Abstract
This study evaluates the impact of pediatric uninary tract infection (UTI)s on the economy and inpatient healthcare utilization in the USA. A retrospective analysis of patient demographics and hospital economics was performed on children less than 18 years of age admitted with a UTI between 2000 and 2006 using the Healthcare Cost and Utilization Project Kids’ Inpatient Database. Our results were stratified as follows. Hospital admissions—nearly 50,000 children/year were admitted with a UTI. Pediatric UTIs represented 1.8% of all pediatric hospitalizations. Seventy-three percent of patients were female and 40% were under 1 year of age. Payer information—from 2000 to 2006, pediatric insurance coverage shifted from the private sector to the public sector. Hospital cost—in 2000, estimated hospital costs for UTIs were $2,858 per hospitalization and rose to $3,838 by 2006. Mean hospital charges increased from $6,279 to $10,489 per stay. By 2006, aggregate hospital charges exceeded $520 million. Our results indicate that UTIs are among the most common pediatric admission diagnoses. Hospitalization is more common in females and younger children. Since 2000, hospital charges for UTIs increased disproportionately to hospital costs. Over time, more children hospitalized with a UTI depend on public agencies to cover healthcare expense. More efforts are needed to evaluate cost-effective strategies for evaluation and treatment of UTIs.
Keywords: Urinary tract infection, Pediatrics, Epidemiology, Economics, Utilization review
Introduction
Urinary tract infections (UTI) are one of the most common and most serious bacterial infections in children [1–3]. Estimates on the cumulative incidence of UTIs in American children indicate that up to 180,000 of the annual birth cohort will be diagnosed with a UTI by 6 years of age (3–7% of girls and 1–2% of boys) [4, 5]. Children diagnosed with UTIs account for over 1 million annual office visits and 500,000 emergency department (ED) visits. Although most UTIs are uncomplicated, some children require inpatient management. Inpatient hospitalization is required in up to 2–3% of cases [6]. As a result, inpatient UTI management is a major contributor to the American healthcare expense.
In the United States, healthcare is provided by many separate legal entities. Healthcare facilities are largely owned and operated by the private sector. Health insurance is primarily provided by the private sector, with the exception of programs like Medicare, Medicaid, TRICARE, and the Children’s Health Insurance Program. In the United States, more money per person is spent on healthcare than in any other nation in the world. Moreover, in the United States, a greater percentage of the gross domestic product is spent on healthcare than nearly any other country [7].
The economic burden of inpatient pediatric UTI management has not been recently quantified in the United States. Therefore, the objective of this study was to evaluate the impact of pediatric UTIs on the economy and inpatient healthcare utilization over the last decade. To accomplish this objective, we first examined the demographics of children admitted to the hospital with a UTI and second evaluated their economic burden by analyzing hospital characteristics, the structure of pediatric insurance coverage, and hospital charges and costs.
Materials and methods
Study design and inclusion criteria
A retrospective analysis was performed using the Healthcare Cost and Utilization Project (HCUP) Kids’ Inpatient Database in 2000, 2003, and 2006 for children less than 18 years of age admitted to the hospital with the primary diagnosis of a UTI in the USA.
Use of the Kids’ Inpatient Database
The Kids’s Inpatient Database (KID), sponsored by the Agency for Healthcare Research and Quality (AHRQ), was designed to identify and track trends in hospital utilization, access, cost, and outcome across the United States [8]. The KID, the AHRQ’s only pediatric-specific database, captures a sample of pediatric discharges from over 2,500 to 4,000 community hospitals (defined as short-term, non-federal, general, and specialty hospitals, excluding hospital units of other institutions). In 2000, the KID included 27 states (representing 6.3 million discharges). In 2003 and 2006, the KID included 36 and 38 states respectively (6.4 and 6.5 million hospitalizations). National estimates were weighted to reflect all 50 states. Detailed information on the content and design of the HCUP-KID is published elsewhere [8].
Patient identification
Children admitted with the primary diagnosis of a UTI were identified using the AHRQ’s Clinical Classification Software (CCS), a system that groups over 12,000 ICD-9-CM diagnosis codes into 260 clinically meaningful categories. Our cohort was identified using the CCS diagnosis code for urinary tract infection (CCS 159); which includes the ICD-9-CM diagnosis codes for kidney infection not otherwise specified, urinary tract infection, cystitis, urethritis, and pyelonephritis [9].
Demographics data collection
Demographic data collected from the KID included number of hospital discharges, age at admission, gender, length of hospitalization, hospital location (rural vs metropolitan), geographic location, and hospital type (general inpatient facility vs pediatric facility). Pediatric facilities were defined by the National Association of Children’s Hospitals and Related Institutions to include pediatric referral centers and a children’s unit located in a general hospital [8].
Financial data collection
Financial data collected from the KID included median household income, insurance payer type (Medicare/Medicaid, private insurance, or uninsured), hospital charges, hospital costs, and hospital charge-to-cost ratios. Hospital costs reflect the actual costs of production, while charges represent what the hospital billed the patient for services rendered during the admission. Total charges were converted to costs using charge-to-cost ratios based on hospital accounting reports from the Centers for Medicare and Medicaid Services (CMS) [8].
Data analysis
To report national estimates, the KID developed discharge weights using the American Hospital Association universe as the standard. With each national estimate, the KID reported standard errors that were calculated using SUDAAN software (RTI International, Research Triangle Park, NC, USA). Statistical significance was determined using a two-tailed p value. A p value<0.05 was considered statistically significant. The analytical methods used to generate these results are described elsewhere [8].
Results
Urinary tract infections are a common illness in infants and young children
From 2000 to 2006, UTIs were one of the most common pediatric admission diagnoses—9th most common in 2000, 10th most common in 2003, and 11th most common in 2006. From 2000–2006, roughly 50,000 children per year were admitted to the hospital with the diagnosis of a UTI. During this period, children with UTIs represented nearly 1.8% of all hospital admissions (Table 1).
Table 1.
Number of hospitalizations for pediatric urinary tract infections (UTIs) by category
| 2000 | 2003 | 2006 | ||
|---|---|---|---|---|
| All admissions (SE)a | 6,351,345 (122,677) | 6,468,292 (109,915) | 6,578,069 (112,712) | |
| UTI admissions | 49,338 (1,630) | 51,899 (1,555) | 49,397 (1,480) | |
| Age group (years) | <1 | 20,114 (877) | 21,863 (884) | 21,255 (804) |
| 1–4 | 10,746 (396) | 10,903 (351) | 10,400 (328) | |
| 5–9 | 8,222 (278) | 8,186 (242) | 7,355 (242) | |
| 10–14 | 4,239 (157) | 4,320 (146) | 3,837 (138) | |
| 15–17 | 6,016 (183) | 6,627 (157) | 6,549 (171) | |
| Gender | Male | 12,906 (643) | 14,269 (651) | 13,348 (573) |
| Female | 36,426 (1,131) | 37,223 (996) | 35,743 (984) | |
| Region | Northeast | 8,969 (763) | 8,867 (633) | 8,731 (574) |
| Midwest | 7,986 (788) | 10,722 (767) | 10,559 (808) | |
| South | 20,963 (1442) | 20,934 (1,364) | 19,549 (1,293) | |
| West | 11,420 (1,033) | 11,378 (965) | 10,557 (895) | |
| Location | Rural | 8,448 (301) | 8,064 (302) | 6,519 (233) |
| Metropolitan | 40,759 (1,602) | 42,729 (1,557) | 41,727 (1,491) |
Standard error reported by the Healthcare Cost and Utilization Project—Kids’ Inpatient Database (HCUP-KID)
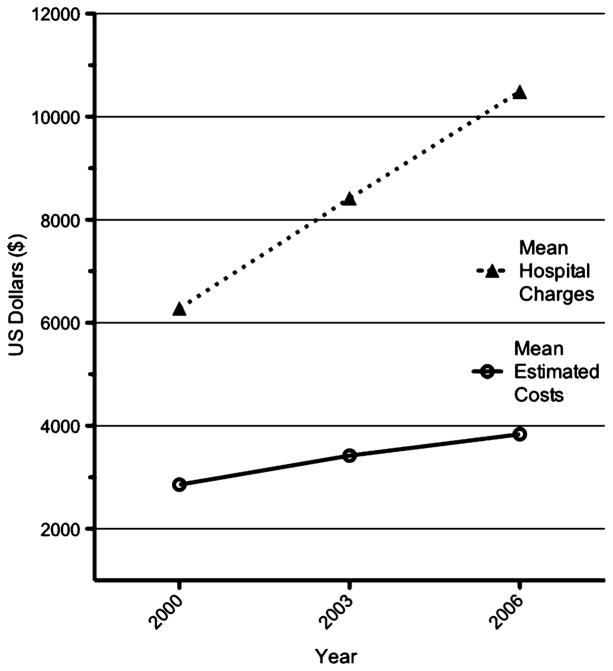
Children less than 1 year of age represented 40% of all UTI hospitalizations (Fig. 1). Overall, girls were 2.5 times more likely to be admitted with a UTI than males. Children were also more likely to be admitted if they lived in an urban setting. Children living in households with a median income in the fourth quartile were more likely to require hospitalization than children from wealthier families. The average hospital stay for a UTI was 3.1±0.1 days. Average hospitalization length did not significantly vary by year, hospital type (general hospital vs pediatric hospital), age group, or gender (p value>0.05).
Fig. 1.
Number of annual urinary tract infection (UTI) admissions by age group
Pediatric insurance coverage has shifted from the private to the public sector
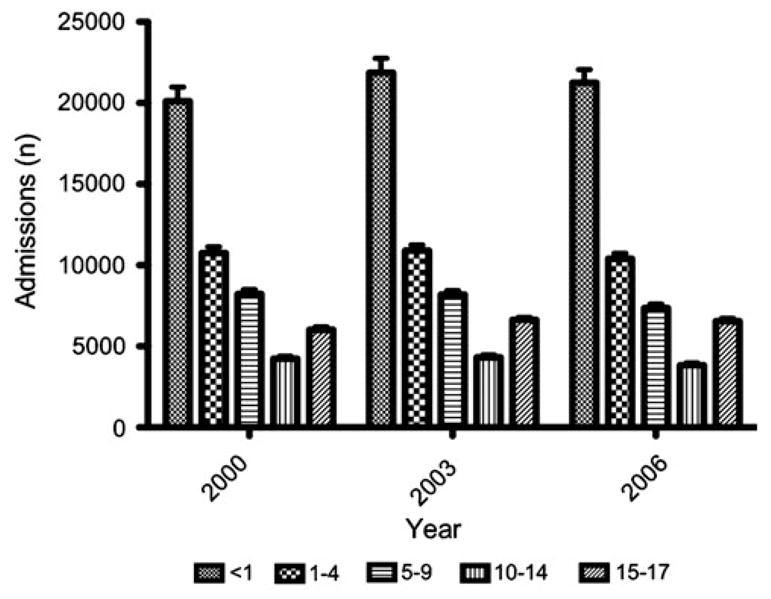
In 2000, 50% of children admitted with a UTI had private insurance as their primary payer. By 2006, only 31% of children admitted with a UTI had private insurance—representing a 19% decrease (p value<0.01). On the other hand, the number of children covered by government agencies (i.e. Medicaid) increased nearly 22% (Fig. 2). In 2000, 42.3% of children with UTIs depended on government insurance; by 2006 this had increased to 51.5% (p value< 0.01). During this period, the percentage of self-payers (i.e. uninsured) remained relatively constant.
Fig. 2.
Coverage composition by primary payer
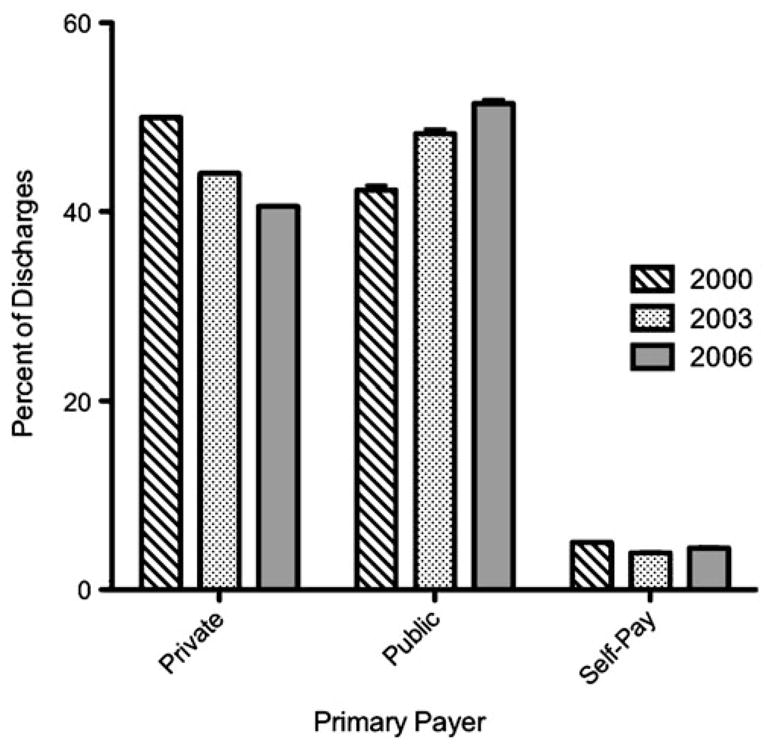
Hospital costs and charge-to-cost ratios have increased over time
From 2000–2006, hospital costs increased (Fig. 3). In 2000, the mean estimated hospital cost for a child admitted with a UTI was $2,858 per hospital stay. In 2006, this rose to $3,838. Costs were significantly higher in boys, children’s hospitals, and metropolitan medical centers (p value<0.05). During this same period, mean hospital charges (the hospital bill) increased from $6,279 to $10,489 per hospitalization—representing a 67% increase. By 2006, aggregate hospital charges exceeded $520 million. In 2000, the average hospital charge/cost ratio was ~2.1. In 2006, this ratio rose to ~2.7. This increase was more pronounced in children’s hospitals than in general inpatient facilities—with a 29.95% increase in pediatric hospitals versus a 23.8% increase in general hospitals.
Fig. 3.
Trends in hospital charges and estimated costs from 2000 to 2006
Discussion
The socioeconomic burden of pediatric UTIs is large and increasing at a rapid rate in the United States. Recently, the National Institute of Diabetes and Digestive Kidney Diseases completed a project entitled “Urologic Diseases in America”, to quantify the financial burden of urological disease on the American public [10]. As part of this project, Freedman published a comprehensive evaluation of the influence of pediatric UTIs on healthcare expenditure [6]. This detailed study also accessed a HCUP database, the Nationwide Inpatient Sample (NIS), to analyze trends in inpatient UTI management during the mid- to late-1990s and 2000. As a complimentary follow-up to this study, we accessed an alternative HCUP database, the KID, to analyze trends in inpatient pediatric UTI management and healthcare expense over the last decade. Although the NIS and KID are both powerful databases that capture a large national sample size, the KID is unique in that it serves as the only all-payer inpatient care database for children in the United States [8]. Therefore, our results, when used in conjunction with the findings published by Freedman, offer additional insight into the socioeconomic impact of pediatric UTIs.
Like Freedman, our data indicate that children with UTIs frequently seek medical attention. Over the last 20 years, both NIS and KID data indicate that UTIs are one of the most common pediatric infections that require hospitalization. When comparing the number of admissions for UTIs with the number of admissions for the most common infection-related diagnoses in the KID, annual UTI admissions do not trail far behind admissions for respiratory infections (i.e. pneumonia and bronchiolitis) or soft tissue infections. Since 2000, inpatient admission rates (50,000 admissions/year) and lengths of hospitalization (3.1 days± 0.1 days) have remained fairly consistent.
Our data indicate that age and gender define differences in inpatient UTI management. The KID data suggest that girls are more likely to require hospitalization than boys. These results are consistent with historical UTI demographics that date back to the 1960s [11, 12]. Moreover, KID data suggest that children less than 1 year of age are nearly 2.5 times more likely to receive inpatient care than older children. This finding is reinforced in several community studies that indicate children less than 1 year of age are at greater risk of developing UTIs than older children [12, 13]. Multiple underlying factors may contribute to this age group discrepancy. Because infants do not typically present with the classic symptoms of a UTI and/or pyelonephritis, there may be a delay in their diagnosis. Consequently, younger patients may be more likely to develop complicated UTIs, bacteremia, or sepsis that necessitates aggressive inpatient management. Moreover, infants with UTIs are more likely than older children to present with underlying congenital genitourinary malformations that require additional inpatient evaluation [14, 15]. In boys, this difference may be a reflection of whether or not the child is circumcised. Uncircumcised infants have been shown to be at greater risk of developing UTIs that require hospitalization than circumcised boys [16, 17]. Although infants are more likely to be admitted with a UTI than older children, it should be noted that approximately 5,000 to 10,000 children in each of the older age groups are admitted annually with a UTI. Therefore, UTIs definitely contribute to patient morbidity and healthcare expense across the entire pediatric age range.
The KID data also suggest that children living in urban environments or impoverished households have higher hospitalization rates for UTIs. This trend is depicted in a 1988 AHRQ report by Millman et al. that indicates that persons living in low-income zip codes have nearly three times more UTI admissions per capita than wealthier zip codes [18]. In part, this may be a reflection of inadequate access to outpatient healthcare in impoverished communities. Because a larger proportion of hospital EDs are located near/in underserved urban environments, they may be more accessible to impoverished families than suburban office-based practices [19, 20]. In 2000, Freedman indicated that children with Medicaid visited EDs for UTI-related care 2.8 times more frequently than children with commercial insurance [6]. As outlined in prior studies, when larger volumes of patients are evaluated in hospital EDs, admission rates tend to increase [19, 21]. Unfortunately, overuse of EDs has been identified as a major factor contributing to increased federal healthcare expense [22, 23].
In attempt to offset rising healthcare expense, the United States federal government massively expanded Medicare and Medicaid coverage. In 1985, roughly 10 million children were enrolled in Medicaid; by 2000, this number had nearly doubled [24]. This trend is depicted in our data. Since 2000, there has been a 22% relative increase in the number of children admitted with UTIs who rely on Medicare/Medicaid as their primary payer. Conversely, there has been a rather pronounced reduction in the number of children who have commercial/private insurance. Several explanations may account for this significant shift in insurance coverage, but they cannot be justified by the KID data.
Even though Medicare/Medicaid expansions may limit the financial burden to its recipients, hospital charges continue to increase. From 2000 to 2006, KID data indicate that hospital charges for UTI management outpaced hospital CMS-allowable costs. In 2006, national aggregate hospital charges exceeded $520 million. While these increases do not imply that hospital reimbursements have increased, they do reflect inflation in pediatric hospital charges relative to CMS-allowable costs. When coupling increased hospital costs with national insurance coverage changes, important questions arise about healthcare policy in the USA—primarily whether the composition of insurance coverage affects hospital-charging practices.
In an attempt to offset rising hospital charges for UTI admissions, physicians need to promptly recognize, evaluate, and appropriately treat a suspected UTI. A complete history and physical examination are just as critical in the evaluation of a child with a suspected UTI as laboratory studies. Recent studies have focused on understanding the patient population and assessing the likelihood of the patient having a UTI [15, 25]. If this is done, an appropriate and timely evaluation can be implemented that minimizes morbidity, excessive testing, treatment delay, and/or unnecessary hospitalization.
Delayed treatment, inappropriate treatment, and unnecessary treatment/hospitalization are major factors contributing to increased healthcare costs [25, 26]. Potential methods of reducing costs for pediatric UTI healthcare include:
Increased dependence on outpatient management
More appropriate utilization of oral antibiotic therapy (compared with more expensive parenteral therapy)
Limiting unnecessary usage of prolonged courses of antibiotic therapy
Minimizing the use of prophylactic antibiotics
Studies of children with UTIs greater than 1 month of age have demonstrated that treatment with parenteral antibiotics in an outpatient setting is safe and effective [27–30]. Moreover, several multicenter, randomized trials have concluded that treatment with oral antibiotics is equally as effective as treatment with intravenous antibiotics [31–33]. To this end, Hoberman et al. demonstrated that mean charges and costs for inpatient UTI therapy are at least twice as high as those for outpatient therapy [31]. Therefore, inpatient UTI management should be reserved for young infants, children with unstable vital signs, severe dehydration, and/or concerns regarding sepsis.
A number of studies have compared short-course and/or single-dose antibiotic therapy with standard therapy for UTIs with mixed results [34–37]. The American Academy of Pediatrics currently recommends a 7- to 14-day course of antibiotic therapy for all children 2 months to 2 years of age with a UTI [38]. However, we were unable to find any evidence that suggests a longer course of antibiotic therapy (11–14 days) is more effective than a shorter course of therapy (7–10 days) in the treatment of pediatric UTIs. Multiple studies demonstrate that a short course of antibiotic therapy has low rates of reinfection and treatment failure [39–41]. Thus, in many situations, widespread adoption of a shorter treatment course would deliver effective and less costly care. Further research to identify the efficacy of even shorter treatment courses in other subsets of children will help determine the most cost-effective and safe treatment regimen.
For many years, long-term antibiotic prophylaxis has been recommended for children at risk of UTIs [38, 42]. This standard has recently been challenged. Within the last 5 years, four published multicenter trials evaluated the efficacy of continuous antimicrobial prophylaxis and showed no reduction in the incidence of recurrent UTIs [43–46]. However, two recent multicenter trials from Australia and Sweden demonstrated a limited effectiveness of antibiotic prophylaxis in reducing the incidence of recurrent UTIs. These results suggest that prophylactic antibiotics may be useful only in particular subsets of children with UTIs [47, 48]. Broad use of antibiotic prophylaxis for all children with a UTI and vesicoureteral reflux (VUR; e.g. low-grade VUR) is not supported by published data and suggests that this area can be another possible avenue for reducing unnecessary healthcare costs [45–47, 49].
Although the KID is a comprehensive and powerful database that captures over 6.5 million annual pediatric hospitalizations, we acknowledge that this study has several limitations. First, the KID does not provide complete financial and demographic data for participating hospitals, and it includes hospitals in only ~70% of states. Because our study population was identified using the AHRQ’s CCS, we may have captured patients who were admitted to the hospital with additional and/or different presenting conditions (i.e. febrile neonates, admission to rule out sepsis, etc.). Also, there is a lack of appropriate data on race and ethnicity. The AHRQ notes that statewide reporting is inconsistent, making national racial/ethnic estimates unreliable. Additionally, financial data on hospital costs for medical services rendered are not readily available; thus, the total costs reported are estimated using hospital accounting reports from the CMS. Moreover, the costs reported only reflect the immediate costs of inpatient treatment and do not account for costs related to the management of underlying abnormalities, chronic sequelae, or loss of societal productivity. Finally, KID data are not available for primary payer reimbursements.
In conclusion, this study was designed to quantify and highlight the socioeconomic impact of pediatric UTIs in the USA. Our data confirm that UTIs are one of the most common pediatric infections that require hospitalization. Since 2000, UTIs represent nearly 2% of all pediatric hospitalizations. Hospitalization is more common in females and younger children. Over the last decade, hospital charges for inpatient UTI management have increased disproportionate to hospital costs. In 2006, US hospital charges for pediatric UTIs exceeded $520 million. As healthcare costs rise, more children are relying on public insurance agencies to cover healthcare expense. These findings emphasize the need for continued research in the area of cost-effective strategies for the management of pediatric UTIs.
Footnotes
Financial disclosure and conflict of interest
The authors have no conflicts of interest or financial relationships relevant to this article to disclose.
Contributor Information
John David Spencer, Division of Nephrology, Department of Pediatrics, Research Institute at the Nationwide Children’s Hospital, Ohio State University, 700 Children’s Drive, Columbus, OH 43205, USA.
Andrew Schwaderer, Division of Nephrology, Department of Pediatrics, Research Institute at the Nationwide Children’s Hospital, Ohio State University, 700 Children’s Drive, Columbus, OH 43205, USA.
Kirk McHugh, Center for Molecular and Human Genetics, Research Institute at the Nationwide Children’s Hospital, Ohio State University, 700 Children’s Drive, Columbus, OH 43205, USA.
David S. Hains, Email: David.Hains@nationwidechildrens.org, Division of Nephrology, Department of Pediatrics, Research Institute at the Nationwide Children’s Hospital, Ohio State University, 700 Children’s Drive, Columbus, OH 43205, USA. Center for Clinical and Translational Research, Research Institute at the Nationwide Children’s Hospital, Ohio State University, 700 Children’s Drive, Columbus, OH 43205, USA
References
- 1.Bachur RG, Harper MB. Predictive model for serious bacterial infections among infants younger than 3 months of age. Pediatrics. 2001;108:311–316. doi: 10.1542/peds.108.2.311. [DOI] [PubMed] [Google Scholar]
- 2.Byington CL, Rittichier KK, Bassett KE, Castillo H, Glasgow TS, Daly J, Pavia AT. Serious bacterial infections in febrile infants younger than 90 days of age: the importance of ampicillin-resistant pathogens. Pediatrics. 2003;111:964–968. doi: 10.1542/peds.111.5.964. [DOI] [PubMed] [Google Scholar]
- 3.Purcell K, Fergie J. Concurrent serious bacterial infections in 2396 infants and children hospitalized with respiratory syncytial virus lower respiratory tract infections. Arch Pediatr Adolesc Med. 2002;156:322–324. doi: 10.1001/archpedi.156.4.322. [DOI] [PubMed] [Google Scholar]
- 4.Beetz R. May we go on with antibacterial prophylaxis for urinary tract infections? Pediatr Nephrol. 2006;21:5–13. doi: 10.1007/s00467-005-2083-6. [DOI] [PubMed] [Google Scholar]
- 5.Chesney RW, Carpenter MA, Moxey-Mims M, Nyberg L, Greenfield SP, Hoberman A, Keren R, Matthews R, Matoo TK. Randomized Intervention for Children with Vesicoureteral Reflux (RIVUR): background commentary of RIVUR investigators. Pediatrics. 2008;122(Suppl 5):S233–S239. doi: 10.1542/peds.2008-1285c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Freedman AL. Urologic diseases in North America project: trends in resource utilization for urinary tract infections in children. J Urol. 2005;173:949–954. doi: 10.1097/01.ju.0000152092.03931.9a. [DOI] [PubMed] [Google Scholar]
- 7.World Heatlh Statistics. World Health Organization; 2009. [Accessed 6 June 2010]. http://www.who.int/whois/whostat/2009/ed.index.html. [Google Scholar]
- 8.HCUP Kids’ Inpatient Database (KID) Healthcare Cost and Utilization Project (HCUP) Agency for Healthcare Research and Quality; Rockville, MD: 2000, 2003, and 2006. www.hcup-us.ahrq.gov/kidoverview.jsp. [Google Scholar]
- 9.HCUP Clinical Classifications Software (CCS) for ICD-10. Health-care Cost and Utilization Project (HCUP) Agency for Healthcare Research and Quality; Rockville, MD: 2000, 2003, and 2006. [Accessed 1 November 2009]. http://www.ahrq.gov/data/hcup/ccsicd10.htm. [Google Scholar]
- 10.Litwin MS, Saigal CS, Yano EM, Avila C, Geschwind SA, Hanley JM, Joyce GF, Madison R, Pace J, Polich SM, Wang M. Urologic diseases in America project: analytical methods and principal findings. J Urol. 2005;173:933–937. doi: 10.1097/01.ju.0000152365.43125.3b. [DOI] [PubMed] [Google Scholar]
- 11.Uhari M, Nuutinen M. Epidemiology of symptomatic infections of the urinary tract in children. BMJ. 1988;297:450–452. doi: 10.1136/bmj.297.6646.450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Winberg J, Andersen HJ, Bergstrom T, Jacobsson B, Larson H, Lincoln K. Epidemiology of symptomatic urinary tract infection in childhood. Acta Paediatr Scand Suppl. 1974:1–20. doi: 10.1111/j.1651-2227.1974.tb05718.x. [DOI] [PubMed] [Google Scholar]
- 13.Shaw KN, Gorelick M, McGowan KL, Yakscoe NM, Schwartz JS. Prevalence of urinary tract infection in febrile young children in the emergency department. Pediatrics. 1998;102:e16. doi: 10.1542/peds.102.2.e16. [DOI] [PubMed] [Google Scholar]
- 14.Jakobsson B, Esbjorner E, Hansson S. Minimum incidence and diagnostic rate of first urinary tract infection. Pediatrics. 1999;104:222–226. doi: 10.1542/peds.104.2.222. [DOI] [PubMed] [Google Scholar]
- 15.Shaikh N, Morone NE, Bost JE, Farrell MH. Prevalence of urinary tract infection in childhood: a meta-analysis. Pediatr Infect Dis J. 2008;27:302–308. doi: 10.1097/INF.0b013e31815e4122. [DOI] [PubMed] [Google Scholar]
- 16.American Academy of Pediatrics. Circumcision policy statement. American Academy of Pediatrics. Task force on circumcision. Pediatrics. 1999;103:686–693. [PubMed] [Google Scholar]
- 17.Schoen EJ, Colby CJ, Ray GT. Newborn circumcision decreases incidence and costs of urinary tract infections during the first year of life. Pediatrics. 2000;105:789–793. doi: 10.1542/peds.105.4.789. [DOI] [PubMed] [Google Scholar]
- 18.Millman M, editor. Committee on monitoring access to personal health care services. National Academy Press; Washington, DC: 1993. Access to health care in America. [PubMed] [Google Scholar]
- 19.De Marco G, Mangani S, Correra A, Di Caro S, Tarallo L, De Franciscis A, Jefferson T, Guarino A. Reduction of inappropriate hospital admissions of children with influenza-like illness through the implementation of specific guidelines: a case-controlled study. Pediatrics. 2005;116:e506–e511. doi: 10.1542/peds.2005-0053. [DOI] [PubMed] [Google Scholar]
- 20.Kemper KJ. Medically inappropriate hospital use in a pediatric population. N Engl J Med. 1988;318:1033–1037. doi: 10.1056/NEJM198804213181605. [DOI] [PubMed] [Google Scholar]
- 21.Cunningham PJ, Clancy CM, Cohen JW, Wilets M. The use of hospital emergency departments for nonurgent health problems: a national perspective. Med Care Res Rev. 1995;52:453–474. doi: 10.1177/107755879505200402. [DOI] [PubMed] [Google Scholar]
- 22.DeVoe JE, Tillotson CJ, Wallace LS. Children’s receipt of health care services and family health insurance patterns. Ann Fam Med. 2009;7:406–413. doi: 10.1370/afm.1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Orszag PR, Ellis P. The challenge of rising health care costs—a view from the Congressional Budget Office. N Engl J Med. 2007;357:1793–1795. doi: 10.1056/NEJMp078190. [DOI] [PubMed] [Google Scholar]
- 24.Centers for Medicare and Medicaid Services: 2002 data compendium
- 25.Quigley R. Diagnosis of urinary tract infections in children. Curr Opin Pediatr. 2009;21:194–198. doi: 10.1097/mop.0b013e328326f702. [DOI] [PubMed] [Google Scholar]
- 26.Condra CS, Parbhu B, Lorenz D, Herr SM. Charges and complications associated with the medical evaluation of febrile young infants. Pediatr Emerg Care. 2010;26:186–191. doi: 10.1097/PEC.0b013e3181d1e180. [DOI] [PubMed] [Google Scholar]
- 27.Dore-Bergeron MJ, Gauthier M, Chevalier I, McManus B, Tapiero B, Lebrun S. Urinary tract infections in 1- to 3-month-old infants: ambulatory treatment with intravenous antibiotics. Pediatrics. 2009;124:16–22. doi: 10.1542/peds.2008-2583. [DOI] [PubMed] [Google Scholar]
- 28.Gauthier M, Chevalier I, Sterescu A, Bergeron S, Brunet S, Taddeo D. Treatment of urinary tract infections among febrile young children with daily intravenous antibiotic therapy at a day treatment center. Pediatrics. 2004;114:e469–e476. doi: 10.1542/peds.2004-0421. [DOI] [PubMed] [Google Scholar]
- 29.Pena DA, Viviani ST, Le Corre PN, Morales MV, Montecinos BC, Gajardo SC. Treatment of urinary tract infections in febrile infants: experience of outpatient intravenous antibiotic treatment. Rev Chilena Infectol. 2009;26:350–354. [PubMed] [Google Scholar]
- 30.Baskin MN, O’Rourke EJ, Fleisher GR. Outpatient treatment of febrile infants 28 to 89 days of age with intramuscular administration of ceftriaxone. J Pediatr. 1992;120:22–27. doi: 10.1016/s0022-3476(05)80591-8. [DOI] [PubMed] [Google Scholar]
- 31.Hoberman A, Wald ER, Hickey RW, Baskin M, Charron M, Majd M, Kearney DH, Reynolds EA, Ruley J, Janosky JE. Oral versus initial intravenous therapy for urinary tract infections in young febrile children. Pediatrics. 1999;104:79–86. doi: 10.1542/peds.104.1.79. [DOI] [PubMed] [Google Scholar]
- 32.Montini G. Antibiotic treatment of pyelonephritis in children. Recent advances. Recenti Prog Med. 2008;99:343–346. [PubMed] [Google Scholar]
- 33.Neuhaus TJ, Berger C, Buechner K, Parvex P, Bischoff G, Goetschel P, Husarik D, Willi U, Molinari L, Rudin C, Gervaix A, Hunziker U, Stocker S, Girardin E, Nadal D. Randomised trial of oral versus sequential intravenous/oral cephalosporins in children with pyelonephritis. Eur J Pediatr. 2008;167:1037–1047. doi: 10.1007/s00431-007-0638-1. [DOI] [PubMed] [Google Scholar]
- 34.Keren R, Chan E. A meta-analysis of randomized, controlled trials comparing short- and long-course antibiotic therapy for urinary tract infections in children. Pediatrics. 2002;109:E70–0. doi: 10.1542/peds.109.5.e70. [DOI] [PubMed] [Google Scholar]
- 35.Michael M, Hodson EM, Craig JC, Martin S, Moyer VA. Short versus standard duration oral antibiotic therapy for acute urinary tract infection in children. Cochrane Database Syst Rev. 2003:CD003966. doi: 10.1002/14651858.CD003966. [DOI] [PubMed] [Google Scholar]
- 36.Tran D, Muchant DG, Aronoff SC. Short-course versus conventional length antimicrobial therapy for uncomplicated lower urinary tract infections in children: a meta-analysis of 1279 patients. J Pediatr. 2001;139:93–99. doi: 10.1067/mpd.2001.114698. [DOI] [PubMed] [Google Scholar]
- 37.Shapiro ED. Short course antimicrobial treatment of urinary tract infections in children: a critical analysis. Pediatr Infect Dis. 1982;1:294–297. doi: 10.1097/00006454-198209000-00002. [DOI] [PubMed] [Google Scholar]
- 38.American Academy of Pediatrics. Practice parameter: the diagnosis, treatment, and evaluation of the initial urinary tract infection in febrile infants and young children. American Academy of Pediatrics. Committee on quality improvement. Subcommittee on urinary tract infection. Pediatrics. 1999;103:843–852. doi: 10.1542/peds.103.4.843. [DOI] [PubMed] [Google Scholar]
- 39.Avner ED, Ingelfinger JR, Herrin JT, Link DA, Marcus E, Tolkoff-Rubin NE, Russell-Getz L, Rubin RH. Single-dose amoxicillin therapy of uncomplicated pediatric urinary tract infections. J Pediatr. 1983;102:623–627. doi: 10.1016/s0022-3476(83)80207-8. [DOI] [PubMed] [Google Scholar]
- 40.Gaudreault P, Beland M, Girodias JB, Thivierge RL. Single daily doses of trimethoprim/sulphadiazine for three or 10 days in urinary tract infections. Acta Paediatr. 1992;81:695–697. doi: 10.1111/j.1651-2227.1992.tb12336.x. [DOI] [PubMed] [Google Scholar]
- 41.Petersen KE. Short-term treatment of acute urinary tract infections in girls. Scand J Infect Dis. 1991;23:213–220. doi: 10.3109/00365549109023403. [DOI] [PubMed] [Google Scholar]
- 42.Downs SM. Technical report: urinary tract infections in febrile infants and young children. The urinary tract subcommittee of the American Academy of Pediatrics committee on quality improvement. Pediatrics. 1999;103:e54. doi: 10.1542/peds.103.4.e54. [DOI] [PubMed] [Google Scholar]
- 43.Garin EH, Olavarria F, Garcia Nieto V, Valenciano B, Campos A, Young L. Clinical significance of primary vesicoureteral reflux and urinary antibiotic prophylaxis after acute pyelonephritis: a multicenter, randomized, controlled study. Pediatrics. 2006;117:626–632. doi: 10.1542/peds.2005-1362. [DOI] [PubMed] [Google Scholar]
- 44.Montini G, Rigon L, Zucchetta P, Fregonese F, Toffolo A, Gobber D, Cecchin D, Pavanello L, Molinari PP, Maschio F, Zanchetta S, Cassar W, Casadio L, Crivellaro C, Fortunati P, Corsini A, Calderan A, Comacchio S, Tommasi L, Hewitt IK, Da Dalt L, Zacchello G, Dall’Amico R. Prophylaxis after first febrile urinary tract infection in children? A multicenter, randomized, controlled, non-inferiority trial. Pediatrics. 2008;122:1064–1071. doi: 10.1542/peds.2007-3770. [DOI] [PubMed] [Google Scholar]
- 45.Pennesi M, Travan L, Peratoner L, Bordugo A, Cattaneo A, Ronfani L, Minisini S, Ventura A. Is antibiotic prophylaxis in children with vesicoureteral reflux effective in preventing pyelonephritis and renal scars? A randomized, controlled trial. Pediatrics. 2008;121:e1489–e1494. doi: 10.1542/peds.2007-2652. [DOI] [PubMed] [Google Scholar]
- 46.Roussey-Kesler G, Gadjos V, Idres N, Horen B, Ichay L, Leclair MD, Raymond F, Grellier A, Hazart I, de Parscau L, Salomon R, Champion G, Leroy V, Guigonis V, Siret D, Palcoux JB, Taque S, Lemoigne A, Nguyen JM, Guyot C. Antibiotic prophylaxis for the prevention of recurrent urinary tract infection in children with low grade vesicoureteral reflux: results from a prospective randomized study. J Urol. 2008;179:674–679. doi: 10.1016/j.juro.2007.09.090. discussion 679. [DOI] [PubMed] [Google Scholar]
- 47.Brandstrom P, Esbjorner E, Herthelius M, Swerkersson S, Jodal U, Hansson S. The Swedish reflux trial in children: III. Urinary tract infection pattern. J Urol. 2010;184:286–291. doi: 10.1016/j.juro.2010.01.061. [DOI] [PubMed] [Google Scholar]
- 48.Craig JC, Simpson JM, Williams GJ, Lowe A, Reynolds GJ, McTaggart SJ, Hodson EM, Carapetis JR, Cranswick NE, Smith G, Irwig LM, Caldwell PH, Hamilton S, Roy LP. Antibiotic prophylaxis and recurrent urinary tract infection in children. N Engl J Med. 2009;361:1748–1759. doi: 10.1056/NEJMoa0902295. [DOI] [PubMed] [Google Scholar]
- 49.Montini G, Hewitt I. Urinary tract infections: to prophylaxis or not to prophylaxis? Pediatr Nephrol. 2009;24:1605–1609. doi: 10.1007/s00467-009-1213-y. [DOI] [PubMed] [Google Scholar]