Abstract
Background Studies have established an increased risk of radiocarpal joint posttraumatic arthritis in patients with displaced intra-articular fractures of the distal radius, although this phenomenon has yet to be evaluated in the distal radioulnar joint (DRUJ).
Purpose We hypothesized that patients with displaced intra-articular fractures of the sigmoid notch would have a higher prevalence of DRUJ arthritis and greater upper extremity dysfunction after operative treatment of distal radius fractures compared with fractures without sigmoid notch involvement. We also hypothesized that the degree of sigmoid notch incongruity would be correlated with the grade of DRUJ arthritis and the severity of upper extremity dysfunction.
Patients and Methods A retrospective review was conducted on surgically treated patients with distal radius fractures with pre- and/or postoperative computed tomography (CT) scans. Patients were divided into groups based on presence or absence of fracture extension into the sigmoid notch. Within the sigmoid notch group, postoperative CT scans were used to measure sigmoid notch fracture step-off and diastasis (mm), as well as volar or dorsal DRUJ subluxation (%). Patients were administered Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaires and radiographs were obtained to grade DRUJ arthritis using the Kellgren-Lawrence (KL) radiographic criteria.
Results Thirty-three patients were included (19 with sigmoid notch involvement and 14 without) with an average radiographic follow-up of 6.3 years (range: 3.5–10.1 years). DASH scores were available for all patients, and radiographic follow-up was available in 24 patients (73%). A trend toward higher grade of DRUJ arthritis and poorer average DASH was found in those with sigmoid notch involvement, but was not statistically different. In the sigmoid notch group there were poorer DASH scores in patients with coronal step-off > 1.0-mm (p < 0.05). There were no significant correlations between sigmoid notch step-off, diastasis or DRUJ subluxation and either KL grade of arthritis or DASH scores.
Conclusion Fractures involving the sigmoid notch did not appear to have a greater prevalence of DRUJ posttraumatic arthritis in operatively treated patients at greater than 6 years of follow-up. Postoperative sigmoid notch step-off, diastasis or DRUJ subluxation had a minimal effect on upper extremity function, but fractures with a coronal step-off of > 1.0-mm exhibited higher levels of upper extremity dysfunction.
Level of Evidence Prognostic, Level III–Case control.
Keywords: distal radial ulnar joint, intra-articular distal radius, sigmoid notch
Fractures of the distal radius are amongst the most common fractures sustained in the United States every year, particularly in the elderly population.1 2 Over the past several decades studies have shown that fractures which disrupt the articular surface of the radiocarpal joint may result in arthritis when there is displacement of the cartilage surfaces. Knirk and Jupiter's landmark study showed a clear correlation between articular step-off and early posttraumatic arthritis at the radiocarpal joint.3 While the need to restore articular congruence of the distal end of the radius has become an accepted dogma in the treatment of these fractures, this is not without controversy. For instance, Kopylov and colleagues showed in a cohort of patients with intra-articular distal radius fractures a higher incidence of degenerative changes in the fractured wrists versus the uninjured side, but minimal subjective evidence of dysfunction.4 Forward and colleagues subsequently showed in a cohort of patients with distal radius fractures that while 68% of patients with intra-articular fractures had radiographic evidence of posttraumatic radiocarpal arthritis, this did not necessarily affect patient-rated outcome.5 A review of the best available evidence of articular step-off and posttraumatic arthritis concluded that in the distal radius measurable articular step-off and diastatsis correlated with a higher incidence of posttraumatic arthritis, but without a clear impact on patient outcome.6
While research to date has focused on the effect of articular incongruity on the risk of later posttraumatic arthritis in the radiocarpal joint of the distal end of the radius, little is known of the factors contributing to posttraumatic arthritis of the distal radio-ulnar. Prior studies have shown an influence of anatomic morphology of the DRUJ in the development of degenerative changes.7
Tanabe8 previously showed a 77% incidence of sigmoid notch involvement in intra-articular fractures of the distal radius, while Nakanishi found the incidence of DRUJ involvement to be 83%, with 28% of these involving multiple fracture fragments.9 DRUJ arthritis has been postulated to arise from a multitude of etiologies, including inflammatory, congenital, degenerative and posttraumatic processes.10 Although to date it has not been clearly demonstrated whether distal radius fractures which involve the DRUJ result in arthritis from displacement of the articular surface of the sigmoid notch.
The purpose of this study was to determine whether patients with disruption of the articular surface of the sigmoid notch were more likely to develop DRUJ arthritis and self-report worse outcomes compared with patients without involvement of the sigmoid notch. We hypothesized that patients with intra-articular fractures of the sigmoid notch would have a higher prevalence of DRUJ arthritis and worse self-reported outcomes compared with fractures without sigmoid notch involvement. We also hypothesized that increasing amount of articular incongruity at the sigmoid notch articular surface would be correlated with an increasing grade of arthritis in the DRUJ and with higher levels of global upper extremity disability.
Materials and Methods
Patient Study Group
After institutional review board approval was obtained, a retrospective analysis was conducted to identify a cohort of all patients undergoing operative treatment of distal radius fractures at a single institution over a 10-year period (1999–2009). A search of the institution's surgical database was conducted for patients undergoing open reduction internal fixation (ORIF) of the distal radius with a volar locked plate (VLP). Results of the search were then reviewed by the authors to evaluate patient inclusion based on the following criteria: (1) patients who were treated at one of the study sites over the past 10 years for fractures of the distal radius, (2) patients with a pre-operative computed tomography (CT) scan (for those without sigmoid notch involvement) or a postoperative CT scan demonstrating clear DRUJ involvement (for those with sigmoid notch involvement), (3) patients consenting to the study. Exclusion criteria included patients with multiple fractures in the same extremity and patients treated with methods other than ORIF with VLP (e.g., spanning external fixation).
All patients with pre-operative CT scans demonstrating no fracture extension into the sigmoid notch were placed into a control group. Patients with CT scans demonstrating involvement of the sigmoid notch, who also had postoperative CT scans to allow for evaluation of sigmoid notch articular reduction and DRUJ congruence after ORIF with a VLP were placed into the experimental group. Patient demographics such as age and sex were recorded. CT scans were then evaluated to assess articular reduction of the sigmoid notch and DRUJ congruency (in the control group the pre-operative CT scan was utilized with the assumption that there should be no postoperative sigmoid notch articular incongruity if there was no pre-operative fracture extension into the sigmoid notch). Measurements of sigmoid notch articular step-off and diastasis and DRUJ subluxation were performed on CT scans for each patient by two of the authors (MAV & DMB) utilizing our institution's proprietary electronic radiology viewing and measurement software (QREADS).
Articular step-off was measured on axial and coronal slices. The measurement was taken anywhere within the articular surface of the DRUJ on the image which demonstrated the maximal amount of step-off of the fracture fragments of the articular surface. Similarly, diastasis was measured on axial and coronal CT slices and was measured on the image which demonstrated the maximal amount of gap of the articular surface (Fig. 1A–C). DRUJ subluxation was calculated in the manner described by Ehman et al on available postoperative CT scans.11 Briefly, subluxation was measured on the axial CT image which showed the widest diameter of the sigmoid notch and ulnar head. A line was drawn spanning the articular surface of the sigmoid notch from inflection points volarly and dorsally. A circle was drawn to simulate the arc of the ulnar head and articular surface. An orthogonal line was then drawn from the sigmoid notch line to pass through the middle of the ulnar circle (Fig. 2). If A is defined as the dorsal line segment, and B is the volar line segment, displacement (D) was calculated as: D = B/(A + B) × 100%-50%.
Fig. 1.
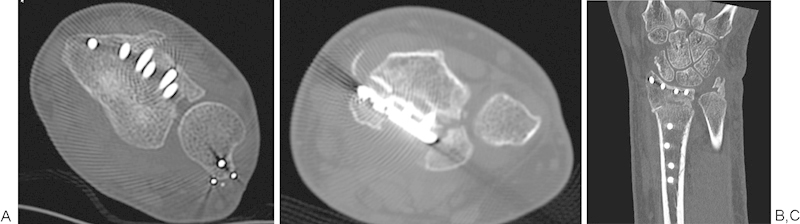
A representative axial CT scan slice in a patient (A) revealing a 1.8-mm axial step-off and 4.4-mm diastasis. A representative axial CT scan slice in another patient (B) revealing an isolated 1.6-mm axial diastasis with no step-off. A coronal CT scan slice in a third patient (C) revealing a 1.5-mm coronal step-off and 2.7-mm diastasis.
Fig. 2.
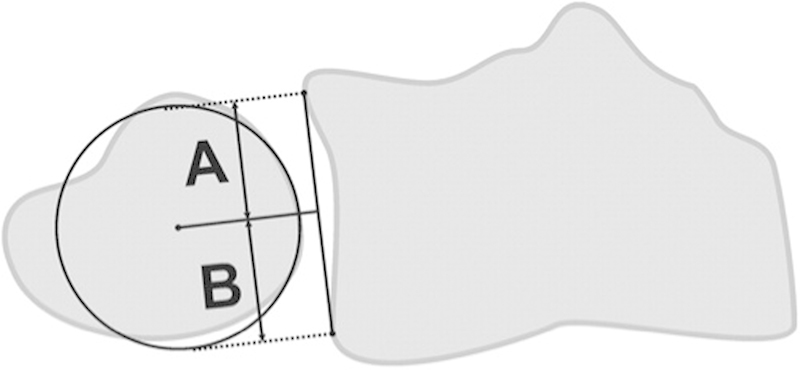
Illustration of calculation of subluxation on axial CT scans. A is the distance from the most dorsal aspect of the sigmoid notch articular surface to the center of the ulna. B is a line from the most volar aspect of the sigmoid notch articular surface. Displacement (D) is calculated as D = B/(A + B) × 100%-50%.
Evaluation and Documentation
Patients were contacted via mail or telephone and invited to participate in prospective collection of additional study data by mail. Each patient was sent the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire to assess upper extremity dysfunction. The DASH score is an established global upper extremity-specific disability instrument used to assess various disorders of the upper extremity with scores ranging from 0 to 100 (with 0 representing no disability to 100 representing maximum disability).12 13 All patients who completed these forms were then invited to obtain new follow-up X-rays of the operative wrist. These films were then assessed for the degree of osteoarthritis at the DRUJ by all four authors independently. Osteoarthritis was graded using the Kellgren-Lawrence (KL) radiographic criteria and recorded along with the length of time from injury to final follow-up.14 The KL scoring system has previously been used to grade osteoarthritis specifically in the wrist and other joints.15 Briefly summarized, grade 0 denotes no evidence of arthritis, grade 1 denotes doubtful narrowing of joint space and possible osteophytic lipping, grade 2 denotes definite osteophytes, definite narrowing of joint space, grade 3 denotes moderate multiple osteophytes, definite narrowing of joint space some sclerosis and possible deformity of bone contour, and grade 4 denotes large osteophytes, marked narrowing of joint space, severe sclerosis, and definite deformity of bone contour (Fig. 3).
Fig. 3.
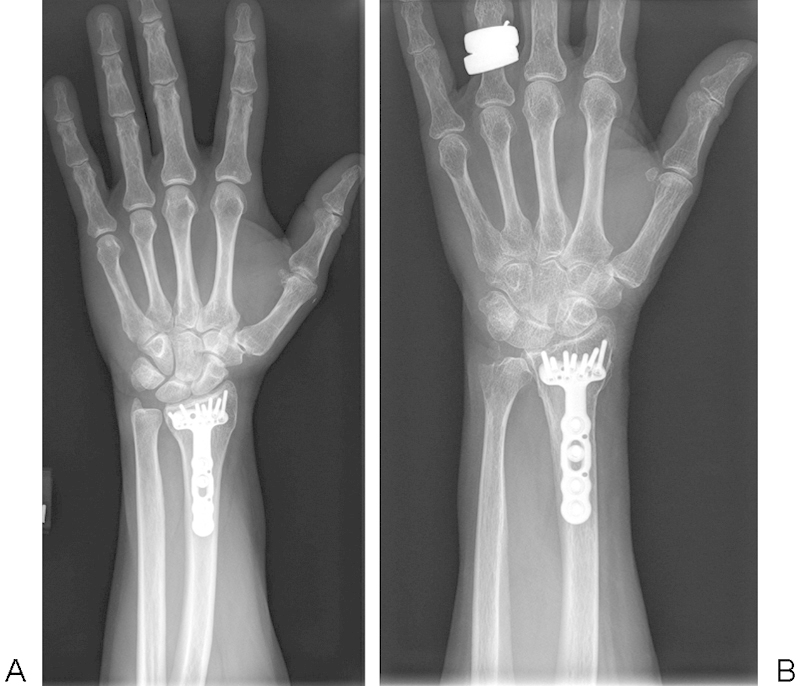
Posteroanterior radiographs of a patient with an average KL score of 0.0 (A) and another patient with an average KL score of 2.8 (B), with grades representing the average of all author scores.
Statistical Analysis
Inter-rater reliability using Chronbach α was calculated for KL score differences between each author pair. The independent t-test and Mann Whitney U-test were used to assess statistically significant differences between groups for mean DASH scores and KL scores, respectively. A Spearman correlation coefficient was calculated to compare the association between DASH scores and KL scores with the degree of articular step-off of the cartilage surface of the DRUJ (mm) in axial and coronal planes, the degree of diastasis (mm) in the axial and coronal planes, and the degree (%) of DRUJ subluxation. A power analysis revealed that in order for a one-sided independent t-test to detect a 1-point difference in arthritis grade on the 5-point KL scale with a standard deviation of 1, an α value of 0.05 and a power of 0.80, 13 patients would be required per group or a total of 26 patients. Statistical analysis was performed using SPSS (IBM SPSS Statistics for Windows, Version 21.0., IBM Corp, Armonk, NY).
No author has any conflict of interest to disclose related to the subject of this paper.
Procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 and 2008.
Informed consent for research purposes was obtained per institutional protocol.
Results
Demographics
An initial search of our database yielded a total of 596 patients undergoing ORIF with VLP of distal radius fractures in the time period specified. Of these, 209 had pre-operative CT scans, but only 20 of these demonstrated no extension into the DRUJ. Of the remaining 189, only 46 had fracture extension into the DRUJ as well as postoperative CT scans. We were able to contact 14 out of 20 patients in the group without DRUJ extension, and 19 of the 46 patients with DRUJ extension. This yielded a final sample size of 33 patients (19 with sigmoid notch involvement and 14 without). Baseline demographic values are summarized in Table 1. The average radiographic follow-up was 6.3 years (SD = 1.7 years, minimum = 3.5 years, maximum = 10.1 years). Both groups were similar with regard to baseline demographic characteristics, and there was no difference in age (p = 0.788, independent t-test), gender (p = 0.744, chi square test), dominant extremity injury (p = 0.506, chi square test), or length of radiographic follow up (p = 0.258, independent t-test) in those patients with or without sigmoid notch involvement of their distal radius fractures. Among patients with sigmoid notch involvement the average sigmoid notch axial plane step-off was 0.8 mm (minimum = 0.0 mm, maximum = 2.4 mm, SD = 0.7) and average sigmoid notch coronal plane step-off was 0.5 (minimum = 0.0, maximum = 1.5 mm, SD = 0.5). Among this same group, the average sigmoid notch axial plane diastasis was 1.6 mm (minimum = 0.0 mm, maximum = 5.5 mm, SD = 1.5 mm), and average sigmoid notch coronal plane diastasis was 0.8 (minimum = 0.0 mm, maximum = 2.7 mm, SD = 0.7 mm). Among all patients with or without sigmoid notch involvement the average absolute (dorsal or volar) DRUJ subluxation was 9.1% (minimum = 0.3%%, maximum = 41.6%, SD = 10.2%).
Table 1. Demographic variables.
| All patients (n = 33) | Without sigmoid notch extension (n = 14) | With sigmoid notch extension (n = 19) | |
|---|---|---|---|
| Age at surgery (years) | 53.8 (12.0) | 54.4 (9.3) | 53.3 (12.0) |
| Gender (% female) | 87.8 | 85.7 | 89.4 |
| Dominant hand affected (%) | 36.3 | 42.9 | 31.6 |
Note: Data reported as mean (SD) or percentage.
Questionnaire Scores
DASH scores were available for all 33 patients (100% questionnaire follow-up). There was a trend toward poorer average DASH in those with sigmoid notch involvement (mean = 53.4, SD = 26.5) versus those without (mean = 42.43, SD = 22.9), but this was not statistically different (p = 0.142) (Table 2). Within the subset of patients with sigmoid notch involvement, there were significantly poorer DASH scores in patients with coronal step-off > 1.0 mm (mean = 94.0, SD = 15.6, n = 2) versus those with step-off ≤ 1.0 mm (mean = 49.4, SD = 23.9, n = 16, p = 0.022). There were no significant differences in DASH scores for those with axial step-off > 1.0 mm versus those with step-off ≤ 1.0 mm. Similarly, there were no significant differences in DASH scores for those with coronal or axial diastasis > 1.0 mm versus those with diastasis ≤ 1.0 mm or differences in DASH scores in those with DRUJ subluxation ≤10% versus those with subluxation > 10% (Table 3). Spearman's correlation analysis revealed no correlation between axial or coronal step-off or diastasis, or DRUJ subluxation and DASH scores (Table 4).
Table 2. KL scores and DASH scores by group.
| Without sigmoid notch extension (n = 14) | Sigmoid notch extension (n = 19) | p-Value | |
|---|---|---|---|
| KL score | 1.1 (0.8) | 1.6 (1.1) | 0.319 |
| DASH score | 42.4 (22.9) | 53.4 (26.5) | 0.222 |
Notes: Data reported as mean (SD). p-Values are reported for Independent Samples t-test (DASH Scores) and Mann Whitney U-test (KL Scores).
Table 3. DASH scores in those with sigmoid notch involvement.
| Radiographic parameter | Subgroup | DASH score | p-Value |
|---|---|---|---|
| Axial sigmoid notch articular step-off | Step-off ≤ 1.0-mm (n = 13) | 52.5 (25.6) | 0.838 |
| Step-off > 1.0-mm (n = 6) | 55.33 (30.8) | ||
| Coronal sigmoid notch step-off | Step-off ≤ 1.0-mm (n = 16) | 49.4 (23.9) | 0.022 |
| Step-off > 1.0-mm (n = 2) | 94.0 (15.6) | ||
| DRUJ subluxation | Subluxation ≤10% (n = 20) | 49.2 (23.0) | 0.903 |
| Subluxation >10% (n = 13) | 48.1 (29.4) |
Notes: Data reported as mean (SD). p-Values are reported for Independent Samples t-test.
Table 4. Correlation analysis of DASH scores and KL scores by group.
| Fracture step-off | Fracture diastasis | ||||
|---|---|---|---|---|---|
| Axial plane | Coronal plane | Axial plane | Coronal plane | DRUJ subluxation | |
| DASH score | −0.045 (0.856) | 0.159 (0.528) | −0.145 (0.555) | −0.030 (0.906) | −0.128 (0.476) |
| KL score | 0.121 (0.707) | 0.261 (0.439) | 0.076 (0.816) | 0.214 (0.528) | −0.084 (0.697) |
Note: Data reported as Spearman's rho correlation coefficient (p-value).
Radiographic Analysis
Long-term radiographic follow-up was available in 24 patients (72.7% radiographic follow-up). There was strong agreement regarding KL grade of arthritis in follow-up radiographs among the four evaluators as demonstrated by a Chronbach's α of 0.883. There was a trend toward higher grade of DRUJ radiographic arthritis in those with sigmoid notch involvement (mean KL score = 1.6, SD = 1.1) versus those without (mean KL score = 1.1, SD = 0.8), but this was not statistically significant (p = 0.319) (Table 5). Spearman's correlation analysis revealed no correlation between axial or coronal sigmoid notch step-off or diastasis, or DRUJ subluxation and KL scores of DRUJ arthritis (Table 4).
Table 5. KL scores in those with sigmoid notch involvement.
| Radiographic parameter | Subgroup | KL score | p-Value |
|---|---|---|---|
| Axial sigmoid notch articular step-off | Step-off ≤ 1.0 mm (n = 11) | 1.6 (1.1) | 1.00 |
| Step-off > 1.0 mm (n = 1) | 1.3 (NA) | ||
| Coronal sigmoid notch articular Step-off | Step-off ≤ 1.0 mm (n = 11) | 1.5 (1.1) | NAa |
| Step-off > 1.0 mm (n = 0) | NA | ||
| DRUJ subluxation | Subluxation ≤10% (n = 16) | 1.2 (0.9) | 0.383 |
| Subluxation >10% (n = 8) | 1.5 (1.0) |
Notes: Data reported as mean (SD). p-Values are reported for Mann Whitney U-test.
Not available (NA) for statistical comparison due to 0 subjects with a step-off > 1.0-mm.
Discussion
Previous studies have established an increased risk of radiocarpal arthritis in fractures of the distal end of the radius with persistent articular step-off of the distal radial articular surface. Knirk and Jupiter examined the outcomes of a series of 40 young-adult patients with distal radius fractures treated with both conservative and operative methods at a mean follow-up of 6.7 years.3 They found that radiographic evidence of arthritis developed in 91% of patients with any radiocarpal joint articular incongruity, while only 11% of the patients who healed with a congruent joint demonstrated evidence of arthritis at final follow-up. In their series 100% of patients who had a residual articular incongruity of the distal radius joint ≥ 2 mm developed radiographic evidence of radiocarpal arthritis. This study has been cited as the source of established dogma that intra-articular fractures should be fixed to within a 2 mm tolerance or better. However, it has been subsequently noted that Knirk and Jupiter's data are often misquoted, with little regard given to the fact that 91% of the fractures that demonstrated any articular incongruity had evidence of posttraumatic arthritis at final follow-up, putting a strict 2 mm threshold into question.16 The effect of persistent joint incongruity on radiocarpal arthritis was confirmed by Porter and Tillman in a group of 22 patients with high energy wrist injuries treated with external fixation.17 Postoperatively, 5 out of 22 patients demonstrated a radiocarpal step-off of 2 mm or greater, all of whom reported symptomatic arthritis.
While Knirk and Jupiter's study served as the catalyst for evaluating the effects of residual articular step-off on the development of DRUJ arthritis in the current study, several methodological flaws should be noted. In the original study, a single reviewer determined the radiographic parameters, only plain films were utilized to assess articular congruity and no patient provided functional outcome parameters.18 Rozental and colleagues previously showed that sigmoid notch articular step-off and gapping were detectable on CT scans of the wrist but not on X-rays in patients with intra-articular distal radius fracture.19 Heo and colleagues subsequently showed that displacement of the sigmoid notch of intra-articular fractures was often missed with plain radiographs, which had a sensitivity of only 74.7% compared with CT scans.20 The design of the current study sought to address the above shortcomings by utilizing CT scans for evaluation of DRUJ articular congruity, diastasis, and subluxation. In our study, four different reviewers separately evaluated the final radiographs for evidence of arthritis and inter-observer agreement was analyzed and quantified and found to have almost perfect agreement. Patient reported outcomes were also measured with the use of a validated global upper extremity questionnaire.
Despite efforts to design a rigorous study design, it remains unclear whether a relationship exists between fractures extension into the articular margin of the sigmoid notch of the DRUJ and subsequent development of arthritis and upper extremity dysfunction. The current study found no significant differences between upper extremity function as assessed by the DASH in those with and without fracture extension into the sigmoid notch of the DRUJ. Some previous research has also found that while patients with intra-articular involvement of the radiocarpal joint of the distal radius have a higher incidence of posttraumatic arthritis, patients with articular injuries often have no notable deleterious effect on subjective outcome. For instance, Kopylov and colleagues reported on a cohort of 76 patients with distal radius fractures with clinical and radiographic follow-up of 27 to 36 years from their injury. In a subset of 47 patients in this cohort with intra-articular fractures at an average of 32 years of follow-up, there was a higher incidence of degenerative changes in the fractured wrists versus the uninjured side, but 87% of these patients reported no subjective difference between the fractured and non-fractured side, although 37% had minor complaints.4 Forward and colleagues subsequently studied a cohort of 106 adults with distal radius fractures at a mean of 38 years of follow-up. In a subset of 40 patients in this cohort with intra-articular distal radius fractures, while 68% of these patients had radiographic evidence of posttraumatic radiocarpal arthritis, DASH scores were not different from population norms, function, as measured by the Patient Evaluation Measure (PEM), was impaired by less than 10%, and no patients were symptomatic enough to require a salvage procedure.5
Interestingly, there were significantly poorer DASH scores in those with a step-off > 1.0 mm compared with those with a step-off ≤ 1.0 mm as measured in the coronal plane on CT scans. It should however be noted that there were only two such patients meeting the criteria of greater than 1.0 mm of coronal plane step-off. While the number of patients with such a degree of coronal plane displacement was low, there was a robust difference in DASH scores which we believe warrants further study. It should be noted that the DASH is a validated instrument to detect global upper extremity dysfunction, although interpretation of DASH scores must be made with the recognition that the DASH is not a wrist or DRUJ-specific instrument.
Knirk and Jupiter's series reported that DRUJ arthritis developed in 75% of the wrists (6 of 8 wrists) with residual articular incongruity compared with only 23% of the wrists (8 of 35 wrists) without DRUJ incongruity. We hypothesized that the degree of DRUJ articular step-off or diastasis would be correlated with the grade of arthritis and/or nominal score of upper extremity dysfunction. However, in contrast to previous findings, the current series of patients did not demonstrate any significant correlations as assessed by Spearman's correlation coefficients between articular step-off measured in axial or coronal planes, or articular diastasis measured in axial or coronal planes of CT scans and either KL scores or DASH scores. Knirk and Jupiter's series also reported that 50% of congruous joints of the distal radius with radiographic DRUJ arthritis (4 of 8 wrists) had clinical evidence of laxity of the DRUJ. DRUJ instability can be caused by either soft-tissue injuries or bony abnormalities21 and the potential exists for chronic instability of the DRUJ to lead to progressive arthritis and dysfunction. Yet, we did not find a significant correlation between the percentage of DRUJ subluxation and either KL scores or DASH scores. It is important to note that we assessed only radiographic DRUJ instability as assessed by CT scans and not clinical DRUJ instability as assessed by physical exam. It is conceivable that some patients may have clinical evidence of DRUJ instability without static radiographic instability; yet the assessment of clinical DRUJ instability was beyond the scope of the present study.
It should be noted that this study has several limitations. Patient collection was performed in a retrospective fashion by identifying those patients with available CT scans, while the decision to obtain pre- or postoperative CT scans was at the discretion of the treating surgeon. However, completion of DASH questionnaires and follow-up radiographs were prospectively obtained. Furthermore, given this studies retrospective nature, it was not possible to exclude pre-existing arthritis of the DRUJ. Another limitation is that identification of patients with sigmoid notch involvement may have introduced an element of selection bias, as patients that require CT scans after surgery likely have some clinical or radiographic problem warranting further such imaging making them different from patients without postoperative CT scans. Similarly, selection of patients for pre-operative CT evaluation may have been biased toward patients with more severe injuries.
The sample size was limited by the ability of patients to obtain follow-up radiographs, yielding a much smaller sample size than the initial identified cohort. This raises the prospect of a potential Type II error due to insufficient sample size, although a-priori power analysis revealed that there was a sufficient sample size in each group to detect a 1-point difference in KL scores between groups. Lastly, there were a small number of patients with large degrees of step-off, diastasis or subluxation after operative reduction and fixation which may have further decreased the ability to detect a significant difference between groups if one existed. This is logical since most surgically treated fractures presumably are treated with the goal of restoring normal anatomy and alignment and reducing articular incongruity in both the distal radio-ulnar and radiocarpal joints.
In summary, our study found no significant correlation between DRUJ step-off, diastasis or subluxation, and posttraumatic arthritis or on patient upper extremity function. A previous summary available evidence from 36 published papers on intra-articular injuries to the distal radius, acetabulum, distal femur, and tibial plateau concluded that extent of articular displacement of various joints only weakly correlated with radiographic evidence of posttraumatic arthritis and patient outcome, and the authors suggested that different joints and even different areas of the same joint appear to have different tolerances for posttraumatic articular step-offs.6 The DRUJ may in fact be a more tolerant joint for articular injury and malalignment than the radiocarpal joint. However, patients with >1 mm step-off in the coronal plane demonstrated poorer upper extremity function as measured by the DASH score. Still, these results should be interpreted with caution as the present study is limited by a small sample size. Therefore, further work is necessary to better identify the effect of DRUJ incongruity on patient outcomes and development of posttraumatic arthritis.
Conflict of Interest None.
Note
This study has been approved by the Institutional Review Board. IRB number: 12–005434 Intra-articular fractures of the sigmoid notch: predictors of radiographic distal radioulnar joint arthritis and upper extremity dysfunction.
References
- 1.Baron J A, Karagas M, Barrett J. et al. Basic epidemiology of fractures of the upper and lower limb among Americans over 65 years of age. Epidemiology. 1996;7(6):612–618. doi: 10.1097/00001648-199611000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Nellans K W, Kowalski E, Chung K C. The epidemiology of distal radius fractures. Hand Clin. 2012;28(2):113–125. doi: 10.1016/j.hcl.2012.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Knirk J L, Jupiter J B. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am. 1986;68(5):647–659. [PubMed] [Google Scholar]
- 4.Kopylov P, Johnell O, Redlund-Johnell I, Bengner U. Fractures of the distal end of the radius in young adults: a 30-year follow-up. J Hand Surg [Br] 1993;18(1):45–49. doi: 10.1016/0266-7681(93)90195-l. [DOI] [PubMed] [Google Scholar]
- 5.Forward D P, Davis T R, Sithole J S. Do young patients with malunited fractures of the distal radius inevitably develop symptomatic post-traumatic osteoarthritis? J Bone Joint Surg Br. 2008;90(5):629–637. doi: 10.1302/0301-620X.90B5.19448. [DOI] [PubMed] [Google Scholar]
- 6.Giannoudis P V, Tzioupis C, Papathanassopoulos A, Obakponovwe O, Roberts C. Articular step-off and risk of post-traumatic osteoarthritis. Evidence today. Injury. 2010;41(10):986–995. doi: 10.1016/j.injury.2010.08.003. [DOI] [PubMed] [Google Scholar]
- 7.Hollevoet N, Verdonk R, Van Maele G. The influence of articular morphology on non-traumatic degenerative changes of the distal radioulnar joint. A radiographic study. J Hand Surg [Br] 2006;31(2):221–225. doi: 10.1016/j.jhsb.2005.10.012. [DOI] [PubMed] [Google Scholar]
- 8.Tanabe K, Nakajima T, Sogo E, Denno K, Horiki M, Nakagawa R. Intra-articular fractures of the distal radius evaluated by computed tomography. J Hand Surg Am. 2011;36(11):1798–1803. doi: 10.1016/j.jhsa.2011.08.021. [DOI] [PubMed] [Google Scholar]
- 9.Nakanishi Y, Omokawa S, Shimizu T, Nakano K, Kira T, Tanaka Y. Intra-articular distal radius fractures involving the distal radioulnar joint (DRUJ): three dimensional computed tomography-based classification. J Orthop Sci. 2013;18(5):788–792. doi: 10.1007/s00776-013-0407-0. [DOI] [PubMed] [Google Scholar]
- 10.Zimmerman R M, Kim J M, Jupiter J B. Arthritis of the distal radioulnar joint: from Darrach to total joint arthroplasty. J Am Acad Orthop Surg. 2012;20(10):623–632. doi: 10.5435/JAAOS-20-10-623. [DOI] [PubMed] [Google Scholar]
- 11.Ehman E C, Hayes M L, Berger R A, Felmlee J P, Amrami K K. Subluxation of the distal radioulnar joint as a predictor of foveal triangular fibrocartilage complex tears. J Hand Surg Am. 2011;36(11):1780–1784. doi: 10.1016/j.jhsa.2011.08.032. [DOI] [PubMed] [Google Scholar]
- 12.Smith M V, Calfee R P, Baumgarten K M, Brophy R H, Wright R W. Upper extremity-specific measures of disability and outcomes in orthopaedic surgery. J Bone Joint Surg Am. 2012;94(3):277–285. doi: 10.2106/JBJS.J.01744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hudak P L, Amadio P C, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand). The Upper Extremity Collaborative Group (UECG) Am J Ind Med. 1996;29(6):602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 14.Kellgren J H, Lawrence J S. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yamazaki H, Uchiyama S, Hata Y, Murakami N, Kato H. Extensor tendon rupture associated with osteoarthritis of the distal radioulnar joint. J Hand Surg Eur Vol. 2008;33(4):469–474. doi: 10.1177/1753193408090098. [DOI] [PubMed] [Google Scholar]
- 16.Porrino J A Jr, Tan V, Daluiski A. Misquotation of a commonly referenced hand surgery study. J Hand Surg Am. 2008;33(1):2–7. doi: 10.1016/j.jhsa.2007.10.007. [DOI] [PubMed] [Google Scholar]
- 17.Porter M L, Tillman R M. Pilon fractures of the wrist. Displaced intra-articular fractures of the distal radius. J Hand Surg [Br] 1992;17(1):63–68. doi: 10.1016/0266-7681(92)90013-r. [DOI] [PubMed] [Google Scholar]
- 18.Haus B M, Jupiter J B. Intra-articular fractures of the distal end of the radius in young adults: reexamined as evidence-based and outcomes medicine. J Bone Joint Surg Am. 2009;91(12):2984–2991. doi: 10.2106/JBJS.I.00269. [DOI] [PubMed] [Google Scholar]
- 19.Rozental T D, Bozentka D J, Katz M A, Steinberg D R, Beredjiklian P K. Evaluation of the sigmoid notch with computed tomography following intra-articular distal radius fracture. J Hand Surg Am. 2001;26(2):244–251. doi: 10.1053/jhsu.2001.22930. [DOI] [PubMed] [Google Scholar]
- 20.Heo Y M, Roh J-Y, Kim S-B. et al. Evaluation of the sigmoid notch involvement in the intra-articular distal radius fractures: the efficacy of computed tomography compared with plain X-ray. Clin Orthop Surg. 2012;4(1):83–90. doi: 10.4055/cios.2012.4.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mulford J S, Axelrod T S. Traumatic injuries of the distal radioulnar joint. Hand Clin. 2010;26(1):155–163. doi: 10.1016/j.hcl.2009.08.015. [DOI] [PubMed] [Google Scholar]


