Abstract
Background Headless screw fixation of scaphoid fractures and nonunions yields predictably excellent outcomes with a relatively low complication profile. However, intramedullary implants affect the load to failure and stress distribution within bone and may be implicated in subsequent fracture.
Case Description We describe a posttraumatic fracture pattern of the scaphoid proximal pole originating at the previous headless screw insertion site in three young male patients with healed scaphoid nonunions. Each fracture was remarkably similar in shape and size, comprised the volar proximal pole, and was contiguous with the screw entry point. Treatment was challenging but successful in all cases.
Literature Review Previous reports have posited that stress-raisers secondary to screw orientation may be implicated in subsequent peri-implant fracture of the femoral neck. Repeat scaphoid fracture after screw fixation has also been reported. However, the shape and locality of secondary fracture have not been described, nor has the potential role of screw fixation in the production of distinct fracture patterns.
Clinical Relevance Hand surgeons must be aware of this difficult complication that may follow antegrade headless screw fixation of scaphoid fracture nonunion, and of available treatment strategies.
Keywords: scaphoid nonunion, refracture, internal fixation, complication, peri-implant
Nondisplaced scaphoid waist fractures may be managed nonoperatively, but require strict and prolonged immobilization. Fracture nonunion is a troublesome complication that leads to prolonged casting or secondary surgery and, if untreated, to carpal collapse and degenerative arthritis.1 2 Unstable or displaced fractures, fracture-dislocations, and fractures involving the proximal pole require anatomic reduction with rigid fixation. Modern headless compression screws demonstrate high union rates, rapid recovery, and good-to-excellent outcomes in most series.1 3 4 5 6 7 8 We were unable to identify reports detailing the potential for secondary proximal pole fracture following scaphoid screw fixation.
In this series we describe three young men with scaphoid fracture nonunion that healed after antegrade headless compression screw fixation (Acumed, Hillsboro, OR, USA). Months later, the men presented with secondary fracture of the proximal pole (Table 1). A consistently proximal and volar fracture pattern was observed that was contiguous with the screw insertion site. The purpose of this case series is to report our experience and raise awareness of a possible risk of retained hardware following antegrade scaphoid nonunion fixation, offer treatment strategies, and report outcomes.
Table 1. Patient information.
| Case | Age, Sex (M/F), & dominance (R/L) | Time between injury & first operation | Nonunion site | Original hardware |
Time between repair & 2nd fracture | Secondary fracture location | Secondary procedure |
|---|---|---|---|---|---|---|---|
| 1 | 15 M R | 3.5 months | L scaphoid waist | 22-mm Acutrak Mini | 7 months | Volar proximal pole | Fixation, allografting, and autogenous vascularized bone grafting |
| 2 | 16 M R | 15 months | R scaphoid waist | 20-mm Acutrak II | 8 months | Volar proximal pole | Scaphoid excision, four-corner arthrodesis |
| 3 | 17 M L | 2.5 months | L scaphoid proximal pole | 18-mm Acutrak II Mini |
13 months | Volar proximal pole | Fixation and autogenous bone grafting |
Case 1
A 15-year-old right-handed lacrosse player presented to our institution after 3.5 months of sport-related left wrist pain had not abated. A scaphoid fracture had been treated as a wrist sprain for 3.5 months with rest and splinting at an outside facility before computed tomography (CT) performed at our institution revealed a scaphoid waist fracture nonunion (Fig. 1a). The nonunion was treated with bone grafting and insertion of a 22-mm Acutrak Mini headless compression screw through a dorsal antegrade approach (Fig. 1b). At 3 months postoperative the patient was pain-free. High-resolution CT confirmed bony union9 (Fig. 1c).
Fig. 1.
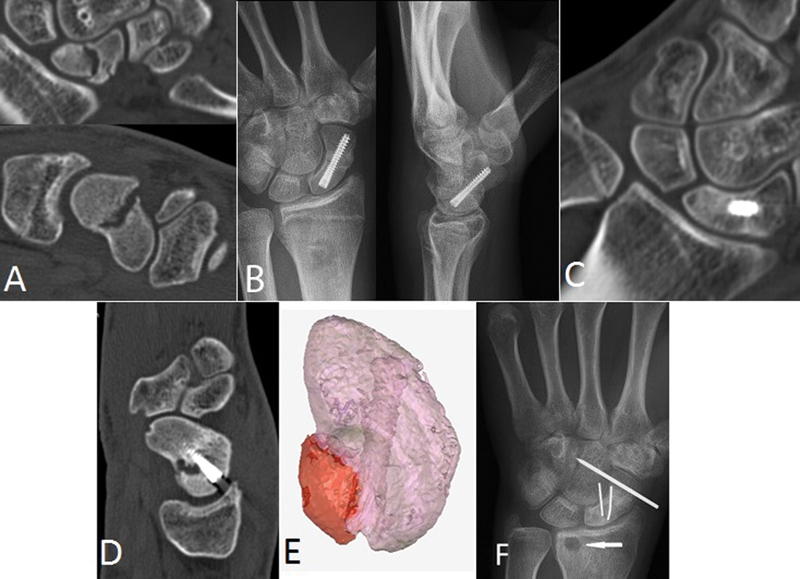
Case 1. (a) Sagittal and coronal CT images of the original mid-waist fracture nonunion. (b) Posteroanterior (PA) and lateral postoperative radiographs show central placement. (c) CT coronal view demonstrating healing at 3 months. (d) Posttraumatic CT sagittal view 4 months after healing demonstrates new fracture and cyst. (e) 3D model rendered from CT data with Mimics software (Materialise, Leuven, Belgium) shows fracture fragment (red) arising about the screw entry site. (f) Postoperative radiographs following secondary repair. A volar cortical defect from Mathoulin grafting is indicated by the arrow.
Four months later, the patient presented with new-onset wrist pain after falling multiple times onto a hyperextended hand while snowboarding. CT revealed an incomplete 8.92-mm × 14.22-mm proximal pole volar marginal shear fracture fragment comprising 17.1% of total scaphoid volume and a cystic defect (Fig. 1d, e). A combined dorsal-volar approach exposed a proximal pole fracture that extended to the screw entry point. The dorsal approach allowed for screw removal and packing of the screw tract with demineralized bone matrix putty (Grafton DBM, BioHorizons, Birmingham, AL, USA); the volar approach was used to pack the cyst cavity and inset a vascularized Mathoulin bone graft from the volar distal radius.10 Two Kirschner wires (K-wires) were utilized to fix the scaphoid and a third to immobilize the distal pole to the capitate for increased stability. The patient was immobilized with a thumb spica cast for 6 weeks, followed by removable splinting for an additional 6 weeks until healing. K-wires were removed at 3 months postoperative when repeat CT demonstrated fracture union (Fig. 1f). The patient returned to school and lacrosse 6.5 months postoperatively with excellent functional recovery and range of motion (ROM) nearly identical to the contralateral wrist.
Case 2
A 16-year-old right-handed football player sustained a hyperextension injury of his dominant wrist during play. Magnetic resonance imaging (MRI) performed at the end of the season at an outside facility revealed a nondisplaced scaphoid waist fracture, and the patient was casted for 8 weeks before being released back to football. Fifteen months after initial injury, the patient presented to our institution with continued wrist pain aggravated by lifting and football. MRI revealed a minimally displaced scaphoid waist nonunion (Fig. 2a). The nonunion was managed through a dorsal approach with curettage, autogenous bone grafting from the ipsilateral dorsal radius, and antegrade insertion of a 20-mm Acutrak II headless compression screw (Fig. 2b). CT imaging 5 months postoperative confirmed fracture union (Fig. 2c).
Fig. 2.
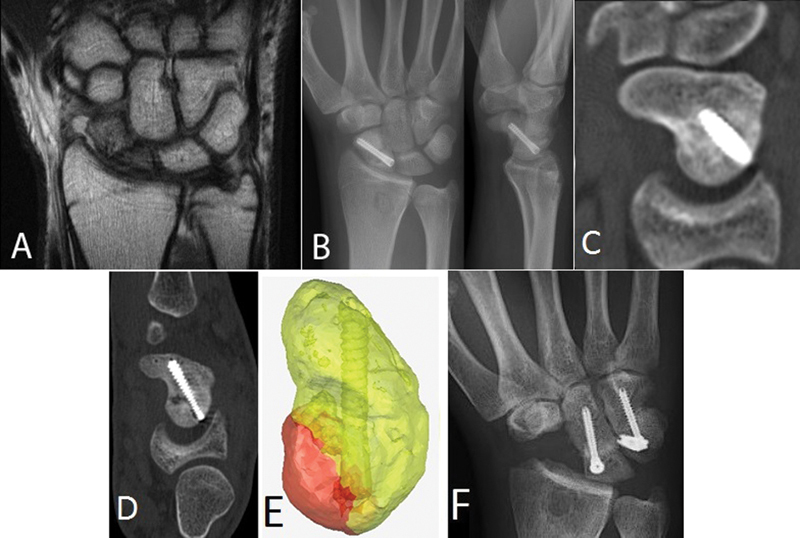
Case 2. (a) MRI 15 months postinjury demonstrates scaphoid midwaist nonunion. (b) Postoperative radiographs demonstrate central screw placement on PA and lateral views. (c) Sagittal CT view confirms healing 5 months postoperatively (d) CT 8 months after repair demonstrates de novo fracture. (e) 3D model rendered from CT data with Mimics software shows fracture fragment (red) arising about the screw entry site. (f) PA radiograph following scaphoid excision and four-corner arthrodesis.
Eight months later, the patient was wrestling and fell onto an outstretched hand. He returned with snuffbox tenderness and marked pain with wrist motion. CT demonstrated union at the original fracture site and a new, proximal and palmar nondisplaced fracture fragment measuring 8.14 mm × 13.75 mm and accounting for 14.0% of total scaphoid volume (Fig. 2d, 2e). Internal fixation with bone grafting of the fracture fragment was strongly recommended. However, given the risks associated with fixation of a small proximal pole fragment, the requisite prolonged immobilization, and the patient's desire to matriculate to culinary school within 2 months, he opted for scaphoid excision and four-corner arthrodesis (Fig. 2f). By 10 weeks he had completed rehabilitation and returned to school. At 6 months, he demonstrated an 80° flexion-extension arc (53% of the opposite side) and grip strength of 41 kg (86% opposite side).
Case 3
A 17-year-old left-handed football player sustained injury to his dominant wrist and did not seek treatment for 2.5 months until the season's end. Plain films at an outside hospital revealed a proximal pole fracture nonunion (Fig. 3a). He was treated at that hospital with antegrade fixation using an 18-mm Acutrak II Mini headless compression screw (Fig. 3b). The patient was then immobilized for 4 months. CT imaging at 6 months demonstrated > 50% bony healing of the scaphoid dorsally, but incomplete healing of the volar fracture line (Fig. 3c). The patient was pain free and was released to activities including weightlifting, lacrosse, and football.
Fig. 3.
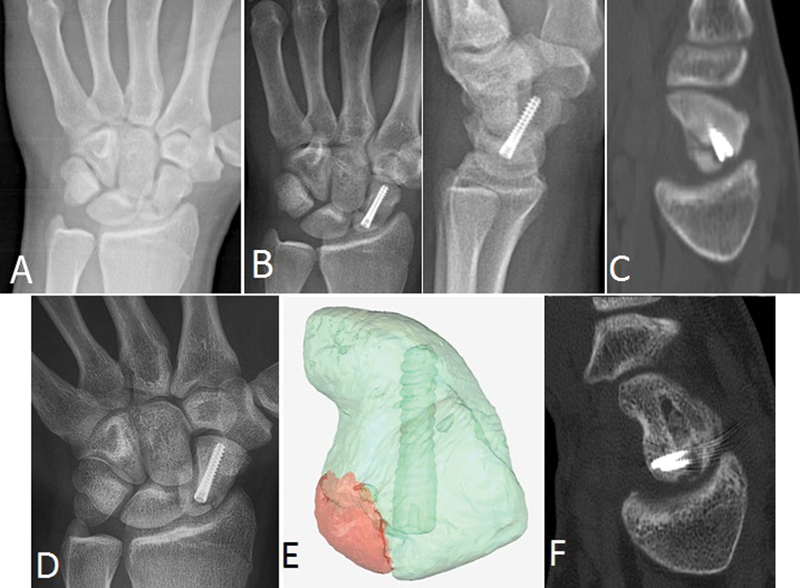
Case 3. (a) PA radiograph reveals proximal waist fracture nonunion. (b) Early postoperative PA and lateral views demonstrate good bony reduction and central screw placement. (c) Sagittal CT view showing consolidation of the fracture dorsally with incomplete healing volarly. (d) PA radiograph 18 months post repair demonstrates a lucency that resembles the original injury. (e) High-resolution CT imaging and Mimics processing reveals a fracture fragment (red) arising about the screw entry site. (f) Sagittal CT 14 weeks post secondary repair shows grafting of the original screw tract and confirms healing.
Twenty-two months after initial injury and 13 months after being released to normal activities, he presented to our center following the recent football season with new-onset wrist pain during activity of 1 month's duration. Plain films (Fig. 3d) and CT at our institution revealed a proximal pole volar marginal shear fracture fragment contiguous with the screw entry site. The fragment measured 7.54 mm × 10.56 mm (Fig. 3e) and represented 6.6% of the scaphoid volumetrically. MRI demonstrated a retained vascular supply to the minimally displaced fracture fragment. The fracture was treated with screw removal, curettage through the screw track, autogenous bone graft packing of the screw channel, and 1.5-mm mini-screw fixation of the fracture fragment (Medartis, Basel, Switzerland). The patient was immobilized for 12 weeks. Follow-up CT at 14 weeks demonstrated fracture consolidation (Fig. 3f). Clinically, the patient was pain free and had 50% active wrist ROM compared with the contralateral wrist when released to full activities. He returned to college and football without incident.
Discussion
Previous authors have posited that stress-raisers secondary to screw orientation may predispose the femoral neck to subsequent peri-implant fracture.11 12 However, we were unable to identify literature evaluating the in vivo biomechanical influence of headless screws on subsequent fracture of the healed scaphoid. Secondary fracture proximal to a Herbert compression screw4 and secondary fracture of the proximal third of another scaphoid after screw fixation with bone grafting13 have been reported. However, CT confirmation of initial fracture healing was not demonstrated in either report, and the shape and location of the secondary fracture fragment were not detailed. Importantly, these reports do not expound upon the potential role of intramedullary implants in secondary fracture.
Several studies examining the in situ biomechanics of scaphoid fixation screws under stress have been performed.14 15 16 17 One cadaveric study evaluating transversely osteotomized scaphoids fixed with one of several commercially available screws via a retrograde approach demonstrated implant-associated distal pole fractures after cyclic loading.14 However, the secondary fractures in our series occurred at the volar aspect of the proximal pole in all three patients and may well represent a different mechanical situation, given that healing had occurred prior to repeat traumatic load application.
In our series, we observed identical secondary proximal pole scaphoid fractures after antegrade compression screw fixation for scaphoid fracture nonunion. The secondary fracture fragments were remarkably consistent in shape and location, distinct from the original healed nonunion. All fragments were similar in size, measuring on average 8.2 mm × 12.84 mm (range 7.54–8.92 mm × 10.56–14.22 mm, Fig. 4) and comprising ∼12.6% (range 6.6–17%) of total scaphoid volume (mm3). Each fragment was also contiguous with the screw insertion site, suggesting a common mechanical etiology in which the headless compression screw is implicated.
Fig. 4.
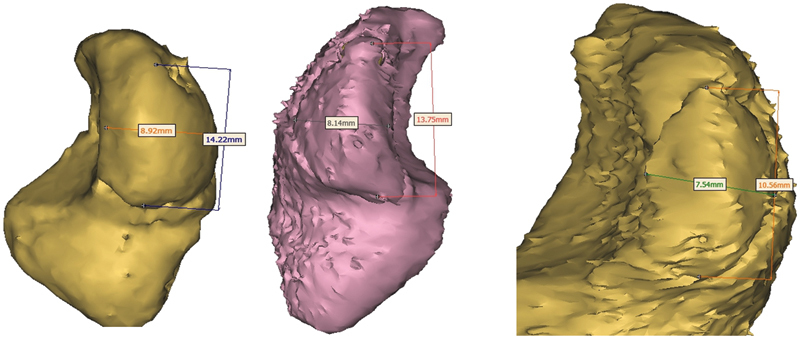
Side-by-side juxtaposition of 3D renderings illustrates the identical volar proximal fracture fragments and comparable fragment dimensions.
In case 3, CT confirmation of complete healing was not available prior to presentation at our facility. While it is possible that the volar marginal shear fracture fragment discussed in this case represents an incompletely healed nonunion, we argue it may more accurately be described as a de novo fracture contiguous with the previously inserted screw. The patient had a long symptom-free interval and had returned to vigorous athletic use, the plane of the fracture was different from the original fracture plane, and the new fracture shared remarkable similarity to the fracture fragments observed in the other two cases.
Our experience suggests the point of maximal weakness of the bone-screw construct is the persistent cortical defect at the screw insertion site. It is reasonable to speculate that an unhealed cortical defect in the scaphoid proximal pole could act as a stress-raiser for this unique fracture pattern. It is also possible that a disparity in Young's modulus between the titanium screw and surrounding bone may have concentrated stress at the volar aspect of the proximal pole during a fall on the hyperextended wrist.
As screw orientation may affect subsequent fracture pattern and load to failure in the femur,11 12 nuances of surgical technique for scaphoid nonunion screw fixation must be considered. In all three patients reported here, the compression screw was placed in the central one-third of the proximal pole. Central placement is associated with shorter time to union and lower probability of persistent nonunion compared with peripheral placement.18 The implications of central screw placement have been evaluated in biomechanical studies of osteotomized fresh cadaveric scaphoid waist fracture repairs.19 20 21 In one study, central placement was shown to confer greater stiffness and load at failure, compared with eccentric placement.21
Although the same screw type was utilized in all three cases, we do not attribute secondary fracture risk to hardware make or model. As refracture after fixation with other screw types4 has been detailed, we cannot make this association with any degree of certainty. Whether the osteoarticular defect left in the scaphoid proximal pole resulting from antegrade screw insertion is the proximate cause of secondary fracture can only be speculated, but given the contiguity of the fracture fragment and the insertion site we believe there is a compelling association. It is also plausible that the initial delay to fracture treatment induced changes in the vascularity and mechanical properties of the proximal pole and potentially predisposed our patients to secondary fracture.
While two previous reports have noted refracture after internal fixation in 2.5% (1/40)4 and 7% (1/14)13 of scaphoids, the exact incidence of secondary fracture is uncertain. However, the potential for this complication in young and active patients warrants discussion with potential patients and should be included in the informed consent. The association of this complication with a single screw type and with the antegrade approach warrants further investigation. We cannot say whether prophylactic screw removal is indicated in young, active persons after scaphoid nonunion repair, or whether a different fixation device may have had a lesser risk of secondary fracture. Risks of hardware removal must also be considered. Although the incidence of secondary fracture may be low, the small size of the fracture fragment and its proximal and volar intra-articular location make it a formidable challenge to access and fix directly. CT is helpful to identify the size and location of the fragment. Our preferred approach is to remove the screw, débride and graft the screw tract, and fix the fragment with mini screws or wires when possible.
Acknowledgments
We thank Parker H. Johnsen, BS, for his assistance with image collection and editorial support for this project.
Footnotes
Conflict of Interest None.
References
- 1.Bond C D, Shin A Y, McBride M T, Dao K D. Percutaneous screw fixation or cast immobilization for nondisplaced scaphoid fractures. J Bone Joint Surg Am. 2001;83-A(4):483–488. doi: 10.2106/00004623-200104000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Kawamura K, Chung K C. Treatment of scaphoid fractures and nonunions. J Hand Surg Am. 2008;33(6):988–997. doi: 10.1016/j.jhsa.2008.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arora R, Gschwentner M, Krappinger D, Lutz M, Blauth M, Gabl M. Fixation of nondisplaced scaphoid fractures: making treatment cost effective. Prospective controlled trial. Arch Orthop Trauma Surg. 2007;127(1):39–46. doi: 10.1007/s00402-006-0229-z. [DOI] [PubMed] [Google Scholar]
- 4.Vinnars B, Pietreanu M, Bodestedt A, Ekenstam Fa, Gerdin B. Nonoperative compared with operative treatment of acute scaphoid fractures. A randomized clinical trial. J Bone Joint Surg Am. 2008;90(6):1176–1185. doi: 10.2106/JBJS.G.00673. [DOI] [PubMed] [Google Scholar]
- 5.Davis E N Chung K C Kotsis S V Lau F H Vijan S A cost/utility analysis of open reduction and internal fixation versus cast immobilization for acute nondisplaced mid-waist scaphoid fractures Plast Reconstr Surg 200611741223–1235., discussion 1236–1238 [DOI] [PubMed] [Google Scholar]
- 6.Rettig M E, Kozin S H, Cooney W P. Open reduction and internal fixation of acute displaced scaphoid waist fractures. J Hand Surg Am. 2001;26(2):271–276. doi: 10.1053/jhsu.2001.21524. [DOI] [PubMed] [Google Scholar]
- 7.Slade J F III, Geissler W B, Gutow A P, Merrell G A. Percutaneous internal fixation of selected scaphoid nonunions with an arthroscopically assisted dorsal approach. J Bone Joint Surg Am. 2003;85-A 04:20–32. doi: 10.2106/00004623-200300004-00003. [DOI] [PubMed] [Google Scholar]
- 8.Yip H S, Wu W C, Chang R Y, So T Y. Percutaneous cannulated screw fixation of acute scaphoid waist fracture. J Hand Surg [Br] 2002;27(1):42–46. doi: 10.1054/jhsb.2001.0690. [DOI] [PubMed] [Google Scholar]
- 9.Sanders W E. Evaluation of the humpback scaphoid by computed tomography in the longitudinal axial plane of the scaphoid. J Hand Surg Am. 1988;13(2):182–187. doi: 10.1016/s0363-5023(88)80045-5. [DOI] [PubMed] [Google Scholar]
- 10.Mathoulin C, Haerle M. Vascularized bone graft from the palmar carpal artery for treatment of scaphoid nonunion. J Hand Surg [Br] 1998;23(3):318–323. doi: 10.1016/s0266-7681(98)80049-1. [DOI] [PubMed] [Google Scholar]
- 11.Oakey J W, Stover M D, Summers H D, Sartori M, Havey R M, Patwardhan A G. Does screw configuration affect subtrochanteric fracture after femoral neck fixation? Clin Orthop Relat Res. 2006;443(443):302–306. doi: 10.1097/01.blo.0000188557.65387.fc. [DOI] [PubMed] [Google Scholar]
- 12.Lichtblau S, Gallina J, Nasser P, Munyoki M, Jepsen K. A biomechanical comparison of two patterns of screw insertion. Bull NYU Hosp Jt Dis. 2008;66(4):269–271. [PubMed] [Google Scholar]
- 13.Riester J N, Baker B E, Mosher J F, Lowe D. A review of scaphoid fracture healing in competitive athletes. Am J Sports Med. 1985;13(3):159–161. doi: 10.1177/036354658501300303. [DOI] [PubMed] [Google Scholar]
- 14.Toby E B, Butler T E, McCormack T J, Jayaraman G. A comparison of fixation screws for the scaphoid during application of cyclical bending loads. J Bone Joint Surg Am. 1997;79(8):1190–1197. doi: 10.2106/00004623-199708000-00011. [DOI] [PubMed] [Google Scholar]
- 15.Carter F M II, Zimmerman M C, DiPaola D M, Mackessy R P, Parsons J R. Biomechanical comparison of fixation devices in experimental scaphoid osteotomies. J Hand Surg Am. 1991;16(5):907–912. doi: 10.1016/s0363-5023(10)80159-5. [DOI] [PubMed] [Google Scholar]
- 16.Kaulesar Sukul D M, Johannes E J, Marti R K, Klopper P J. Biomechanical measurements on scaphoid bone screws in an experimental model. J Biomech. 1990;23(11):1115–1121. doi: 10.1016/0021-9290(90)90004-m. [DOI] [PubMed] [Google Scholar]
- 17.Takase K, Yamamoto K. Mechanical strength and optimal site of placement of a threaded bone screw assessed on the basis of the screw breakage for non-union of the scaphoid: a biomechanical study. Hand Surg. 2005;10(2–3):225–230. doi: 10.1142/S0218810405002863. [DOI] [PubMed] [Google Scholar]
- 18.Trumble T E, Clarke T, Kreder H J. Non-union of the scaphoid. Treatment with cannulated screws compared with treatment with Herbert screws. J Bone Joint Surg Am. 1996;78(12):1829–1837. doi: 10.2106/00004623-199612000-00005. [DOI] [PubMed] [Google Scholar]
- 19.Guo Y, Tian G L, Jiang B G, Chen S L, Han N. Central placement of screw fixation for scaphoid fracture: a biomechanical study [in Chinese] Beijing Da Xue Xue Bao. 2013;45(5):684–687. [PubMed] [Google Scholar]
- 20.Dodds S D, Panjabi M M, Slade J F III. Screw fixation of scaphoid fractures: a biomechanical assessment of screw length and screw augmentation. J Hand Surg Am. 2006;31(3):405–413. doi: 10.1016/j.jhsa.2005.09.014. [DOI] [PubMed] [Google Scholar]
- 21.McCallister W V, Knight J, Kaliappan R, Trumble T E. Central placement of the screw in simulated fractures of the scaphoid waist: a biomechanical study. J Bone Joint Surg Am. 2003;85-A(1):72–77. doi: 10.2106/00004623-200301000-00012. [DOI] [PubMed] [Google Scholar]


