Abstract
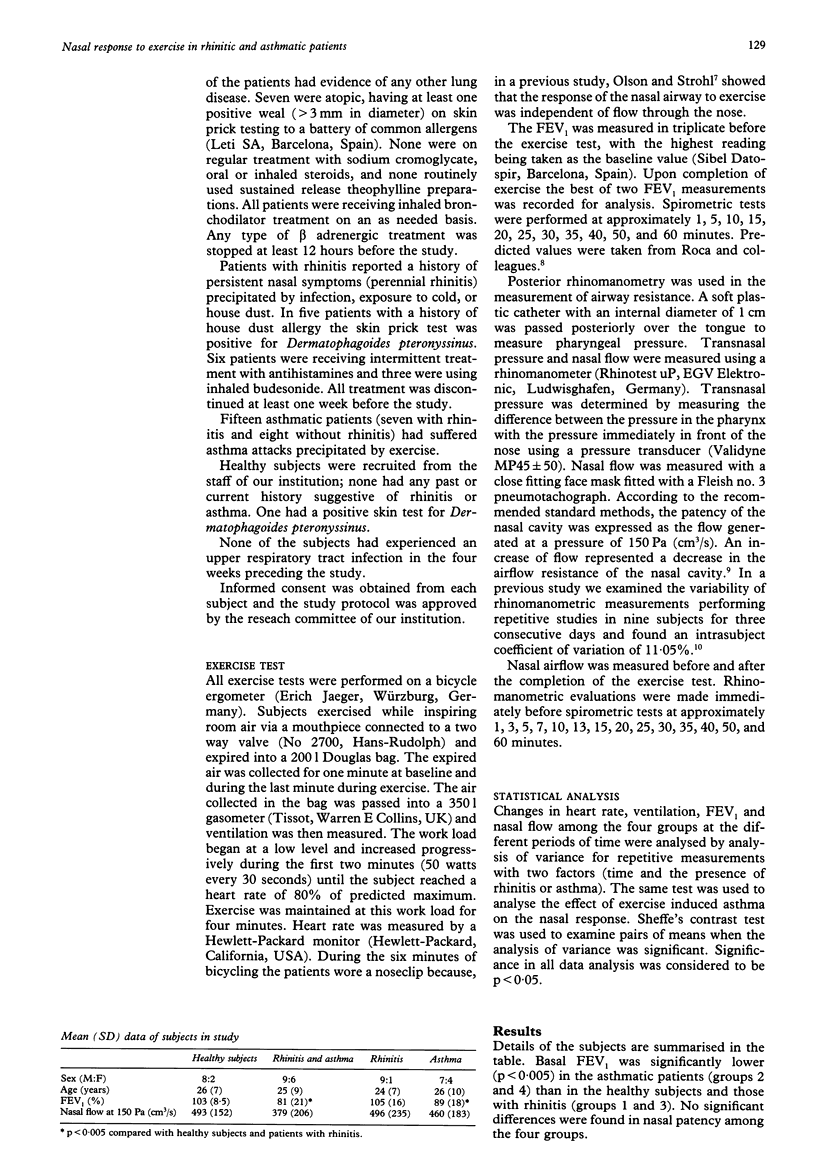
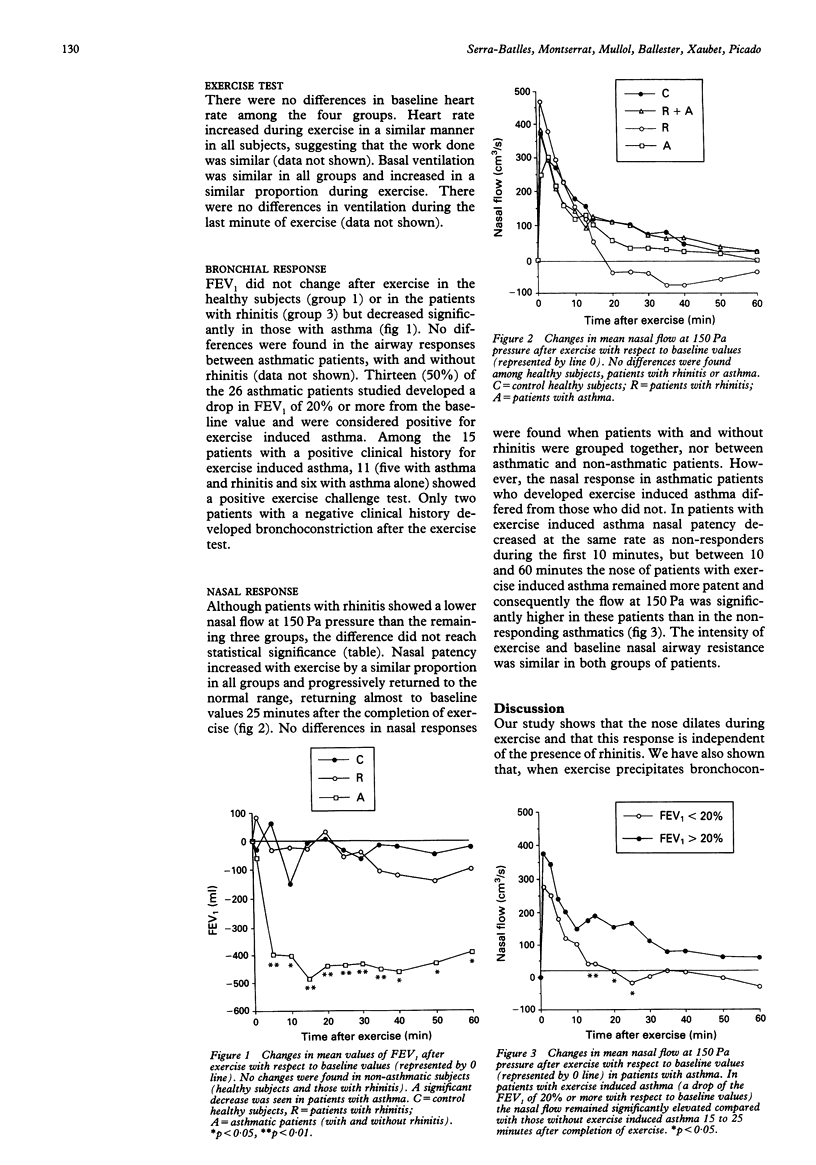
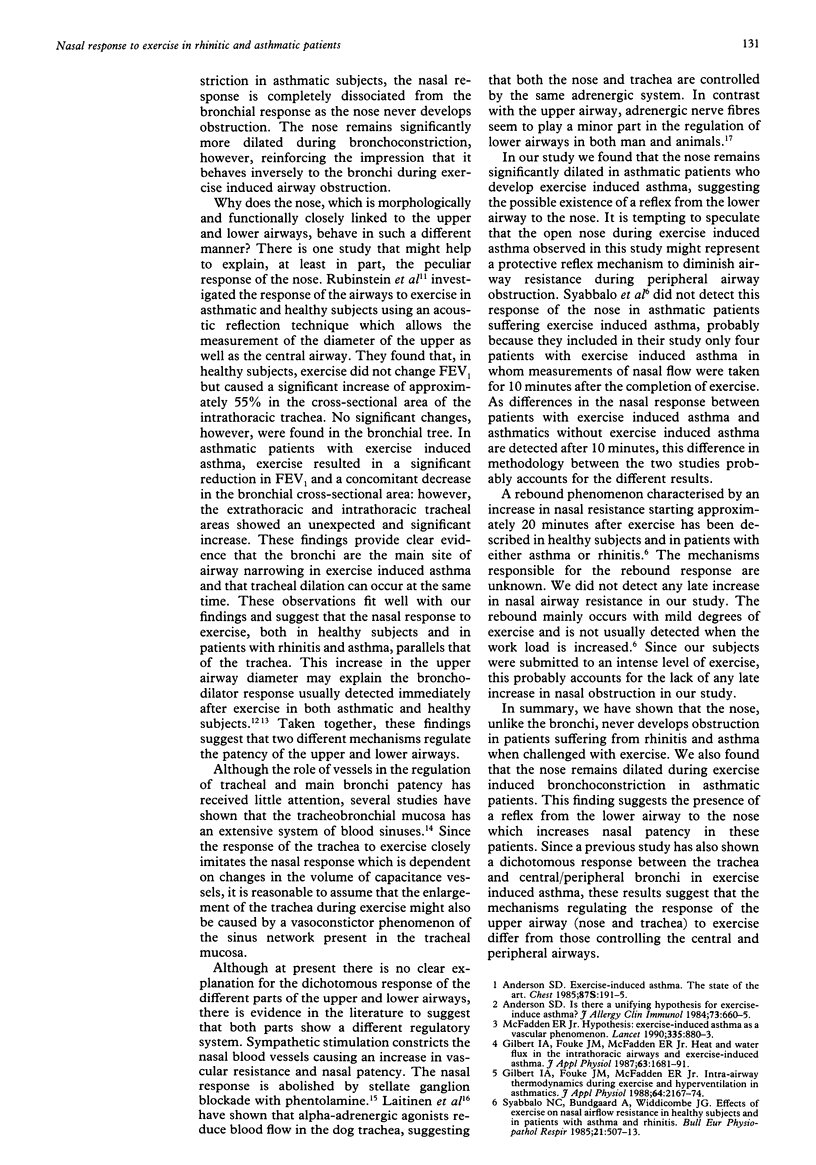
BACKGROUND--Although the nose and the bronchi are both involved in the process of regulating respiratory heat exchange, thermal changes may precipitate airway obstruction during exercise but rarely cause nasal obstruction in patients with rhinitis. The cause of the different response of the nose and bronchial tree has hardly been investigated. This study was performed to assess the response of the nose during exercise in the presence of rhinitis, asthma, and in normal controls. METHODS--Ten healthy subjects (group 1), 15 patients with asthma and rhinitis (group 2), 10 with rhinitis only (group 3), and 11 with asthma only (group 4) were included in the study. Exercise was performed on a bicycle ergometer for six minutes, reaching a heart rate of 80% of predicted. Bronchial and nasal responses were measured by forced expiratory volume in one second (FEV1) and posterior rhinomanometry, respectively. A drop in the FEV1 of 20% or more was considered a positive exercise induced asthma challenge test. RESULTS--Heart rate and ventilation increased by a similar proportion in the four groups. The FEV1 significantly decreased in asthmatic patients (groups 2 and 4) but it did not change in healthy subjects (group 1) or in those with rhinitis (group 3). Thirteen asthmatic patients developed exercise induced asthma. Nasal patency increased with exercise by a similar proportion in all groups, and no differences were detected between those with rhinitis (groups 2 and 3) and those without (groups 1 and 4). Nasal patency had returned to basal values at 25 minutes after completion of exercise in the four groups. The nose of patients with exercise induced asthma, however, remained significantly more patent than in patients without exercise induced asthma between 10 and 30 minutes after exercise. CONCLUSIONS--These results suggest that the nose responds differently from the bronchi during exercise induced airway obstruction: whereas the bronchial tree responds by becoming narrowed, the nose becomes more patent. These findings suggest that the mechanisms regulating the response of the nose to exercise are different from those involved in the response of the bronchial tree.
Full text
PDF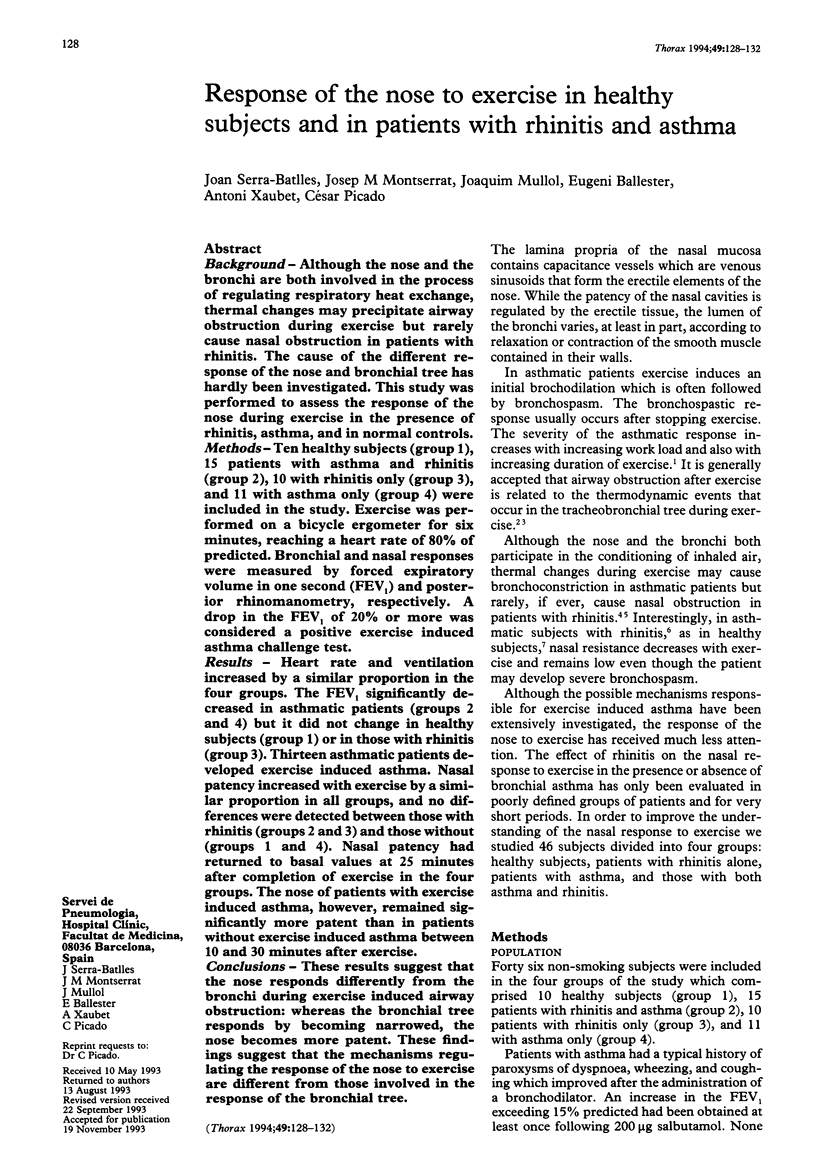

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anderson S. D. Is there a unifying hypothesis for exercise-induced asthma? J Allergy Clin Immunol. 1984 May;73(5 Pt 2):660–665. doi: 10.1016/0091-6749(84)90301-4. [DOI] [PubMed] [Google Scholar]
- Gelb A. F., Tashkin D. P., Epstein J. D., Gong H., Jr, Zamel N. Exercise-induced bronchodilation in asthma. Chest. 1985 Feb;87(2):196–201. doi: 10.1378/chest.87.2.196. [DOI] [PubMed] [Google Scholar]
- Gilbert I. A., Fouke J. M., McFadden E. R., Jr Heat and water flux in the intrathoracic airways and exercise-induced asthma. J Appl Physiol (1985) 1987 Oct;63(4):1681–1691. doi: 10.1152/jappl.1987.63.4.1681. [DOI] [PubMed] [Google Scholar]
- Gilbert I. A., Fouke J. M., McFadden E. R., Jr Intra-airway thermodynamics during exercise and hyperventilation in asthmatics. J Appl Physiol (1985) 1988 May;64(5):2167–2174. doi: 10.1152/jappl.1988.64.5.2167. [DOI] [PubMed] [Google Scholar]
- Haas F., Pasierski S., Levine N., Bishop M., Axen K., Pineda H., Haas A. Effect of aerobic training on forced expiratory airflow in exercising asthmatic humans. J Appl Physiol (1985) 1987 Sep;63(3):1230–1235. doi: 10.1152/jappl.1987.63.3.1230. [DOI] [PubMed] [Google Scholar]
- McFadden E. R., Jr Hypothesis: exercise-induced asthma as a vascular phenomenon. Lancet. 1990 Apr 14;335(8694):880–883. doi: 10.1016/0140-6736(90)90478-n. [DOI] [PubMed] [Google Scholar]
- Olson L. G., Strohl K. P. The response of the nasal airway to exercise. Am Rev Respir Dis. 1987 Feb;135(2):356–359. doi: 10.1164/arrd.1987.135.2.356. [DOI] [PubMed] [Google Scholar]
- Richerson H. B., Seebohm P. M. Nasal airway response to exercise. J Allergy. 1968 May;41(5):269–284. doi: 10.1016/0021-8707(68)90032-4. [DOI] [PubMed] [Google Scholar]
- Roca J., Sanchis J., Agusti-Vidal A., Segarra F., Navajas D., Rodriguez-Roisin R., Casan P., Sans S. Spirometric reference values from a Mediterranean population. Bull Eur Physiopathol Respir. 1986 May-Jun;22(3):217–224. [PubMed] [Google Scholar]
- Serra Batlles J., Montserrat J. M., Martos J. A., Picado C., Agustí Vidal A. Rinomanometría anterior. An Otorrinolaringol Ibero Am. 1990;17(2):159–164. [PubMed] [Google Scholar]
- Syabbalo N. C., Bundgaard A., Widdicombe J. G. Effects of exercise on nasal airflow resistance in healthy subjects and in patients with asthma and rhinitis. Bull Eur Physiopathol Respir. 1985 Nov-Dec;21(6):507–513. [PubMed] [Google Scholar]


