Abstract
Background
Gastric and esophageal adenocarcinomas are major global cancer burdens. These cancer forms are characterized by a poor prognosis and a modest response to chemo- radio- and targeted treatment. Hence there is an obvious need for further enhanced diagnostic and treatment strategies. The aim of this study was to examine the expression and prognostic impact of human epidermal growth factor receptor 1 (HER1/EGFR) and 3 (HER3), as well as the occurrence of EGFR and KRAS mutations in gastric and esophageal adenocarcinoma.
Methods
Immunohistochemical expression of EGFR and HER3 was analysed in all primary tumours and a subset of lymph node metastases in a consecutive cohort of 174 patients with adenocarcinoma of the stomach, cardia and esophagus. The anti-HER3 antibody used was validated by siRNA-mediated knockdown, immunohistochemistry and quantitative real-time PCR. EGFR and KRAS mutation status was analysed by pyrosequencing tecchnology.
Results and Discussion
High EGFR expression was an independent risk factor for shorter overall survival (OS), whereas high HER3 expression was associated with a borderline significant trend towards a longer OS. KRAS mutations were present in only 4% of the tumours and had no prognostic impact. All tumours were EGFR wild-type. These findings contribute to the ongoing efforts to decide on the potential clinical value of different HERs and druggable mutations in gastric and esophageal adenocarcinomas, and attention is drawn to the need for more standardised investigational methods.
Introduction
Gastric adenocarcinoma is, although declining, the third most common cause of cancer-related death worldwide[1]. The incidence of esophageal and gastroesophageal junction adenocarcinoma is lower but has shown a substantial increase in Western countries in recent decades, most likely due to increasing rates of obesity, gastro-esophageal reflux and Barrett´s esophagus[2–6]. Recent insights into the molecular pathways of gastric and esophageal carcinogenesis have led to progress in treatment strategies. The introduction of neoadjuvant, perioperative and palliative chemo-, radio- and targeted therapy as a complement to surgical treatment has led to a prolonged median overall survival (OS)[7–10]. Still, in most parts of the world the five-year OS remains around 25%[3] and the median OS for patients in a palliative setting is below one year[10]. Thus, there is an obvious need for improved diagnostic and treatment strategies.
Human epidermal growth factor receptors, HER1 (EGFR), HER2, HER3 and HER4, are a family of receptor tyrosine kinases that activate intracellular signalling pathways in response to extracellular signals[11]. They have a general structure consisting of an extracellular ligand binding domain, a transmembrane region, an intracellular kinase domain and an intracellular c-terminal tail[11, 12]. When ligands bind to receptors on the extracellular domain[12], the receptors interact and form homo- or heterodimers with other members of the HER family[12]. One exception is HER2, which is not ligand-regulated[11, 13]. All HER tyrosine kinases but HER3, which has a severly impaired tyrosine kinase activity[11, 14], respond to the dimerization by phosphorylation of the c-terminal tail tyrosine residue, thus activating intracellular signalling pathways involved in cell proliferation, differentiation, migration and survival[12, 13, 15]. In this way, a diversity of homo- and heterodimer complexes with potential functional differences can form within the HER family[12].
Although the untangling of this network of signalling activities is far from completed, it is well established that the abnormal activation of these receptors, e.g. by ligand binding, receptor overexpression or mutations, is deeply involved in the pathogenesis of several solid tumours[16–18]. Along this line, both EGFR and HER3 have been suggested as prognostic markers in several types of cancer[17, 19–21] as well as drug targets[13, 22, 23], and also to be involved in drug resistance in e.g. breast, lung and ovarian cancers[12, 15, 24, 25]. However, data regarding the prognostic and predictive role of EGFR and HER3 alterations are conflicting[12, 22, 26, 27].
There are several studies related to the expression and prognostic impact of EGFR and HER3 alterations in gastric adenocarcinoma[19, 21, 26, 28, 29]. As regards esophageal adenocarcinoma, some studies have merely examined the expression of EGFR and HER3[30, 31], and very few have also reported their prognostic significance[32–34] [35].
The aim of this study was to examine the immunohistochemical (IHC) expression of EGFR and HER3, as well as the occurrence of EGFR and KRAS mutations, in gastric and esophageal adenocarcinoma, with particular reference to their relationship with clinicopathological factors, HER2 expression, and OS.
Materials and Methods
Study Design and Participants
The study was performed on a consecutive cohort of 174 patients with adenocarcinoma in the upper gastrointestinal tract (esophagus, cardia and stomach), who had been surgically treated in the university hospitals of Lund and Malmö during the period Jan 1st 2006 –Dec 31st 2010. The cohort has previously been described in detail[36–38]. In brief, all tumours were histopathologically re-examined. Siewert type 1 and 2 tumours were classified as esophageal and Siewert type 3 as gastric tumours. Clinical data, information on recurrence, vital status and cause of death were obtained from the medical charts. Patient and tumour characteristics are provided in S1 Table. None of the patients had received neoadjuvant treatment. All EU and national regulations and requirements for handling human samples have been fully complied with during the conduct of this project; i.e. decision no. 1110/94/EC of the European Parliament and of the Council (OJL126 18,5,94), the Helsinki Declaration on ethical principles for medical research involving human subjects, and the EU Council Convention on human rights and Biomedicine. The study was approved of by the Ethics committee of Lund University (ref nr 445/07), whereby the committee waived the need for consent other than by the option to opt out.
Tissue Microarrays
Tissue microarrays (TMA´s) were constructed using a semi-automated arraying device (TMArrayer, Pathology Devices, Westminister, MD, USA) as previously described[37, 39]. Two 1 mm tissue cores, each from a separate donor block, were obtained from all 174 primary tumours. In addition, two 1 mm cores were obtained from synchronous lymph node metastases in 81 cases, always representing two different lymph nodes in cases with more than one metastatic node. In cases with mixed morphology, samples were obtained from the intestinal component, since the poorly cohesive cells are more difficult to target. Intestinal metaplasia (IM), including Barrett´s esophagus, was sampled in 73 cases, normal squamous epithelium in 96 cases and normal gastric mucosa in 131 cases. Normal squamous epithelium and gastric mucosa was represented in single cores, IM in 1–3 cores.
Antibody Validation
Human gastric adenocarcinoma AGS cells were purchased from Sigma-Aldrich Co, St Loius MO, and growth medium, fetal bovine serum (FBS) and antibiotics from Nordic Biolabs AB, Täby Sweden. The cells were maintained in Kaighn´s modification of Ham´s F-12 medium supplemented with 10% FBS and antibiotics (100 U/ml penicillin and 100 μg/ml streptomycin) in a humified 5% CO2 atmosphere at 37°C. Antibody validation was performed by quantitative real-time PCR (qPCR) and immunocytochemistry of cells following siRNA transfection against HER3. All reagents were purchased from ThermoFisher Scientific, Rockford IL, unless stated otherwise.
For siRNA transfection, cells were seeded in T-25 flasks (5x105 cells) and incubated 72h at 37°C. The cells were then washed twice with PBS and received growth medium without FBS or antibiotics, together with lipofectamine 2000 and siRNA negative control or anti-HER3 (#s4780) in OptiMEM to a final siRNA concentration of 50 nM. The transfection was stopped after 4.5h, medium changed to full growth medium and the cells were left to recover overnight. The following day, cells were harvested and spun down to pellets. The pellets were either fixated, dehydrated and embedded in paraffin for immunocytochemistry or resuspended in RLT buffer (GmbH, Hilden, Germany) and stored in -20°C for qPCR.
For immunocytochemical analysis, cell pellet arrays were constructed from the paraffin-embedded cell pellets in the same manner as the tissue samples, as was the subsequent staining of the cells.
For qPCR analysis, the cell samples were thawed and spun down to remove cell debris. RNA purification was performed using QIAcube with RNeasy mini kit (QIAGEN). Prior to real-time PCR, cDNA reverse transcription was performed with the High-capacity cDNA reverse transcription kit and total cDNA concentration was determined using Qubit with the DNA HS kit. 10 ng per reaction of each sample was used to run real-time PCR with HER3 TaqMan gene expression assay, with samples run in triplicates (assay ID Hs00176538_m1). 18S was used as endogenous control (assay ID Hs03928985_g1).
Immunohistochemistry and staining evaluation
For IHC, consecutive unstained 4 μm sections were prepared from the TMA paraffin blocks and baked in a heated chamber for 120 minutes at 60°C. Endogenous peroxidase was blocked using peroxidase blocking reagent and then ready-to-use serum free protein block (both from Dako, Glostrup, Denmark) was applied. Antigen retrieval was performed automatically using HIER (PT link system Dako, pH 9, heated to 97°C for 20 minutes for HER3 and Target retrieval solution S1699 from Dako, 1:10, pH 9, heated to 121°C for 3 minutes in a pressure chamber for EGFR). For HER3, monoclonal rabbit antibody (clone SP71 Novus Biologicals LTD, Cambridge, UK) diluted 1:100 was applied and for EGFR monoclonal mouse antibody (clone 31G7 Invitrogen) diluted 1:25. All stainings were performed in an Autostainer Plus (Dako), visualized using DAB as chromogen and counterstained with hematoxylin (Dako´s EnVision Flex detection system).
EGFR as well as HER3 protein expression was evaluated using the guidelines for gastric HER2 biopsy specimen staining pattern[40] by a pathologist who was blinded to clinical and outcome data. In cases with different expression between the two cores, the one with the highest scoring was used, in accordance with the biopsy guidelines. Cytoplasmic staining was denoted as a separate category (4), but grouped with 0–1 in the statistical analyses. Protein expression was grouped as low (0–2 or 4) or high (3) in the statistical analyses. HER2 was evaluated as previously described[41].
Analysis of EGFR and KRAS mutation status
The PyroMark Q24 system (QIAGEN) was used for pyrosequencing analysis of EGFR and KRAS mutations in DNA from 1 mm formalin-fixed, paraffin-embedded tumour tissue cores. In brief, genomic DNA was extracted from tumour tissue in QIAamp MinElute spin columns (QIAGEN) and DNA regions of interest were amplified by PCR (Veriti 96 Well Fast Thermal Cykler, Applied Biosystems Inc., Foster City CA). Using therascreen KRAS Pyro Kit and EGFR Pyro Kit (QIAGEN) KRAS mutations of codon 12, 13 and 61 and EGFR deletions in exon 19 and mutations in exon 18 codon 719, exon 20 codon 768 plus 790 and exon 21 codon 858–861 were analysed. All samples with a potential low-level mutation were reexamined in duplicates.
Statistical Analysis
For analysis of the differences in EGFR and HER3 expression between tissue types, paired t-test was used. To analyse the relationship between EGFR and HER3 expression and clinicopathological parameters the non-parametric Mann-Whitney U test was applied for continuous variables and the chi-squared test for categorical variables. The OS rates according to EGFR as well as HER3 low expression (IHC 0–2) versus high expression (IHC3) were calculated using Kaplan-Meier analysis. The log rank test was used to assess differences in the Kaplan Meier curves. Unadjusted and adjusted hazard ratios (HR) for OS were calculated by Cox regression proportional hazard modeling. The adjusted model included age, sex, T stage, N stage, M stage, location, differentiation and resection margin. A backward conditional method was used for variable selection in the adjusted model. For all analyses, IBM SPSS Statistics version 22.0 (SPSS Inc., Chicago, IL, USA) was used. p-values <0.05 were considered significant. All tests were two-sided.
Results
Antibody validation
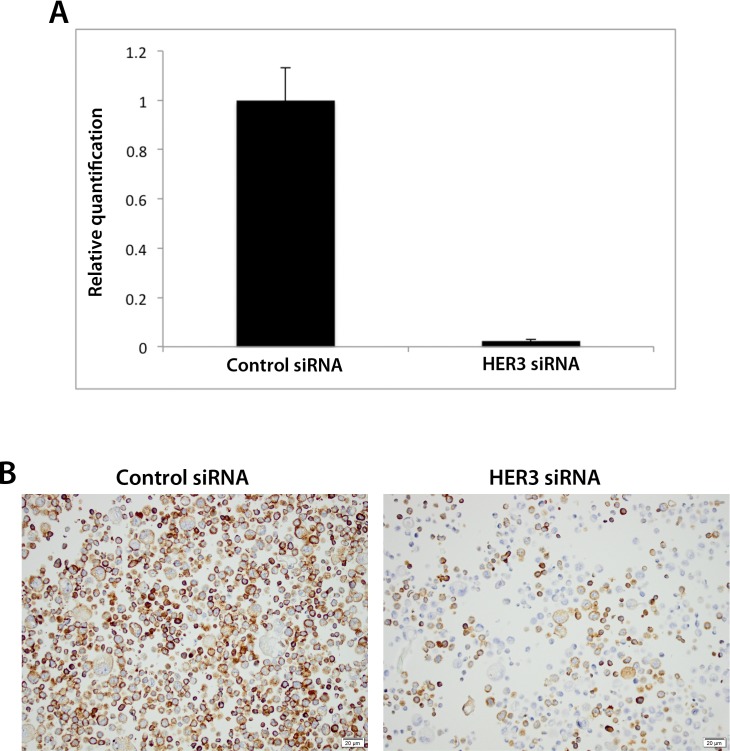
The siRNA-mediated knockdown of human gastric adenocarcinoma AGS cells was shown to be successful by qPCR analysis in that the levels of HER3 were substantially lower in cells treated with anti-HER3 siRNA compared to siRNA control (Fig 1).
Fig 1. Assessment of the specificity of the anti-HER3 antibody SP71 using siRNA technology and immunocytochemistry.
siRNA-mediated knockdown of HER3 in human gastric adenocarcinoma AGS cells as visualised by (A) real-time PCR and (B) immunocytochemistry of cells transfected with negative control or anti-HER3 siRNA. Graph displays relative quantification as mean ± SE. Representative graph and images from one of three independent experiments are shown.
For antibody validation, immunocytochemical staining displayed noticeably reduced expression of HER3 in cells transfected with anti-HER3, as compared with controls (Fig 1). This finding was in concordance with the knockdown visualized by qPCR and thus validates the specificity of the antibody.
Distribution of immunohistochemical EGFR and HER3 expression in benign tissue, primary tumours and paired lymph node metastases
EGFR could be evaluated in 45/96 (46.9%) samples with normal squamous epithelium, 116/131 (88.5%) samples with normal gastric mucosa, 53/73 (72.6%) samples with intestinal metaplasia (IM), 170/174 (97.7%) primary tumours and 71/81 (87.7%) metastases.
HER3 could be evaluated in 48/96 (50.0%) samples with normal squamous epithelium, 116/131 (88.5%) samples with normal gastric mucosa, 57/73 (78.1%) samples with IM, 168/174 (96.6%) primary tumours and 74/81 (91.4%) metastases. Sample immunohistochemical images are shown in Fig 2. As demonstrated in Fig 3, the expression of EGFR and HER3 was higher in tumours than in normal tissue, although this difference was not significant (data not shown). Conversion of protein expression between primary tumour and metastatic lymph nodes was seen in 8 cases (6 from low to high, 2 from high to low) for EGFR and in 4 cases (all low to high) for HER3.
Fig 2. Sample images of EGFR and HER3 protein expression.
Sample images (10X magnification) of EGFR and HER3 expression displaying score 0, (1a, 2a), score 1(1b, 2b), score 2(1c, 2c) and score 3 (1d, 2d).
Fig 3. Visualization of EGFR and HER3 expression according to tissue type.
Distribution of EGFR (left) and HER3 (right) expression according to tissue type in the entire cohort.
Associations of EGFR and HER3 expression in primary tumours with clinicopathological and investigative parameters
As shown in Table 1 there were no significant associations between IHC expression of EGFR and HER3 and conventional clinicopathological parameters.
Table 1. Associations of EGFR and HER3 protein expression with clinicopathological characteristics.
| Factor | EGFR | HER3 | ||||
|---|---|---|---|---|---|---|
| low | high | P | low | high | P | |
| n(%) | 162 (95.4) | 8 (4.7) | 128 (76.2) | 40 (23.8) | ||
| Age | ||||||
| Mean | 70.0 | 74.9 | 0.276 | 70.1 | 70.2 | 0.957 |
| Median | 69.3 | 75.1 | 69.6 | 71.0 | ||
| (Range) | 42.6–94.4 | 58.5–88.6 | 42.6–94.4 | 48.4–88.8 | ||
| Sex | ||||||
| Women | 38 (23.5) | 1 (12.5) | 0.473 | 27 (21.1) | 11 (27.5) | 0.399 |
| Men | 124 (76.5) | 7 (87.5) | 101 (78.9) | 29 (72.5) | ||
| T stage | ||||||
| 1 | 16 (10.0) | 1 (12.5) | 0.712 | 12 (9.5) | 4 (10.0) | 0.245 |
| 2 | 31 (19.4) | 1 (12.5) | 21 (16.7) | 10 (25.0) | ||
| 3 | 88 (55.0) | 4 (50.0) | 70 (55.6) | 22 (55.0) | ||
| 4 | 25 (15.6) | 2 (25.0) | 23 (18.3) | 4 (10.0) | ||
| Unknown | 2 | 2 | ||||
| N stage | ||||||
| 0 | 54 (33.3) | 2 (25.0) | 0.917 | 36 (28.1) | 19 (47.5) | 0.278 |
| 1 | 27 (16.7) | 3 (37.5) | 25 (19.5) | 4 (10.0) | ||
| 2 | 40 (24.7) | 1 (12.5) | 36 (28.1) | 5 (12.5) | ||
| 3 | 41 (25.3) | 2 (25.0) | 31 (24.2) | 12 (30.0) | ||
| M Stage | ||||||
| 0 | 142 (87.7) | 6 (75.0) | 0.299 | 109 (85.2) | 37 (92.5) | 0.231 |
| 1 | 20 (12.3) | 2 (25.0) | 19 (14.8) | 3(7.5) | ||
| Differentiation grade | ||||||
| High | 8 (4.9) | 0 (0.0) | 0.924 | 5 (3.9) | 2 (5.0) | 0.078 |
| Intermediate | 48 (29.6) | 3 (37.5) | 34 (26.6) | 17 (42.5) | ||
| Low | 106 (65.4) | 5 (62.5) | 89 (69.5) | 21 (52.5) | ||
| Morphology | ||||||
| Intestinal | 109 (67.3) | 8 (100.0) | 0.059 | 91 (71.1) | 25 (62.5) | 0.186 |
| Diffuse | 44 (27.2) | 0 (0.0) | 29 (22.7) | 14 (35.0) | ||
| Mixed | 9 (5.6) | 0 (0.0) | 8 (6.3) | 1 (2.5) | ||
| Location | ||||||
| Esophageal | 66 (40.7) | 4 (50.0) | 0.605 | 57 (44.5) | 12 (30.0) | 0.104 |
| Gastric | 96 (59.3) | 4 (50.0) | 71 (55.5) | 28 (70.0) | ||
| Resection margin | ||||||
| R0 | 116 (71.6) | 4 (50.0) | 0.192 | 87 (68.0) | 31 (77.5) | 0.251 |
| R1, Rx | 46 (28.4) | 4 (50.0) | 41 (32.0) | 9 (22.5) | ||
| HER2 status* | ||||||
| No overexpression | 125 (81.7) | 6 (75.0) | 0.636 | 106 (84.4) | 24 (68.6 | 0.030 |
| Overexpression | 28 (18.3) | 2 (25.0) | 19 (15.2) | 11 (31.4) | ||
| Unknown | 9 | 3 | ||||
Low expression = immunohistochemical score 0–2 or 4, high expression = immunohostochemical score 3
R0 = radical resection according to pathology report, R1 = non-radical resection, Rx = margin status uncertain
N1 = metastasis in 1–2 regional lymph nodes, N2 = metastasis in 3–6 regional lymph nodes, N3 = metastasis in 7 or more regional lymph nodes
*Overexpression = IHC3+ and/or amplified
A significant correlation was seen between overexpression of HER2 and HER3 (p = 0.030). There was no significant correlation between EGFR and HER3 expression (data not shown).
Impact of EGFR and HER3 expression on survival
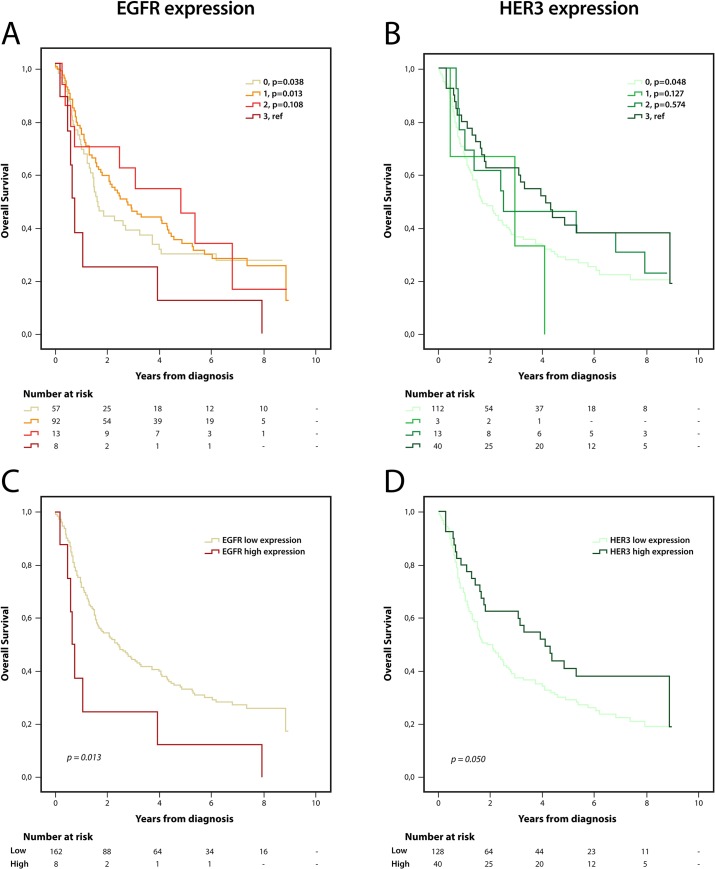
Kaplan Meier analysis of the impact of EGFR and HER3 expression on OS is shown in Fig 4. As regards EGFR, high (3) expression was associated with the shortest OS, compared with all other categories of expression, with significant differences in relation to negative (0) and weak (1) expression (Fig 4A), also using a dichotomized variable of 0–2 vs 3 (Fig 4C). This correlation was not significant when the analysis was stratified for esophageal and gastric location (data not shown). Conversely, patients with tumours expressing high levels of HER3 had a prolonged OS, although this difference was only significant between tumours with high (3) and negative (0) expression (Fig 4B), remaining borderline significant with a dichotomized variable of 0–2 vs 3 (Fig 4D). Analysis in strata according to location revealed that the prognostic impact of EGFR was significant in esophageal cancer (p = 0.014), but non-significant in gastric cancer. Of note, the groups were very small (4 patients had esophageal tumours with high expression of EGFR).
Fig 4. Kaplan-Meier estimates of overall survival according to EGFR and HER3 expression.
Overall survival according to all (A) EGFR and (B) HER3 scores, and according to dichotomized (C) EGFR and (D) HER3 scores.
As shown in Table 2, the prognostic value of EGFR was confirmed in unadjusted as well as in adjusted Cox regression analysis in relation to OS (HR = 2.42; 95% CI 1.18–4.96, p = 0.016 and HR = 2.42; 95% CI 1.16–5.07, p = 0.019, respectively). HER3 was borderline prognostic in unadjusted, but not in adjusted, Cox regression analysis (HR = 0.65; 95% CI 0.41–1.04, p = 0.052 and HR = 0.92; 95% CI 0.57–1.48, p = 0.732, respectively). Conversion between primary tumour and lymph node metastasis had no prognostic impact for EGFR or HER3 (p = 0.998 and 0.375, respectively, data not shown).
Table 2. Hazard ratio for death according to clinicopathological factors, EGFR and HER3 overexpression.
| Overall survival | ||||||
|---|---|---|---|---|---|---|
| Unadjusted | p-value | Adjusted | p-value | |||
| n (events) | HR (95%CI) | n (events) | HR (95%CI) | |||
| Age | ||||||
| Continuous | 173 (126) | 1.03 (1.02–1.05) | <0.001 | 166 (122) | 1.04 (1.03–1.06) | 0 < .001 |
| Gender | ||||||
| Female | 40 (31) | 1.00 | 38 (29) | 1.00 | ||
| Male | 133 (95) | 0.75 (0.50–1.13) | 0.166 | 128 (93) | 0.95 (0.59–1.54) | 0.830 |
| T-stage | ||||||
| T1 | 18 (7) | 1.00 | 16 (7) | 1.00 | ||
| T2 | 32 (21) | 2.11 (0.89–4.96) | 0.089 | 31 (20) | 1.36 (0.55–2.32) | 0.506 |
| T3 | 93 (73) | 3.22 (1.48–7.03) | 0.003 | 92 (72) | 1.58 (0.70–3.58) | 0.272 |
| T4 | 27 (23) | 4.81 (2.05–11.30) | <0.001 | 27 (23) | 2.18 (0.86–5.52) | 0.101 |
| N-stage | ||||||
| N0 | 58 (32) | 1.00 | 55 (30) | 1.00 | ||
| N1 | 30 (22) | 1.56 (0.90–2.68) | 0.111 | 29 (22) | 1.97 (1.12–3.45) | 0.017 |
| N2 | 41 (32) | 2.00 (1.22–3.27) | 0.006 | 41 (32) | 2.75 (1.62–4.65) | <0.001 |
| N3 | 44 (40) | 3.49 (2.14–5.60) | <0.001 | 41 (38) | 4.77 (2.80–8.14) | <0.001 |
| M-stage | ||||||
| M0 | 151 (104) | 1.00 | 144 (100) | 1.00 | ||
| M1 | 22 (22) | 2.58 (1.61–4.14) | <0.001 | 22 (22) | 1.51 (0.92–2.49) | 0.107 |
| Location | ||||||
| Esophagus (including Siewert 1–2) | 70 (50) | 1.00 | 68 (50) | 1.00 | ||
| Stomach | 103 (76) | 1.04 (0.73–1.49) | 0.836 | 98 (72) | 1.15 (0.76–1.74) | 0.505 |
| Differentiation | ||||||
| High-Moderate | 60 (36) | 1.00 | 57 (36) | 1.00 | ||
| Low | 113 (90) | 1.64 (1.12–2.43) | 0.012 | 109 (86) | 1.37 (0.92–2.05) | 0.125 |
| Resection margin | ||||||
| R0 | 121 (77) | 1.00 | 117 (76) | 1.00 | ||
| R1, Rx | 52 (49) | 2.80 (1.92–4.07) | <0.001 | 49 (46) | 2.22 (1.49–3.30) | 0 < .001 |
| EGFR expression | ||||||
| Low (IHC 0–2) | 162 (116) | 1.00 | 158 (114) | 1.00 | ||
| High (IHC 3) | 8 (8) | 2.42 (1.18–4.96) | 0.016 | 8 (8) | 2.42 (1.16–5.07) | 0.019 |
| HER3 expression | ||||||
| Low (IHC 0–2) | 128 (98) | 1.00 | 126 (97) | 1.00 | ||
| High (IHC 3) | 40 (25) | 0.65 (0.41–1.04) | 0.052 | 40(25) | 0.92 (0.57–1.48) | 0.732 |
N1 = metastasis in 1–2 regiona lymph nodes, N2 = metastasis in 3–6 regional lymph nodes, N3 = metastasis in 7 or more regional lymph nodes
Occurrence of EGFR and KRAS mutations in primary tumours
Analyses of EGFR and KRAS mutations were successfully performed in 170/174 (97.7%) primary tumours. Seven cases (4.1%) were KRAS-mutated, 4 in codon 12 and 3 in codon 13. The distribution of KRAS mutation was similar in gastric and esophageal tumours, 3 (4.3%) and 4 (4.0%) respectively. None of the tumours were EGFR-mutated.
Kaplan Meier analysis revealed no significant correlation between KRAS mutation status and OS, neither in the entire cohort, nor in strata according to tumour location (data not shown). Because of the low percentage of KRAS-mutated tumours, no further statistical analyses were performed.
There were no significant correlations between KRAS mutation status and expression of EGFR, HER2 or HER3, (data not shown).
Discussion
In this study we examined the protein expression of EGFR and HER3 as well as the mutational status of EGFR and KRAS in gastric and esophageal adenocarcinoma. High EGFR expression was found to be an independent risk factor for shorter OS, whereas high HER3 expression was associated with a borderline significant trend towards a longer OS. KRAS mutations were present in only 4% of the tumours and all tumours were EGFR wild-type.
As described above, EGFR and HER3 are members of the HER family that forms an integral part of a complex signalling network. In normal cells, EGFR plays an essential role in e.g. organogenesis[14, 18], but structural alterations as well as overexpression of EGFR is seen in many types of cancer[18]. HER3 also has important functions in normal development,[15, 18], cell proliferation and survival[14, 15]. As with EGFR, increased expression of HER3 is seen in several cancer forms[18] and although it has a severely impaired intrinsic tyrosine kinase activity [11, 13, 17], making heterodimerization with other HER family members essential[12, 42], HER3 has been demonstrated to function as a, possibly HER2-dependent, oncogene[11, 23, 43]. In vitro and in vivo studies demonstrate that the oncogenic function of HER3 appears to lie predominantly in its ability to activate PI3K and Akt signalling by binding directly to the regulatory sites of PI3K [11, 44], which is unique within the HER family[12, 45].
KRAS acts downstream of EGFR, in the RAS-RAF-MAP pathway[46]. Activating mutations in KRAS are common in colorectal cancer[47] but have also been reported in 5–16% of gastric and esophageal adenocarcinomas[27, 48, 49], causing unregulated signalling along its pathway, independently of EGFR status. KRAS mutations do not appear to be prognostic in gastric or gastroesophageal junction adenocarcinoma[49, 50]. As regards EGFR mutations, these appear to be rare in gastric and esophageal adenocarcinomas[27, 48, 51, 52], as also supported by the results in this study wherein all tumours were found to be EGFR wild-type.
Hence, EGFR and HER3 are potential prognostic biomarkers and drug targets. The most promising drug agents are monoclonal antibodies (mAbs) and tyrosine kinase inhibitors (TKIs)[13]. mAbs target the extracellular ligand-binding domain whereas TKIs target the intracellular tyrosine kinase domain to interrupt downstream signaling[13]. Several mAbs[13, 53–55] as well as TKIs[13, 27, 51, 52, 56, 57] directed against EGFR have been evaluated in different settings for metastatic esophageal and gastric cancer. mAbs against HER3 have also been examined, mostly in preclinical settings but also in clinical trials e.g. for breast and colorectal cancer[13, 58, 59]. Moreover, HER3 may function as a signalling hub for the HER family, that leads to compensatory pathways when other HER receptors are blocked[60], thus promoting resistance to multiple therapeutic agents[12, 15, 24]. For TKIs, this appears to happen by a compensatory upregulation of membranous HER3, possibly due to MET-amplification[43], via a shift in the HER3 phosphorylation-dephosphorylation equilibrium, making the effect of the drug transient[11, 24]. The importance of the role of HER3 is further exemplified in the study by Garrett et al where HER3 was upregulated in breast tumours after inhibition of HER2 with lapatinib, but where inhibition of HER3 sensitized HER2-positive breast cancer cells to lapatinib[59]. A study by Tao et al showed a similar upregulation of HER3 as described above, which was reduced by the addition of a dual EGFR and HER3 inhibitor[61]. Although some drug trials, for example on mAbs targeting EGFR, have had limitations such as lack of control arm[13], the results have been discouraging with an only modestly improved, or sometimes even shortened, OS[13, 27, 51, 52, 56]. A few studies have however demonstrated more promising results, for example by dual inhibition of both EGFR and HER3 as described above[13, 57, 58, 61, 62].
Of note, none of the patients included in the present study had received neoadjuvant treatment, and very few received adjuvant chemotherapy. Therefore, the relationship between EGFR and HER3 expression and survival should reflect their potential prognostic values. However, as patients with gastric and esophageal cancer are increasingly being treated with neoadjuvant therapy, future studies should also examine the effects of neoadjuvant treatment by comparing the expression and predictive effects of different HERs, in particular HER3, in tumour tissue before and after treatment.
In line with the results from this study, the majority of reports on the prognostic impact of EGFR expression in gastric and esophageal adenocarcinoma have demonstrated correlations with shorter OS[20, 21, 29, 33], although one study found an independent correlation to a longer OS[63]. HER3 expression has also been correlated with shorter OS in gastric as well as other cancer forms[17, 19, 26], but also with longer, or trends towards longer, OS in colorectal and breast cancer[60, 64, 65]. Other studies could not demonstrate any prognostic impact for EGFR[26, 27, 32] or HER3 [27] in upper gastrointestinal cancer. Of note, comparatively few studies related to EGFR and HER3 expression in upper gastrointestinal cancer have included the esophagus, which is somewhat surprising considering the increasing incidence of esophageal adenocarcinoma and indications of better EGFR TKI response in esophageal than gastric adenocarcinoma[13].
The reason for HER3 being upregulated in tumours but not having any clear impact on OS could be that it is expressed in non-proliferating parts of a tumour, in line with the HER3 expression pattern in the upper, non-proliferating parts of normal colonic crypts, as indicated in a study by Jarde[66]. This could also shed light on why studies on HER3-targeting drugs have been disappointing, as these drugs may target differentiated cells and contribute to the elimination of the tumour bulk, but not affect the proliferative cancer stem cell-like population.
While the lack of consistent results may raise questions with regard to the suitability of EGFR and HER3 as druggable targets in upper gastrointestinal cancer, it is noteworthy that many of the studies used different methods to evaluate EGFR and HER3 alterations, such as mutation analyses[27, 52], gene copy number analyses[21, 27, 34, 51], mRNA analyses[27] and different antibodies and evaluation systems for IHC protein expression[19, 20, 29, 67],[21, 26, 31–34]. There is also a considerable variation in biomarker inclusion criteria of different clinical trials[52–54, 56]. The reported rates of overexpression vary from 2–40% for EGFR[19, 26, 32] and from 20–87% for HER3[34, 67]. It is well established that the use of validated antibodies is of the utmost importance in order to achieve correct reults[68]. The need for validated methods and testing algorithms for EGFR and HER3 has been highlighted in several studies[17, 29, 51] and differences in the reported rates of overexpression may mainly be due to non-standardized testing procedures, as others have suggested before us[69]. Of note, the true effects of trastuzumab on HER2-overexpressing breast cancer were discovered synchronously with the development of an optimal technique to evaluate the biomarker[9, 17]. Moreover, few studies attempted to control for other important prognostic factors that may have confounded the association with survival[20, 67], which may affect the result. Therefore, to render our results credibility, we used a well-validated EGFR antibody[70, 71]. Since not many validation studies for HER3 antibodies have been performed and to our best knowledge none that demonstrated sufficient specificity and sensitivity[71], we have herein performed a thorough validation of the herein used anti-HER3 antibody, demonstrating its specificity, for the HER3 antibody we used. Moreover, to date, no classification system has been implemented for assessment of EGFR or HER3 status in gastric or esophageal cancer. To our best knowledge, we have used the best validated and most widely used evaluation systems for gastric HER family scoring[17, 29, 72, 73], and we have described our scoring system carefully to make our study easily reproducible. One other study used the same scoring system and cut-off level, and their results demonstrated a significant correlation between EGFR expression and shorter OS[29]. We chose the cutoff level 0–2 versus 3 with clinical perspective as this has been shown to have the best therapeutic correlation for HER2. A possible limitation to our study is that the analyses have been performed on TMAs, which confers an inherent risk of sampling bias. It must however be pointed out that full-face sections also represent only a fraction of the tumour, and the TMA technique is a well-validated tool for biomarker studies[73, 74]. Of note, in our study, each of the two cores representing the primary tumour and lymph node metastases, respectively, was, whenever possible taken from two different blocks from the primary tumour and from separate metastases, to further reduce the risk of sampling bias.
As a cautionary remark, several of the herein presented results are derived from analyses of rather small subgroups and need validation in additional patient cohorts.
HER3 expression was highly concordant between primary tumours and lymph node metastases, which is in line with a study examining HER3 expression in colorectal cancer[22]. The proportion of cases with primary-lymph node conversion was higher for EGFR, and this has, to our best knowledge, not been reported previously. In contrast to previous findings regarding HER2 expression in the herein investigated cohort[41], conversion of EGFR or HER3 had no prognostic impact. The significant correlation between HER2 and HER3 is in accordance with previous studies and further underlines their close relationship[67].
Taken together, the results from this study demonstrate divergent prognostic roles for EGFR and HER3 expression in gastric and esophageal adenocarcinoma, based on IHC analysis of chemo- radiotherapy-naive tumours from a clinically well-characterized, consecutive cohort of surgically treated patients. Moreover, KRAS mutations were found to be rare and all tumours were EGFR wild-type. These findings contribute to the ongoing efforts to decide on the potential clinical value of different HERs and druggable mutations in gastric and esophageal adenocarcinoma.
Supporting Information
R0 = Radical resection according to pathology report, R1 = non-radical resection, Rx = resection margin uncertain. N1 = metastasis in 1–2 regional lymph nodes, N2 = metastasis in 3–6 regional lymph nodes, N3 = metastasis in 7 or more regional lymph nodes.
(DOCX)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by Swedish Cancer Society, KJ 2014/540, the Crafoord Foundation, to JE; the Olle Engkvist Foundation, to JE; the Anna Lisa and Sven-Eric Lundgren Foundation, to JE; the Mrs Berta Kamprad Foundation, to JE; Lund University Faculty of Medicine, to KJ; Lund University Hospital Research Grants, to KJ; and the Swedish Government Grant for Clinical Research, to CH JE KJ. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. International journal of cancer Journal international du cancer. 2014. 10.1002/ijc.29210 . [DOI] [PubMed] [Google Scholar]
- 2.Bosetti C, Levi F, Ferlay J, Garavello W, Lucchini F, Bertuccio P, et al. Trends in oesophageal cancer incidence and mortality in Europe. International journal of cancer Journal international du cancer. 2008;122(5):1118–29. 10.1002/ijc.23232 . [DOI] [PubMed] [Google Scholar]
- 3.Society AC. Global Cancer Facts & Figures 2nd Edition Atlanta: American Cancer Society; 2011. [cited 2011]. 2nd:[Available from: http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-027766.pdf. [Google Scholar]
- 4.Lauwers GY. Epithelial Neoplasms of the Stomach In: Odze RD, Goldblum JR, editors. Surgical Pathology of the GI Tract, Liver, Biliary Tract and Pancreas: Expert Consult—Online and Print. 1. 2d ed. Philadelphia: Saunders Elsevier; 2009. p. 563–80. [Google Scholar]
- 5.Devesa SS, Blot WJ, Fraumeni JF Jr. Changing patterns in the incidence of esophageal and gastric carcinoma in the United States. Cancer. 1998;83(10):2049–53. . [PubMed] [Google Scholar]
- 6.Buas MF, Vaughan TL. Epidemiology and risk factors for gastroesophageal junction tumors: understanding the rising incidence of this disease. Seminars in radiation oncology. 2013;23(1):3–9. 10.1016/j.semradonc.2012.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cunningham D, Allum WH, Stenning SP, Thompson JN, Van de Velde CJ, Nicolson M, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. The New England journal of medicine. 2006;355(1):11–20. 10.1056/NEJMoa055531 . [DOI] [PubMed] [Google Scholar]
- 8.van Hagen P, Hulshof MC, van Lanschot JJ, Steyerberg EW, van Berge Henegouwen MI, Wijnhoven BP, et al. Preoperative chemoradiotherapy for esophageal or junctional cancer. The New England journal of medicine. 2012;366(22):2074–84. 10.1056/NEJMoa1112088 . [DOI] [PubMed] [Google Scholar]
- 9.Bang YJ, Van Cutsem E, Feyereislova A, Chung HC, Shen L, Sawaki A, et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet. 2010;376(9742):687–97. 10.1016/S0140-6736(10)61121-X . [DOI] [PubMed] [Google Scholar]
- 10.Group G, Oba K, Paoletti X, Bang YJ, Bleiberg H, Burzykowski T, et al. Role of chemotherapy for advanced/recurrent gastric cancer: an individual-patient-data meta-analysis. European journal of cancer. 2013;49(7):1565–77. 10.1016/j.ejca.2012.12.016 . [DOI] [PubMed] [Google Scholar]
- 11.Hsieh AC, Moasser MM. Targeting HER proteins in cancer therapy and the role of the non-target HER3. British journal of cancer. 2007;97(4):453–7. 10.1038/sj.bjc.6603910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Amin DN, Campbell MR, Moasser MM. The role of HER3, the unpretentious member of the HER family, in cancer biology and cancer therapeutics. Seminars in cell & developmental biology. 2010;21(9):944–50. 10.1016/j.semcdb.2010.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Desai MD, Saroya BS, Lockhart AC. Investigational therapies targeting the ErbB (EGFR, HER2, HER3, HER4) family in GI cancers. Expert opinion on investigational drugs. 2013;22(3):341–56. 10.1517/13543784.2013.761972 . [DOI] [PubMed] [Google Scholar]
- 14.Yarden Y, Pines G. The ERBB network: at last, cancer therapy meets systems biology. Nature reviews Cancer. 2012;12(8):553–63. 10.1038/nrc3309 . [DOI] [PubMed] [Google Scholar]
- 15.Mujoo K, Choi BK, Huang Z, Zhang N, An Z. Regulation of ERBB3/HER3 signaling in cancer. Oncotarget. 2014;5(21):10222–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hynes NE, Lane HA. ERBB receptors and cancer: the complexity of targeted inhibitors. Nature reviews Cancer. 2005;5(5):341–54. 10.1038/nrc1609 . [DOI] [PubMed] [Google Scholar]
- 17.Ocana A, Vera-Badillo F, Seruga B, Templeton A, Pandiella A, Amir E. HER3 overexpression and survival in solid tumors: a meta-analysis. Journal of the National Cancer Institute. 2013;105(4):266–73. 10.1093/jnci/djs501 . [DOI] [PubMed] [Google Scholar]
- 18.Yarden Y, Sliwkowski MX. Untangling the ErbB signalling network. Nature reviews Molecular cell biology. 2001;2(2):127–37. 10.1038/35052073 . [DOI] [PubMed] [Google Scholar]
- 19.Hayashi M, Inokuchi M, Takagi Y, Yamada H, Kojima K, Kumagai J, et al. High expression of HER3 is associated with a decreased survival in gastric cancer. Clinical cancer research: an official journal of the American Association for Cancer Research. 2008;14(23):7843–9. 10.1158/1078-0432.CCR-08-1064 . [DOI] [PubMed] [Google Scholar]
- 20.Chen C, Yang JM, Hu TT, Xu TJ, Yan G, Hu SL, et al. Prognostic role of human epidermal growth factor receptor in gastric cancer: a systematic review and meta-analysis. Archives of medical research. 2013;44(5):380–9. 10.1016/j.arcmed.2013.07.001 . [DOI] [PubMed] [Google Scholar]
- 21.Kim MA, Lee HS, Lee HE, Jeon YK, Yang HK, Kim WH. EGFR in gastric carcinomas: prognostic significance of protein overexpression and high gene copy number. Histopathology. 2008;52(6):738–46. 10.1111/j.1365-2559.2008.03021.x . [DOI] [PubMed] [Google Scholar]
- 22.Ledel F, Stenstedt K, Hallstrom M, Ragnhammar P, Edler D. HER3 expression in primary colorectal cancer including corresponding metastases in lymph node and liver. Acta oncologica. 2015;54(4):480–6. 10.3109/0284186X.2014.983654 . [DOI] [PubMed] [Google Scholar]
- 23.Jaiswal BS, Kljavin NM, Stawiski EW, Chan E, Parikh C, Durinck S, et al. Oncogenic ERBB3 mutations in human cancers. Cancer cell. 2013;23(5):603–17. 10.1016/j.ccr.2013.04.012 . [DOI] [PubMed] [Google Scholar]
- 24.Sergina NV, Rausch M, Wang D, Blair J, Hann B, Shokat KM, et al. Escape from HER-family tyrosine kinase inhibitor therapy by the kinase-inactive HER3. Nature. 2007;445(7126):437–41. 10.1038/nature05474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Campbell MR, Amin D, Moasser MM. HER3 comes of age: new insights into its functions and role in signaling, tumor biology, and cancer therapy. Clinical cancer research: an official journal of the American Association for Cancer Research. 2010;16(5):1373–83. 10.1158/1078-0432.CCR-09-1218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Begnami MD, Fukuda E, Fregnani JH, Nonogaki S, Montagnini AL, da Costa WL Jr., et al. Prognostic implications of altered human epidermal growth factor receptors (HERs) in gastric carcinomas: HER2 and HER3 are predictors of poor outcome. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2011;29(22):3030–6. 10.1200/JCO.2010.33.6313 . [DOI] [PubMed] [Google Scholar]
- 27.Wainberg ZA, Lin LS, DiCarlo B, Dao KM, Patel R, Park DJ, et al. Phase II trial of modified FOLFOX6 and erlotinib in patients with metastatic or advanced adenocarcinoma of the oesophagus and gastro-oesophageal junction. British journal of cancer. 2011;105(6):760–5. 10.1038/bjc.2011.280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kimura M, Tsuda H, Morita D, Ichikura T, Ogata S, Aida S, et al. A proposal for diagnostically meaningful criteria to classify increased epidermal growth factor receptor and c-erbB-2 gene copy numbers in gastric carcinoma, based on correlation of fluorescence in situ hybridization and immunohistochemical measurements. Virchows Archiv: an international journal of pathology. 2004;445(3):255–62. 10.1007/s00428-004-1048-7 . [DOI] [PubMed] [Google Scholar]
- 29.Terashima M, Kitada K, Ochiai A, Ichikawa W, Kurahashi I, Sakuramoto S, et al. Impact of expression of human epidermal growth factor receptors EGFR and ERBB2 on survival in stage II/III gastric cancer. Clinical cancer research: an official journal of the American Association for Cancer Research. 2012;18(21):5992–6000. 10.1158/1078-0432.CCR-12-1318 . [DOI] [PubMed] [Google Scholar]
- 30.Fichter CD, Timme S, Braun JA, Gudernatsch V, Schopflin A, Bogatyreva L, et al. EGFR, HER2 and HER3 dimerization patterns guide targeted inhibition in two histotypes of esophageal cancer. International journal of cancer Journal international du cancer. 2014;135(7):1517–30. 10.1002/ijc.28771 . [DOI] [PubMed] [Google Scholar]
- 31.Wei Q, Chen L, Sheng L, Nordgren H, Wester K, Carlsson J. EGFR, HER2 and HER3 expression in esophageal primary tumours and corresponding metastases. International journal of oncology. 2007;31(3):493–9. . [PubMed] [Google Scholar]
- 32.Wilkinson NW, Black JD, Roukhadze E, Driscoll D, Smiley S, Hoshi H, et al. Epidermal growth factor receptor expression correlates with histologic grade in resected esophageal adenocarcinoma. Journal of gastrointestinal surgery: official journal of the Society for Surgery of the Alimentary Tract. 2004;8(4):448–53. 10.1016/j.gassur.2004.01.006 . [DOI] [PubMed] [Google Scholar]
- 33.Gibson MK, Abraham SC, Wu TT, Burtness B, Heitmiller RF, Heath E, et al. Epidermal growth factor receptor, p53 mutation, and pathological response predict survival in patients with locally advanced esophageal cancer treated with preoperative chemoradiotherapy. Clinical cancer research: an official journal of the American Association for Cancer Research. 2003;9(17):6461–8. . [PubMed] [Google Scholar]
- 34.Yoon HH, Sukov WR, Shi Q, Sattler CA, Wiktor AE, Diasio RB, et al. HER-2/neu gene amplification in relation to expression of HER2 and HER3 proteins in patients with esophageal adenocarcinoma. Cancer. 2014;120(3):415–24. 10.1002/cncr.28435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang KL, Wu TT, Choi IS, Wang H, Resetkova E, Correa AM, et al. Expression of epidermal growth factor receptor in esophageal and esophagogastric junction adenocarcinomas: association with poor outcome. Cancer. 2007;109(4):658–67. 10.1002/cncr.22445 . [DOI] [PubMed] [Google Scholar]
- 36.Jonsson L, Hedner C, Gaber A, Korkocic D, Nodin B, Uhlen M, et al. High expression of RNA-binding motif protein 3 in esophageal and gastric adenocarcinoma correlates with intestinal metaplasia-associated tumours and independently predicts a reduced risk of recurrence and death. Biomarker research. 2014;2:11 10.1186/2050-7771-2-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fristedt R, Gaber A, Hedner C, Nodin B, Uhlen M, Eberhard J, et al. Expression and prognostic significance of the polymeric immunoglobulin receptor in esophageal and gastric adenocarcinoma. J Transl Med. 2014;12(1):83 10.1186/1479-5876-12-83 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hedner C, Gaber A, Korkocic D, Nodin B, Uhlen M, Kuteeva E, et al. SATB1 is an independent prognostic factor in radically resected upper gastrointestinal tract adenocarcinoma. Virchows Arch. 2014. 10.1007/s00428-014-1667-6 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kononen J, Bubendorf L, Kallioniemi A, Barlund M, Schraml P, Leighton S, et al. Tissue microarrays for high-throughput molecular profiling of tumor specimens. Nat Med. 1998;4(7):844–7. Epub 1998/07/14. . [DOI] [PubMed] [Google Scholar]
- 40.Ruschoff J, Hanna W, Bilous M, Hofmann M, Osamura RY, Penault-Llorca F, et al. HER2 testing in gastric cancer: a practical approach. Modern pathology: an official journal of the United States and Canadian Academy of Pathology, Inc. 2012;25(5):637–50. 10.1038/modpathol.2011.198 . [DOI] [PubMed] [Google Scholar]
- 41.Hedner C, Tran L, Borg D, Nodin B, Jirstrom K, Eberhard J. Discordant human epidermal growth factor receptor 2 overexpression in primary and metastatic upper gastrointestinal adenocarcinoma signifies poor prognosis. Histopathology. 2015. 10.1111/his.12744 . [DOI] [PubMed] [Google Scholar]
- 42.Pinkas-Kramarski R, Soussan L, Waterman H, Levkowitz G, Alroy I, Klapper L, et al. Diversification of Neu differentiation factor and epidermal growth factor signaling by combinatorial receptor interactions. The EMBO journal. 1996;15(10):2452–67. [PMC free article] [PubMed] [Google Scholar]
- 43.Engelman JA, Zejnullahu K, Mitsudomi T, Song Y, Hyland C, Park JO, et al. MET amplification leads to gefitinib resistance in lung cancer by activating ERBB3 signaling. Science. 2007;316(5827):1039–43. 10.1126/science.1141478 . [DOI] [PubMed] [Google Scholar]
- 44.Soltoff SP, Carraway KL 3rd, Prigent SA, Gullick WG, Cantley LC. ErbB3 is involved in activation of phosphatidylinositol 3-kinase by epidermal growth factor. Molecular and cellular biology. 1994;14(6):3550–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fedi P, Pierce JH, di Fiore PP, Kraus MH. Efficient coupling with phosphatidylinositol 3-kinase, but not phospholipase C gamma or GTPase-activating protein, distinguishes ErbB-3 signaling from that of other ErbB/EGFR family members. Molecular and cellular biology. 1994;14(1):492–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McCubrey JA, Steelman LS, Abrams SL, Lee JT, Chang F, Bertrand FE, et al. Roles of the RAF/MEK/ERK and PI3K/PTEN/AKT pathways in malignant transformation and drug resistance. Advances in enzyme regulation. 2006;46:249–79. 10.1016/j.advenzreg.2006.01.004 . [DOI] [PubMed] [Google Scholar]
- 47.Kocarnik JM, Shiovitz S, Phipps AI. Molecular phenotypes of colorectal cancer and potential clinical applications. Gastroenterology report. 2015. 10.1093/gastro/gov046 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ali SM, Sanford EM, Klempner SJ, Rubinson DA, Wang K, Palma NA, et al. Prospective comprehensive genomic profiling of advanced gastric carcinoma cases reveals frequent clinically relevant genomic alterations and new routes for targeted therapies. The oncologist. 2015;20(5):499–507. 10.1634/theoncologist.2014-0378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Takahashi N, Yamada Y, Taniguchi H, Fukahori M, Sasaki Y, Shoji H, et al. Clinicopathological features and prognostic roles of KRAS, BRAF, PIK3CA and NRAS mutations in advanced gastric cancer. BMC research notes. 2014;7:271 10.1186/1756-0500-7-271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Luber B, Deplazes J, Keller G, Walch A, Rauser S, Eichmann M, et al. Biomarker analysis of cetuximab plus oxaliplatin/leucovorin/5-fluorouracil in first-line metastatic gastric and oesophago-gastric junction cancer: results from a phase II trial of the Arbeitsgemeinschaft Internistische Onkologie (AIO). BMC cancer. 2011;11:509 10.1186/1471-2407-11-509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Janmaat ML, Gallegos-Ruiz MI, Rodriguez JA, Meijer GA, Vervenne WL, Richel DJ, et al. Predictive factors for outcome in a phase II study of gefitinib in second-line treatment of advanced esophageal cancer patients. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2006;24(10):1612–9. 10.1200/JCO.2005.03.4900 . [DOI] [PubMed] [Google Scholar]
- 52.Dragovich T, McCoy S, Fenoglio-Preiser CM, Wang J, Benedetti JK, Baker AF, et al. Phase II trial of erlotinib in gastroesophageal junction and gastric adenocarcinomas: SWOG 0127. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2006;24(30):4922–7. 10.1200/JCO.2006.07.1316 . [DOI] [PubMed] [Google Scholar]
- 53.Okines AF, Ashley SE, Cunningham D, Oates J, Turner A, Webb J, et al. Epirubicin, oxaliplatin, and capecitabine with or without panitumumab for advanced esophagogastric cancer: dose-finding study for the prospective multicenter, randomized, phase II/III REAL-3 trial. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2010;28(25):3945–50. 10.1200/JCO.2010.29.2847 . [DOI] [PubMed] [Google Scholar]
- 54.Rao S, Starling N, Cunningham D, Sumpter K, Gilligan D, Ruhstaller T, et al. Matuzumab plus epirubicin, cisplatin and capecitabine (ECX) compared with epirubicin, cisplatin and capecitabine alone as first-line treatment in patients with advanced oesophago-gastric cancer: a randomised, multicentre open-label phase II study. Annals of oncology: official journal of the European Society for Medical Oncology / ESMO. 2010;21(11):2213–9. 10.1093/annonc/mdq247 . [DOI] [PubMed] [Google Scholar]
- 55.Jiang N, Wang D, Hu Z, Shin HJ, Qian G, Rahman MA, et al. Combination of anti-HER3 antibody MM-121/SAR256212 and cetuximab inhibits tumor growth in preclinical models of head and neck squamous cell carcinoma. Molecular cancer therapeutics. 2014;13(7):1826–36. 10.1158/1535-7163.MCT-13-1093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ferry DR, Anderson M, Beddard K, Tomlinson S, Atherfold P, Obszynska J, et al. A phase II study of gefitinib monotherapy in advanced esophageal adenocarcinoma: evidence of gene expression, cellular, and clinical response. Clinical cancer research: an official journal of the American Association for Cancer Research. 2007;13(19):5869–75. 10.1158/1078-0432.CCR-06-1970 . [DOI] [PubMed] [Google Scholar]
- 57.Dutton SJ, Ferry DR, Blazeby JM, Abbas H, Dahle-Smith A, Mansoor W, et al. Gefitinib for oesophageal cancer progressing after chemotherapy (COG): a phase 3, multicentre, double-blind, placebo-controlled randomised trial. The lancet oncology. 2014;15(8):894–904. 10.1016/S1470-2045(14)70024-5 . [DOI] [PubMed] [Google Scholar]
- 58.LoRusso P, Janne PA, Oliveira M, Rizvi N, Malburg L, Keedy V, et al. Phase I study of U3-1287, a fully human anti-HER3 monoclonal antibody, in patients with advanced solid tumors. Clinical cancer research: an official journal of the American Association for Cancer Research. 2013;19(11):3078–87. 10.1158/1078-0432.CCR-12-3051 . [DOI] [PubMed] [Google Scholar]
- 59.Garrett JT, Olivares MG, Rinehart C, Granja-Ingram ND, Sanchez V, Chakrabarty A, et al. Transcriptional and posttranslational up-regulation of HER3 (ErbB3) compensates for inhibition of the HER2 tyrosine kinase. Proceedings of the National Academy of Sciences of the United States of America. 2011;108(12):5021–6. 10.1073/pnas.1016140108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Seo AN, Kwak Y, Kim WH, Kim DW, Kang SB, Choe G, et al. HER3 protein expression in relation to HER2 positivity in patients with primary colorectal cancer: clinical relevance and prognostic value. Virchows Archiv: an international journal of pathology. 2015;466(6):645–54. 10.1007/s00428-015-1747-2 . [DOI] [PubMed] [Google Scholar]
- 61.Tao JJ, Castel P, Radosevic-Robin N, Elkabets M, Auricchio N, Aceto N, et al. Antagonism of EGFR and HER3 enhances the response to inhibitors of the PI3K-Akt pathway in triple-negative breast cancer. Science signaling. 2014;7(318):ra29 10.1126/scisignal.2005125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Petty R. http://conference.ncri.org.uk/epidermal-growth-factor-receptor-copy-number-gain-egfr-cng-and-response-to-gefitinib-in-oesophageal-cancer-oc-results-of-a-biomarker-analysis-of-a-phase-iii-trial-of-gefitinib-versus-placebo-tra/ [2015-10-13].
- 63.Kim JS, Kim MA, Kim TM, Lee SH, Kim DW, Im SA, et al. Biomarker analysis in stage III-IV (M0) gastric cancer patients who received curative surgery followed by adjuvant 5-fluorouracil and cisplatin chemotherapy: epidermal growth factor receptor (EGFR) associated with favourable survival. British journal of cancer. 2009;100(5):732–8. 10.1038/sj.bjc.6604936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Baiocchi G, Lopes A, Coudry RA, Rossi BM, Soares FA, Aguiar S, et al. ErbB family immunohistochemical expression in colorectal cancer patients with higher risk of recurrence after radical surgery. International journal of colorectal disease. 2009;24(9):1059–68. 10.1007/s00384-009-0702-6 . [DOI] [PubMed] [Google Scholar]
- 65.Quinn CM, Ostrowski JL, Lane SA, Loney DP, Teasdale J, Benson FA. c-erbB-3 protein expression in human breast cancer: comparison with other tumour variables and survival. Histopathology. 1994;25(3):247–52. . [DOI] [PubMed] [Google Scholar]
- 66.Jarde T, Kass L, Staples M, Lescesen H, Carne P, Oliva K, et al. ERBB3 Positively Correlates with Intestinal Stem Cell Markers but Marks a Distinct Non Proliferative Cell Population in Colorectal Cancer. PloS one. 2015;10(9):e0138336 10.1371/journal.pone.0138336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.He XX, Ding L, Lin Y, Shu M, Wen JM, Xue L. Protein expression of HER2, 3, 4 in gastric cancer: correlation with clinical features and survival. Journal of clinical pathology. 2015;68(5):374–80. 10.1136/jclinpath-2014-202657 . [DOI] [PubMed] [Google Scholar]
- 68.Vyberg M, Nielsen S. Proficiency testing in immunohistochemistry-experiences from Nordic Immunohistochemical Quality Control (NordiQC). Virchows Archiv: an international journal of pathology. 2015. 10.1007/s00428-015-1829-1 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Thiel A, Ristimaki A. Targeted therapy in gastric cancer. APMIS: acta pathologica, microbiologica, et immunologica Scandinavica. 2015;123(5):365–72. 10.1111/apm.12359 . [DOI] [PubMed] [Google Scholar]
- 70.Bhargava R, Chen B, Klimstra DS, Saltz LB, Hedvat C, Tang LH, et al. Comparison of two antibodies for immunohistochemical evaluation of epidermal growth factor receptor expression in colorectal carcinomas, adenomas, and normal mucosa. Cancer. 2006;106(8):1857–62. 10.1002/cncr.21782 . [DOI] [PubMed] [Google Scholar]
- 71.Anagnostou VK, Welsh AW, Giltnane JM, Siddiqui S, Liceaga C, Gustavson M, et al. Analytic variability in immunohistochemistry biomarker studies. Cancer epidemiology, biomarkers & prevention: a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2010;19(4):982–91. 10.1158/1055-9965.EPI-10-0097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hechtman JF, Polydorides AD. HER2/neu gene amplification and protein overexpression in gastric and gastroesophageal junction adenocarcinoma: a review of histopathology, diagnostic testing, and clinical implications. Archives of pathology & laboratory medicine. 2012;136(6):691–7. 10.5858/arpa.2011-0168-RS . [DOI] [PubMed] [Google Scholar]
- 73.Ruschoff J, Dietel M, Baretton G, Arbogast S, Walch A, Monges G, et al. HER2 diagnostics in gastric cancer-guideline validation and development of standardized immunohistochemical testing. Virchows Arch. 2010;457(3):299–307. Epub 2010/07/29. 10.1007/s00428-010-0952-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Torhorst J, Bucher C, Kononen J, Haas P, Zuber M, Kochli OR, et al. Tissue microarrays for rapid linking of molecular changes to clinical endpoints. Am J Pathol. 2001;159(6):2249–56. Epub 2001/12/06. 10.1016/S0002-9440(10)63075-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
R0 = Radical resection according to pathology report, R1 = non-radical resection, Rx = resection margin uncertain. N1 = metastasis in 1–2 regional lymph nodes, N2 = metastasis in 3–6 regional lymph nodes, N3 = metastasis in 7 or more regional lymph nodes.
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.