Abstract
Introduction
Studies have shown high initial mortality in Antiretroviral Therapy (ART) programs from resource-limited settings. However, there is dearth of evidence on treatment outcomes and associated determinant factors in public hospitals. Therefore, the objective of this study is to assess survival and identify predictors of death in adult HIV-infected patients initiating ART at a public hospital in Eastern Ethiopia.
Methods
A retrospective cohort study was conducted by reviewing baseline and follow-up records of patients who started ART between December 1, 2007 and December 31, 2011 at Kharamara hospital. Time to death was the main outcome measure. Kaplan-Meier models were used to estimate mortality and Cox proportional hazards models to identify predictors of mortality.
Results
A total of 784 patients (58.4% females) were followed for a median of 60 months. There were 87 (11.1%) deaths yielding an overall mortality rate of 5.15/100 PYO (95% CI: 4.73-6.37). The estimated mortality was 8.4%, 9.8%, 11.3%, 12.7% and 14.1% at 6, 12, 24, 36 and 48 months respectively. The independent predictors of death were single marital status (AHR: 2.31; 95%CI: 1.18-4.50), a bedridden functional status (AHR: 5.91; 95%CI: 2.87-12.16), advanced WHO stage (AHR: 7.36; 95%CI: 3.17-17.12), BMI < 18.5 Kg/m2 (AHR: 2.20; 95%CI: 1.18-4.09), CD4 count < 50 cells/µL (AHR: 2.70; 95%CI: 1.26-5.80), severe anemia (AHR: 4.57; 95%CI: 2.30-9.10), and TB co-infection (AHR: 2.30; 95%CI: 1.28-4.11).
Conclusion
Improved survival was observed in patients taking ART in Somali region of Ethiopia. The risk for death was higher in patients with advanced WHO stage, low CD4 count, low Hgb, low BMI, and concomitant TB infection. Intensive case management is recommended for patients with the prognostic factors. Optimal immunologic and weight recoveries in the first 6 months suggest increased effort to retain patients in care at this period.
Keywords: HIV, Aids, antiretroviral therapy, Ethiopia
Introduction
According to the 2012 UNAIDS report, there are an estimated 34 million People Living with HIV (PLHIV) worldwide, Sub-Saharan Africa (SSA) accounting for 69%, with nearly 1 in every 20 adults (4.9%) living with HIV; Around 1.7 million people died from AIDS-related causes worldwide, 70% occurred in SSA [1]. Ethiopia is one of the hardest hit sub-Saharan African countries by the HIV pandemic. By the end of 2012, there were 759,268 people living with HIV; 41,444 deaths from AIDS-related causes and 20,158 new HIV infections [2]. For 2007, the estimated life expectancy was 52.5 years, with 3.9 years lost to AIDS [3]. In January 2005, the FDRE Ministry of Health (MoH) launched the free ART rollout program. By the end of 2011 there were 249,174 patients on treatment, making the ART coverage for adult population of PLHIV 86% [4]. The introduction of HAART witnessed a decrease in AIDS-defining opportunistic infections, a decline in AIDS related mortalities, and improved survival of PLHIV. Despite increased availability of ARV and promising efficacy reported from ART programs in resource-limited settings, mortality has been high particularly the first few months after initiating ART [5, 6]. Reporting treatment outcomes of patients enrolled in ART programs is important to demonstrate program effectiveness and justify continued funding, while assessment of factors associated with outcomes can help to identify opportunities for program improvement [7]. Few studies have reported baseline socio-demographic and clinical factors in predicting survival after ART initiation [8–10]. However, there are no studies describing mortality on ART and its associated factors over longer follow up periods. Therefore, this study determines factors associated with survival and progressive immunologic and weight changes among adult PLHIV receiving ART in Somali region, Ethiopia.
Methods
Study setting: the study was conducted at Kharamara hospital, in Jijiga town from March to May 2013. Jijiga, the administrative capital of Somali region, is located 614 km to the east of Addis Ababa, Ethiopia's capital. The hospital provides general outpatient and inpatient services, surgical and obstetric emergency, and regional referral hospital for ophthalmologic service. In the comprehensive HIV care and treatment service at the hospital, there are 9,208 patients enrolled, of which 1,501 ever-started ART, and 1,432 currently on ART.
Study design: a retrospective cohort study was conducted to assess survival and determinants of mortality among PLHIV receiving antiretroviral therapy. A total of 784 PLHIV aged ≥15 years, initiating ART at Kharamara hospital between December 1, 2007 and December 31, 2011 were included in the study. The independent variables were socio-demographic characteristics, baseline clinical, laboratory and ART information. The main outcome measure in the study was follow-up time till Death. The second outcome measures were median changes in CD4 count and weight.
Participants: the source population was adult HIV/AIDS patients who started ARV and were on follow up at the ART clinic during the study period. Patients who initiated treatment outside Kharamara hospital, women who were pregnant and lactating mothers on PMTCT, and patients with competing causes of death (accident, or any non-AIDS malignancies) were excluded. The sample size was determined by taking the mortality rates in two groups of PLHIV on ART based on their WHO clinical stage as exposure status. The mortality rate among exposed (WHO stage IV) is 0.3% and among non-exposed (WHO stage II-III), 0.1% [10]. The study participants were randomly selected using patients’ unique identification number and were retrospectively followed for additional 60 months until December 31, 2012.
Data collection and quality control: to compile the required information a data collection form was developed from the national ART intake and follow-up forms. The data were collected by reviewing pre-ART register, ART intake form, laboratory request, monthly cohort form, and follow up form. The most recent laboratory results before starting ART were used as a baseline value. If there were no pre-treatment laboratory tests, results obtained within one month of ART initiation were used as baseline. If two results were obtained within a month, their mean would be used. Death from all AIDS related causes was ascertained by reviewing patients’ medical records in the hospital, or registrations reported by adherence supporters. The data were collected by two experienced ART nurses who were trained on comprehensive HIV care and who are working in the ART clinic at Kharamara hospital. A supervisor supervised the data collection process. The data collectors and the supervisor were trained on the data collection procedures for two days. The investigator oversaw the overall process. All completed data collection forms were examined for completeness, consistency and clarity during data management, storage, and analysis.
Data analysis: data exploration was carried out to check for any inconsistencies, coding error, out of range, and missing values and appropriate corrections were made. Descriptive analyses of the continuous and categorical data describing the cohort's characteristics at baseline and during follow-up were made. Patients were censored on the date of any one of the following events, whichever occurred first: if lost to follow-up, if transferred to another health facility, or if alive at the end of follow up. The outcomes of each patient were dichotomized into censored or dead. Kaplan-Meier model was be used to assess survival functions stratified by baseline and follow up variables, and the log-rank test was used to assess statistical difference among groups (for equality of survival distributions). Cox-proportional Hazards model was used to identify prognostic factors of death, and to calculate their bivariate and adjusted hazard ratios. All analyses were conducted using SPSS version 16.0 for windows (SPSS® Inc., Chicago, IL, USA).
Results
The study cohort included 784 patients with a mean age of 34 (SD±10). Out of the total study population, 485 (58.4%) were females. Three hundred twenty five (41.5%) were married and 455 (58%) had dependent children at home. Four hundred eighty seven (62.1%) had at least completed primary education, and 359 (45.8%) had no occupation. The majority 431 (55%) had good ART adherence (see Table 1). At the time of ART initiation, 455 (58.0%) were in WHO clinical stage III&IV and 242 (30.9%) had an ambulatory functional status. Among the study participants, 449 (57.3%) had a BMI < 18.5 Kg/m2 and 311 (39.7%) developed active TB infection. With regard to chemoprophylaxis, the majority 658 (83.9%) were given cotrimoxazole and only 61 (7.8%) received INH. The median (IQR) weight, CD4 count and hemoglobin of the cohort were 50kg (44-56), 146 cells /µL (102-196) and 11.5 g/dL (10-13) respectively (see Table 2).
Table 1.
Socio-demographic characteristics of adult PLHIV receiving ART in Somali region, Ethiopia (N = 784), May 2013
| Variables | Total (N,%) | Dead (N,%) | Active (N,%) | Log-rank P |
|---|---|---|---|---|
| Sex | ||||
| Male | 326 (41.6%) | 46 (52.9%) | 280 (40.2%) | 0.019 |
| Female | 458 (58.4%) | 41 (47.1%) | 417 (59.8%) | |
| Age category | ||||
| 15-24 | 108 (13.8%) | 6 (6.9%) | 102 (14.6%) | 0.249 |
| 25-34 | 327 (41.7%) | 41 (47.1%) | 102 (14.6%) | |
| 35-44 | 229 (29.2%) | 25 (28.7%) | 204 (29.3%) | |
| 45+ | 120 (15.3%) | 15 (17.2%) | 105 (15.1%) | |
| Religion | ||||
| Muslim | 319 (40.7%) | 35 (11.0%) | 284 (89.0%) | 0.714 |
| Orthodox | 438 (55.9%) | 50 (11.4%) | 388 (88.6%) | |
| Protestant | 27 (3.4%) | 2 (7.4%) | 25 (92.6%) | |
| Marital status | ||||
| Married | 325 (41.5%) | 27 (31.0%) | 298 (42.8%) | 0.002 |
| Single | 115 (14.7%) | 24 (27.6%) | 91 (13.1%) | |
| Separated | 27 (3.4%) | 1 (1.1%) | 26 (3.7%) | |
| Divorced | 226 (28.8%) | 26 (29.9%) | 200 (28.7%) | |
| Widowed | 91 (11.6%) | 9 (10.3%) | 82 (11.8%) | |
| Educational status | ||||
| No education | 297 (37.9%) | 48 (55.2%) | 249 (35.7%) | 0.000 |
| Primary | 217 (27.7%) | 27 (31.0%) | 190 (27.3%) | |
| Secondary | 207 (26.4%) | 10 (11.5%) | 197 (28.3%) | |
| College/Above | 63 (8.0%) | 2 (2.3%) | 61 (8.8%) | |
| Dependent children | ||||
| Yes | 455 (58.0%) | 52 (59.8%) | 403 (57.8%) | 0.889 |
| No | 329 (42.0%) | 35 (40.2%) | 294 (42.2%) | |
| ART Adherence | ||||
| Good | 431 (55.0%) | 36 (41.4%) | 395 (56.7%) | 0.000 |
| Fair | 431 (55.0%) | 20 (23.0%) | 157 (22.5%) | |
| Poor | 176 (22.4%) | 31 (35.6%) | 145 (20.8%) |
Table 2.
Clinical and laboratory markers of adult PLHIV receiving ART in Somali region, Ethiopia (N = 784), May 2013
| Variables | Total (N,%) | Dead (N,%) | Active (N,%) | Log-rank P |
|---|---|---|---|---|
| Functional status | ||||
| Working | 434 (55.4%) | 12 (13.8%) | 422 (60.5%) | 0.000 |
| Ambulatory | 242 (30.9%) | 37 (42.5%) | 205 (29.4%) | |
| Bedridden | 108 (13.8%) | 38 (43.7%) | 70 (10.0%) | |
| WHO staging | ||||
| Stage I & II | 329 (42.0%) | 10 (11.5%) | 319 (45.8%) | 0.000 |
| Stage III | 327 (41.7%) | 38 (43.7%) | 289 (41.5%) | |
| Stage IV | 128 (16.3%) | 39 (44.8%) | 89 (12.8%) | |
| BMI for age | ||||
| ≥18.5 Kg/m2 | 335 (42.7%) | 23 (26.4%) | 312 (44.8%) | 0.000 |
| < 18.5 Kg/m2 | 449 (57.3%) | 64 (73.6%) | 385 (55.2%) | |
| Cotrimoxazole | ||||
| Given | 658 (83.9%) | 66 (75.9%) | 592 (84.9%) | 0.032 |
| Not given | 126 (16.1%) | 21 (24.1%) | 105 (15.1%) | |
| INH Given | ||||
| Given | 61 (7.8%) | 20 (23.0%) | 41 (5.9%) | 0.000 |
| Not given | 723 (92.2%) | 67 (77.0%) | 656 (98.3%) | |
| TB co-infected | ||||
| Yes | 311 (39.7%) | 45 (51.7%) | 266 (38.2%) | 0.015 |
| No | 473 (60.3%) | 42 (48.3%) | 431 (61.8%) | |
| Weight (Kg) + | 50 (44-56) |
43 (37-50) |
51 (45-56) |
0.000 |
| CD4 (cells/ µL) + | 146 (102-196) |
48 (31-99) |
156 (116-206) |
0.000 |
| Hemoglobin (g/dL) + | 11.5 (10.0-13.0) |
9.4 (7.9-11.3) |
11.8 (10.3-13.1) |
0.000 |
Median value (25th-75th percentile)
Follow up
A total of 87 (11.1%) patients died during the five year follow-up period, with majority of deaths 49(56.3%) occurring in the first 3 months (HR: 0.022). One hundred fifty seven (20.0%) patients were transferred to other facility and 193 (24.6%) were lost-to-follow up. The remaining 344 (43.9%) were active until the last censoring date. The median survival time for event (death) was 20.7 months (IQR, 17.5-22.6). The overall mortality rate in the cohort during the 1,608 person-years of observation (PYO) was 5.15/100 PYO (95% CI: 4.73-6.37). The estimated mortality was 8.4%, 9.8%, 11.3%, 12.7% and 14.1% at 6, 12, 24, 36 and 48 months respectively (see Figure 1).
Figure 1.
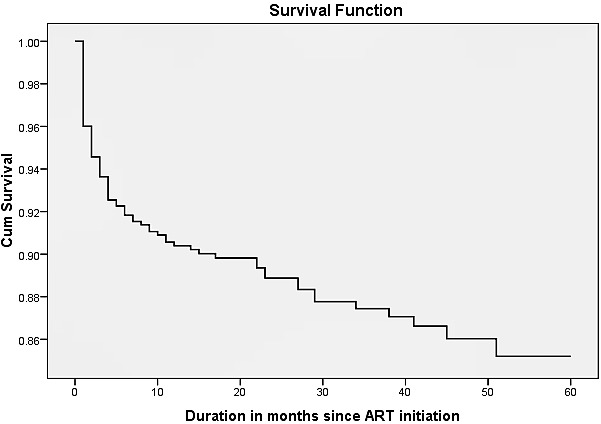
Cumulative survival of adult PLHIV receiving ART in Somali region, Ethiopia, May 2013
Predictors of mortality
In bivariate Cox regression analysis, sex, marital status, education level, functional status, WHO clinical stage, BMI, CD4 count, Anemia, cotrimoxazole prophylaxis, INH prophylaxis, TB co-infection, and ART adherence were all associated with survival (P < 0.05). In the multivariate Cox regression analysis, the independent, significant predictors of mortality in PLHIV on ART at Kharamara hospital were single marital status (AHR: 2.31; 95%CI: 1.18-4.50), a bedridden functional status (AHR: 5.91; 95%CI: 2.87-12.16), advanced WHO stage (AHR: 7.36; 95%CI: 3.17-17.12), BMI < 18.5 Kg/m2 (AHR: 2.20; 95%CI: 1.18-4.09), CD4 count < 50 cells/µL (AHR: 2.70; 95%CI: 1.26-5.80), severe anemia (AHR: 4.57; 95%CI: 2.30-9.10), and TB co-infection (AHR: 2.30; 95%CI: 1.28-4.11) (see Table 3).
Table 3.
Predictors of mortality among adult PLHIV receiving ART in Somali region, Ethiopia (N = 784), May 2013
| Variables | Crude HR (95% CI) | P value | AHR (95% CI) | P value |
|---|---|---|---|---|
| Marital status | ||||
| Married | 1 | - | 1 | - |
| Single | 2.69 (1.55, 4.66) | 0.001 | 2.31 (1.18, 4.50) | 0.015 |
| Separated | 0.40 (0.05, 2.94) | 0.367 | 0.13 (0.014, 1.21) | 0.073 |
| Divorced | 1.41 (0.82, 2.41) | 0.215 | 1.47 (0.80, 2.71) | 0.215 |
| Widowed | 1.15 (0.54, 2.44) | 0.719 | 1.27 (0.56, 2.86) | 0.566 |
| Educational status | ||||
| No education | 5.66 (1.38, 23.29) | 0.016 | 4.73 (1.07, 22.40) | 0.038 |
| Primary | 4.26 (1.01, 17.91) | 0.048 | 3.83 (0.80, 18.30) | 0.082 |
| Secondary | 1.54 (0.34, 7.05) | 0.575 | 2.43 (0.50, 12.01) | 0.281 |
| College/Above | 1 | - | 1 | - |
| Functional status | ||||
| Working | 1 | - | 1 | - |
| Ambulatory | 6.16 (3.21, 11.82) | 0.000 | 2.12 (1.05, 4.26) | 0.035 |
| Bedridden | 15.42 (8.05, 29.53) | 0.000 | 5.91 (2.87, 12.16) | 0.000 |
| WHO staging | ||||
| Stage I&II | 1 | - | 1 | - |
| Stage III | 5.28 (2.60, 10.71) | 0.000 | 4.00 (1.83, 8.74) | 0.000 |
| Stage IV | 16.22 (7.93, 33.20) | 0.000 | 7.36 (3.17, 17.12) | 0.000 |
| BMI for age | ||||
| ≥18.5 Kg/m2 | 1 | - | 1 | |
| < 18.5 Kg/m2 | 2.27 (1.41, 3.66) | 0.001 | 2.20 (1.18, 4.09) | 0.013 |
| CD4 category | ||||
| ≥ 200 | 1 | - | 1 | - |
| 125-200 | 3.87 (2.05, 7.27) | 0.000 | 1.33 (0.65, 2.72) | 0.440 |
| 50-125 | 5.62 (3.04, 10.41) | 0.000 | 2.24 (1.08, 4.65) | 0.031 |
| < 50 | 17.36 (9.96, 30.28) | 0.000 | 2.70 (1.26, 5.80) | 0.011 |
| Anemia | ||||
| Normal | 1 | - | 1 | - |
| Mild | 1.16 (0.56, 2.42) | 0.695 | 1.16 (0.52, 2.60) | 0.724 |
| Moderate | 3.27 (1.69, 6.32) | 0.000 | 2.90 (1.36, 6.16) | 0.006 |
| Severe | 8.01 (4.53, 14.17) | 0.000 | 4.57 (2.30, 9.10) | 0.000 |
| TB co-infected | ||||
| Yes | 2.21 (1.35, 3.62) | 0.002 | 2.30 (1.28, 4.11) | 0.005 |
| No | 1 | - | 1 | - |
Weight and CD4 change during the follow-up
Weight and CD4 recovery were used as supplementary indicators for comprehensive treatment outcomes. At the start of ART, the median weight of the cohort was 50.0 Kg. During the follow-up period, the median weight (IQR) at 6, 12, 24, 36, 48 and 60 months were 54 (48-61), 55 (48-64), 56 (50-64), 56 (49-64), 57 (50-65) and 57 (50-64), Kg., respectively (Figure 2). Similarly, the median CD4 count at baseline was 146cells/µL. In the follow-up period, the median CD4 count (IQR) changed to 258 (172-369), 286 (201-406), 351 (246-506), 389 (270-549), 405 (302-565) and 567 (390-770) at 6, 12, 24, 36, 48 and 60 months, respectively (Figure 3). During the follow-up period, 123 patients had their CD4 count declined to below or equal to the baseline values yielding an immunologic treatment failure rate of 7.84/100 PYO (95%CI:6.89-8.81).
Figure 2.
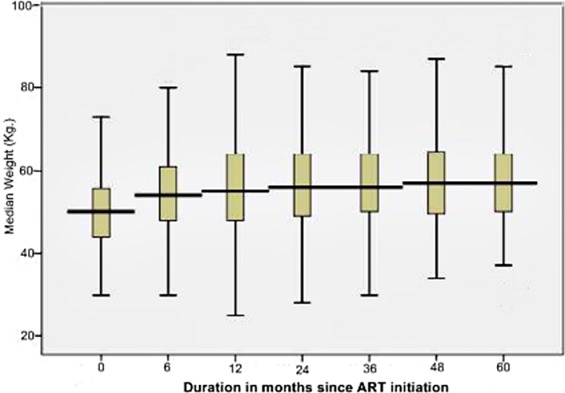
Median weight change during follow-up for adult PLHIV receiving ART in Somali region, Ethiopia, May 2013
Figure 3.
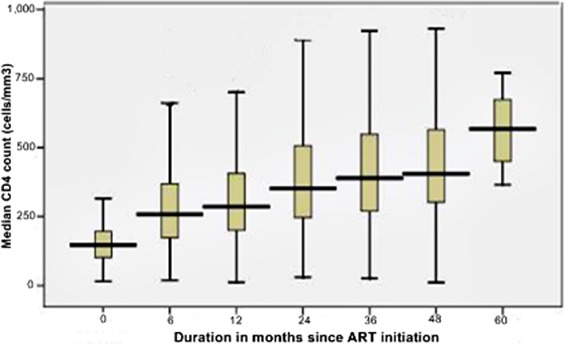
Median CD4 change during follow-up for adult PLHIV receiving ART in Somali region, Ethiopia, May 2013
Discussion
In this historical longitudinal study, there were 87 deaths in 1,608 PYO, yielding an incidence density of 5.15/100 PYO (95%CI: 4.73-6.37). The independent predictors of mortality include single marital status, being illiterate, bedridden functional status, advanced WHO status, low BMI, low CD4 count, severe anemia and TB co-infection. The estimated survival probability of the cohort at 6, 12, 24, 36 and 48 months was 91.6%, 90.2%, 88.7%, 87.3% and 85.9%, respectively. This shows a better survival compared to other studies in Africa. According to a study in a Malawian cohort, the probability of being alive on ART at 6, 12 and 18 months was 89.8%, 83.4% and 78.8% respectively [11]. On the other hand, the death rate was comparable to most studies, especially, in the 1st six months [6, 8, 9]. This might be explained by the fact that most of the patients in this study had advanced disease status (78% had CD4 < 200 cells/mL and 58% were in WHO stage III & IV). Patients who were illiterate had high risk of mortality compared to those with college education or above (AHR: 4.73; 95%CI: 1.07-22.40). A study conducted in Ethiopia also found a strong association between level of education and survival [12]. Single patients had a higher risk for death compared to married patients (AHR: 2.31; 95%CI: 1.18-4.50). This difference might be due to married patients’ psychological preparedness to seek partners’ and social support, conceive the facts, and adhere to ART [13].
The result from this study shows patients with a CD4 count of < 50 cells/mL have a higher risk of mortality (AHR: 2.70; 95%CI: 1.26-5.80) compared to those with a CD4 count of ≥ 200 cells/mL. Majority of previous studies also found twice or more risk of mortality in patients with lower CD4 count compared to those with a CD4 count of ≥ 200 cells/mL [5, 12, 14]. Patients with severe anemia were 4.57 more at risk of death compared to those with normal levels. In a study from Tanzania, patients with severe anemia were 15 times higher at risk of dying during the first year on ART compared to those with a normal hemoglobin level [6]. Other studies have also indicated patients with low hemoglobin level (<10 mg/dL) had increased risk of death [5, 9, 15]. Although there is no concrete evidence on casual association between anemia and mortality, the incidence of anemia increased with progression of HIV disease [14]. In this study also, severe anemia was associated with an advanced WHO stage (24.2% in Stage IV vs. 8.8% in stage I&II). One of the most important side effects of AZT is myelotoxicity leading to severe anemia [15]. In this cohort, severe anemia in patients taking AZT was higher (46.7%) among the dead compared to those censored (8.8%). In the current study, the risk of death in patients with a BMI < 18.5 Kg/m2 was more than two times higher (AHR: 2.20; 95%CI: 1.18-4.09) compared to those with a BMI < 18.5kg/m2. Study conducted in rural Malawi showed individuals who were severely malnourished (BMI < 16kg/m2) had six times higher risk of dying in the first three months than those with a normal nutritional status [16]. BMI is an indicator of patient nutritional status but may also be influenced by late-stage AIDS conditions, such as wasting syndrome and opportunistic infections, or by progression of the HIV itself [17]. In the current cohort, there was a significant difference in mean BMI between TB +VE patients (18.10; 95%CI: 17.66-18.54) and TB -VE ones (18.77; 95%CI: 18.40-19.14), and also, between WHO stage I&II (19.68; 95%CI: 19.24-20.13) and WHO stage IV (17.13; 95%CI: 16.49-17.77). TB co-infection at baseline or later was also associated with increased risk of mortality (AHR: 2.30; 95%CI: 1.28-4.11). Study conducted in Uganda shows, after adjusting for a history of HIV related infections, the overall relative hazard for death associated with tuberculosis was 1.81 (95%CI: 1.24-2.65) [18]. Manosuthi et.al also showed patients who delayed ART for > 6 months after TB diagnosis had a higher mortality rate than those who initiated ART < 6 months after TB diagnosis [19]. Other studies in Ethiopia have also showed the similar relationship [10, 20]. High mortality in patients living with HIV/AIDS in poor countries was linked to concomitant TB infection [15]. This may be because TB is the leading cause of death worldwide, and the virulence of the mycobacterium increases in HIV infected patients, where the host's immune system is suppressed, enabling it to establish infection very easily [21].
Different studies conducted in African countries, including Ethiopia, have shown a progressive change in CD4 count and weight after initiation of ART [9, 22]. These studies showed that the most significant increment in the median CD4 count occurred in the first six months of ART which is also the case in the current study; wherein a 76.2% increase from baseline median level was observed in the 1st six months. The recovery in weight also showed a similar progress in the 1st six months (8% gains). However, the change in median CD4 and median weight in subsequent months was minimal, with an average gain of 17% and 1.4%, respectively. In addition, the immunologic recovery was much slower in patients with baseline AIDS defining disease [18].
Conclusion
Improved survival was observed in patients taking ART in Somali region of Ethiopia. However, the risk for death was higher in patients with bed-ridden functional status, advanced WHO stage, low CD4 count, severe anemia, low BMI, and concomitant TB infection. Intensive clinical and nutritional rehabilitation is recommended during the earliest follow up periods on ART for patients with these prognostic factors. Providing screening and chemoprophylaxis for TB to patients on ART is insurmountable in deterring the infection and decreasing mortality. Optimal immunologic and weight recoveries occurred in the first six months indicating the need for patient retention, esp. during this crucial period.
Acknowledgments
We would like to thank and appreciate all patients who participated in the study. We are indebted to the staff at Kharamara hospital ART clinic, especially, Azenegash Mekonen and Samrawit Mekonen for their invaluable contributions in collection and quality control of data. We are grateful to the adherence supporters Abun Dube and Aynalem Bekele who carried out home visits to ascertain patients’ final outcome status. We are also grateful to Somali Regional Health Bureau for facilitating conditions while carrying out this study. We would like to extend our heartfelt gratitude and appreciations to Tiringo Nigusse for her financial support to this project.
Competing interests
The authors declare no competing interests.
Authors’ contributions
BD was the lead author who led the design and conducted the study as well as the developed the manuscript. BM gave input into the design and statistical aspects of the study, and revised the manuscript critically for publication. TA provided guidance on study design and development of the study. All authors read and approved the final manuscript.
References
- 1.UNAIDS. Report on the global AIDS epidemic 2012: Joint United Nations Programme on HIV/AIDS. Geneva, Switzerland: 2012. ISBN 978-92-9173-592-1. [Google Scholar]
- 2.HAPCO. HIV/AIDS Estimates and Projections in Ethiopia, 2011-2016. HAPCO; 2012. [Google Scholar]
- 3.CSA/ICF, Macro. Ethiopia Demographic and Health Survey. Central statistics Agency (CSA); 2011. [Google Scholar]
- 4.FMoH/HAPCO. Country Progress Report on HIV/AIDS Response. Ethiopia: Addis Ababa; 2012. [Google Scholar]
- 5.Ojikutu BO, Zheng H, Walensky RP, Lu Z, Losina E, Giddy J, Kenneth AF. Predictors of mortality in patients initiating antiretroviral therapy in Durban, South Africa. S Afr Med J. 2008;98(3):204–208. [PMC free article] [PubMed] [Google Scholar]
- 6.Johannessen A, Naman E, Ngowi BJ, Sandvik L, Matee MI, Aglen HE, Gundersen SG, Bruun JN. Predictors of mortality in HIV-infected patients starting antiretroviral therapy in a rural hospital in Tanzania. BMC Infect Dis. 2008;8:52. doi: 10.1186/1471-2334-8-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boerma JT, Stanecki KA, Newell ML, Luo C, Beusenberg M, Garnett GP, Little K, Calleja JG, Crowley S, Kim JY, Zaniewski E, Walker N, Stover J, Ghys PD. Monitoring the scale-up of antiretroviral therapy programmes: methods to estimate coverage. Bull World Health Organ. 2006;84(2):145–150. doi: 10.2471/blt.05.025189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jerene D, Endale A, Hailu Y, Lindtjorn B. Predictors of early death in a cohort of Ethiopian patients treated with HAART. BMC Infect Dis. 2006;6:136. doi: 10.1186/1471-2334-6-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Worku A, Miguel SS. Pattern and determinants of survival in adult HIV patients on antiretroviral therapy in, Ethiopia. Global Health Action. 2010;3:1–10. doi: 10.3402/gha.v3i0.5398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jerene D, Naess A, Lindtjorn B. Antiretroviral therapy at a district hospital in Ethiopia prevents death and tuberculosis in a cohort of HIV patients. AIDS Res Ther. 2006;3(1):10. doi: 10.1186/1742-6405-3-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Banda AC, Makombe SD, Jahn A, Tweya H, Chuka S, Yu JK, Hedt B, Ralf W, Nkhata A, Schouten EJ, Kamoto K, Harries AD. Antiretroviral Therapy in the Malawi Defense Force: Access, Treatment Outcomes and Impact on Mortality. PLoS ONE. 2008;3(1):e1445. doi: 10.1371/journal.pone.0001445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sibhatu B, Ayalu AR, Tesfaye D. Predictors of mortality among HIV infected patients taking antiretroviral treatment in Ethiopia: a retrospective cohort study. AIDS Research and Therapy. 2012;9:15. doi: 10.1186/1742-6405-9-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Auld AF, Mbofana F, Shiraishi RW, Sanchez M, Alfredo C, Nelson LJ, Ellerbrock T. Four year treatment outcomes of adult patients enrolled in Mozambique's rapidly expanding antiretroviral therapy program. PLoS One. 2011;6(4):e18453. doi: 10.1371/journal.pone.0018453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Johansson KA, Robberstad B, Norheim OF. Further benefits by early start of HIV treatment in low income countries: Survival estimates of early versus deferred antiretroviral therapy. AIDS Research and Therapy. 2010;7:3. doi: 10.1186/1742-6405-7-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Canestri A, Sow PS, Vray M, Ngom F, M'boup S, Kane CT, Delaporte E, Gueye M, Peytavin G, Girard PM, Landman R. Poor Efficacy and Tolerability of Stavudine, Didanosine, and Efavirenz-based Regimen in Treatment-Naive Patients in Senegal. Med Gen Med. 2007;9(4):7. doi: 10.1186/1758-2652-9-4-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zachariah R, Fitzgerald M, Massaquoi M, Pasulani O, Arnould L, Makombe S, Harries AD. Risk factors for high early mortality in patients on antiretroviral treatment in a rural district of Malawi. AIDS. 2006;20(18):2355–60. doi: 10.1097/QAD.0b013e32801086b0. [DOI] [PubMed] [Google Scholar]
- 17.Van der Sande MA, Schim van der Loeff MF, Aveika AA, Sabally S, Togun T, Sarge-Njie R, Alabi AS, Jaye A, Corrah T, Whittle HC. Body mass index at time of HIV diagnosis: a strong and independent predictor of survival. J Acquir Immune Defic Syndr. 2004;37(2):1288–1294. doi: 10.1097/01.qai.0000122708.59121.03. [DOI] [PubMed] [Google Scholar]
- 18.Kigozi BK, Sumba S, Mudyope P, Namuddu B, Kalyango J, Karamagi C, Odere M, Katabira E, Mugyenyi P, Ssali F. The effect of AIDS defining conditions on immunological recovery among patients initiating antiretroviral therapy at Joint Clinical Research Centre, Uganda. AIDS Research and Therapy. 2009;6(17):1–10. doi: 10.1186/1742-6405-6-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Manosuthi W, Chottanapand S, Thongyen S, Chaovavanich A, Sungkanuparph S. Survival rate and risk factors of mortality among HIV/tuberculosis-coinfected patients with and without antiretroviral therapy. J Acquir Immune Defic Syndr. 2006;43(1):42–6. doi: 10.1097/01.qai.0000230521.86964.86. [DOI] [PubMed] [Google Scholar]
- 20.Eyuel T, Alemayehu W. Assessment of antiretroviral treatment outcome in public hospitals, South Nations Nationalities and Peoples Region, Ethiopia. Ethiop J Health Dev. 2011;25(2):102–109. [Google Scholar]
- 21.Khan FA, Minion J, Pai M, Royce S, Burman W, Harries AD, Menzies D. Treatment of Active Tuberculosis in HIV-coinfected Patients: A Systematic Review and Meta-Analysis. CID. 2010;50(9):1288–1299. doi: 10.1086/651686. [DOI] [PubMed] [Google Scholar]
- 22.Lawn SD, Myer L, Bekker LG, Wood R. CD4 cell count recovery among HIV-infected patients with very advanced immunodeficiency commencing antiretroviral treatment in sub-Saharan Africa. BMC Infect Dis. 2006;6:59. doi: 10.1186/1471-2334-6-59. [DOI] [PMC free article] [PubMed] [Google Scholar]


