
| Never smoked | 561 | 197.2 | 72.8 | 641.3 | 911.4 |
| Former smoker | 222 | 243.2 | 60.9 | 799.0 | 1,103.1 |
| Current smoker | 65 | 205.7 | 189.1 | 561.1 | 955.8 |
|
Diagnosis by doctor
| |||||
| Allergic rhinitis | 516 | 276.2 | 106.3 | 778.4 | 1,160.9 |
| Non-allergic nasal problems | 33 | 308.4 | 48.5 | 1,057.2 | 1,414.1 |
| Asthma | 187 | 402.8 | 160.2 | 772.2 | 1,335.2 |
| Eczema | 146 | 345.3 | 87.5 | 736.0 | 1,168.6 |
| COPD | 8 | 527.9 | 0.0 | 30.1 | 558.0 |
| None of these diagnoses | 251 | 84.0 | 34.0 | 467.4 | 585.4 |
Abbreviation: COPD, chronic obstructive pulmonary disease.
Discussion
Main findings
This is the first study to assess the total costs for allergic rhinitis at a national level. The mean annual direct and indirect costs were €210.3 and €750.8, respectively, resulting in a total cost of €961.1 per individual/year. The total annual cost of self-reported allergic rhinitis in Sweden was estimated at €1.3 billion. This is three to four times the estimated total cost of asthma in Sweden.7 Absenteeism represented 8% of the total cost and presenteeism 70%. The average reduction in work ability was 17%. The later estimation is well in line with previous reports.8,9 The total costs of €961.1 is, as expected, somewhat higher than the previously reported mean indirect costs of €729.6 for any form of rhinitis, including allergy and common cold.6 Together, the two investigations corroborate the idea of allergic rhinitis being a very costly disease for society.
Interpretation of findings in relation to previously published work
n the present investigation, the direct costs accounted for 22% of the total cost with an equal distribution between medication and health-care costs. This is in contrast with previous studies from the United States conducted in the 1990s that report physician’s visits and medication as the dominant cost-driving factors. Even though a later study has acknowledged the role of reduced work capacity, most studies in the field include no or insufficient evaluations of the role of presenteeism.3,10,11 Another reason for the discrepancy is probably related to differences in the recruitment of the study patients. Previous investigations generally relied on participants being recruited through medical units, something that might skew the health-economic analysis towards the direct costs.
The unique Swedish national address register (SPAR) made it possible to include all working age residents in the randomisation process. By using a representative national sample, selection bias related to socio-economic, geographical or other differences in selected populations is minimised. This approach revealed that the factor of presenteeism was of major importance. It could also be shown that more severe disease, moderate to severe allergic rhinitis, had a far more severe impact on health economy than mild symptoms. An improvement in symptoms will therefore reduce the costs.
Eighty-one per cent of the participants in this study used some kind of medication to control their allergic rhinitis symptoms. Antihistamines were most commonly used (72%), followed by nasal steroids (44%) and, somewhat surprisingly, nasal decongestants (41%). In the ARIA guidelines, antihistamines by themselves are only recommended for mild disease. They can also be used as add-on treatment in moderate to severe disease.1 In all the guidelines, nasal steroids are considered to be the most effective drugs for nasal obstruction, which is the most common symptom in allergic rhinitis and the one by which allergic rhinitis patients are most troubled.12 It is therefore surprising that antihistamines are used by almost twice as many participants compared with nasal steroids. This might be explained by patient impatience. It is well recognised that it usually takes days for the steroids to induce symptom relief, whereas oral antihistamines and nasal decongestants have a faster onset of action. The high use of nasal decongestants is also worth noting, in spite of the fact that Swedish national treatment guidelines, as well as most physicians and pharmacies, have been advising against their use for years, even for the short-term treatment of allergic rhinitis.
Strengths and limitations of this study
The population-based design of this study using a national random sample would have decreased the risk of ‘selection bias’. Self-reported data are, however, subject to recall bias, and thus the results must be interpreted with caution. The response rate of 44% is also a weakness in this study, although the demographic data are indicative of a representative population sample. Previous Swedish health economic studies have shown a response rate between 35 and 50%.6,13 Generalisation to other countries, both within EU and elsewhere, should be done with care. A number of factors will affect the outcome such as differences in healthcare and insurance systems. In addition, the degree of presenteeism and absenteeism is influenced by the labour culture and income loss associated with sickness absence in each country.
Implications for future research, policy and practice
To our knowledge, this is the first time an attempt has been made to estimate the full extent of the total costs of allergic rhinitis in a whole national population in working age. The total costs were estimated at €961.1 per individual/year, giving an annual cost for allergic rhinitis in Sweden of €1.3 billion. These results are attributable to the Swedish population of 9.5 million and the Swedish health-care system. If we assume that the demographics and health-care costs were comparable in other EU countries, the annual cost of allergic rhinitis in Germany, France and Great Britain would be between €9.4 and €9.9 billion each. Our estimate is based on official population figures and prevalence information from country-specific ARIA reports (http://europa.eu/about-eu/countries/member-countries/france/index_sv.htm).
To summarise, allergic rhinitis constitutes a prevalent condition in which relatively small individual contributions add significantly to the costs. Changes resulting in even a modest improvement in symptoms may therefore have a large impact on national costs. Given the poor adherence to the existing guidelines for treatment reported in the present study, alterations in the heath-care system that make rhinitis patients more prone to follow the advice given could save considerable sums for society. Research resulting in better treatment would, in addition to improving the quality of life for patients, add even more to these savings.
Conclusions
The total cost of allergic rhinitis in Sweden, with a population of 9.5 million, was estimated at €1.3 billion annually. These unexpectedly high costs could be related to the high prevalence of disease, in combination with the previously often underestimated indirect costs. Improved adherence to guidelines might ease the economic burden on society.
Materials and methods
Study design and study population
This study is a cross-sectional, population-based survey study that was performed on participants drawn from the SPAR Register (Statens PersonAdressRegister) that comprises all residents living in Sweden (population about 9.5 million in 2013, Statistics Sweden, www.scb.se). The 8,001 participants (male/female ratio 50/50) between 18 and 65 years of age (working age) were randomly selected to represent a national Swedish population sample. The SPAR Register is administered by the Swedish Tax Authority (www.skatteverket.se). Access was granted after approval from the regional ethics committee in Stockholm (D numbers: 2013/630-31/5 and 2013/1425-32) and application to the Tax Authority.
Data collection and study variables
Each participant was mailed a questionnaire on self-reported allergic rhinitis, followed by a reminder to reply by mail 2–4 weeks later. Seventeen questions on age, gender, smoking habits and type of employment/studies (full time or part time) were used to characterise the cohort (see Supplementary Appendix 1). Self-reported allergic rhinitis was assessed with the following question: 'Do you have any nasal allergy including hay fever?' Questions about doctor-diagnosed allergic rhinitis, non-allergic rhinitis, asthma, eczema or chronic obstructive pulmonary disease were included. The use of pharmacological treatments for allergic nose or eye symptoms (nasal steroids, nasal/oral antihistamines, nasal/oral decongestants, systemic steroids or alternative medicine) was probed, along with previous treatment with allergy vaccinations.
Self-reported allergic rhinitis was classified according to the ARIA guidelines as intermittent vs. persistent and mild vs. moderate/severe.1 Persistent was defined as an affirmative answer to the question: 'Do you have problems more than four days a week during the same week?' and/or 'Have they lasted more than four weeks in a row?' Moderate to severe disease was defined as confirming one or more of the following items: poor sleep, affected school or work performance, sport or leisure activities or other troublesome symptoms. Health-care contacts in relation to allergic rhinitis were assessed on a scale from no contacts to more than 10 contacts. Contacts were differentiated between aid obtained from physicians, nurses, telephone counselling, pharmacy personnel and/or the internet.
The direct costs included pharmaceuticals and health-care contacts such as physician and nurse visits and/or telephone consultations. The unit costs of pharmaceuticals were collected from Pharmaceutical Specialties in Sweden 2014 (www.FASS.se) and from www.apotea.se. The unit costs of health-care contacts were collected from a Swedish regional cost database (www.skane.se). Indirect costs were based on the human capital approach, and they were calculated separately for men and women.14 Using this approach, the value of time lost from work because of illness is directly related to the expected earnings lost during the period: i.e., 1 day of lost productivity is equal to one day of salary plus social costs. Information about income was obtained from Statistics Sweden, and it was adjusted according to the Consumer Price Index in February 2014.15–17 The cost of payroll taxes and pension fees was obtained from another Swedish database.18 Absenteeism and presenteeism were based on the number of days the participant reported having been home from work or working with symptoms because of allergic rhinitis during the last year. In the event of presenteeism, the participants were also asked to estimate the reduction in their working capacity (0–100%). All costs are expressed in euros (€), 2014 prices. The average exchange rate in January to June 2014 was SEK 1=€0.1117; €1=SEK 8.95 (www.riksbank.se).
The respondents in this study constitute a large national population sample (N=3,501), and the prevalence of both allergic rhinitis (24%) and rhinoconjunctivitis (19%) was in accordance with previous findings.19 The prevalence of several items such as doctor-diagnosed asthma, 9%, and non-smokers, 60%, was comparable to data from the Swedish National Institute of Public Health. In the 16- to 84-year age group, 56% of men and 60% of women are non-smokers (http://www.folkhalsomyndigheten.se/about-folkhalsomyndigheten-the-public-health-agency-of-sweden/), whereas the asthma prevalence is 9%.20
Statistical analyses
Descriptive analyses including frequencies, mean, median, s.d., minimum and maximum values were conducted for all the questions in the survey and for the direct, indirect and total costs. Statistical analyses were performed using STATA Statistical Software: Release 13.1 College Station, TX, USA.
Acknowledgments
This study was supported by the Swedish Rhinological Research Alliance (SRFA). The authors would especially like to acknowledge Charlotte Cervin-Hoberg, Carina Israelsson and Agneta Wittlock for supporting the distribution and retrieval of the questionnaires.
FUNDING
The grant providers to the funder Swedish Rhinological Research Alliance (SRFA) played no part in the study design, data collection, data analysis, data interpretation or writing of the report.
Footnotes
The Swedish Rhinological Research Alliance (SRFA) has funded this study. The SRFA is an independent national Swedish upper airway research network including Ear, Nose and Throat researchers at the main university hospitals in Sweden. The SRFA has received unrestricted research grants from MEDA AB Sweden and ALK Sweden. L-OC, MA and JH have participated in meetings funded by MEDA AB and ALK. L-OC and MA are on an advisory board for MEDA AB. MA holds patents for microemulsions for the treatment of allergic rhinitis. PO is an employee of Novartis AG, Switzerland. The remaining authors declare no conflict of interest.
References
- Brozek, J. L. et al. Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines: 2010 revision. J. Allergy Clin. Immunol. 126: 466–476 (2010). [DOI] [PubMed] [Google Scholar]
- McMenamin, P. Costs of hay fever in the United States in 1990. Ann. Allergy 73: 35–39 (1994). [PubMed] [Google Scholar]
- Crystal-Peters, J. , Crown, W. H. , Goetzel, R. Z. & Schutt, D. C. The cost of productivity losses associated with allergic rhinitis. Am. J. Manag. Care 6: 373–378 (2000). [PubMed] [Google Scholar]
- Meltzer, E. O. & Bukstein, D. A. The economic impact of allergic rhinitis and current guidelines for treatment. Annal. Allergy Asthma Immunol. 106 (2 Suppl): S12–S16 (2011). [DOI] [PubMed] [Google Scholar]
- Zuberbier, T. , Lotvall, J. , Simoens, S. , Subramanian, S. V. & Church, M. K. Economic burden of inadequate management of allergic diseases in the European Union: a GA(2) LEN review. Allergy 69: 1275–1279 (2014). [DOI] [PubMed] [Google Scholar]
- Hellgren, J. , Cervin, A. , Nordling, S. , Bergman, A. & Cardell, L. O. Allergic rhinitis and the common cold-high cost to society. Allergy 65: 776–783 (2010). [DOI] [PubMed] [Google Scholar]
- Jansson, S. A. et al. The economic consequences of asthma among adults in Sweden. Respir. Med. 101: 2263–2270 (2007). [DOI] [PubMed] [Google Scholar]
- Bramley, T. J. , Lerner, D. & Sames, M. Productivity losses related to the common cold. J. Occup. Environ. Med. 44: 822–829 (2002). [DOI] [PubMed] [Google Scholar]
- Bousquet, J. et al. Severity and impairment of allergic rhinitis in patients consulting in primary care. J. Allergy Clin. Immunol. 117: 158–162 (2006). [DOI] [PubMed] [Google Scholar]
- Malone, D. C. , Lawson, K. A. , Smith, D. H. , Arrighi, H. M. & Battista, C. A cost of illness study of allergic rhinitis in the United States. J. Allergy Clin. Immunol. 99 (1 Pt 1): 22–27 (1997). [DOI] [PubMed] [Google Scholar]
- Schramm, B. et al. Cost of illness of atopic asthma and seasonal allergic rhinitis in Germany: 1-yr retrospective study. Eur. Resp. J. 21: 116–122 (2003). [DOI] [PubMed] [Google Scholar]
- Shedden, A. Impact of nasal congestion on quality of life and work productivity in allergic rhinitis: findings from a large online survey. Treat. Respir. Med. 4: 439–446 (2005). [DOI] [PubMed] [Google Scholar]
- Lokk, J. , Olofsson, S. & Persson, U. Willingness to pay for a new drug delivery in Parkinson patients. J. Multidiscip. Healthc. 7, 431–440 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drummond, M. F. , Sculpher, M. , Torrance, G. , O'Brian, B. & Stoddart, G. Methods for the Economic Evaluation of Health Care Programmes. Oxford University Press: New York, (2005). [Google Scholar]
- Statistics Sweden. Statistical Yearbook of Sweden. http//www.scb.se/en_/Finding-statistics/Statistics-by-subject-area/Prices-and-Consumption/Consumer-Price-Index/Consumer-Price-Index-CPI (accessed on 10 March 2014).
- Statistics Sweden. Labour Force Surveys: Population aged 15-74 (LFS) by sex, age and labour status. Year 2005 - 2013 (2014). www.scb.se (accessed on 10 March 2014).
- Statistics Sweden. Total income from employment and business 2012: Income for employed individuals age 20-64 (2014). www.scb.se (accessed on 10 March 2014).
- Ekonomifakta. Sociala avgifter (2011); www.ekonomifakta.se.
- Olsson, P. , Berglind, N. , Bellander, T. & Stjarne, P. Prevalence of self-reported allergic and non-allergic rhinitis symptoms in Stockholm: relation to age, gender, olfactory sense and smoking. Acta Otolaryngol. 123: 75–80 (2003). [DOI] [PubMed] [Google Scholar]
- Ekerljung, L. et al. Has the increase in the prevalence of asthma and respiratory symptoms reached a plateau in Stockholm, Sweden? Int. J. Tuberc. Lung Dis. 14 : 764–771 (2010). [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


