Abstract
Introduction
Laparoscopic pyeloplasty is considered a standard treatment for ureteropelvic junction obstruction (UPJO). However, the presence of another pathology makes it a more challenging operation and guides the surgeon towards open conversion. In this study, we present our experience in difficult pyeloplasty cases managed by laparoscopy.
Material and methods
Six patients (4 females and 2 males) with an average age of 44 and a range of 27 to 60 years old, were diagnosed for UPJO. Three were on the left side and 3 on the right side. In addition to UPJO, 2 patients had renal stones, one patient had both renal ptosis and an umbilical hernia, 3 patients had a para-pelvic cyst, hepatomegaly and malrotated kidney, respectively. All patients had a preoperative ultrasound, CT or IVU, and a renal isotope scan. Laparoscopic pyeloplasty was performed according to the dismembered Anderson-Hynes technique with auxiliary maneuver, according to the pathology.
Results
All patients were treated successfully for UPJO and the concomitant pathologies, except hepatomegaly and malrotation. Mean operative time was 125 minutes and estimated blood loss was <50 ml.
Conclusions
Laparoscopic pyeloplasty can be performed in difficult situations provided that the surgeon has enough experience with laparoscopy.
Keywords: difficult pyeloplasty, laparoscopic pyeloplasty, ureteropelvic junction obstruction
INTRODUCTION
UPJO, although usually a congenital disease, can present clinically at any age, with an incidence rate of 1:1000 at time of birth [1]. Primary UPJO can be associated with other renal anomalies, such as horseshoe kidney and ectopic kidney, in which UPJO is present in 30% and 40%, respectively [2]. Concomitant nephrolithiasis can be present in about 20% of UPJO patients [3, 4].
Laparoscopic pyeloplasty as a minimally invasive procedure is now considered the standard technique for the treatment of UPJO, with equal success results as open surgery [5–8], However, the presence of another pathology represents further surgical challenge for laparoscopic surgeons to perform laparoscopic pyeloplasty, as the ability to perform this operation and the related complications are affected significantly by the complexity of the surgical procedure and the surgeon's experience [9].
In this case series, we present 6 patients who were managed for UPJO and at the same time had concomitant pathology, such as renal stones, hepatomegaly due to multiple large hepatic cysts, para-pelvic renal cyst, umbilical hernia, renal ptosis, and renal malrotation. In all these cases, UPJO was managed successfully with laparoscopic pyeloplasty, with auxiliary surgical intervention according to the concomitant pathology.
MATERIAL AND METHODS
By retrospective analysis of all laparoscopic pyeloplasty cases in our institute and after exclusion of all cases with only UPJO with no other pathology, six patients who underwent laparoscopic pyeloplasty between September 2010 and June 2012 were included in this study. This cohort included 4 females and 2 males with an average age of 44 years old and a range of 27 to 60 years. Body mass index (BMI) ranged between 18.7 and 22.4 Kg/m2. Three patients were left sided (50%) and 3 were right sided (50%). In addition to UPJO, 2 patients had renal stones, one patient had both renal ptosis and an umbilical hernia, 3 patients had a para-pelvic cyst (5x4 cm), hepatomegaly due to multiple hepatic cysts (largest was 20 cm), and malrotated kidney, respectively.
Preoperative evaluation: Material
All patients presented with mild to moderate flank pain and were investigated with ultrasound, CT or IVU, and renal isotope scan that revealed salvageable split kidney function of the affected renal unit in all patients.
Operative technique
After obtaining informed written consent, including the possibility for open conversion, laparoscopic pyeloplasty was performed. Pneumoperitoneum was created by mini laparotomy technique through a small incision in the periumbilical ring. Then, a 10 mm port for the laparoscopic 30° lens was introduced. Carbon dioxide was insufflated up to 15 mm Hg pressure. The other 2 ports (5 and 12 mm) were fixed in the midclavicular line under direct vision. Then, the colon was reflected and the ureter was identified. Dissection was continued until the easily identified dilated renal pelvis was seen. Four patients (66%) had a crossing vessel towards the lower pole of the kidney that was successfully preserved in all cases. After dissection of the peripelvic tissue, the renal pelvis was fixed by a staying suture to the lateral abdominal wall. The pyeloplasty was performed with dismembered Anderson- Hynes technique and the ureter was spatulated towards the medial border of the kidney to avoid ureteral rotation during suturing. Anastomosis was performed by 4/0 vicryl starting by suturing the apex of the ureteral spatulation to the most dependent part of the pylotomy after transpositioning of the ureter above the crossing vessel. A double J stent was fixed in the antegrade way through the upper lateral port before completing the anastomosis by running watertight suturing. A drain was fixed at the end and the port sites were closed in layers.
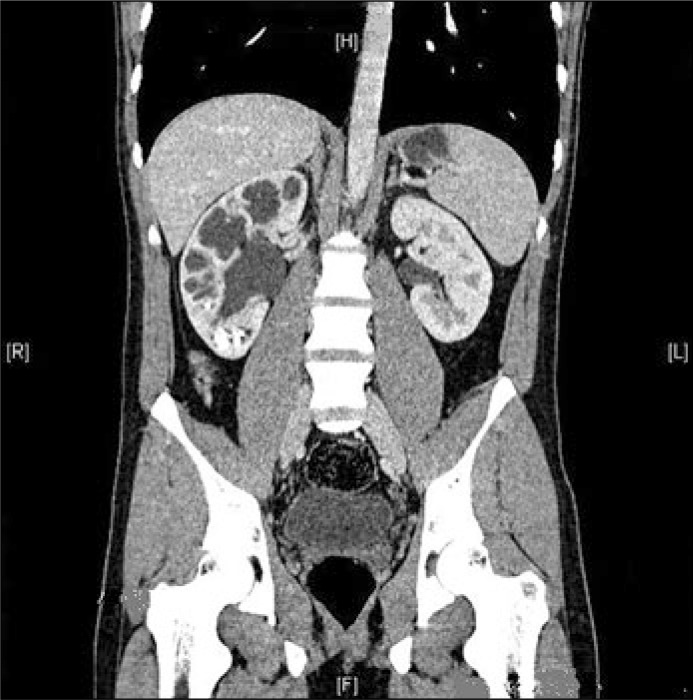
In the 2 cases with renal stones, the first case had multiple lower calyceal stones, thin parenchyma due to marked hydronephrosis as a sequele for UPJO, and a narrow calyceal neck. Laparoscopic nephrolithotomy was performed before pyeloplasty. The perinephric fat was dissected to expose the parenchyma. A small lower pole nephrotomy was performed by mono-polar hook and the stones were retrieved by laparoscopic grasper. The lower calyx was irrigated by suction to wash out any blood clots or small gravels. The nephrotomy was closed by continuous 0/0 vicryl suturing and the suture was controlled by abs luck (Figure 1).
Figure 1.
Right sided ureteropelvic obstreuction with marked hydronephrosis and multiple lower calyceal stones.
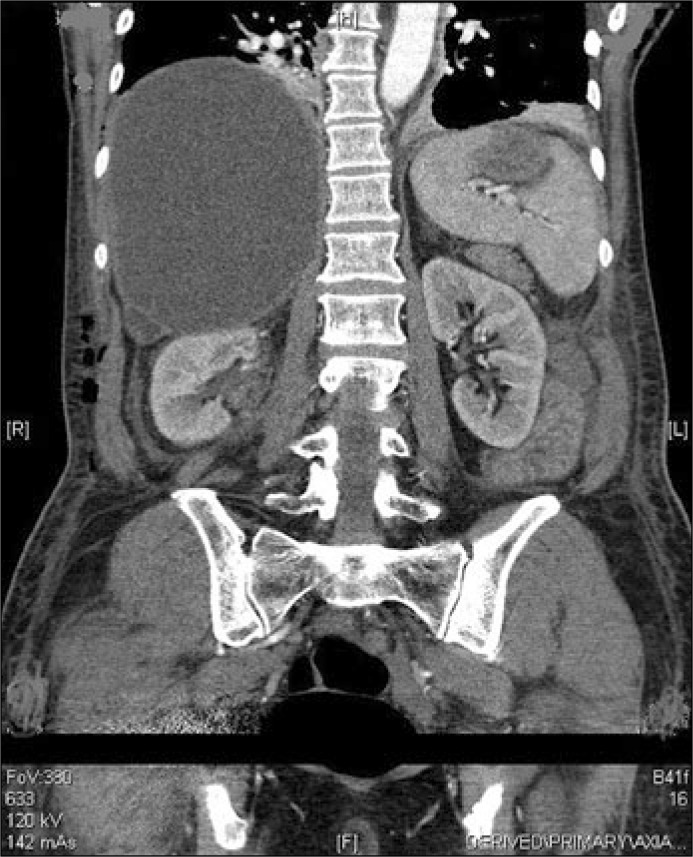
The second case had a single lower calyceal stone with slightly normal parenchyma and a wide calyceal neck. After division of the renal pelvis during laparoscopic pyeloplasty, flexible URS was advanced through the 12 mm port into the renal pelvis and the lower calyx and the stone was retrieved (Figure 2).
Figure 2.
Left sided ureteropelvic obstreuction with single lower calyceal stone.
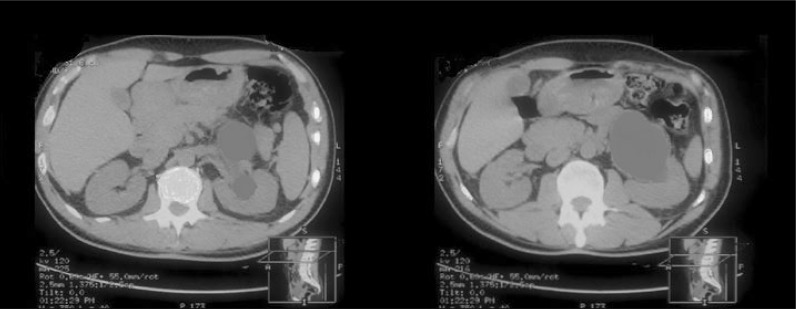
In the third case with a huge hepatic cyst, the challenge in performing laparoscopic pyeloplasty was the anatomical changes, as the kidney was in a lower position than normal due to the effect of the space occupying cyst; therefore, the working space was very limited. During minilaprotomy at the start of the operation, some resistance beneath the peritoneum was felt by the finger due to the liver, which was retracted up and laterally by the finger before opening the peritoneum and fixation of the camera port. This maneuver resulted in a small hepatic laceration. The other two ports were fixed in a triangular manner but in lower than usual sites. The hepatic laceration could be easily controlled by compression with a sponge, then application of synthetic haemostatic material (Figure 3).
Figure 3.
Right sided ureteropelvic obstreuction with huge hepatic cyst compressing the right kidney.
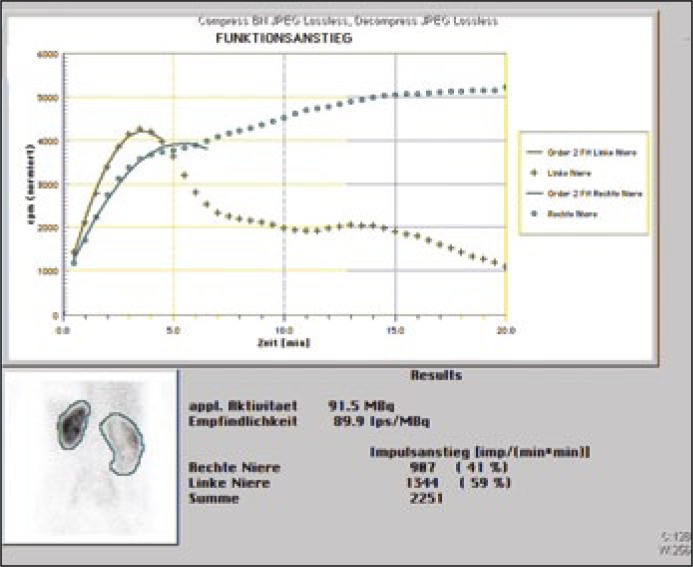
The fourth patient had ipsilateral renal ptosis and an umblical hernia that was first reduced and then an incision was carefully created over the hernial site, and the port was fixed under direct vision to avoid bowel injury. The kidney was grasped higher than its normal anatomical position and fixed from Gerota's fascia to the lateral abdominal wall by a stay suture from outside, then pyeloplasty was performed in this position. After pyeloplasty, nephropexy was performed by suturing the renal capsule to the posterolateral abdominal wall by two 0/0 absorbable interrupted sutures. After removal of the trocars, the umbilical incision was extended laterally by 1 cm on each side. The peritoneum was released all around the hernial defect and closed with 3/0 absorbable sutures. The hernial defect was closed in double layer by the fascia over fascia technique (Figure 4).
Figure 4.
Renal isotope scan showing obstructed pattern of the right kidney with low position due to renal ptosis.
The fifth patient had a para-pelvic cyst (5x4 cm) that was masked the renal pelvis. The cyst was dissected first from the renal pelvis and de-roofed with mono-polar hook, then pyeloplasty was performed (Figure 5).
Figure 5.
Left sided ureteropelvic obstruction with para-pelvic cyst.
In the sixth case with malrotation, difficulty of pyeloplasty was overcom by complete mobilization of the kidney. It was then re-rotated and fixed through the pelvis by a staying suture in a position suitable for intra-corporeal suturing. The ureter was spatulated towards the lower pole after partial cutting of the renal pelvis and before complete division to avoid disorientation and subsequent ureteral rotation.
RESULTS
All patients were treated successfully for UPJO and the concomitant pathologies, except hepatomegaly and malrotation. Estimated blood loss was less than 50 ml. Mean operative time was 125 minutes. There were no intra or postoperative complications except the hepatic laceration in the third patient, which was easily managed.
All patients were ready for discharge in the second post operative day. The double J was removed after six weeks. The 2 patients with renal stones both had a postoperative stone free abdominal computed tomography. Renal function assessment by renal isotope scan MAG3 at 3, 12 months post operative revealed stabilized function as pre operative values with no more deterioration or obstruction.
DISCUSSION
Laparoscopic pyeloplasty was first intoduced by Schuessler in 1993 [5]. Many publications confirmed that laparoscopic pyeloplasty has equal success rates in comparison to the open technique with less morbidity for the patient [5–8]. In our experience, we usually fix the first port for the camera in the periumbilical ring for better cosmotic results, provided that the patient's BMI is within normal, as in the patients included in this study. In obese patients, we use the lateral rectus border for better accessibility.
UPJO can be associated with other pathologies, either congenital such as malrotation or parapelvic cysts or acquired pathologies such as renal stones, hepatomegaly, and renal ptosis. These pathologies can be just concomitant and not directly related to the UPJO, or may be as a result of obstruction and inadequate urinary drainage, such as in renal stones. Presence of concomitant pathology with UPJO makes laparoscopic pyeloplasty more complex and challenging for surgeons, especially those who are starting laparoscopic pyeloplasty, because the associated pathology either needs auxiliary surgical intervention to be corrected, or at least makes laparoscopic pyeloplasty more difficult due to anatomical changes or limited working space. Although robotic assisted laparoscopic pyeloplasty can be a good alternative to conventional laparoscopy in complex situations, the very high financial cost is still the main limiting factor.
Although the volume of this study is small, it represents a wide variety of pathologies that may be associated with UPJO. All available literature reports on the management of UPJO with associated stones. Yin Z. and colleagues reported on successful management of UPJO with stones in sixteen patients using laparoscopic pyeloplasty and flexible URS [10]. Juan G R and colleagues reported on successful management of renal stones during laparoscopic pyeloplasty using flexible URS in eight patients and laparoscopic grasper in four patients [11].
Associated renal stones can be treated by different methods; for example, laparoscopic pyelolithotomy, laparoscopic nephrolithotomy, fexible URS, or PCNL. This depends on the stone number, location, degree of hydronephrosis, and parenchymal thickness [12]. We used laparoscopic nephrolithotomy in the first case, as the stone burden was located in the lower calyx and the parenchyma was thin. In the second case, flexible URS was considered less invasive, as the parenchyma was quiet thick and the calceal neck was wide [13, 14]. Percutaneus approach by performing PCNL and endopylotomy incision can be an alternative for laparoscopy in UPJO with renal stones, but the lower success rate of endopylotomy in comparison to laparoscopic pyeloplasty in primary UPJO makes this approach questionable [15].
Para-pelvic cyst was excised to avoid mechanical compression over the pelvis that may affect urine flow from the kidney, with subsequent persistence of the symptoms. Renal ptosis was corrected by nephropexy to exclude this factor as a cause for postoperative flank pain
Hepatomegaly and malrotation were considered uncorrectable pathologies, but they represented difficult situations due to a small working space and difficult access for intracorporial suturing.
CONCLUSIONS
Laparoscopic pyeloplasty can be performed in complex situations due to associated pathologies, provided that the surgeon has enough experience. However, bigger series are needed to assess the feasibility of laparoscopic pyeloplasty in these complex cases.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
References
- 1.Cohen B, Goldman SM, Kopilnick M, Khurana AV, Salik JO. Ureteropelvic junction obstruction: its occurrence in 3 members of a single family. J Urol. 1978;120:361–364. doi: 10.1016/s0022-5347(17)57175-x. [DOI] [PubMed] [Google Scholar]
- 2.Shapiro E, Bauer SB, Chow JS. Anomalies of the Upper Urinary Tract. In: Walsh PC, Retik AB, Vaughan ED Jr, Wein AJ, editors. Campbell‘s Urology. 10th edn. Philadelphia: Saunders; 2012. pp. 3123–3160. [Google Scholar]
- 3.Juan GR, Sergio AG, Maria A, et al. Transperitoneal laparoscopic pyeloplasty in the treatment of ureteropelvic junction obstruction. Cent European J Urol. 2013;66:361–367. doi: 10.5173/ceju.2013.03.art31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tadahiro I, Hideto I, Seiya I, et al. Hydronephrosis after retroperitoneal laparoscopic dismembered Anderson–Hynes pyeloplasty in adult patients with ureteropelvic junction obstruction: A longitudinal analysis. Cent European J Urol. 2014;67:101–106. doi: 10.5173/ceju.2014.01.art24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen RN, Moore RG, Kavoussi LR. Laparoscopic pyeloplasty. Indications, technique, and long-term outcome. Urol Clin North Am. 1998;25:323–330. doi: 10.1016/s0094-0143(05)70021-5. [DOI] [PubMed] [Google Scholar]
- 6.Schuessler WW, Grune MT, Tecuanhuey LV, Preminger GM. Laparoscopic dismembered pyeloplasty. J Urol. 1993;150:1795–1804. doi: 10.1016/s0022-5347(17)35898-6. [DOI] [PubMed] [Google Scholar]
- 7.Janetschek G, Peschel R, Altarac S, Bartsch G. Laparoscopic and retroperitoneoscopic repair of ureteropelvic junction obstruction. Urology. 1996;47:311–317. doi: 10.1016/S0090-4295(99)80444-0. [DOI] [PubMed] [Google Scholar]
- 8.Recker F, Subotic B, Goepel M, Tscholl R. Laparoscopic dismembered pyeloplasty: preliminary report. J Urol. 1995;153:1601–1605. doi: 10.1016/s0022-5347(01)67472-x. [DOI] [PubMed] [Google Scholar]
- 9.Rene J, David C. Difficulties in Urologic Laparoscopy Complications. In: Ahmed M, Inderbir S, editors. Difficult Conditions in Laparoscopic Urologic Surgery. Heidelberg: springer; 2011. pp. 405–431. [Google Scholar]
- 10.Yin Z, Wei YB, Liang BL, et al. Initial experiences with laparoscopy and flexible ureteroscopy combination pyeloplasty in management of ectopic pelvic kidney with stone and ureter-pelvic junction obstruction. Urolithiasis. 2015;43:255–260. doi: 10.1007/s00240-015-0753-9. [DOI] [PubMed] [Google Scholar]
- 11.Juan GR, Sergio AG, Leslie CS, et al. Approach to kidney stones associated with ureteropelvic junction obstruction during laparoscopic pyeloplasty. Cent European J Urol. 2014;66:440–444. doi: 10.5173/ceju.2013.04.art13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hruza M, Schulze M, Teber D, Gözen AS, Rassweiler JJ. Laparoscopic techniques for removal of renal and ureteral calculi. J Endourol. 2009;23:1713–1718. doi: 10.1089/end.2009.1539. [DOI] [PubMed] [Google Scholar]
- 13.Rahul A. Desai, Dean G. Assimos. Role of Laparoscopic Stone Surgery. Urology. 2008;71:578–580. doi: 10.1016/j.urology.2007.10.052. [DOI] [PubMed] [Google Scholar]
- 14.Whelan JP, Wiesenthal JD. Laparoscopic pyeloplasty with simultaneous pyelolithotomy using a flexible ureteroscope. Can J Urol. 2004;11:2207–2209. [PubMed] [Google Scholar]
- 15.Szydełko T, Kopeć R, Kasprzak J, et al. Antegrade endopyelotomy versus laparoscopic pyeloplasty for primary ureteropelvic junction obstruction. J Laparoendosc Adv Surg Tech A. 2009;19:45–51. doi: 10.1089/lap.2008.0104. [DOI] [PubMed] [Google Scholar]