Abstract
Background:
Eosinophilic granuloma (EG) of bone refers to a generally benign form of Langerhans cell histiocytosis localized to the bone. Patients may present with a solitary lesion (monostotic) or multiple sites of involvement (polyostotic).
Materials and Methods:
This study was done to evaluate the clinicopathological pattern of 6 cases of EGs of the skull diagnosed at a tertiary care hospital. All patients of EG were included with the help of medical records over a 5-year period that is, November 2009 to November 2014. They all had been preoperatively evaluated by skull X-ray and computed tomography. To rule out a multifocal disease scintigraphy was performed in all cases preoperatively. Surgical excision was performed, and EG was diagnosed on histopathology and immunohistochemistry.
Results:
There was a male predominance. Parietal bone was the most common affected bone. Total excision of the lesion was performed in all cases. No patient received postoperative radiotherapy. The follow-up period ranged from 6 months to 3 years. No tumor recurrence was noted.
Conclusion:
With an unknown etiology, nonspecific clinical and radiological findings with diagnosis possible only on histopathological examination, EG needs to be considered in the differential diagnosis as a skull mass, especially in children.
Keywords: Eosinophilic granuloma, histiocytosis, skull
INTRODUCTION
Eosinophilic granuloma (EG) is a benign disorder that affects children and young adults particularly males. It is one of the three clinical variants of Langerhans cell histiocytosis (LCH). The other two variants are Letterer–Siwe disease and Hand–Schuller–Christian disease. The term “Eosinophilic Granuloma“ was first introduced by Lichtenstein and Jaffe in 1940.[1] It affects male children in more than 90% of the cases with preferential involvement of the skeletal system. The sites of involvement are the skull, mandible, spine, ribs, and long bones in order of decreasing frequency.[2] EG can be asymptomatic or present as local swelling, pain or tenderness. If at the skull, then a hematoma after a mild injury is a common finding.[3]
Radiographically, the lesion consists of a punched out, well-defined lytic lesion most commonly seen in the parietal or frontal bone.[4] EG is characterized morphologically by the proliferation of mononuclear and multinucleated Langerhans cells with characteristic grooves and folds. On Immunohistochemical evaluation, these cells stain positively for CD1a and S-100.[5]
MATERIALS AND METHODS
This study was conducted in the Department of Pathology, Government Medical College, Srinagar. It was a retrospective study done over a period of 5 years November 2009 to November 2014. All cases were retrieved with the help of medical records. Preliminary data such as age, sex, clinical and radiologic findings, treatment, and follow-up, were recorded from each patient. They all had been preoperatively evaluated by skull X-ray and computed tomography (CT). To rule out a multifocal disease, scintigraphy was performed in all cases preoperatively. Surgical excision of the lesions was performed. No patient received postoperative radiotherapy or chemotherapy. Slides were reviewed by two pathologists, and EG was diagnosed on histopathology and immunohistochemistry.
RESULTS
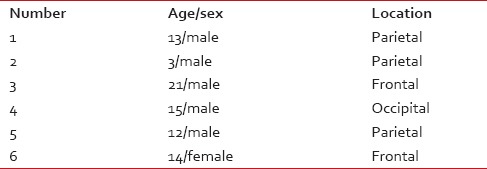
Our series consisted of 6 cases (5 males and 1 female; mean age 13 years; range 3-21 years). The patients age, sex, and tumor location are summarized in Table 1. Four patients had a painless skull mass as the chief complaint, whereas 2 patients experienced pain. Parietal bone was the most frequently (3/6) affected site followed by frontal (2/6 cases) and occipital bone (1/6 cases). The radiographic appearance of EG was that of a lytic punched out a lesion in the bone. All hematological parameters were normal in these patients. Wide excision of the lesion was performed in all cases. No patient received postoperative radiotherapy or chemotherapy. In all cases, the histopathology showed EG characterized by Langerhans histiocytes and multinucleated reactive histiocytic giant cells against a background of polymorphous inflammatory infiltrate rich in eosinophils. This was followed by immunohistochemistry which showed strong membrane positivity for CD1a. The follow-up ranged from 6 months to 4 years, and no recurrence was documented.
Table 1.
Distribution of cases according to age, sex and site of lesion
DISCUSSION
Eosinopilic granuloma is part of a spectrum of LCH usually presenting as a monostotic lesion affecting flat and long bones it is the most common form of LCH, accounting for 70% of all cases. EG most commonly presents as a solitary lesion in the skull, whereas femur, mandible, ribs, pelvis, and spine are other common locations.[2] The most common symptom of the EG is that of a gradually enlarging tender skull mass. Solitary lesions may also be asymptomatic and incidentally discovered on a skull X-ray. However, acute presentation of a solitary EG with an epidural hematoma has been described.[3]
Laboratory tests in EG may reveal elevated erythrocyte sedimentation rate and mild peripheral eosinophilia.[6] However, none of our patients exhibited eosinophilia. In our cases, on X-ray the lesions appeared as round or oval punched out radiolucent lesion [Figure 1]. On CT, a soft tissue mass with a lytic lesion, having a central density could be demonstrated [Figure 2]. However, the recommendation is that a diagnosis of EG must be confirmed by a biopsy of the tumor because clinical and radiological features are nonspecific.[7] The characteristic finding on histology is the Langerhans cell with abundant, often vacuolated cytoplasm and vesicular nuclei containing linear grooves or folds.[8] As seen in our cases, there is an admixed polymorphous population of numerous eosinophils, neutrophils, lymphocytes, plasma cells, multinucleated giant cells, and macrophages [Figure 3]. The tissue stains positively for S-100 protein and CD1a. All cases in our study showed intense membrane positivity for CD1a [Figure 4]. CD1a is a well-recognized marker that immunoreacts with Langerhans cells.[9,10] The presence of Birbeck granules on electron microscopy is characteristic of EG. Electron microscopy was not performed in our cases as was not considered essential for diagnosis in previous studies.[11]
Figure 1.

Lateral radiograph of skull showing a punched out lesion in the parietal bone
Figure 2.
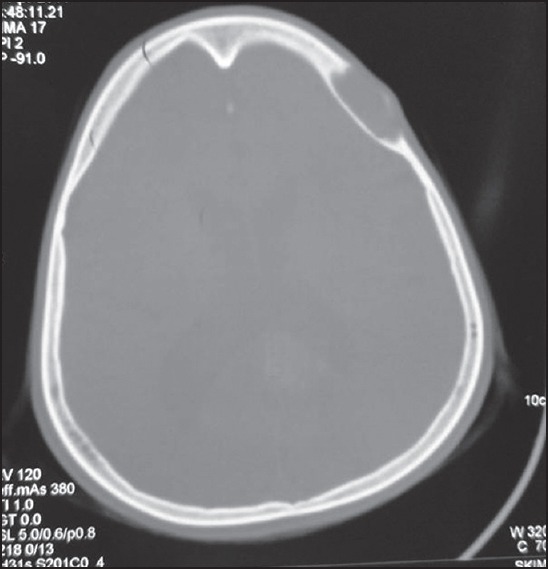
Computed tomography scan of the patient demonstrating an osteolytic lesion with beveled bone edges in the parietal bone
Figure 3.
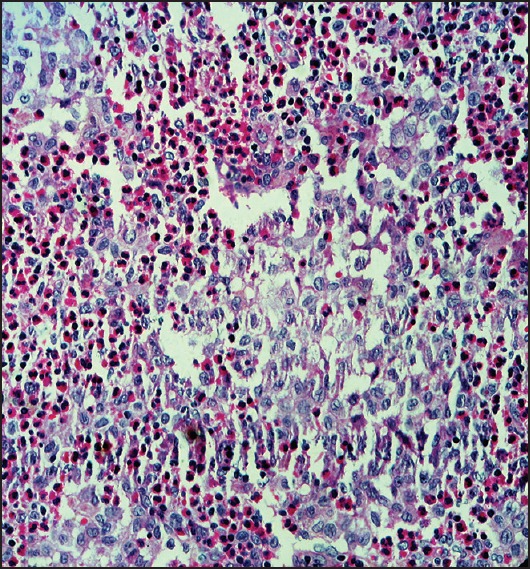
Photomicrograph showing characteristic Langerhans cells with characteristic grooves against a background of polymorphic inflammatory infiltrate rich in eosinophils (H and E, ×40)
Figure 4.
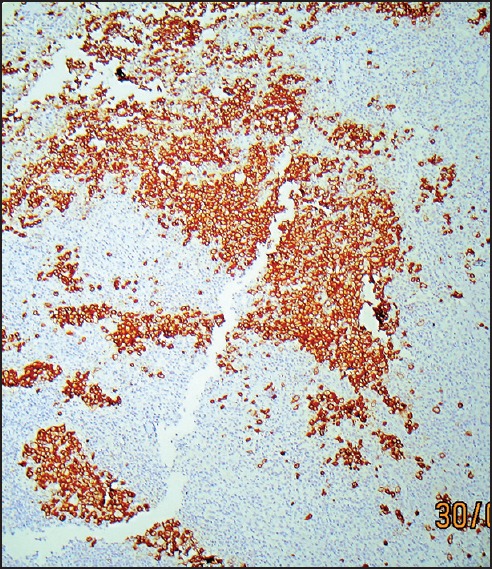
Langerhans cells showing intense membrane positivity for CD1a
The differential diagnosis includes osteomyelitis, epidermoid cyst, Ewing's sarcoma, osteosarcoma, multiple myeloma, and metastasis.[12]
The prognosis of skull EG is usually excellent. Furthermore, there are also reports of spontaneous resolution by fibrosis occurring within 1-2 years.[13,14] Nevertheless there is no generally accepted prognostic factor, and no completely satisfactory clinical classification yet established.[15]
We conclude that with an unknown etiology, nonspecific clinical and radiological findings with diagnosis possible only on histopathological examination, EG needs to be considered in the differential diagnosis as a skull mass, especially in children. Although no recurrence was noted in our patients, a close follow-up for the development of additional lesions is required.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Lichtenstein L, Jeffe HL. Eosinophilic granuloma of bone: With report of a case. Am J Pathol. 1940;16:595–6043. [PMC free article] [PubMed] [Google Scholar]
- 2.Park SH, Park J, Hwang JH, Hwang SK, Hamm IS, Park YM. Eosinophilic granuloma of the skull: A retrospective analysis. Pediatr Neurosurg. 2007;43:97–101. doi: 10.1159/000098380. [DOI] [PubMed] [Google Scholar]
- 3.Martínez-Lage JF, Bermúdez M, Martínez-Barba E, Fuster JL, Poza M. Epidural hematoma from a cranial eosinophilic granuloma. Childs Nerv Syst. 2002;18:74–6. doi: 10.1007/s003810100491. [DOI] [PubMed] [Google Scholar]
- 4.Golla SK, Kavanagh EC. MRI, CT, scintigraphic and histological features of a vanishing scapular eosinophilic granuloma. Ir J Med Sci. 2009;178:107–10. doi: 10.1007/s11845-008-0133-3. [DOI] [PubMed] [Google Scholar]
- 5.Redhu R, Nadkarni T, Mahesh R. Diabetes insipidus associated with a thickened pituitary stalk in a case of Langerhans cell histiocytosis. J Pediatr Neurosci. 2011;6:62–4. doi: 10.4103/1817-1745.84412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang J, Wu X, Xi ZJ. Langerhans cell histiocytosis of bone in children: A clinicopathologic study of 108 cases. World J Pediatr. 2010;6:255–9. doi: 10.1007/s12519-010-0205-0. [DOI] [PubMed] [Google Scholar]
- 7.Kilborn TN, Teh J, Goodman TR. Paediatric manifestations of Langerhans cell histiocytosis: A review of the clinical and radiological findings. Clin Radiol. 2003;58:269–78. doi: 10.1016/s0009-9260(02)00537-8. [DOI] [PubMed] [Google Scholar]
- 8.Herwig MC, Wojno T, Zhang Q, Grossniklaus HE. Langerhans cell histiocytosis of the orbit: Five clinicopathologic cases and review of the literature. Surv Ophthalmol. 2013;58:330–40. doi: 10.1016/j.survophthal.2012.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baltacioglu E, Senel FC, Ozen B, Ofluoglu AD, Ersöz S, Kebudi R, et al. Clinical, pathological and radiological evaluation of disseminated Langerhans’ cell histiocytosis in a 30-month-old boy. Dentomaxillofac Radiol. 2007;36:526–9. doi: 10.1259/dmfr/71449570. [DOI] [PubMed] [Google Scholar]
- 10.Gabbay LB, Leite Cda C, Andriola RS, Pinho Pda C, Lucato LT. Histiocytosis: A review focusing on neuroimaging findings. Arq Neuropsiquiatr. 2014;72:548–58. doi: 10.1590/0004-282x20140063. [DOI] [PubMed] [Google Scholar]
- 11.Kilpatrick SE. Fine needle aspiration biopsy of Langerhans cell histiocytosis of bone: Are ancillary studies necessary for a definitive diagnosis? Acta Cytol. 1998;42:820–3. [PubMed] [Google Scholar]
- 12.Egeler RM, Neglia JP, Aricò M, Favara BE, Heitger A, Nesbit ME, et al. The relation of Langerhans cell histiocytosis to acute leukemia, lymphomas, and other solid tumors. The LCH-Malignancy Study Group of the Histiocyte Society. Hematol Oncol Clin North Am. 1998;12:369–78. doi: 10.1016/s0889-8588(05)70516-5. [DOI] [PubMed] [Google Scholar]
- 13.Yanagawa T, Watanabe H, Shinozaki T, Ahmed AR, Shirakura K, Takagishi K. The natural history of disappearing bone tumours and tumour-like conditions. Clin Radiol. 2001;56:877–86. doi: 10.1053/crad.2001.0795. [DOI] [PubMed] [Google Scholar]
- 14.Yamaguchi S, Oki S, Kurisu K. Spontaneous regression of Langerhans cell histiocytosis: A case report. Surg Neurol. 2004;62:136–40. doi: 10.1016/j.surneu.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 15.Broadbent V, Egeler RM, Nesbit ME Jr. Langerhans cell histiocytosis – clinical and epidemiological aspects. Br J Cancer Suppl. 1994;23:S11–6. [PMC free article] [PubMed] [Google Scholar]


