Abstract
In a phase 3 trial of denosumab vs zoledronic acid in patients (n=1776) with bone metastases and solid tumors or multiple myeloma, denosumab was superior to zoledronic acid for the primary end point of prevention of skeletal-related events. There was no difference in overall survival between the two groups; however, an ad hoc overall survival analysis in the multiple myeloma subset of patients (n=180) favored zoledronic acid (hazard ratio (HR) 2.26; 95% confidence interval (CI) 1.13–4.50; P=0.014). In the present analysis, we found imbalances between the groups with respect to baseline risk characteristics. HRs with two-sided 95% CIs were estimated using the Cox model. After adjustment in a covariate analysis, the CI crossed unity (HR 1.86; 95% CI 0.90–3.84; P=0.0954). Furthermore, we found a higher rate of early withdrawals for the reasons of lost to follow-up and withdrawal of consent in the zoledronic acid group; after accounting for these, the HR was 1.31 (95% CI 0.80–2.15; P=0.278). In conclusion, the survival results in multiple myeloma patients in this trial were confounded and will eventually be resolved by an ongoing phase 3 trial.
Introduction
Patients with advanced cancer and bone metastases frequently experience skeletal-related events (SREs), defined as spinal cord compression, pathologic fracture and surgery or radiation to bone (hypercalcemia may also be included as a SRE, though this was not the case in the present work).1 Bone-targeted agents including bisphosphonates and the RANKL (receptor activator of nuclear factor-κB ligand) inhibitor, denosumab, are used to prevent SREs in patients with bone metastases. In three phase 3 trials conducted in patients with bone metastases, denosumab was superior to zoledronic acid for the primary end point of time to first on-study SRE in patients with prostate cancer (n=1904)2 and breast cancer (n=2046),3 and noninferior in patients with solid tumors (other than prostate or breast) or multiple myeloma (n=1776; hazard ratio (HR) 0.84; 95% confidence interval (CI) 0.71–0.98; P=0.0007).4
No differences in overall survival between treatment groups were observed in any of the phase 3 studies,2, 3, 4 or in a prespecified integrated analysis;5 however, in an ad hoc subset analysis, overall survival favored denosumab (HR 0.80; 95% CI 0.67–0.95; P=0.01) in patients with lung cancer (n=811)6 and favored zoledronic acid in patients with multiple myeloma (n=180; HR 2.26; 95% CI 1.13–4.50; P=0.014).4 An evaluation of the lung cancer data has been reported separately.6
Multiple myeloma patients were included in this trial based on preclinical evidence for a role for RANKL inhibition in decreasing osteolytic bone lesions and tumor burden in murine myeloma models.7, 8 As myeloma patients represented only 10% of the total sample and the primary end point was prevention of SREs rather than survival or tumor response, the study design did not include stratification for myeloma-specific prognostic factors. The aim of the present analysis was to evaluate potential differences between the denosumab and zoledronic acid treatment groups that might have contributed to the overall survival results in the myeloma subset of this phase 3 trial.
Materials and methods
In this international, double-blind, randomized, phase 3 trial (NCT00330759; the ‘244 study'), patients were randomized 1:1 to receive 120 mg subcutaneous denosumab or 4 mg (dose adjusted for renal function) intravenous zoledronic acid every 4 weeks. Eligible patients were adults with biopsy-confirmed advanced solid tumors or multiple myeloma with current or prior radiographic evidence of at least one bone metastasis (or lytic bone lesion from myeloma), and an Eastern Cooperative Oncology Group (ECOG) performance status of 0, 1 or 2. Randomization was stratified by tumor type (non-small-cell lung cancer, limited to 60% of total; multiple myeloma, limited to 10% of total; or other), systemic therapy (chemotherapy, biologic therapy or other (yes or no)) and previous SRE (yes or no). Patients were followed for survival for 2 years after the last dose of investigational product.
The present post hoc analysis includes all patients in the myeloma subset (n=180). Descriptive analyses were performed for baseline/on-study variables and adverse events. Kaplan–Meier estimates for overall survival were presented graphically and HRs with two-sided 95% CIs were estimated using the Cox proportional hazards model. To account for differences between the groups for early withdrawals because of ‘consent withdrawn' and ‘lost to follow-up,' an additional post hoc analysis was done in which these withdrawals were treated as events. A P-value was calculated using Fisher's exact test for the difference between groups for osteonecrosis of the jaw.
Results
Of the 1776 randomized patients, 180 (10%) had multiple myeloma (93 zoledronic acid; 87 denosumab). In the myeloma subset, denosumab was similar to zoledronic acid for the primary end point of time to first on-study SRE (HR 1.03; 95% CI 0.68–1.57; P=0.9), comparable to the results in the overall trial population. Denosumab was also similar to zoledronic acid for the time to first and subsequent SREs (HR 1.21; 95% CI 0.86–1.71; P=0.3). Mean (s.d.) follow-up time was 18.4 (8.0) months for zoledronic acid and 17.0 (7.8) months for denosumab.
We evaluated differences in baseline/on-study variables in the study arms that may have contributed to the difference in survival. As shown in Table 1, more patients who received zoledronic acid had ECOG score 0 (32% vs 24% for denosumab) and International Staging System (ISS) stage I disease (14% vs 10%), although these differences were not statistically significant. On the other hand, poor renal function in the lowest creatinine clearance group of 30–40 ml/min was more common in denosumab patients at baseline (10% vs 2% for zoledronic acid). The difference between the groups for the distribution of creatinine clearance categories was highly significant (P<0.001). Indeed, there were six more deaths in the denosumab group (7/9 patients) compared with the zoledronic group (1/2 patients) in patients with creatinine clearance ⩾30 to <40 ml/min. Although there were more zoledronic acid patients in the ⩾40 to ⩽60 ml/min creatinine clearance categories, the difference in deaths was minimal (0/2 for denosumab vs 2/23 for zoledronic acid). The difference in poor renal function accounts for some, but not all, of the difference in deaths between the groups, as seven more patients with normal renal function (>60 ml/min) also died in the denosumab group (16/76 vs 9/64 for zoledronic acid). In addition, stem cell transplantation had been given more frequently in the zoledronic acid group (25% vs 17% for denosumab) and novel myeloma therapies such as proteasome inhibitors and immunomodulatory drugs (one or more of bortezomib, thalidomide and lenalidomide) were used more frequently in the zoledronic acid group (96% vs 88% for denosumab). These latter differences were not individually statistically significant; however, after adjusting for ECOG performance status, renal function at baseline, stem cell transplant before study and on study and use of novel antineoplastic treatments in the Cox model, the HR was reduced and the CI crossed unity (HR 1.86; 95% CI 0.90–3.84; P=0.0954).
Table 1. Baseline/on-study characteristics in the multiple myeloma subset of the phase 3 study.
| Characteristic, n (%) | Zoledronic acid (n=93) | Denosumab (n=87) |
|---|---|---|
| Sex | ||
| Male | 54 (58%) | 57 (66%) |
| Age, years | ||
| Mean (s.d.) | 63 (11) | 62 (10) |
| ECOG performance status at study entry | ||
| 0 | 30 (32%) | 21 (24%) |
| 1 | 44 (47%) | 50 (58%) |
| 2 | 18 (19%) | 15 (17%) |
| Creatinine clearance at baseline | ||
| ⩾30 ml/min to <40 ml/min | 2 (2%) | 9 (10%) |
| ⩾40 ml/min to ⩽60 ml/min | 23 (25%) | 2 (2%) |
| >60 ml/min | 64 (69%) | 76 (87%) |
| Missing | 4 (4%) | 0 (0%) |
| Primary ISS stage at diagnosis–multiple myeloma | ||
| I | 13 (14%) | 9 (10%) |
| II | 23 (25%) | 28 (32%) |
| III | 56 (60%) | 49 (56%) |
| Autologous stem cell transplant (before or on study), n | 93 23 (25%) | 86 15 (17%) |
| Anti-myeloma treatments on study,a n | 92 | 86 |
| Melphalan | 48 (52%) | 34 (40%) |
| Thalidomide | 44 (48%) | 32 (37%) |
| Bortezomib | 25 (27%) | 28 (33%) |
| Cyclophosphamide | 19 (21%) | 25 (29%) |
| Lenalidomide | 19 (21%) | 16 (19%) |
Abbreviations: ECOG, Eastern Cooperative Oncology Group; ISS, International Staging System.
Further details on combination regimens were not collected.
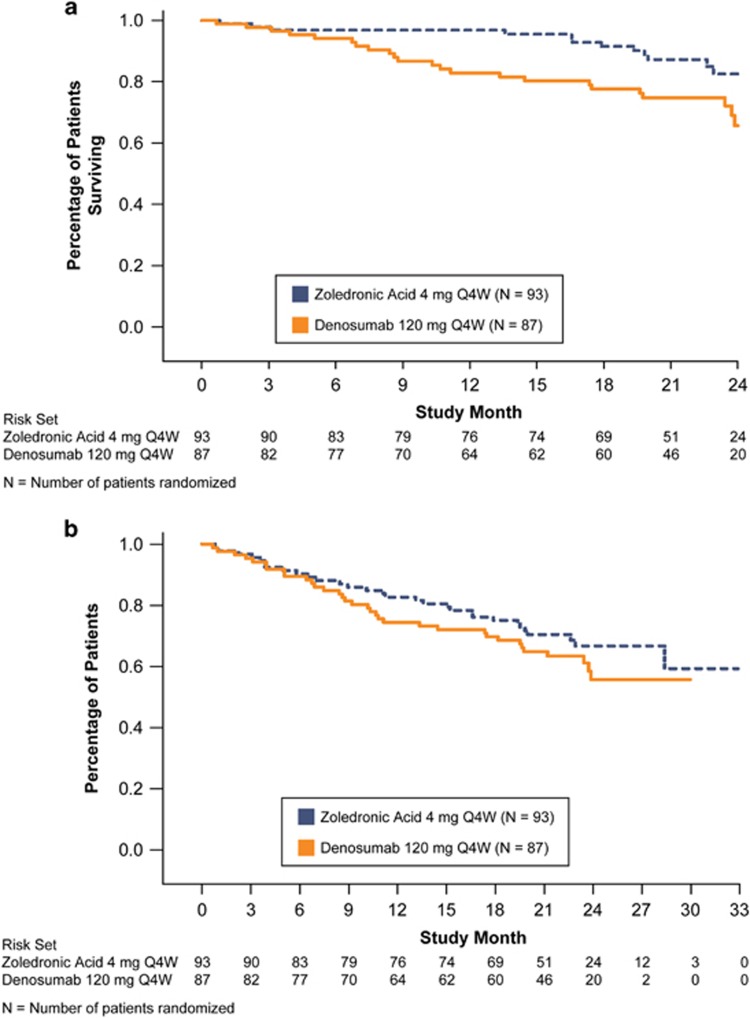
The patient incidence of death as of the primary analysis cutoff date for the multiple myeloma subset was 8 (9%) for zoledronic acid and 19 (22%) for denosumab (P=0.02; Table 2). The overall survival curve for the multiple myeloma patients in this study is shown in Figure 1a. We observed that between months 3 and 15, there were no deaths in the zoledronic acid group (note the plateau in the survival curve) and during this period the withdrawals from study because of consent withdrawn or lost to follow-up were higher in the zoledronic acid group (14% (13 patients zoledronic acid) and 7% (6 patients denosumab)), although the difference was not statistically significant. As there was no survival follow-up for patients who withdrew for these reasons, they have the potential to confound the survival results, particularly as the overall number of deaths was very small.
Table 2. Patient disposition.
| Characteristic, n (%) | Zoledronic acid (n=93) | Denosumab (n=87) |
|---|---|---|
| Withdrew before primary data cutoff | 45 (48%) | 48 (55%) |
| Death | 8 (9%) | 19 (22%) |
| Consent withdrawn | 16 (17%) | 11 (13%) |
| Other | 3 (3%) | 6 (7%) |
| Disease progression | 1 (1%) | 6 (7%) |
| Subject request | 6 (7%) | 3 (3%) |
| Adverse event | 7 (8%) | 2 (3%) |
| Protocol deviation | 0 (0%) | 1 (1%) |
| Noncompliance | 2 (2%) | 0 (0%) |
| Ineligibility determined | 1 (1%) | 0 (0%) |
| Lost to follow-up | 1 (1%) | 0 (0%) |
Figure 1.
(a) Overall survival analysis, multiple myeloma subset. (b) Time to death, consent withdrawn or lost to follow-up. Q4W, every 4 weeks.
We therefore performed a clinical review on these patients. This clinical review of patients who had withdrawn consent between months 3 and 15 (no patient was lost to follow-up during this time) suggested that these patients, particularly those in the zoledronic acid group, had a poorer prognosis at baseline and worsening disease at the time of discontinuation. Specifically, 10 of 13 patients in the zoledronic acid group and 5 of 6 patients in the denosumab group who withdrew consent had not been newly diagnosed at the time of study entry; 6 patients in the zoledronic acid group and 2 patients in the denosumab group were >65 years of age at baseline; 3 patients, all in the zoledronic acid group, met the definition of hypercalcemia (serum albumin-adjusted calcium ⩾2.6 mmol) at baseline; 4 patients, also all in the zoledronic acid group, had poor performance status (an ECOG score of 2) at baseline. In addition, 8 patients in the zoledronic acid group and 3 patients in the denosumab group had low albumin (<3.5 g/dl); 7 zoledronic acid patients and 3 denosumab patients had elevated bone turnover (urinary N-telopeptide >100 nM); and 9 zoledronic acid patients and 3 denosumab patients had prior SREs. All of the above factors suggest that many of the patients who withdrew consent or were lost to follow-up had poor prognostic values and aggressive features of myeloma disease at baseline that may have contributed to early withdrawal from the study. In addition, we note that laboratory assessments in these patients showed signs of disease progression in both treatment groups as evidenced by a worsening of renal function.
To evaluate the impact of these patients, we conducted an analysis in which events of death, consent withdrawal or loss to follow-up were treated as events (Figure 1b). The resulting HR was reduced and the 95% CI crossed unity: HR 1.31 (95% CI 0.80–2.15); P=0.278. Furthermore, we noted that in this analysis, the plateau in the zoledronic acid curve was no longer present and the two curves look more similar.
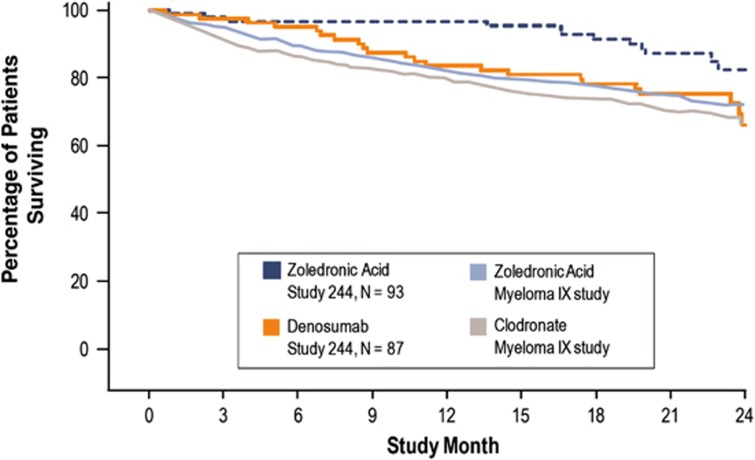
We compared the survival curves from the 244 study with those previously reported for zoledronic acid vs clodronate in the Myeloma IX study, a large randomized, controlled, population-based, phase 3 British Medical Research Council trial.9 With the caveat that cross-study comparisons should be approached with caution, we found that the survival rate of the 244 zoledronic acid arm was higher than the corresponding zoledronic acid arm in Myeloma IX, whereas the 244 denosumab arm was comparable to the Myeloma IX zoledronic acid arm (Figure 2).
Figure 2.
Overall survival rate: Myeloma IX study vs study 244 multiple myeloma subgroup.
In the 244 study, the incidence of adverse events was 99% for zoledronic acid and 98% for denosumab, and of serious adverse events was 51% and 58%, respectively. Hypocalcemia, a known adverse event for bone-targeted agents, was reported in 10 (11%) zoledronic acid patients and 12 (14%) denosumab patients. Osteonecrosis of the jaw occurred in 2 (2%) zoledronic acid patients and 4 (5%) denosumab patients (P=0.43). Cumulative mean (s.d.) drug exposure, defined as the time from the first dose to the last dose plus 28 days, was 16.9 (8.0) months for zoledronic acid and 16.6 (7.8) months for denosumab.
Discussion
In this post hoc analysis of a phase 3 trial of denosumab vs zoledronic acid for the delay or prevention of SREs in patients with bone metastases, we examined possible reasons for the favorable survival in the subset of patients with multiple myeloma in the zoledronic acid group. As multiple myeloma patients represented only 10% of the sample and this trial was designed to examine the end point of SREs, and not survival, the study design had not included randomization stratification for myeloma-specific prognostic factors. We found imbalances between the study arms including a higher proportion of patients in the zoledronic acid arm with positive prognostic characteristics such as ECOG score 0 and ISS stage 1, whereas the denosumab arm contained a higher proportion of patients with poor renal function, a well-established negative prognostic factor.10 Furthermore, effective myeloma treatments including transplantation and novel myeloma therapies such as proteasome inhibitors and immunomodulatory drugs were more commonly used in the zoledronic acid group. As use of these drugs has been shown to double overall survival in multiple myeloma,11 imbalances between the study arms could have affected the survival results. These individual differences were not statistically significant (except for the distribution of creatinine clearance categories) likely because of small sample size; however, a covariate analysis adjusting for these factors together substantially reduced the HR for overall survival, with a 95% CI that crossed unity. Although there is a clear effect of this type of covariate adjustment, it is limited by the number of covariates available for inclusion. Moreover, key factors such as M-protein and immunofixation at baseline, β2 microglobulin, type of immunoglobulin, light chain, cytogenetics and chromosome karyotype and plasma cell index were not collected in this study and therefore could not be accounted for in this analysis.
Furthermore, we observed a complete absence of deaths in the zoledronic acid group for a 12-month period between months 3 and 15, a finding that was anomalous compared with survival curves produced in prior studies. Upon further examination, we discovered that 13 patients in the zoledronic acid group withdrew consent to continue on study during this period, and as such, no further survival data could be generated for these patients. In addition, a large number of these patients had high-risk characteristics and worsening disease, indicating that death may have ensued after withdrawal. In the context of a small difference between the groups in the absolute number of deaths (n=16) among multiple myeloma patients overall, it is clear that a few patients without follow-up data have the potential to affect the survival results. When these types of withdrawals were counted as events in the survival analysis, an analysis that was requested by regulatory authorities, there was no statistically significant difference between the groups and the plateau observed in the zoledronic acid arm was eliminated. These observations may also explain why the survival rate of the 244 zoledronic acid arm was higher than that in the Myeloma IX study,9 whereas survival in the 244 denosumab arm was comparable to the survival reported with zoledronic acid in Myeloma IX. The survival rate in the 244 denosumab arm was furthermore consistent with that seen in prior clinical trials and epidemiological studies,12, 13, 14, 15, 16, 17, 18, 19, 20 whereas the rate observed in the 244 zoledronic acid arm was comparatively greater than that reported in these historical studies. We acknowledge that cross-study comparisons should be made with caution; however, the predominance of evidence suggests that the survival of the zoledronic acid group in this study was anomalous.
In conclusion, in this phase 3 study of denosumab vs zoledronic acid, imbalances in the baseline and on-study variables and unequal early withdrawal censoring confounded the interpretation of survival in the multiple myeloma subset. An adequately sized confirmatory phase 3 trial of denosumab and zoledronic acid in multiple myeloma patients including randomization stratification by prognostic and disease variables is currently underway (NCT01345019) and will definitively resolve this issue. Until these data are available, the present report underlines the weaknesses of ad hoc subset analyses in clinical trials.
Acknowledgments
This study was sponsored and supported by Amgen Inc. Wanda J Krall, whose work was funded by Amgen Inc., and Geoff Smith of Amgen Inc., assisted in the writing of this manuscript. Amgen was involved in the design of the study, the analysis of data and the decision to publish.
Footnotes
N Raje has received honoraria from Celgene, Millennium and Onyx for advisory boards and research funding from Eli Lilly, Actelion and Amgen. W Willenbacher has received honoraria from Amgen for educational lectures, data acquisition in noninterventional studies and participation in advisory boards, as well as research grants and is a member of the steering committee of the AMGEN 20090482 trial. S Vadhan-Raj has received honoraria from Amgen for participation in the advisory board, and research funding for clinical trials. E Terpos has received honoraria from Amgen for participation in advisory boards and also research grants; he is a member of the steering committee of the Amgen 20090482 trial. GD Roodman has received consultancy fees from Amgen. T Facon has received advisory board fees from Amgen and Novartis. A Balakumaran and A Feng are employees of Amgen and hold Amgen stock. A Braun was an employee of Amgen when the work was conducted. AK Stewart, V Hungria, A Spencer and Y Alexeeva declare no conflict of interest.
References
- 1Coleman RE. Clinical features of metastatic bone disease and risk of skeletal morbidity. Clin Cancer Res 2006; 12: 6243s–6249s. [DOI] [PubMed] [Google Scholar]
- 2Fizazi K, Carducci M, Smith M, Damião R, Brown J, Karsh L et al. Denosumab versus zoledronic acid for treatment of bone metastases in men with castration-resistant prostate cancer: a randomised, double-blind study. Lancet 2011; 377: 813–822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3Stopeck AT, Lipton A, Body JJ, Steger GG, Tonkin K, de Boer RH et al. Denosumab compared with zoledronic acid for the treatment of bone metastases in patients with advanced breast cancer: a randomized, double-blind study. J Clin Oncol 2010; 28: 5132–5139. [DOI] [PubMed] [Google Scholar]
- 4Henry DH, Costa L, Goldwasser F, Hirsh V, Hungria V, Prausova J et al. Randomized, double-blind study of denosumab versus zoledronic acid in the treatment of bone metastases in patients with advanced cancer (excluding breast and prostate cancer) or multiple myeloma. J Clin Oncol 2011; 29: 1125–1132. [DOI] [PubMed] [Google Scholar]
- 5Lipton A, Fizazi K, Stopeck AT, Henry DH, Brown JE, Yardley DA et al. Superiority of denosumab to zoledronic acid for prevention of skeletal-related events: a combined analysis of 3 pivotal, randomised, phase 3 trials. Eur J Cancer 2012; 48: 3082–3092. [DOI] [PubMed] [Google Scholar]
- 6Scagliotti GV, Hirsh V, Siena S, Henry DH, Woll PJ, Manegold C et al. Overall survival improvement in patients with lung cancer and bone metastases treated with denosumab versus zoledronic acid: subgroup analysis from a randomized phase 3 study. J Thorac Oncol 2012; 7: 1823–1829. [DOI] [PubMed] [Google Scholar]
- 7Croucher PI, Shipman CM, Lippitt J, Perry M, Asosingh K, Hijzen A et al. Osteoprotegerin inhibits the development of osteolytic bone disease in multiple myeloma. Blood 2001; 98: 3534–3540. [DOI] [PubMed] [Google Scholar]
- 8Vanderkerken K, De Leenheer E, Shipman C, Asosingh K, Willems A, Van Camp B et al. Recombinant osteoprotegerin decreases tumor burden and increases survival in a murine model of multiple myeloma. Cancer Res 2003; 63: 287–289. [PubMed] [Google Scholar]
- 9Morgan GJ, Davies FE, Gregory WM, Cocks K, Bell SE, Szubert AJ et al. First-line treatment with zoledronic acid as compared with clodronic acid in multiple myeloma (MRC Myeloma IX): a randomised controlled trial. Lancet 2010; 376: 1989–1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10Kumar SK, Rajkumar SV, Dispenzieri A, Lacy MQ, Hayman SR, Buadi FK et al. Improved survival in multiple myeloma and the impact of novel therapies. Blood 2008; 111: 2516–2520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11Kumar SK, Dispenzieri A, Gertz MA, Lacy MQ, Lust JA, Hayman SR et al. Continued improvement in survival in multiple myeloma and the impact of novel agents. ASH Annual Meeting Abstracts 2012; 120: (abstract 3972). [Google Scholar]
- 12San Miguel JF, Schlag R, Khuageva NK, Dimopoulos MA, Shpilberg O, Kropff M et al. Bortezomib plus melphalan and prednisone for initial treatment of multiple myeloma. N Engl J Med 2008; 359: 906–917. [DOI] [PubMed] [Google Scholar]
- 13Rajkumar SV, Rosinol L, Hussein M, Catalano J, Jedrzejczak W, Lucy L et al. Multicenter, randomized, double-blind, placebo-controlled study of thalidomide plus dexamethasone compared with dexamethasone as initial therapy for newly diagnosed multiple myeloma. J Clin Oncol 2008; 26: 2171–2177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14Rajkumar SV, Jacobus S, Callander NS, Fonseca R, Vesole DH, Williams ME et al. Lenalidomide plus high-dose dexamethasone versus lenalidomide plus low-dose dexamethasone as initial therapy for newly diagnosed multiple myeloma: an open-label randomised controlled trial. Lancet Oncol 2010; 11: 29–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15Facon T, Darre S. Frontline treatment in multiple myeloma patients not eligible for stem-cell transplantation. Best Pract Res Clin Haematol 2007; 20: 737–746. [DOI] [PubMed] [Google Scholar]
- 16Palumbo A, Bringhen S, Caravita T, Merla E, Capparella V, Callea V et al. Oral melphalan and prednisone chemotherapy plus thalidomide compared with melphalan and prednisone alone in elderly patients with multiple myeloma: randomised controlled trial. Lancet 2006; 367: 825–831. [DOI] [PubMed] [Google Scholar]
- 17Barlogie B, Kyle RA, Anderson KC, Greipp PR, Lazarus HM, Hurd DD et al. Standard chemotherapy compared with high-dose chemoradiotherapy for multiple myeloma: final results of phase III US Intergroup Trial S9321. J Clin Oncol 2006; 24: 929–936. [DOI] [PubMed] [Google Scholar]
- 18Child JA, Morgan GJ, Davies FE, Owen RG, Bell SE, Hawkins K et al. High-dose chemotherapy with hematopoietic stem-cell rescue for multiple myeloma. N Engl J Med 2003; 348: 1875–1883. [DOI] [PubMed] [Google Scholar]
- 19Attal M, Harousseau JL, Stoppa AM, Sotto JJ, Fuzibet JG, Rossi JF et al. A prospective, randomized trial of autologous bone marrow transplantation and chemotherapy in multiple myeloma. Intergroupe Francais du Myelome. N Engl J Med 1996; 335: 91–97. [DOI] [PubMed] [Google Scholar]
- 20Attal M, Harousseau JL, Facon T, Guilhot F, Doyen C, Fuzibet JG et al. Single versus double autologous stem-cell transplantation for multiple myeloma. N Engl J Med 2003; 349: 2495–2502. [DOI] [PubMed] [Google Scholar]