Abstract
Introduction
There are a myriad of treatment options available for patients suffering with the increasingly prevalent condition of stress urinary incontinence (SUI). The minimally invasive nature of periurethral bulking agents makes them an attractive proposition in the correctly selected patient. There is, however, limited data available on the medium to long term safety and efficacy of this procedure. The aim of our study is to evaluate the outcomes of Polyacrylamide Hydrogel (PAHG) (Bulkamid®) as a periurethral bulking agent at our institution.
Material and methods
From 2006 to 2011, two hundred and fifty six women underwent periurethral bulking with PAHG in the management of SUI or mixed urinary incontinence (MUI). Women were assessed with at least yearly quality of life and ICIQ questionnaires.
Results
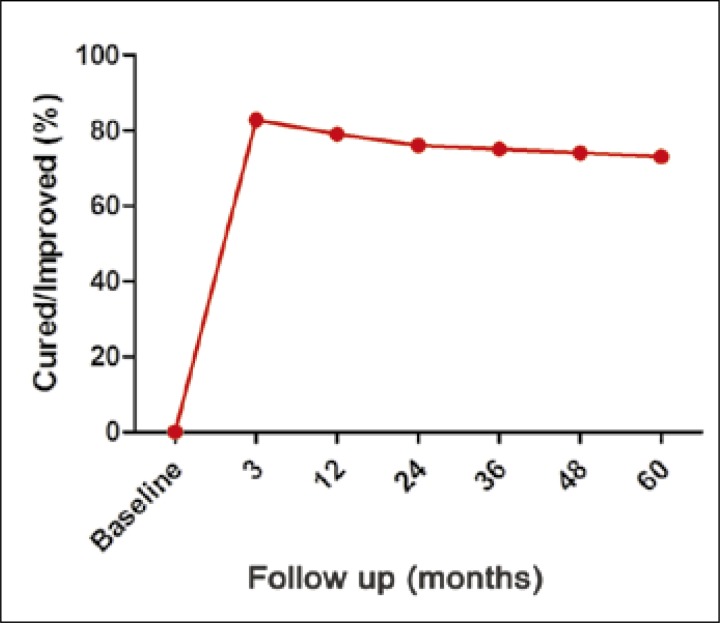
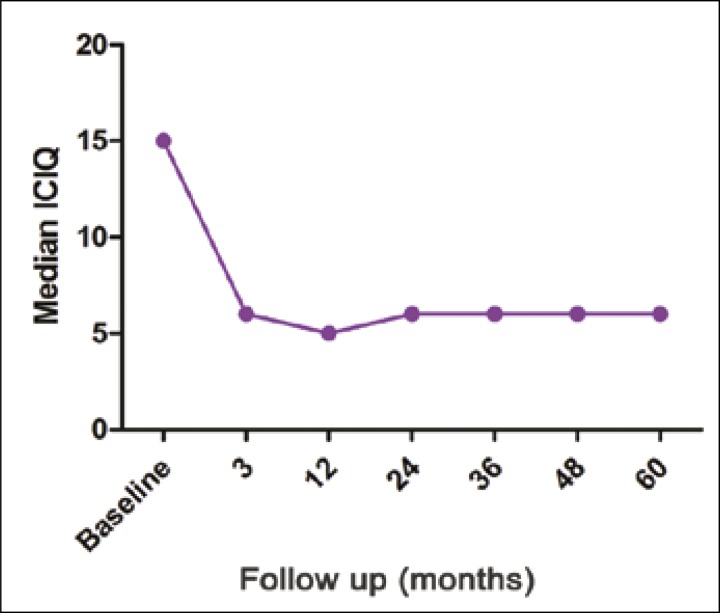
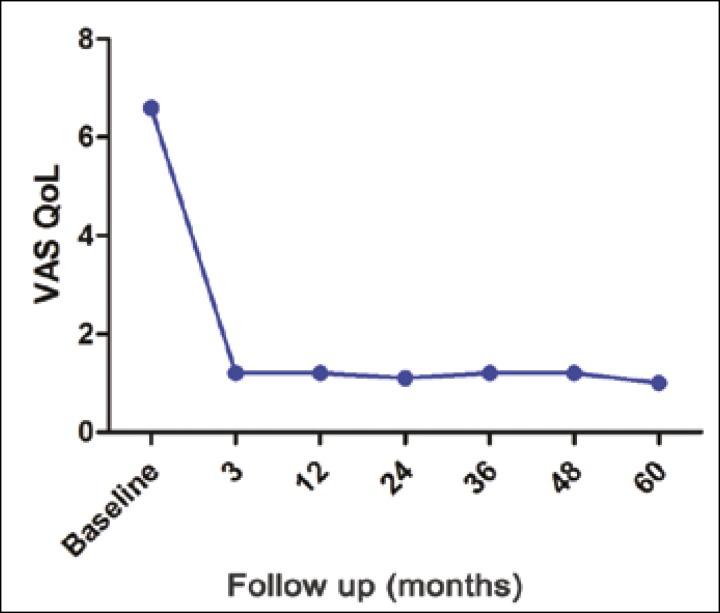
The majority of patients had the procedure under a local anaesthetic, with a median operative time of 9 minutes. Median follow up was 38 months. 82% of patients reported cure/significant improvement at 3 months. Importantly, this high satisfaction rate was maintained at final follow up and was reflected in both VAS and ICIQ scores. There were no reported adverse reactions and no significant safety concerns.
Conclusions
We conclude that Bulkamid® injection is an efficacious, minimally invasive, and safe procedure for a selected group of patients with stress incontinence. In our study, PAHG has been shown to be durable and safe.
Keywords: stress urinary incontinence, Bulkamid®, trans-urethral injection, polyacrylamide hydrogel
INTRODUCTION
Stress urinary incontinence (SUI) is a morbid condition, which is increasing in prevalence [1]. An increasingly diverse cohort of patients now seek management for their SUI. The minimally invasive nature of intra urethral bulking agents makes them an attractive proposition for the management of female stress urinary incontinence.
As early as 1904, Meyer described periurethral injections of paraffin for the compression of the urethra to cure urinary incontinence [2]. However, the technique has been plagued by the inability to provide an efficacious, durable, and safe bulking agent. Injectable materials including Teflon® polytetrafluoroethylene, autologous fat injections, and hyaluronic acid/dextranomer copolymer (Zuidex) have been associated with problems, including particle migration and safety concerns, which have led to their withdrawal [3].
Polyacrylamide hydrogel (PAHG) Bulkamid® is a sterile gel consisting of 2.5% cross-linked Polyacrylamide and 97.5% non pyrogenic water [4]. PAHG has been used extensively in plastic surgery and has been shown to be biocompatible, non- toxic, and non- resorbable [5, 6, 7]. PAHG was subsequently introduced as a promising periurethral bulking agent by Lose et al. in 2006 [8]. In subsequent multi-institution trials, PAHG has shown responder rates of 64% at two year follow up and good tolerability [9]. However, doubts remain about the durability and cost effectiveness of periurethral bulking agents. Studies have shown that the success rates of periurethral bulking agents are disappointing, with increasing failure rates after 24 months [10].
The aim of our study is to describe our institution's use of periurethral PAHG bulking in the management of female stress and mixed urinary incontinence.
MATERIAL AND METHODS
From June 2006 to October 2011, the majority of our patients with SUI or MUI were offered periurethral bulking PAHG by a single surgeon (WA). The median BMI was 27.6 kg/m2 (19.5–47) and the median number of pregnancies was 2 (0–4). All patients included in this study had urodynamically proven urinary stress incontinence with a median maximum cystometric capacity of 322 ml (245–502) and median valsalva leaking pressure of 59 cmH20 (38–100) with no evidence of outflow obstruction (Qmax <15 ml/sec, Pvesmax >50 cmH2O). Patients with concomitant urinary tract infection, previous surgery for stress incontinence, functional bladder capacity <200 mls, and pelvic organ prolapse ≥ stage 2 were not included in the study. Only patients with a duration of symptoms of more than one year, failed conservative treatment, and incontinence episodes >1 per 24 hours were included in the study.
At the initial screening visit, all women were clinically evaluated with a complete history, physical evaluation, daily pad count, and urine dipstick. Urodynamic investigation was completed as a standard, with the inclusion of post void residual measurement, urethral pressure profile, pressure flow profile, and leak point pressure. At baseline, patient subjective satisfaction was assessed using patient-completed International Consultation on Incontinence Questionnaires (ICIQ) [11] for evaluation of lower urinary tract symptoms and their impact on the quality of life with a ten point visual analgoue scale (VAS QoL) [12].
Procedure
All patients were given prophylactic gentamicin. The patient was positioned on the operating table with slight hip flexion. Lubricant containing local anaesthetic was placed inside the urethra and was followed by slow trans-urethral instillation of 2% lignocaine solution. The PAHG injection was performed under endoscopic control using a single use PAHG Bulkamid® cystoscope connected to 0 degree optic to make the sub–mucosal injection of PAHG precise and accurate. The rotating sheath over the cystoscope allows the working channel to rotate 360 degrees to provide optimal access and visual control of the injection sites without moving the whole cystoscope. Points of technique include slow advancement of the needle to avoid accidental urethral mucosa injury and an angulation of less than five degrees to avoid deep injection. The ideal sub-mucosal injection sites are 3, 6, and 9 o'clock and within 1 cm distal to the bladder neck (proximal urethra). To achieve good coaptation of the urethral wall, 1–2 mls of Bulkamid® are injected at 3 sites with no more than 0.5 ml at each site (Figure 1).
Figure 1.
Coaptation of the urethral walls post PAHG transurethral bulking.
All patients were discharged home the same day after spontaneous voiding with residual volume less than 100 mls, except one who went into acute urinary retention (0.45%). Patients were assessed at 3 months post operatively, including urine analysis and objective assessment with bladder scan for residual volume. The patients were subsequently followed up at 12 months and then on an annual basis with ICIQ and VAS QoL.
The primary end point of the study was whether patients were completely dry (cured) or leaked once a week or less (significant improvement) as assessed by question 2 of the ICIQ questionnaire. Secondary endpoints included quality of life assessment and safety profile.
Statistics
We used Graphpad Prism version 5.0 to analyse the data. We used the Wilcoxon sign rank test to assess the difference in scores before and after PAHG injection. Those variables which were assessed on more than two occasions were assessed using the Friedman ANOVA test.
RESULTS
Two hundred and fifty six consecutive patients with stress urinary incontinence with a median age of 59.8 years (31 to 93) underwent transurethral PAHG injection. Clinically, stress incontinence was pure in 148 patients (67.8%), while the remainder had mixed incontinence with predominant stress incontinence. 225 patients had the procedure performed under local anaesthesia. The remaining 21 patients opted for the procedure under a short general anaesthesia. The median operative time was 9 minutes (Inter quartile range (IQR) 5 to 14).
Two hundred and twelve patients (82.8%) had a subjective improvement (subjectively cured or significant improvement) at 3 month follow up. 110 of the patients were cured (42.9%). The percentage of patients cured/improved at 3 months was maintained throughout follow up with a non statistically significant reduction between 3 months and five years (Figure 2). Median follow up was 38 months (IQR 22 to 57 months) (Table 1).
Figure 2.
Subjective success rates according to time.
Table 1.
Number of patients who reached each stage of follow up
| Baseline | 3 months |
12 months |
24 months |
36 months |
48 months |
60 months |
|
|---|---|---|---|---|---|---|---|
| Mean | 256 | 256 | 218 | 179 | 138 | 99 | 60 |
The median ICIQ score showed a significant improvement at three months (p <0.0001). This was maintained at 12 months and on subsequent yearly follow up to five years (Figure 3). Similarly, the overall QoL VAS score decreased significantly from a baseline median of 6.6 to 1.2 after 3 months and 1 at 12 months follow-up (Figure 4).
Figure 3.
Median ICIQ score according to time.
Figure 4.
Median VAS QoL according to time.
The median number of incontinence episodes in a 24 hour period decreased from baseline (p <0.0001) and was maintained throughout follow up (Table 2). There was no significant change in median post operative residual volume, with a baseline volume of 44 mls (IQR 10 to 80) and a value of 24 mls (IQR 10 to 55) at 3 months. The mean urine leakage on a 24 hour pad test was reduced after treatment, ranging from 56.5 grams (IQR 32 to 138) at baseline to 4.5 g (IQR 2.3 to 5.2) at 3 months (p <0.0001). Longer term data on urinary leakage and post void residual was not collected.
Table 2.
Incontinence episodes per 24 hour period
| Baseline | 3 months |
12 months |
24 months |
36 months |
48 months |
60 months |
|
|---|---|---|---|---|---|---|---|
| Mean | 3.8 | 0.6 | 0.8 | 0.6 | 0.6 | 0.6 | 0.7 |
| Standard deviation | 2.5 | 1.6 | 1.7 | 1.5 | 1.4 | 1.4 | 1.4 |
Two patients recorded worsening of their urinary symptoms with development of de novo overactivity symptoms. Four patients were seen by their general practitioner three days after Bulkamid® injection with symptoms suggestive of acute cystitis and were treated with oral antibiotics. One patient (0.45%) was unable to void post injection and subsequently failed 2 trials without catheters. Part of the PAHG was squeezed out and she managed to void successfully and remained dry. Eighteen patients who had continued stress urinary incontinence had a second PAHG injection (Bulkamid® booster) which cured their urinary incontinence.
In those patients with no improvement in symptoms who had good coaptation at the time of initial Bulkamid® injection, it was felt that they would not be helped by a further booster. These patients were offered further surgery pending anaesthetic fitness and patient preference.
Safety
None of the patients developed infection, abscess, or allergic reaction at the site of the injection. No other adverse events were described. As described previously, one patient developed urinary retention and this was resolved.
DISCUSSION
There have been concerns over the durability and medium/long term safety of bulking agents. Previous studies have shown responder rates of 67% and 88%, respectively, to periurethral bulking agents at follow up of 24 months [9, 13]. Uniquely, we provide evidence of the efficacy of PAHG periurethral bulking at a median follow up of 38 months and in a limited cohort of patients at 60 months. This durability is supported by all parameters, including VAS Qol scores and ICIQ.
This study shows excellent, durable results for a minimally invasive procedure. We feel that the durable nature of PAHG as a periurethral bulking agent is supported by the outcomes from other specialities. PAHG has been used in breast surgery, and has shown that it does not migrate and is non-degradable even after ten years of follow up [5]. It has similar, long term results as a soft tissue filler in plastic surgery [6, 14]. These long term results from other specialities illustrate its inert nature, which can be utilised as a periurethral bulking agent. There are various management options available for patients with stress urinary incontinence. There are however, patients in whom a bulking agent may be preferable, including patients unfit for a general anaesthetic, women of childbearing age, and patients with gross obesity (Table 3) [15, 16, 17]. In addition to these primary indications, PAHG periurethral bulking can be offered to women with persistent or recurrent stress incontinence who have failed previous incontinence surgery [18].
Table 3.
Indications for PAHG periurethral bulking
| Internal Sphincter Deficiency |
| Women who prefer minimally invasive surgery |
| Women of childbearing age |
| Patient not suitable for more invasive surgery: elderly, severe vaginal stenosis, high risk for regional or general anaesthesia. |
| Gross Obesity |
| Detrusor hypo-activity (Low flow, low voiding pressure <15 cmH20) |
This study shows excellent, durable results for a minimally invasive procedure. We feel that the durable nature of PAHG as a periurethral bulking agent is supported by the outcomes from other specialities. PAHG has been used in breast surgery, and has shown that it does not migrate and is non-degradable even after ten years of follow up [5]. It has similar, long term results as a soft tissue filler in plastic surgery [6, 14]. These long term results from other specialities illustrate its inert nature, which can be utilised as a periurethral bulking agent. There are various management options available for patients with stress urinary incontinence. There are however, patients in whom a bulking agent may be preferable, including patients unfit for a general anaesthetic, women of childbearing age, and patients with gross obesity (Table 3) [15–17]. In addition to these primary indications, PAHG periurethral bulking can be offered to women with persistent or recurrent stress incontinence who have failed previous incontinence surgery [18].
The other important message from our study is the lack of any reported adverse reactions, indicating the inert nature of PAHG. This good safety profile has been replicated in other studies describing the use of PAHG as a periurethral bulking agent and in its use in other specialities [7, 19–22]. The durability of PAHG is further backed up by the work of Mouritsen et al. who found that PAHG deposits were still visible on vaginal ultrasound in eleven patients eight year post injection [23].
In this study, 42.9% of patients were cured (complete resolution of their symptoms in absence of any post-operative complications). This compares to the 2007 findings of Albo et al. in a large study on colposuspension and pubovaginal sling with an overall success rate of 47% [24]. In their 2002 prospective multicentre randomised trial of tension free vaginal tape and colposuspension, Ward et al. showed a 66% complete cure rate in the vaginal tape arm [25]. More recent studies have however shown higher success rates for sub urethral slings [26]. We note that bulking agents are more expensive than tapes, although they are quicker to inject and can be an in-office procedure. As suggested by Ghoniem et al. [13], we would like to recommend a randomised study of periurethral bulking agent and tension free vaginal tape to include cost benefit analysis.
We acknowledge that we only had five year follow up on a minority of patients. There is no evidence that the patients who were lost to follow up were suffering from lack of efficacy or durability of the treatment. We do acknowledge that this is a source of potential bias and a limitation of our study. Our study did not have a control group and lacked randomisation. In addition, we did not have longer term data on 24 hour pad test. However, we feel that quality of life and subjective measures were more important parameters.
CONCLUSIONS
Bulkamid® is a promising bulking agent for women with stress urinary incontinence. It is safe, durable, and easily adminstered under local anaesthesia with an initial success rate of over 80%. Bulkamid® injection can be used as a primary procedure in a carefully selected group of patients.
CONFLICTS OF INTEREST
The authors reported no conflict of interest. The authors alone are responsible for the content and writing of the paper. This study is funded solely by our hospital's research and development department.
References
- 1.Reynolds WS, Dmochowski RR, Penson DF. Epidemiology of stress urinary incontinence in women. Curr Urol Rep. 2011;12:370–376. doi: 10.1007/s11934-011-0206-0. [DOI] [PubMed] [Google Scholar]
- 2.Berg S. Polytef augmentation urethroplasty. Correction of surgically incurable urinary incontinence by injection technique. Arch Surg. 1973;107:379–381. doi: 10.1001/archsurg.1973.01350210017006. [DOI] [PubMed] [Google Scholar]
- 3.Chapple CR, Haab F, Cervigni M, Dannecker C, Fianu-Jonasson A, Sultan AH. An open, multicentre study of NASHA/Dx Gel (Zuidex) for the treatment of stress urinary incontinence. Eur Urol. 2005;48:488–494. doi: 10.1016/j.eururo.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 4.Zarini E, Supino R, Pratesi G, et al. Biocompatibility and tissue interactions of a new filler material for medical use. Plast Reconstr Surg. 2004;114:934–942. doi: 10.1097/01.prs.0000133425.22598.d0. [DOI] [PubMed] [Google Scholar]
- 5.Christensen LH, Breiting VB, Aasted A, Jørgensen A, Kebuladze I. Long-term effects of polyacrylamide hydrogel on human breast tissue. Plast Reconstr Surg. 2003;111:1883–890. doi: 10.1097/01.PRS.0000056873.87165.5A. [DOI] [PubMed] [Google Scholar]
- 6.Rauso R. 5-year study of a polyacrylamide hydrogel-based filler for rehabilitation of hiv-related facial lipoatrophy. Aesthet Surg J. 2015 May 7; doi: 10.1093/asj/sjv036. 2015 May 7. pii: sjv036. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 7.Negredo E, Puig J, Ornelas A, et al. Ten-Year Safety with Polyacrylamide Gel Used to Correct Facial Lipoatrophy in HIV-Infected Patients. AIDS Res Hum Retroviruses. 2015;31:817–821. doi: 10.1089/AID.2015.0004. [DOI] [PubMed] [Google Scholar]
- 8.Lose G, Mouritsen L, Nielsen JB. A new bulking agent (polyacrylamide hydrogel) for treating stress urinary incontinence in women. BJU Int. 2006;98:100–104. doi: 10.1111/j.1464-410X.2006.06205.x. [DOI] [PubMed] [Google Scholar]
- 9.Toozs-Hobson P, Al-Singary W, Fynes M, Tegerstedt G, Lose G. Two-year follow-up of an open-label multicenter study of polyacrylamide hydrogel (Bulkamid®) for female stress and stress-predominant mixed incontinence. Int Urogynecology J. 2012;23:1373–1378. doi: 10.1007/s00192-012-1761-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gorton E, Stanton S, Monga A, Wiskind AK, Lentz GM, Bland DR. Periurethral collagen injection: a long-term follow-up study. BJU Int. 1999;84:966–971. doi: 10.1046/j.1464-410x.1999.00321.x. [DOI] [PubMed] [Google Scholar]
- 11.Abrams P, Avery K, Gardener N, Donovan J, ICIQ Advisory Board The International Consultation on Incontinence Modular Questionnaire: www.iciq.net. J Urol. 2006;175:1063–1066. doi: 10.1016/S0022-5347(05)00348-4. [DOI] [PubMed] [Google Scholar]
- 12.Stach-Lempinen B, Kujansuu E, Laippala P, Metsänoja R. Visual analogue scale, urinary incontinence severity score and 15 D--psychometric testing of three different health-related quality-of-life instruments for urinary incontinent women. Scand J Urol Nephrol. 2001;35:476–483. doi: 10.1080/003655901753367587. [DOI] [PubMed] [Google Scholar]
- 13.Ghoniem G, Corcos J, Comiter C, Westney OL, Herschorn S. Durability of urethral bulking agent injection for female stress urinary incontinence: 2-year multicenter study results. J Urol. 2010;183:1444–1449. doi: 10.1016/j.juro.2009.12.038. [DOI] [PubMed] [Google Scholar]
- 14.Narins RS, Coleman WP, Rohrich R, et al. 12-Month controlled study in the United States of the safety and efficacy of a permanent 2.5% polyacrylamide hydrogel soft-tissue filler. Dermatol Surg. 2010;(suppl 3):1819–1829. doi: 10.1111/j.1524-4725.2010.01736.x. [DOI] [PubMed] [Google Scholar]
- 15.Groenen R, Vos MC, Willekes C, Vervest HAM. Pregnancy and delivery after mid-urethral sling procedures for stress urinary incontinence: case reports and a review of literature. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:441–448. doi: 10.1007/s00192-007-0509-3. [DOI] [PubMed] [Google Scholar]
- 16.McGuire EJ. Pathophysiology of stress urinary incontinence. Rev Urol. 2004;(suppl 5):S11–7. [PMC free article] [PubMed] [Google Scholar]
- 17.Kanonidou Z, Karystianou G. Anesthesia for the elderly. Hippokratia. 2007;11:175–177. [PMC free article] [PubMed] [Google Scholar]
- 18.Koski ME, Enemchukwu EA, Padmanabhan P, Kaufman MR, Scarpero HM, Dmochowski RR. Safety and efficacy of sling for persistent stress urinary incontinence after bulking injection. Urology. 2011;77:1076–1080. doi: 10.1016/j.urology.2010.10.010. [DOI] [PubMed] [Google Scholar]
- 19.Martan A, Mašata J, Švabík K, El-Haddad R, Hubka P, Krhut J. [Transurethral injection of polyacrylamide hydrogel (Bulkamid®) for the treatment of recurrent stress urinary incontinence after failed tape surgery] Ceská Gynekol Ceská Lékarská Spolecnost J Ev Purkyne. 2015;80:25–29. [PubMed] [Google Scholar]
- 20.Sokol ER, Karram MM, Dmochowski R. Efficacy and safety of polyacrylamide hydrogel for the treatment of female stress incontinence: a randomized, prospective, multicenter North American study. J Urol. 2014;192:843–849. doi: 10.1016/j.juro.2014.03.109. [DOI] [PubMed] [Google Scholar]
- 21.Cloutier J, Blais A-S, Moore K, Bolduc S. Prospective study using a new bulking agent for the treatment of vesicoureteral reflux: polyacrylamide hydrogel. J Urol. 2013;190:1034–1037. doi: 10.1016/j.juro.2013.03.071. [DOI] [PubMed] [Google Scholar]
- 22.Lose G, Sørensen HC, Axelsen SM, Falconer C, Lobodasch K, Safwat T. An open multicenter study of polyacrylamide hydrogel (Bulkamid®) for female stress and mixed urinary incontinence. Int Urogynecology J. 2010;21:1471–1477. doi: 10.1007/s00192-010-1214-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mouritsen L, Lose G, Møller-Bek K. Long-term follow-up after urethral injection with polyacrylamide hydrogel for female stress incontinence. Acta Obstet Gynecol Scand. 2014;93:209–212. doi: 10.1111/aogs.12283. [DOI] [PubMed] [Google Scholar]
- 24.Albo ME, Richter HE, Brubaker L, et al. Burch colposuspension versus fascial sling to reduce urinary stress incontinence. N Engl J Med. 2007;356:2143–2155. doi: 10.1056/NEJMoa070416. [DOI] [PubMed] [Google Scholar]
- 25.Ward K, Hilton P, United Kingdom and Ireland Tension-free Vaginal Tape Trial Group Prospective multicentre randomised trial of tension-free vaginal tape and colposuspension as primary treatment for stress incontinence. BMJ. 2002;325:67. doi: 10.1136/bmj.325.7355.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ward KL, Hilton P, UK and Ireland TVT Trial Group Tension-free vaginal tape versus colposuspension for primary urodynamic stress incontinence: 5-year follow up. BJOG Int J Obstet Gynaecol. 2008;115:226–233. doi: 10.1111/j.1471-0528.2007.01548.x. [DOI] [PubMed] [Google Scholar]