To the Editors
We read with interest the retrospective study by Unge et al1 that showed that an antiretroviral treatment program in Kibera, Kenya, had low clinic retention rates. They found that residents from Kibera were 11 times more likely to drop out of the community-based health clinic run by the African Medical and Research Foundation and Ministry of Medical Services, Kenya. The clinic was based in Kibera, the largest urban informal settlement in Kenya, and provided free treatment and care for HIV-infected individuals. An estimated 26% of participants dropped out over 12 months; and the authors concluded that “harsh conditions associated with living in an urban slum like Kibera are likely related to this risk elevation and may include underlying causes of dropout such as premature death, competing causes of diseases, alcohol or substance abuse, poverty, and high mobility.”1
We are writing because the results from our own antiretroviral treatment clinic based in Nairobi near Kibera do not reflect a higher rate of dropout among residents from Kibera compared with those living outside of this informal settlement. In 2004, the University of Washington and the Coptic Hospital implemented an HIV clinic in Nairobi, Kenya, called the Coptic Hope Center for Infectious Diseases. With support from the President’s Emergency Plan for AIDS Relief, free antiretroviral medications, comprehensive medical care, and counseling, nutritional, and social work services were provided by the Hope Center. Nearly 9000 patients have been enrolled at this urban site, which is a 20-minute walk from Kibera.
From March 2006, when residence data were first collected at the Hope Center, to December 2007, the clinic enrolled 1231 patients who were antiretroviral naive, above the age of 15 years, and initiated highly active antiretroviral therapy (HAART). Of the 1231 patients, 110 (9%) resided in Kibera, 871 (71%) resided outside Kibera, and 250 (20%) did not have residential data collected. Loss-to-follow-up was defined as not returning to clinic more than 30 days after the next scheduled pharmacy appointment (n = 966) or 120 days after last medical follow-up visit if pharmacy information was missing (n = 15). At 12 months follow-up after enrollment, the probability of retention among non-Kibera residents was 0.89 [95% Confidence Interval (CI), 0.87 to 0.92] and among Kibera residents was 0.90 (95% CI, 0.76 to 0.96) (Fig. 1). In an adjusted Cox proportional hazards model accounting for baseline tuberculosis status, age, gender, and weight, residence in Kibera was not associated with a greater risk of loss to follow-up (hazard ratio, 1.02; 95% CI, 0.47 to 2.24).
FIGURE 1.
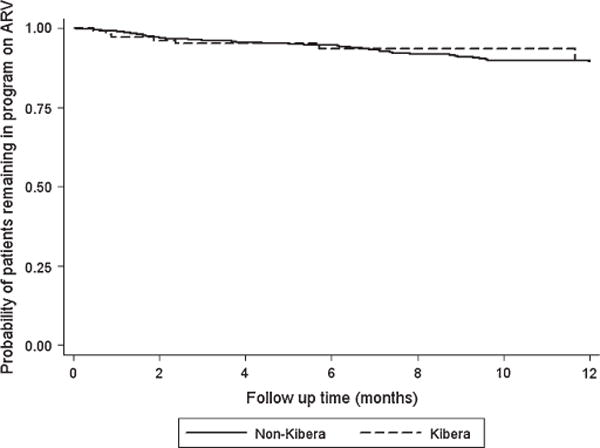
Survival analysis comparing retention between Kibera and non-Kibera residents at the Coptic Hope Center for Infectious Diseases in Nairobi, Kenya (P = 0.89).
Thus, we caution against the conclusion that residing in Kibera or any urban slum is a risk factor for poor retention or that programs that implement antiretroviral treatment programs in poor urban settlements may risk higher dropouts and worse clinical outcomes. There are a few points of discussion that should be raised in relation to this study. First, it is important to note that Kibera is a very large area covering a diverse range of socioeconomic backgrounds. Some residents are middle-class Kenyans with a yearly salary and not necessarily day laborers with low incomes. Some in Kibera live in cement apartment housing and not in tin roof shacks, whereas others are college educated. Because of this diversity, instead of differentiating based on residence in Kibera, it may be more helpful to characterize patients by income, housing, and educational status.
Second, it is necessary to know that during the period described by this study (2005–2007), President’s Emergency Plan for AIDS Relief was beginning to support many different free antiretroviral treatment programs in Nairobi. The authors note that the clinic they examined “is reportedly suffering from a heavy workload and reduced workspace that threatens the quality of services.”1 Given this situation, if Kibera residents had other HIV treatment options available to them within walking distance or easy public transportation, they may have taken this opportunity to transfer care. One of main reasons for dropping out may therefore have been to receive medical treatment at another adjacent HIV clinic, particularly if waiting times were less or if free services were more comprehensive.
Third, the proximity of the clinic to home may have been a problem in retention. The study found that “a substantial number of patients drop out of ART treatment despite being provided with ART free of charge at a clinic only a short distance from home.”1 However, instead of a short distance being a benefit, this may have actually been a deterrent to patients seeking anonymity of care. HIV remains a highly stigmatizing disease in Kenya, and we have found that patients often seek care where they may not be recognized. Many also prefer to attend HIV clinics in hospital settings where the type of medical assistance can be disguised until well after they walk through the hospital gates. HIV-infected individuals may be reluctant to attend an HIV clinic in their own backyard if they haven’t disclosed their status to friends and family members, and it is well known that only those with HIV enter the building for treatment.
In conclusion, we realize the importance of the study by Unge et al1 in describing challenges for ART scale-up in resource-limited setting, however, we believe that their poor clinic retention rates were less a reflection of Kibera residence than of the location and state of their antiretroviral treatment program in comparison to other HIV programs providing free treatment in the area.
Acknowledgments
Michael H. Chung is supported by a K23 grant, National Institutes of Health (5K23AI065222-04). The Coptic Hope Center for Infectious Diseases is supported by the President’s Emergency Plan for AIDS Relief through a cooperative agreement (U62/CCU024512-04) from the US Centers for Disease Control and Prevention.
References
- 1.Unge C, Sodergard B, Ekstrom AM, et al. Challenges for scaling up ART in a resource-limited setting: a retrospective study in Kibera, Kenya. J Acquir Immune Defic Syndr. 2009;50:397–402. doi: 10.1097/QAI.0b013e318194618e. [DOI] [PubMed] [Google Scholar]


