Abstract
This article summarizes the management of distal fractures utilizing Acumed fragment-specific family of plates. No single plate option can address every fracture pattern of the distal radius. These fragment-specific plates are usually adjuncts to allow the surgeon to expand the armamentarium in the management of complex volar and dorsal comminuted distal radius fracture patterns.
Keywords: distal radius, fragment-specific, wrist, fracture, ulna
Displaced intra-articular fractures of the distal radius are a unique subset of distal radius fractures.1 2 This is usually a high-energy impaction injury resulting in a comminuted fracture pattern, and is less amendable to traditional methods of closed manipulation and casting. The prognosis for these injuries depends on radial shortening, both the radial carpal and radial ulnar articular reduction, and associated soft tissue injuries. These injuries are clearly a wrist injury, rather than a distal radius fracture alone.
The distal radius and ulna has been described as a three-column concept addressing fractures of the distal radius. The radial column, which is important for ligament support and stabilization, the intermediate column, involving the lunate facet, which is important for load transmission across the wrist, and, lastly, the ulnar column, which is important for forearm rotation and transmission across the wrist. When addressing these very difficult fractures, it is important to stabilize each of these three columns.
Currently, the majority of intra-articular fractures of the distal radius are managed by the volar approach.3 4 5 The majority of fractures of the distal radius can be managed in this manner. However, no single plate can adequately reduce every single comminuted fracture pattern of the distal radius. Therefore, it is useful to have a family of plates to address this complex fracture pattern from both a volar and dorsal approach.6 7 8 9 Fernandez and Geissler, in a review of 40 patients, describe the importance of fragment-specific reduction and fixation. This would include the radial styloid fragment, the volar and dorsal lunate facet fragments, and the metaphyseal shaft.10
The purpose of this article is to describe the management of comminuted distal radius fractures with a variety of Acumed fragment-specific plates (Hillsboro, OR) (Fig. 1). Fragment-specific plates are a useful adjunct to traditional volar and dorsal plates to stabilize a specific fracture fragment or can be used independently for fracture stabilization. This allows the surgeon to expand his armamentarium for management of these complex injuries.
Fig. 1.

Acumed (Hillsboro, OR) fragment-specific plates, including the divergent radial styloid plate, volar lunate suture plate, dorsal lunate plate, and dorsal rim buttress plate.
Surgical Technique
The Acumed fragment-specific plate system is composed of four plates. These include the dorsal rim plate, the dorsal lunate facet plate, the volar lunate facet plate, and the radial styloid plate. In addition, this system is supplemented with the Frag-Loc screw, which attaches to the Acu-Loc volar plate, and the volar ulnar distal ulnar plate for fractures of the distal ulna for the ulna column.
Frag-Loc Compression Screw
The Frag-Loc screw allows the surgeon to capture and stabilize dorsal fragments via a volar distal radius plate (Fig. 2). Basically, the Frag-Loc screw is a small screw with a washer that screws into a locked volar screw applied through the plate from the volar aspect. In this technique, a volar plate is applied and the fracture is stabilized. If the surgeon wants additional dorsal fixation, the Frag-Loc screw is applied from the volar aspect (Fig. 3). A K-wire guide is placed through the screw from the volar aspect out dorsally. A small incision made on the dorsal aspect of the distal radius over the guidewire. Dissection is carried down directly to bone to insure the guidewire is not piercing any extensor tendons. The dorsal cortex is then reamed over the guidewire, and the Frag-Loc screw is placed dorsally over the guidewire to lock into the screw inserted into the volar distal radius plate (Figs. 4 and 5).
Fig. 2.

Lateral radiograph of an intraarticular volar Barton's fracture.
Fig. 3.

Photograph of the volar locking screw being placed for the Frag-Loc system.
Fig. 4.
The Frag-Loc being inserted dorsally into the locking screw from the volar plate. Note the incision made to insure the Frag-Loc does not impale any extensor tendons dorsally.
Fig. 5.

Lateral radiograph showed anatomic joint surface with additional distal support from the Frag-Loc screw.
Dorsal Rim Buttress Plate
The dorsal approach to distal radius has several advantages. It provides an excellent view of the fracture fragments, it is relatively an easy approach as there is no neurovascular worries, and sometimes it is easier to push the fragments back to restore volar tilt from the dorsal approach. Indications for dorsal plating include severe initial dorsal displacement greater than 20 degrees from normal, marked dorsal comminution greater than or equal to 50% of the diameter of the distal radius, residual dorsal tilt greater than 10 degrees past neutral following reduction, 10 mm of radial shortening, and dorsal intra-articular fragments displaced more than 5 mm (Figs. 6 and 7). In the authors' experience, delayed presentation, malunions, and fractures with very distal dorsal comminution can be well managed from the dorsal approach.
Fig. 6.

PA radiograph of a distal intra-articular fracture of the distal radius.
Fig. 7.

Lateral radiograph showing the distal intra-articular fracture of the distal radius.
The dorsal rim plate provides excellent stability from the dorsal approach. The plate itself provides excellent support to the lunate facet with three separate screws and stabilizes the radial styloid with two separate screws. The plate runs down the ulna aspect of the radius to minimize irritation to the extensor tendons. In addition, the plate has a smooth arm that reaches from ulnar to radial to support the entire dorsal rim of the distal radius, while minimizing irritation to the extensor tendons.
The standard dorsal approach is made to the distal radius. The extensor pollicis longus is released from the third dorsal compartment, and the second and fourth dorsal compartments are elevated exposing the fracture site. The Acumed dorsal rim plate is placed on the dorsal ulnar aspect of the radial shaft and positioned under fluoroscopic control. Lister tubercle is frequently involved in the fracture and does not affect the position of the plate. The proximal distal relationship of the plate is accessed under fluoroscopy. Once the most ideal position of the plate is confirmed, a nonlocking screw is placed through the oblong nonlocking screw hole. In this manner, the plate can be (fine-tuned) adjusted so that the distal rim of the plate supports the dorsal articular surface of the distal radius. It is important to note that the vertical leg of the plate sits parallel to the ulnar aspect of the shaft of the radius. It is important that the first screw is placed through the oblong hole, and is aimed in an ulnar to radial direction to get bicortical fixation. If the screw is placed too vertically in the anterior/posterior plane, the screw may only purchase one cortex. The screw is not self-tapping and, if there is hard bone, may need to be tapped prior to insertion of the screw.
Once the first screw has been placed in the oblong hole, the distal screws may be inserted. Usually, the lunate facet screws are placed first. The plate has three options, including nonlocking screws, locking screws, or locking pegs. As the screws primarily function as buttress-type screws, locking pegs are usually utilized. However, it is the surgeon's preference and certainly locking or nonlocking screws may be used as well. The radial styloid screw is inserted following the lunate facet screws. The extensor carpi radialis longus and brevis may be retracted radially to gain access to the hole in the plate. However, an easier option is to dissect between the extensor carpi radialis longus and brevis tendons to obtain access to the radial screw hole.
Following placement of the radial styloid screw, the homerun screw is placed. This screw runs from ulnar to radial direction into the very tip of the radial styloid. The screw may be locking or nonlocking; if the locking option is used, then the locking guide is utilized. This guide can be placed initially on the plate prior to inserting the plate onto the bone, or the guide is inserted after the plate has been positioned on the distal radius. It is the authors' preference to put the locking guide on after the initial screws have been placed as previously described (Fig. 8). It is sometimes helpful to place a Hohmann retractor between the radius and ulna, and in this manner, the radius can be gently elevated posterior to the ulna to make it easier to place the guide. Once the guide is placed, the homerun screw is inserted into the tip of the radial styloid. The screw is placed just distal to the previously inserted radial styloid screw, to give support to the distal aspect of the homerun screw because of its relatively long length. The remaining 2.3-mm locking screws are then inserted into the radial shaft (Fig. 9). The extensor pollicis longus is left free, and the retinaculum of the second and fourth dorsal compartments is then closed (Figs. 10 and 11).
Fig. 8.

Photograph of the Acumed dorsal rim buttress plate with locking guide placed on the dorsal ulnar surface of the radius.
Fig. 9.

Radiograph showing placement of locking and non-locking screws into the dorsal rim buttress plate.
Fig. 10.

Posterior/anterior radiograph showing anatomic reduction of the joint surface with stable fixation of both the lunate and radial styloid fragments with a low profile of the dorsal rim plate.
Fig. 11.

Lateral radiograph showing anatomic reduction of the intra-articular distal radius.
Dorsal Lunate Plate
The Acumed dorsal lunate facet plate is designed to provide support to fracture patterns that involve the dorsal lunate facet of the distal radius and the sigmoid notch (Fig. 12). This plate can be used in isolation or combined with other plates to provide additional dorsal support. The dorsal lunate plate can be inserted through a smaller incision than the standard dorsal plate.
Fig. 12.

Lateral radiograph showing a dorsal Barton's intra-articular fracture with a radial styloid fracture.
The plate sits along the ulnar aspect of the radial shaft and supports the lunate facet. The first screw is placed in the oblong slot with a nonlocking screw once ideal positioning of the plate is confirmed under fluoroscopy. Three locking, nonlocking screws, or locking pegs are placed distally so that the plate supports the lunate facet. The remaining proximal screws are placed in the shaft (Fig. 13).
Fig. 13.

Photograph showing restoration of the dorsal Barton fracture with Acumed's dorsal lunate plate.
Usually this plate is used as an adjunct to the volar Acu-Loc plate when additional dorsal support is required. This plate is indicated particularly for very small distal fragments of the dorsal radius. It can be used in combination with other fragment-specific plates (Fig. 14).
Fig. 14.

Posterior/anterior radiograph showing anatomic reduction with the dorsal lunate plate and an Acutrak screw (Hillsboro, OR) securing the radial styloid fragment. This provided very stable fixation with low profile implants.
Volar Lunate Suture Plate
This is a useful plate for very distal fractures involving the volar aspect of the lunate facet. Frequently, these are very high-energy injuries and the fragment is rotated with the articular surface facing proximally (Figs. 15 and 16). A standard volar approach is made to the wrist. The wrist can be approached through the standard flexor carpi radialis approach or, alternatively, through an interval between the flexor tendons and the ulnar neurovascular bundle. The volar ulnar fragment is usually rotated with its capsular attachment. The fragment is de-rotated under direct visualization. Multiple sutures are placed into the capsule rotating the fragment back anatomically (Fig. 17). Once the fragment is de-rotated, the sutures are passed through the volar ulnar fragment–specific plate (Fig. 18). The plate is then positioned onto the distal radius with confirmation of ideal placement using fluoroscopy. The first screw placed is through the oblong slot in the plate. The nonlocking screw secures the plate to the bone. Once ideal confirmation of the plate is identified under fluoroscopy, the sutures are then tied securing the volar ulnar fragment with the plate acting as a buttress plate. The remaining proximal screws are placed. Usually, screws are not placed distally into the plate as this is truly a buttress for these very small distal volar ulnar fragments of the distal radius.
Fig. 15.

Extensively comminuted intra-articular distal radial fracture from a PA radiograph.
Fig. 16.

Lateral radiograph showing the comminuted intra-articular distal radius fracture.
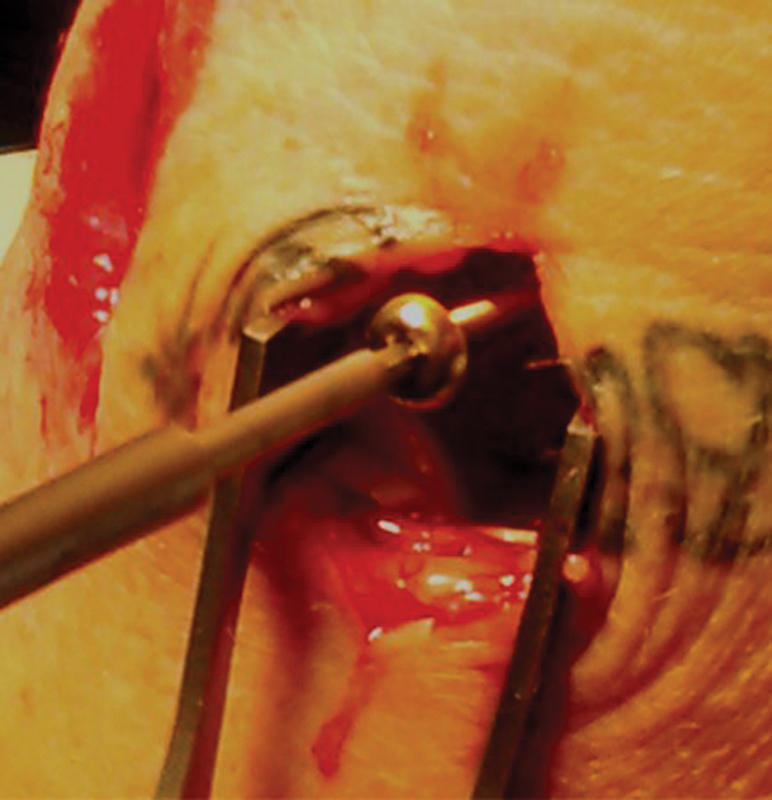
Fig. 17.

Sutures being placed through a rotated very distal volar ulnar fragment of the distal radius. The fragment is rotated so the articular surface faces distally.
Fig. 18.

The sutures are then placed through Acumed's volar lunate suture plate. The sutures are tied after the plate is stabilized to the radial shaft. The plate is used as a buttress to support the small volar fragment.
This plate is commonly used as an adjunct to dorsal plate fixation. Following stabilization of the volar cortex, the standard dorsal approach is made and either a dorsal plate or dorsal fragment–specific plate is utilized (Fig. 19). This plate aligns itself very well with the Acumed standard dorsal plate which is placed along the radial side of the volar radius (Figs. 20 and 21).
Fig. 19.

The patient was extremely large, requiring both the dorsal plate and dorsal lunate plate to support the dorsal comminution.
Fig. 20.

Posterior/anterior radiographs shows anatomic restoration to the joint surface.
Fig. 21.

Lateral radiograph demonstrating a plate sandwich with anatomic restoration to the very comminuted intra-articular fracture to the distal radius.
Divergent Radial Styloid Plate
The divergent radial styloid plate is utilized for fractures of the radial styloid that have metaphyseal comminution or as an adjunct to either volar of dorsal plate fixation when additional support of the radial styloid is required (Fig. 22).
Fig. 22.

Posterior/anterior radiograph of a radial styloid fracture with metaphyseal comminution.
The plate is applied through a standard dorsal radial approach or through the dorsal approach. Care is taken to protect the dorsal sensory branch of the radial nerve. The interval between the first and second dorsal compartments is chosen for placement of the plate. The divergent locking screws with this plate were designed to achieve stable fixation in the presence of styloid comminution. The first screw placed is in the radial shaft in the oblong hole to secure the plate to the bone. Then the distal locking and nonlocking screws may be placed (Fig. 23). The fixed angle arrangement of the plate has been designed to allow the use of this plate in combination with the additional fragment-specific plates without screw interference. In addition, the plate may be used in combination with the standard Acu-Loc volar or dorsal plate (Fig. 24).
Fig. 23.
Stabilization of the radial styloid fracture with the divergent radial styloid plate.
Fig. 24.

Posterior/anterior radiograph showing anatomic restoration to the joint surface with the divergent radial styloid plate and stabilization of a lunate fracture.
Volar Distal Ulna Plate
Ulnar head fractures are relatively rare, occurring in ∼5% of all wrist fractures. While fractures of the head are relatively rare, they can significantly result in limited forearm rotation and hand positioning (Fig. 25). Fractures with significant displacement are best treated by open reduction and internal fixation to prevent loss of forearm rotation. The Acumed volar ulnar plate is designed specifically for fractures of distal head and neck. The plate is usually placed on the volar aspect just proximal to the sigmoid notch to stabilize the ulnar head and allow for full forearm rotation. By placing the plate on the volar aspect, it is surrounded by muscle, making it less symptomatic, requiring fewer potential complications in the future requiring removal of hardware.
Fig. 25.

Posterior/anterior radiograph showing a very comminuted fractures involving both the distal radius and ulna.
The straight ulnar approach is made between the flexor carpi ulnaris and extensor carpi ulnaris tendons. Close attention is made to identify the dorsal sensory branch of the ulnar nerve. The flexor carpi ulnaris and extensor carpi ulnaris tendons are subperiosteally elevated to expose the fracture site. Anatomic reduction of the distal ulnar fracture is performed. Sometimes it is easier to hold the wrist in a straight neutral position to facilitate reduction of the fracture and placement of the plate as compared with full supination of the wrist. Full supination of the wrist makes it easier to place the plate on the volar aspect, but may make reduction of the fracture more difficult.
Once the reduction is performed, the volar ulnar plate is ideally placed on the volar aspect (Fig. 26). The first screw place is a 3.5-mm nonlocking screw in the oval slot of the plate. In this manner, the proximal distal relationship of the plate may be fine-tuned under fluoroscopy. Once the plate is secured to the ulnar shaft, a series of locking, nonlocking, or locking 2.3-mm pegs may be placed in the distal aspect of the plate. Usually, locking screws are utilized. It is important to note that screws cross as they pass into ulnar head for additional stability at the fracture site. It is important to not place the distal screws too long potentially violating the distal radioulnar joint. Usually a screw 2 mm shorter than measured is utilized. At the surgeon's discretion, the plate may be placed in the straight ulnar position if the fracture pattern necessitates this position. If this technique is used, sometimes the opposite-sided plate may fit the fraction pattern better. If the plate is positioned in the straight ulnar position, it may need to be removed in the future as compared with placement of the plate on the volar aspect of the distal ulnar. The remaining 3.5-mm locking screws are placed in the proximal shaft (Fig. 27).
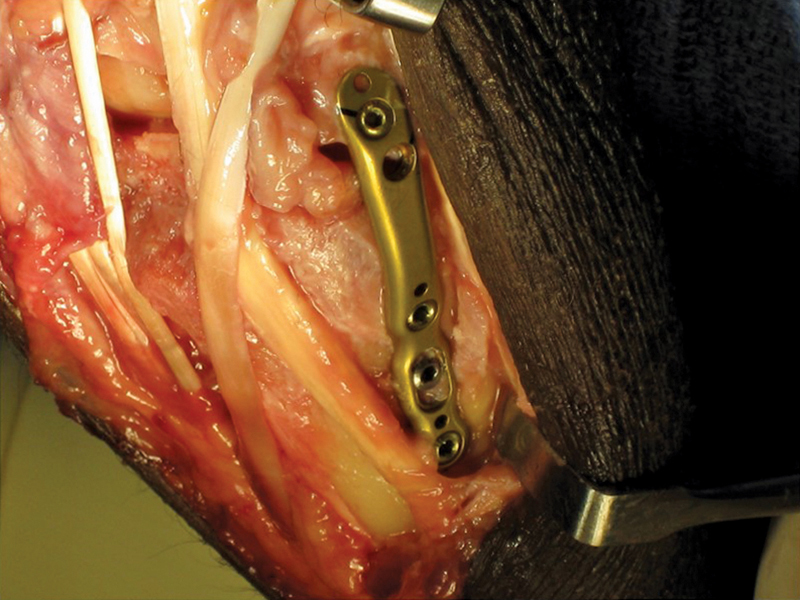
Fig. 26.

Photograph demonstrating placement of the Acumed volar distal ulnar plate placed on the volar aspect of the distal ulna.
Fig. 27.

Posterior/anterior radiograph showing anatomic reduction of both of the distal radius and ulna with the volar distal ulna plate.
Footnotes
Conflict of Interest None.
References
- 1.McKay S D, MacDermid J C, Roth J H, Richards R S. Assessment of complications of distal radius fractures and development of a complication checklist. J Hand Surg Am. 2001;26(5):916–922. doi: 10.1053/jhsu.2001.26662. [DOI] [PubMed] [Google Scholar]
- 2.Catalano L W III, Cole R J, Gelberman R H, Evanoff B A, Gilula L A, Borrelli J Jr. Displaced intra-articular fractures of the distal aspect of the radius. Long-term results in young adults after open reduction and internal fixation. J Bone Joint Surg Am. 1997;79(9):1290–1302. doi: 10.2106/00004623-199709000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Missakian M L, Cooney W P, Amadio P C, Glidewell H L. Open reduction and internal fixation for distal radius fractures. J Hand Surg Am. 1992;17(4):745–755. doi: 10.1016/0363-5023(92)90327-l. [DOI] [PubMed] [Google Scholar]
- 4.Freeland A E, Luber K T. Biomechanics and biology of plate fixation of distal radius fractures. Hand Clin. 2005;21(3):329–339. doi: 10.1016/j.hcl.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 5.Orbay J L, Fernandez D L. Volar fixed-angle plate fixation for unstable distal radius fractures in the elderly patient. J Hand Surg Am. 2004;29(1):96–102. doi: 10.1016/j.jhsa.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 6.Geissler W B. Management distal radius and distal ulnar fractures with fragment specific plate. J Wrist Surg. 2013;2(2):190–194. doi: 10.1055/s-0033-1341409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ring D Prommersberger K Jupiter J B Combined dorsal and volar plate fixation of complex fractures of the distal part of the radius J Bone Joint Surg Am 200587(Suppl 1[Pt 2]):195–212. [DOI] [PubMed] [Google Scholar]
- 8.Rikli D A. Philadelphia, PA: Elsevier; 2009. Dorsal double plating and combined palmar and dorsal plating for distal radius fractures; pp. 125–133. [Google Scholar]
- 9.Simic P M, Robison J, Gardner M J, Gelberman R H, Weiland A J, Boyer M I. Treatment of distal radius fractures with a low-profile dorsal plating system: an outcomes assessment. J Hand Surg Am. 2006;31(3):382–386. doi: 10.1016/j.jhsa.2005.10.016. [DOI] [PubMed] [Google Scholar]
- 10.Fernandez D L, Geissler W B. Treatment of displaced articular fractures of the radius. J Hand Surg Am. 1991;16(3):375–384. doi: 10.1016/0363-5023(91)90001-r. [DOI] [PubMed] [Google Scholar]


