Abstract
Background Nowadays, the wrist is not limited to a dorsal visualization; the joint can be thought of as a “box,” which can be visualized from almost every perspective. The purpose of this study was to describe a new volar central portal for the wrist, following three principles: a single incision that allows access to both the radiocarpal and midcarpal joints, centered on the lunate, with the volar structures at risk protected not only by retractors, but also by tendons.
Description of Technique The incision begins in the distal wrist crease and extended 1.5 cm proximally up to the proximal wrist crease, following the axis of the third intermetacarpal space. The flexor superficialis tendons are identified and retracted toward the radial side. Next, the fourth and fifth flexor digitorum profundus tendons are retracted toward the ulnar side, while the third and second tendons are retracted toward the radial side. The volar central midcarpal portal is performed under direct vision just over the anterior horn of the lunate through the Poirier space. The volar central radiocarpal portal is created under the lunate through the interval between the ulnocarpal ligaments and the short radioulnar ligament.
Methods An anatomical study was performed on 14 cadaver specimens. Two data were recorded: iatrogenic injuries of the structures at risk and the distances to the structures at risk.
Results The median (interquartile range [IQR]) distances from the volar central radiocarpal portal to the median nerve, palmar cutaneous branch of the median nerve, and ulnar neurovascular bundle were 10.5 (7.8–15.0), 18.5 (15.8–20.3), and 7.0 (5.0–10.5) mm, respectively. The median (IQR) distances from the volar central midcarpal portal to the median nerve, palmar cutaneous branch of the median nerve, and ulnar neurovascular bundle were 7.0 (4.8–10.3), 16.0 (14.8–19.0), and 4.5 (3.8–9.0) mm, respectively. No iatrogenic injuries were observed.
Conclusion The volar central portal is reproducible and safe. The risk of iatrogenic injury is low. The capsule is pierced through one of its thinner portions, and both the radiocarpal and midcarpal joints can be inspected through one single incision.
Keywords: wrist arthroscopy, volar central portals, intercarpal ligaments
Although the majority of arthroscopies can be performed adequately through dorsal portals, today the wrist is not limited to a dorsal visualization; the joint can be thought of as a “box,” which can be visualized from almost every perspective.1
The two main volar portals currently used are the volar radial portal2 and the volar ulnar portal.3 They may be useful in some situations to visualize and treat the different structures of the radial and ulnar sides of the wrist, respectively. However, a complete evaluation of the wrist is difficult through only one of them and it can be also difficult to enter into the midcarpal joint through a peripheral portal, without damaging certain important ligaments.
A volar portal centered on the lunate could allow a complete evaluation of both the midcarpal and radiocarpal joints, and could be useful when performing certain surgical techniques. Thus, the purpose of this study was to describe a volar central portal of the radiocarpal and midcarpal joints that follows three principles and check its safety with an anatomical study.
The following three principles were used to define the portal:
A single incision should allow access to both the radiocarpal and midcarpal joints.
Both the radiocarpal and midcarpal portals should be centered on the lunate, allowing the capsule to be broken through a less resistant portion and the complete joint to be easily inspected.
The volar structures at risk should be protected not only by retractors, but also by tendons, to minimize the risk of injury.
Surgical Technique
With the hand suspended from a traction tower with 4.5 to 6 kg of countertraction, standard dorsal radiocarpal and midcarpal portals are created.
The cutaneous incision is located centered on the lunate and had to be long enough to allow access to both the radiocarpal and midcarpal joints. The incision begins in the distal wrist crease, which corresponds with the midcarpal joint, and extended 1.5 cm proximally up to the proximal wrist crease, which corresponds with the radiocarpal joint. The incision follows the axis of the third intermetacarpal space, just ulnar to the palmaris longus tendon (Fig. 1).
Fig. 1.
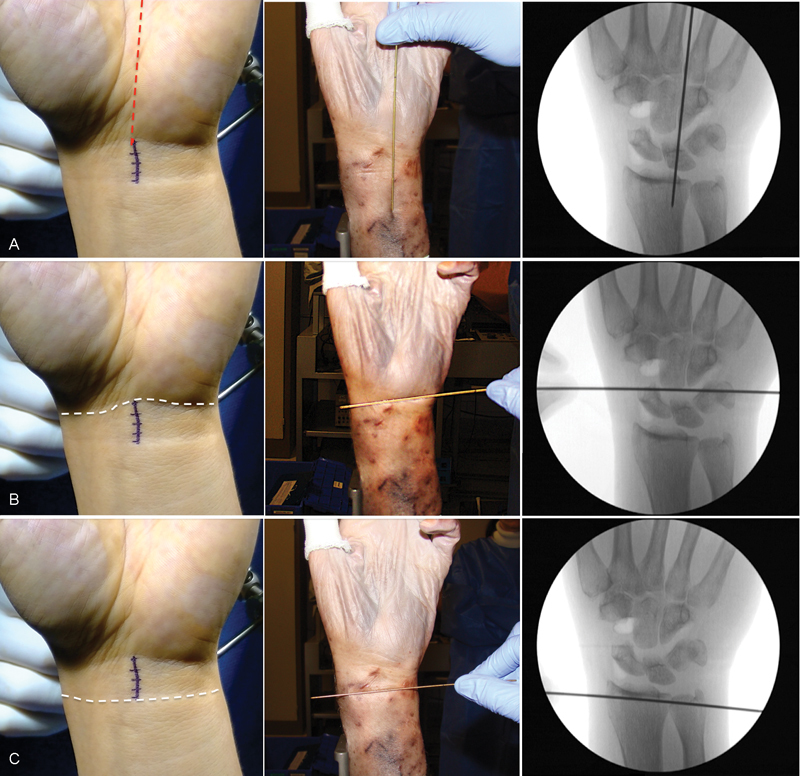
References for the cutaneous incision. (A) Third intermetacarpal space. (B) Distal wrist flexion crease. (C) 1.5 cm proximal to the distal wrist flexion crease.
The first structures encountered are the flexor digitorum superficialis (FDS) tendons. The fifth FDS tendon is identified and retracted with the rest of the flexor superficialis tendons toward the radial side. As there are no finger traps in the fifth finger, the fifth FDS tendon could be easily located by tractioning of the tendon and observing the flexion of the fifth finger.
The next structures encountered in depth are the flexor digitorum profundus (FDP) tendons. The plane between the third and fourth tendons is identified, and the fourth and fifth FDP tendons are retracted toward the ulnar side, while the third and second tendons are retracted toward the radial side. In this way, the capsular plane is reached and can be easily observed by transillumination (Fig. 2).
Fig. 2.
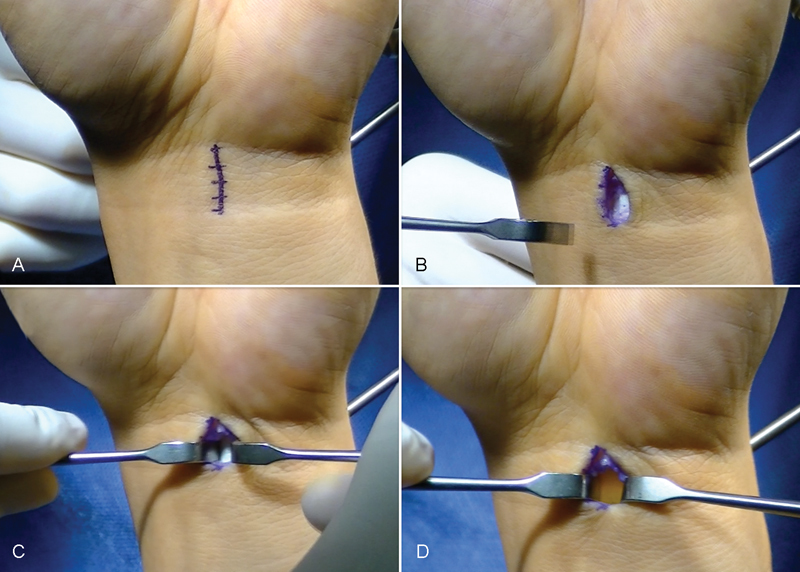
Surgical technique. (A) Cutaneous incision. (B) The flexor digitorum superficialis tendons. (C) The fourth and fifth flexor profundus tendons. (D) The volar capsule easily seen by transillumination.
Establishment of the Volar Central Midcarpal Portal
With the scope in the ulnar midcarpal portal, a 22-gauge needle is introduced just over the anterior horn of the lunate. Using the tip of a number 11 scalpel, the volar capsule is incised and then widened by blunt forceps. A 2.4-mm-wide Kirschner wire is used as a Wissinger rod, and the arthroscopy sheath was introduced into the midcarpal joint following the wire (Fig. 3). The complete joint is visualized by a subtle movement of the scope and by turning the camera from the radial to the ulnar side (Fig. 4).
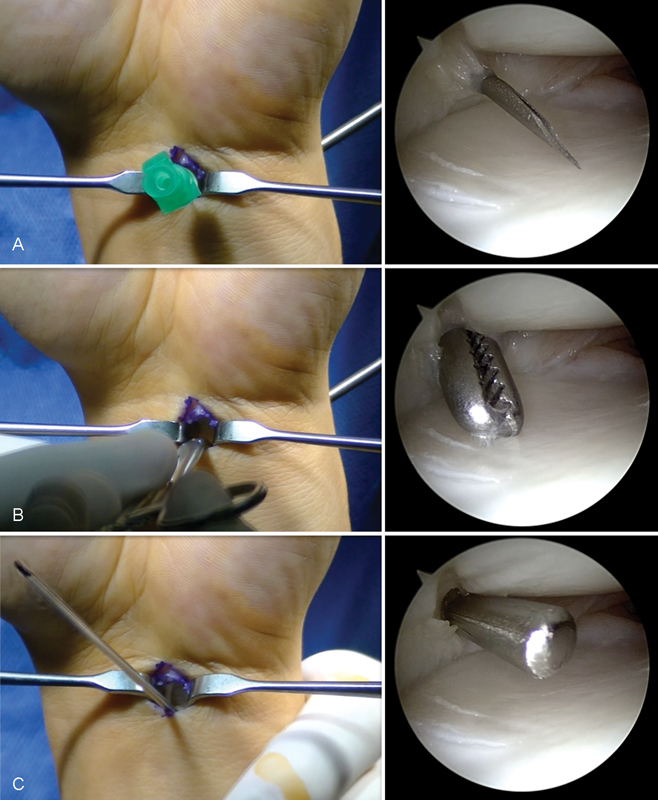
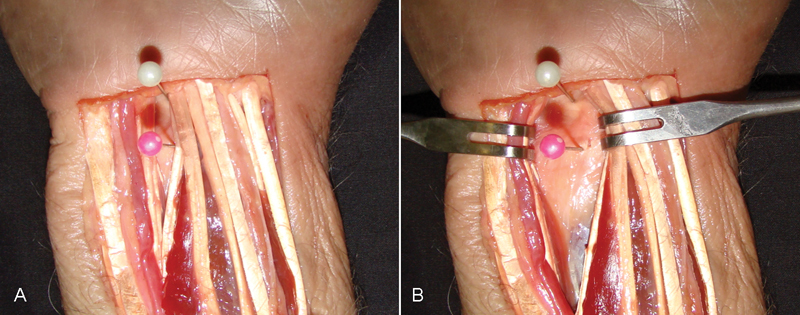
Fig. 3.
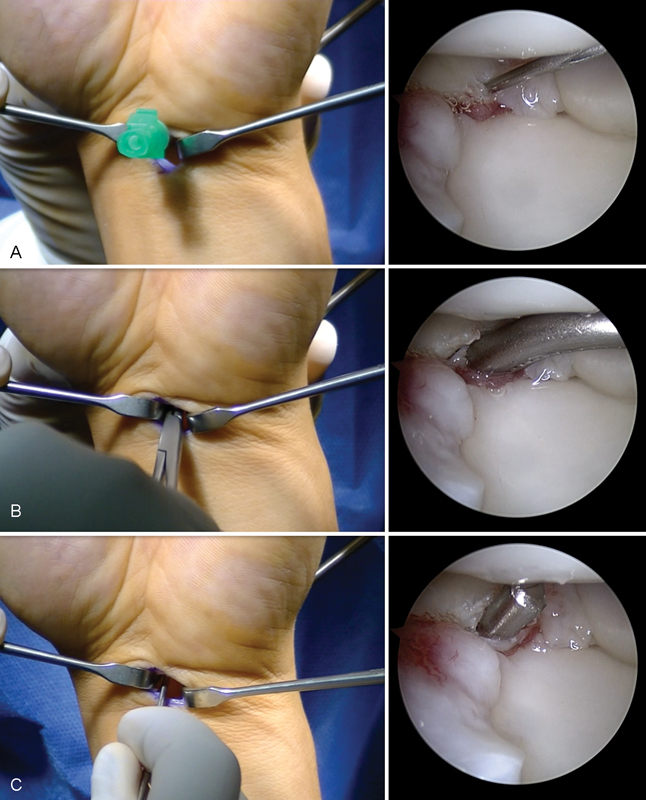
Establishment of the volar central midcarpal portal. (A) Scope in the ulnar midcarpal portal; a 22-gauge needle was introduced just over the anterior horn of the lunate. (B) The volar capsule was incised and then widened by blunt forceps. (C) A 2.4-mm-wide Kirschner wire was used as a Wissinger rod.
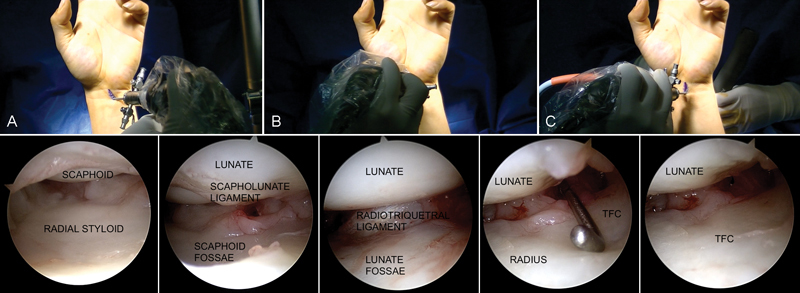
Fig. 4.
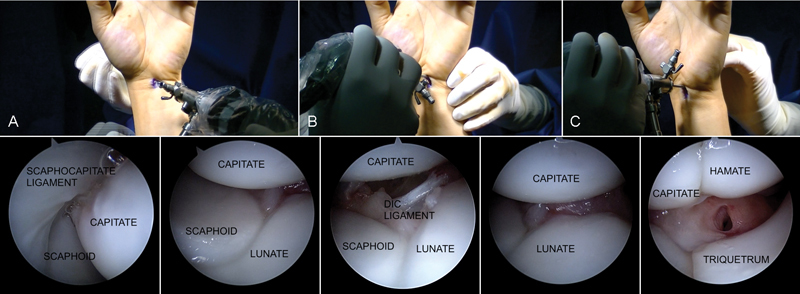
(A) Radial portion of the midcarpal joint. (B) Central portion of the midcarpal joint. (C) Ulnar portion of the midcarpal joint. DIC ligament: dorsal intercarpal ligament.
Establishment of the Volar Central Radiocarpal Portal
The volar central radiocarpal portal is created similarly to the midcarpal portal. In brief, with the arthroscope in the 6R portal, a 22-gauge needle is introduced just under the lunate. The volar capsule is incised using the tip of a number 11 scalpel and then widened by blunt forceps. A 2.4-mm Kirschner wire is used as a Wissinger rod, and the arthroscopy sheath is introduced into the radiocarpal joint following the wire (Fig. 5). By moving the arthroscope and turning the camera toward the radial or ulnar side, the complete radiocarpal joint could be visualized (Fig. 6).
Fig. 5.
Establishment of the volar central radiocarpal portal. (A) Scope in the 6R portal; a 22-gauge needle was introduced just under the lunate. (B) The volar capsule was incised and then widened by blunt forceps. (C) A 2.4-mm Kirschner wire was used as a Wissinger rod.
Fig. 6.
(A) Radial portion of the radiocarpal joint. (B) Central portion of the radiocarpal joint. (C) Ulnar portion of the radiocarpal joint.
The technique of the volar central portal can be seen in Video 1.
Video 1
Surgical technique of the volar central portal. The video is divided into three headings. (1) Surgical approach. (2) Establishment of the volar central radiocarpal portal. (3) Establishment of the volar central midcarpal portal. Online content including video sequences viewable at: https://www.thieme-connect.com/products/ejournals/html/10.1055/s-0035-1570741.
Materials and Methods
An anatomical study was performed to check the safety of the portal.
A total of 7 pairs of frozen human cadavers (14 upper limbs) were examined. There were four male and three female cadavers, with a mean age of 64 years (range, 45–80 years). The clinical histories of all cadavers were available, and no subject had a history of upper limb joint surgery.
The arterial system was injected with red latex for visualization. Using standard dissection tools and retractors, the radiocarpal and midcarpal volar portals were created as described below.
The incision began at the distal wrist flexion crease and extended 1.5 cm proximally, following the third intermetacarpal space.
The first structures encountered were the FDS tendons. The fifth FDS tendon was identified and retracted with the rest of the flexor superficialis tendons toward the radial side. The next structures encountered were the FDP tendons. The plane between the third and fourth tendons was identified, and the fourth and fifth FDP tendons were retracted toward the ulnar side, while the third and second tendons were retracted toward the radial side. In this way, the capsular plane was reached.
A needle in the radiocarpal portal and a needle in the midcarpal portal were left in place after the portals were created (Fig. 7). The correct position of the needles in both the midcarpal and radiocarpal joints was checked through a dorsal capsulotomy.
Fig. 7.
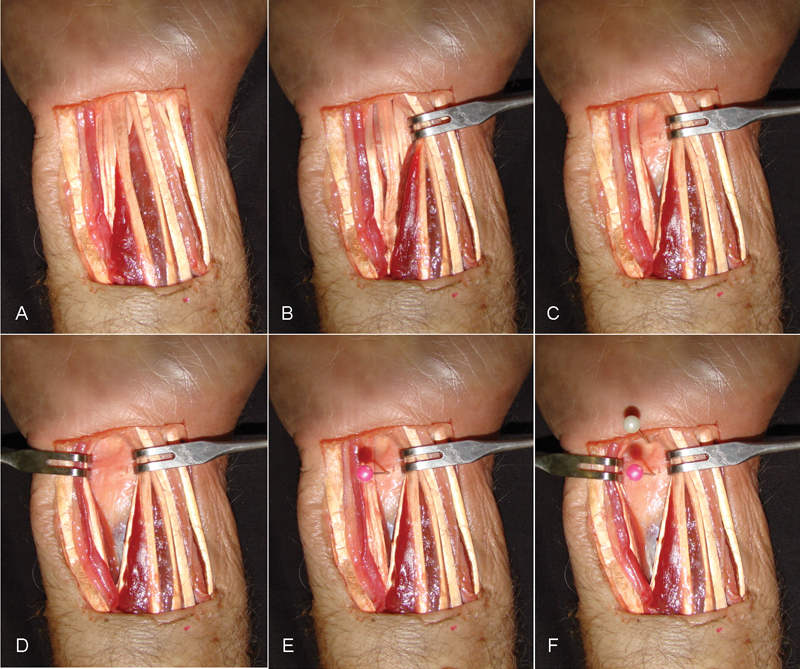
(A) Anatomical dissection of the volar wrist. (B) The flexor digitorum superficialis tendons were retracted toward the radial side. (C) The second and third flexor digitorum profundus tendons were retracted toward the radial side. (D) The fourth and fifth flexor digitorum profundus tendons were retracted toward the ulnar side. (E) Pink needle in the radiocarpal portal. (F) White needle in the midcarpal portal.
The specimens were dissected under 2.5 power loupe magnification to study the periportal anatomy. The structures considered at risk included the median nerve, the superficial branch of the median nerve, and the ulnar neurovascular bundle.
Two data were recorded and analyzed: first the presence of any injury of the structures at risk and second the distances to these structures from the radiocarpal and midcarpal portal. These distances were measured as the shortest distance from the needle (located in the radiocarpal or midcarpal portal) to the structure at risk, going ulnar to radial in the same anatomical plane of the structure (Fig. 8). Measurements were made with a universal caliper (Tesa, Renens, Switzerland) by (M.O.) and observed by (F.C.) and (T.V.) to ensure quality control. All the measures were obtained after removing the retractors. Despite the fact that the portal was created using retractors (the same as in real practice), we decided to measure the distances without them to notice which structure was at higher risk. However, we can be sure that the distances to the structures at risk in real practice are longer (Fig. 9).
Fig. 8.
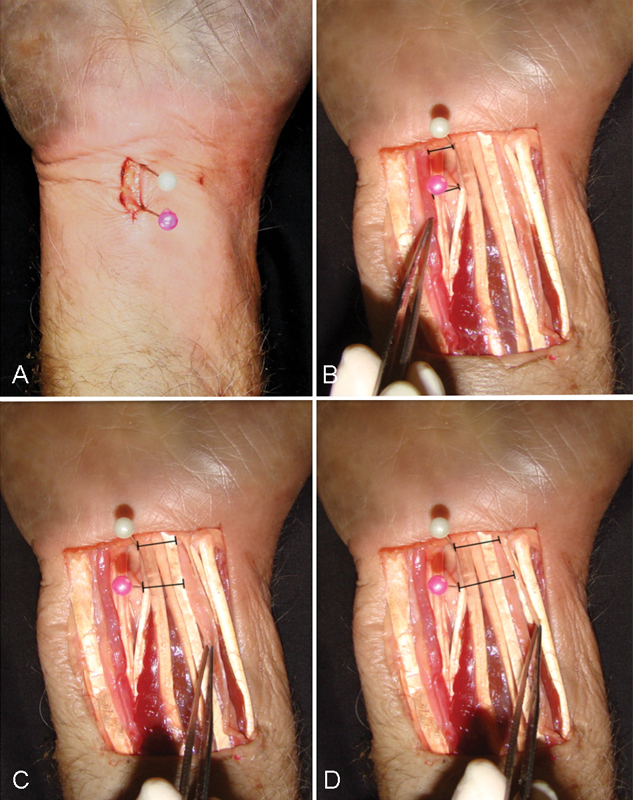
The shortest distance from the needle (located in the radiocarpal and midcarpal portal) to the structure at risk. (A) Radiocarpal (pink needle) and midcarpal (white needle) portals. (B) Ulnar neurovascular bundle. (C) Median nerve. (D) Palmar cutaneous branch of the median nerve.
Fig. 9.
The distances from the needle (located in the radiocarpal and midcarpal portal) to the structure at risk. (A) Without retractors. (B) With retractors.
Statistical Analysis
SPSS software for Windows (version 18.0; SPSS, Chicago, IL) was used for the statistical analysis. Nonparametric statistical tests were used because of the small sample and the fact that the values were not normally distributed; and these values were expressed as median and interquartile range (IQR). The Wilcoxon signed-rank test was used to perform paired comparisons of portals. Correction of statistical significance was not used. Statistical significance was defined as p < 0.05. Power analysis was not performed because there have been no similar previous studies, and we did not know what effect size to expect.
Results
There were no iatrogenic damages to the flexor tendons, the median nerve, the palmar cutaneous branch of the median nerve, or the ulnar neurovascular bundle in any of the cadavers.
The median (IQR) distances from the volar central radiocarpal portal to the median nerve, palmar cutaneous branch of the median nerve, and ulnar neurovascular bundle were 10.5 (7.8–15.0), 18.5 (15.8–20.3), and 7.0 (5.0–10.5) mm, respectively (Table 1).
Table 1. Distances (millimeters) from the volar central radiocarpal portal to the volar structures at risk.
| Volar central radiocarpal portal distances (mm) | |||
|---|---|---|---|
| Median nerve | Palmar cutaneous branch of the median nerve | Ulnar neurovascular bundle | |
| Case 1 | 15 | 20 | 6 |
| Case 2 | 11 | 20 | 5 |
| Case 3 | 8 | 13 | 12 |
| Case 4 | 7 | 16 | 4 |
| Case 5 | 18 | 21 | 30 |
| Case 6 | 8 | 15 | 7 |
| Case 7 | 20 | 21 | 10 |
| Case 8 | 10 | 20 | 5 |
| Case 9 | 9 | 19 | 3 |
| Case 10 | 6 | 17 | 15 |
| Case 11 | 11 | 18 | 8 |
| Case 12 | 15 | 21 | 6 |
| Case 13 | 11 | 16 | 7 |
| Case 14 | 6 | 12 | 8 |
| Median (IQR) | 10.5 (7.8–15.0) | 18.5 (15.8–20.3) | 7.0 (5.0–10.5) |
Abbreviation: IQR, interquartile range.
The median (IQR) distances from the volar central midcarpal portal to the median nerve, palmar cutaneous branch of the median nerve, and ulnar neurovascular bundle were 7.0 (4.8–10.3), 16.0 (14.8–19.0), and 4.5 (3.8–9.0) mm, respectively (Table 2).
Table 2. Distances (millimeters) from the volar central midcarpal portal to the volar structures at risk.
| Volar central midcarpal portal distances (mm) | |||
|---|---|---|---|
| Median nerve | Palmar cutaneous branch of the median nerve | Ulnar neurovascular bundle | |
| Case 1 | 10 | 19 | 4 |
| Case 2 | 12 | 22 | 2 |
| Case 3 | 7 | 18 | 6 |
| Case 4 | 5 | 17 | 4 |
| Case 5 | 3 | 16 | 26 |
| Case 6 | 4 | 15 | 3 |
| Case 7 | 15 | 16 | 8 |
| Case 8 | 10 | 20 | 4 |
| Case 9 | 9 | 19 | 2 |
| Case 10 | 5 | 11 | 12 |
| Case 11 | 7 | 16 | 4 |
| Case 12 | 11 | 15 | 5 |
| Case 13 | 4 | 14 | 15 |
| Case 14 | 5 | 13 | 6 |
| Median (IQR) | 7.0 (4.8–10.3) | 16.0 (14.8–19.0) | 4.5 (3.8–9.0) |
Abbreviation: IQR, interquartile range.
Paired comparisons using the Wilcoxon signed-rank test showed that the radiocarpal portal was safer than the midcarpal portal in terms of the distances to the median nerve (p = 0.004) and ulnar neurovascular bundle (p = 0.023). However, due to the small number of limbs examined, no significant differences were found regarding the distance to the palmar cutaneous branch (p = 0.152) (Table 3).
Table 3. Results of statistical analysis using multiple Wilcoxon signed-rank tests to perform paired comparisons for volar central portals regarding their distance to the structures at risk.
| Radiocarpal portal | Midcarpal portal | p | |
|---|---|---|---|
| n = 14 | n = 14 | ||
| Median nerve | 10.5 (7.8–15.0) | 7.0 (4.8–10.3) | 0.004 |
| Palmar cutaneous branch | 18.5 (15.8–20.3) | 16.0 (14.8–19.0) | 0.152 |
| Ulnar neurovascular bundle | 7.0 (5.0–10.5) | 4.5 (3.8–9.0) | 0.023 |
Note: Data are presented as the median (interquartile range) distances from the portals to the structures at risk (mm).
Discussion
The description of a new volar portal centered on the lunate could improve the visualization of the wrist from volar and help in the development and improvement of wrist arthroscopy techniques.
Before Slutsky's description of the volar radial and volar ulnar portals in 2002,2 few studies have described the utility of volar portals. In 1994, Jantea et al, using cadavers, described two ulnar radiocarpal portals that were medial and lateral to the flexor carpi ulnaris tendon.4 Moreover, in 1999, Tham et al described a radial portal under the flexor carpi radialis sheath, for radial styloidectomy, synovectomy, and arthroscopic-assisted fracture reduction.5
More recently, Slutsky described two volar portals in detail.2 3 Both these portals were created through a 2-cm skin incision. The radial portal was created under the flexor carpi radialis sheath, and the entry point to the radiocarpal joint was located between the radioscaphocapitate (RSC) ligament and the long radiolunate (LRL) ligament in four specimens, and through the LRL ligament in one specimen. The pathologies in 10/30 patients that were not visible from a dorsal portal included hypertrophic synovitis of the dorsal capsule, avulsion of the RSC ligament, and tears of the palmar region of the scapholunate ligament and dorsal radiocarpal ligament.2
On the other hand, the volar ulnar portal was created under the flexor tendons, and its approach ran between the ulnar neurovascular bundle and all the flexor digitorum tendons. The entry point to the radiocarpal joint was through the ulnolunate ligament adjacent to the radial insertion of the triangular fibrocartilage. The author discovered tears extending into the palmar aspect of the lunotriquetral ligament, which were not seen from a dorsal portal, in 8/23 patients.3
In the present study, the skin incision used for the volar central portal was located just ulnar to the palmaris longus tendon. This is similar to the skin incision used for the ulnar volar portal described above, but is located more radial.
At the level of the radiocarpal and midcarpal portal, the FDS tendons are more radial than the FDP tendons, and as the bigger insertion of the muscle belly is located in the radius bone, it is really easy to retract all the FDS tendons radially. The FDP tendons extend more ulnar at the level of the portal and it is more difficult to retract all the tendons radially, because the bigger insertion of the muscle belly is in the ulnar bone. Therefore, great force should be applied to reach the lunate bone. Furthermore, the interval between the 3 and 4 FDP is located just in front of the lunate bone. That is why this approach has been chosen.
The volar capsule has many resistant ligaments that form an inverted “v.” The distal portion of this “v” is the arcuate ligament, whose radial and ulnar components are the scaphocapitate (SC) and triquetrohamocapitate (THC) ligaments, respectively.6 If the volar entrance into the midcarpal joint is performed in its radial or ulnar side, both the SC and THC ligaments are at risk of injury. These ligaments are highly important structures, as lesions of these ligaments are known to cause midcarpal instability.7 Conversely, the volar central portal pierces the volar capsule over the anterior horn of the lunate, proximal to the arcuate ligament, just in the Poirier space, thus avoiding injury to the SC and THC ligaments (Fig. 10).
Fig. 10.
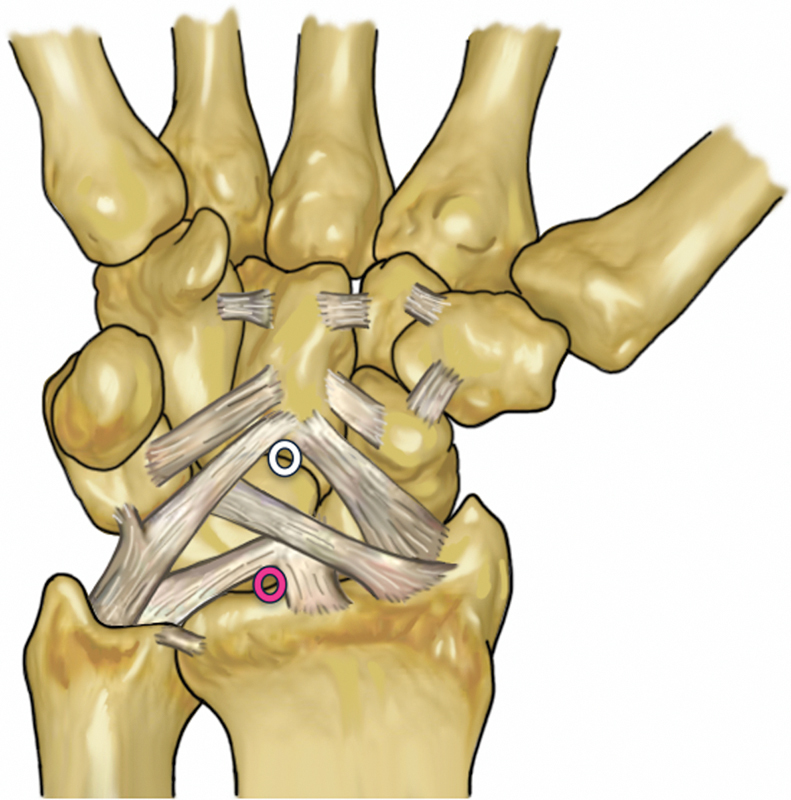
Volar ligaments of the wrist. The white circle indicates the volar central midcarpal portal, located in the anterior horn of the lunate under the scaphocapitate and triquetrohamocapitate ligaments. The pink circle indicates the volar central radiocarpal portal, located under the lunate through the interval between the ulnocarpal ligaments and the short radioulnar ligaments.
At the radiocarpal joint, the RSC and ulnocarpal ligaments (ulnotriquetral, ulnocapitate, and ulnolunate ligaments) form the proximal origin of the inverted “v,” paralleling the course of the arcuate ligament. The functions of the RSC ligament include constraint against radiocarpal pronation and ulnocarpal translocation, and stabilization of the distal pole of the scaphoid.8 9 The ulnocarpal ligaments are likely to be stretched tensely in wrist radial extension,10 and this extension seems to be equivalent to the extension phase of the dart-throw motion in the wrist.11 Injuries to these ligaments have been demonstrated to cause type IC lesions of the triangular fibrocartilage complex (TFCC).12 As the volar central portal is created under the lunate through the interval between the ulnocarpal ligaments and the short radioulnar ligament, the risk of damage to the RSC or ulnocarpal ligaments is minimized (Fig. 10).
When the portal is created, the real distances to the structures at risk are much longer than the measures obtained in cadaver studies, as retractors are used to move them away. Hence, despite the proximity of the structures at risk, no injuries have been reported with the use of this portal, and it is thus considered safe when performed in the method described herein. However, as demonstrated in the present study, the risks associated with the use of a midcarpal portal are greater than those with a radiocarpal portal. Thus, great care should be taken during dissection at the distal portion of the incision. We recommend beginning the dissection in the proximal side, being conscious that the ulnar neurovascular bundle is the structure at higher risk, and hence always the soft tissues dissection should be performed in a longitudinal manner until the tendons are identified.13
We believe that these portals may be useful while performing some techniques, especially certain advanced techniques such as ligamentoplasties,13 arthroscopic arthrodesis,14 15 proximal row carpectomies,16 and others.17
To date, we have used the volar central portal in 21 arthroscopic ligamentoplasties of the scapholunate ligament,13 6 arthroscopic dorsal ganglionectomies, 3 arthroscopic radioscapholunate arthrodesis, 1 four-corner arthrodesis, 2 arthroscopic arthrolysis of the wrist, 2 sutures of the dorsal portion of the TFCC, and 3 arthroscopic proximal row carpectomies. The advantage of this portal in arthroscopic scapholunate ligamentoplasties is that using the portal it is easy to pass the graft through the lunate and close the scapholunate graft by tractioning from volar. The advantage of using the volar central portal in arthroscopic arthrodesis and proximal row carpectomies is that it is easy to visualize and remove or decorticate the dorsal portions of the carpal bone and that a “third” portal in the midcarpal joint helps a lot because two instruments can be used simultaneously in the joint (such as periosteal elevator and rongeur). Finally, the advantage of using the portal in dorsal ganglionectomies or in the repair of the dorsal portion of the TFCC is that it is easy to visualize these lesions just from the opposite side instead of from a peripheral side. However, we are currently collecting and analyzing these data, and the results of this prospective clinical series will be reported.
In conclusion, we found that volar central portals are reproducible and safe when performed through a 1.5-cm longitudinal incision. In this portal, a single incision allows access to the radiocarpal and midcarpal joints, the capsule is pierced through one of its thinner portions, and the volar structures at risk are protected not only by retractors, but also by tendons. We are currently using the volar central portal as a working or visualization portal in many techniques, especially in certain advanced techniques, and we believe that this portal may aid in the development of future indications and techniques in wrist arthroscopy.
Footnotes
Conflict of Interest None.
References
- 1.Bain G I, Munt J, Turner P C. New advances in wrist arthroscopy. Arthroscopy. 2008;24(3):355–367. doi: 10.1016/j.arthro.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 2.Slutsky D J. Wrist arthroscopy through a volar radial portal. Arthroscopy. 2002;18(6):624–630. doi: 10.1053/jars.2002.34106. [DOI] [PubMed] [Google Scholar]
- 3.Slutsky D J. The use of a volar ulnar portal in wrist arthroscopy. Arthroscopy. 2004;20(2):158–163. doi: 10.1016/j.arthro.2003.11.015. [DOI] [PubMed] [Google Scholar]
- 4.Jantea C L, McCarthy D M, Herndon J H, Horikoshi M. Palmar approaches/portals for arthroscopy of the wrist. Arthroskopie. 1994;7:225–231. [Google Scholar]
- 5.Tham S, Coleman S, Gilpin D. An anterior portal for wrist arthroscopy. Anatomical study and case reports. J Hand Surg [Br] 1999;24(4):445–447. doi: 10.1054/jhsb.1999.0166. [DOI] [PubMed] [Google Scholar]
- 6.Chang W, Peduto A J, Aguiar R O, Trudell D J, Resnick D L. Arcuate ligament of the wrist: normal MR appearance and its relationship to palmar midcarpal instability: a cadaveric study. Skeletal Radiol. 2007;36(7):641–645. doi: 10.1007/s00256-006-0251-9. [DOI] [PubMed] [Google Scholar]
- 7.Lichtman D M, Wroten E S. Understanding midcarpal instability. J Hand Surg Am. 2006;31(3):491–498. doi: 10.1016/j.jhsa.2005.12.014. [DOI] [PubMed] [Google Scholar]
- 8.McAdams T R, Srivastava S. Arthroscopic evaluation of scaphoid waist fracture stability and the role of the radioscaphocapitate ligament. Arthroscopy. 2004;20(2):152–157. doi: 10.1016/j.arthro.2003.11.023. [DOI] [PubMed] [Google Scholar]
- 9.Ritt M J, Stuart P R, Berglund L J, Linscheid R L, Cooney W P III, An K N. Rotational stability of the carpus relative to the forearm. J Hand Surg Am. 1995;20(2):305–311. doi: 10.1016/s0363-5023(05)80031-0. [DOI] [PubMed] [Google Scholar]
- 10.Moritomo H, Murase T, Arimitsu S, Oka K, Yoshikawa H, Sugamoto K. Change in the length of the ulnocarpal ligaments during radiocarpal motion: possible impact on triangular fibrocartilage complex foveal tears. J Hand Surg Am. 2008;33(8):1278–1286. doi: 10.1016/j.jhsa.2008.04.033. [DOI] [PubMed] [Google Scholar]
- 11.Wolfe S W, Crisco J J, Orr C M, Marzke M W. The dart-throwing motion of the wrist: is it unique to humans? J Hand Surg Am. 2006;31(9):1429–1437. doi: 10.1016/j.jhsa.2006.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Palmer A K. Triangular fibrocartilage complex lesions: a classification. J Hand Surg Am. 1989;14(4):594–606. doi: 10.1016/0363-5023(89)90174-3. [DOI] [PubMed] [Google Scholar]
- 13.Corella F, Del Cerro M, Ocampos M, Larrainzar-Garijo R. Arthroscopic ligamentoplasty of the dorsal and volar portions of the scapholunate ligament. J Hand Surg Am. 2013;38(12):2466–2477. doi: 10.1016/j.jhsa.2013.09.021. [DOI] [PubMed] [Google Scholar]
- 14.Ho P C. Arthroscopic partial wrist fusion. Tech Hand Up Extrem Surg. 2008;12(4):242–265. doi: 10.1097/BTH.0b013e318190244b. [DOI] [PubMed] [Google Scholar]
- 15.del Piñal F, Klausmeyer M, Thams C, Moraleda E, Galindo C. Early experience with (dry) arthroscopic 4-corner arthrodesis: from a 4-hour operation to a tourniquet time. J Hand Surg Am. 2012;37(11):2389–2399. doi: 10.1016/j.jhsa.2012.08.026. [DOI] [PubMed] [Google Scholar]
- 16.Weiss N D, Molina R A, Gwin S. Arthroscopic proximal row carpectomy. J Hand Surg Am. 2011;36(4):577–582. doi: 10.1016/j.jhsa.2011.01.009. [DOI] [PubMed] [Google Scholar]
- 17.Abe Y, Doi K, Hattori Y, Ikeda K, Dhawan V. Arthroscopic assessment of the volar region of the scapholunate interosseous ligament through a volar portal. J Hand Surg Am. 2003;28(1):69–73. doi: 10.1053/jhsu.2003.50020. [DOI] [PubMed] [Google Scholar]


