Abstract
Introduction:
Mastectomy in patients with breast cancer can severely affect their body esteem. It also changes the emotions and attitudes of patients toward their body and causes psychological reactions such as depression, anxiety, and stress.
Aims:
This study was conducted with the aim of assessing correlation between body esteem and mental health in patients with breast cancer after mastectomy.
Materials and Methods:
This study is a descriptive study. One hundred patients with breast cancer after mastectomy were selected by convenience sampling from Seyed Al Shohada Hospital in Isfahan. Data gathering tools were questionnaires of body esteem and SCL-25 mental health and were analyzed by SPSS-PC (v.17).
Results:
According to the score of body esteem (2.80) and the overall average score for body esteem (36.46), patients had low body esteem. About dimensions of the mental health, the highest average was associated with depressive disorders. According to the results of the Spearman correlation coefficient, there was a direct linear relationship between body esteem and mental health.
Conclusion:
Considering the impact of mastectomy on body esteem and mental health and the relationship between the variables, nurses take steps for identifying and referring patients to the counseling centers to prevent psychological disorder aspects.
Keywords: Breast cancer, mastectomy, mental health
INTRODUCTION
Nowadays, breast cancer is the most important factor threatening women's health. Based on the WHO report, over 1.1 million new cases of breast cancer are detected among women, which is 10% of total new cases of cancer and 23% of total cancers among women.[1] In Iran, this disease is the most common type of cancer among women and is one of their major health problems.[2] For most of the women, mastectomy leads to missing a part of body, which seems necessary for the preservation of womanhood, attraction, and self-confidence. Due to the important role of breasts in women, their reaction to mastectomy may be in the form of fear, hopelessness, depression, and a negative attitude about their body.[3] As breasts are considered as important parts of imagining a women's body, any abnormality in breast and the related treatments can lead to negative body esteem in women, as a surgery makes them feel that they have missed everything.[4] As everybody likes a perfect body, mastectomy influences patients' physical attraction and appearance and can affect their emotional stability, lead to unpleasant emotional tension, negatively change their body image, and threaten their mental health.[5] However, every individual is a combination of sociopsychological and physiologic dimensions, and a change in any of these dimensions can affect others. Positive or negative reactions of the family members and relatives and their support may change the patients' body esteem.[6] The society reinforces the approaches of body esteem in different ways as it puts a high value on physical attraction. It can be noted that even from the viewpoint of the society, physical and body attraction is more noticed by the public, compared to other variables. Therefore, the society and relatives' support can alter our viewpoints about what our body is like and what it should look like.[7] Breast cancer and its treatments including mastectomy are disturbing events for the women, which can lead to notable mental effects among them. Research shows that the patients are more likely to have changes in all of their psychological dimensions after mastectomy, and this type of treatment can even influence their mental health.[8] Mental health is among primary principles of mental health care. Mastectomy seems to negatively affect not only physical function, but also mental, psychological, and social functions of the patients.[9] Studies have reported that individuals' psychological dimension can be a criterion to evaluate their mental health.
Mental health plays a pivotal role in dynamicity and self-efficacy of each person and is one of the elements to evaluate health status in societies.
Therefore, it can be said that all societies aim at provision of conditions in which individuals' health is preserved and promoted.[10] Body esteem is closely associated with mental health as body esteem highly affects the trend of thoughts, psychological conditions, behavior, values and goals, and generally human's mental health[11] with regard to inevitable impact of breast cancer on body esteem and mental health and the necessity of investigating the related variables.
Objective
The present study aimed to investigate the association between body esteem and mental health among breast cancer patients after mastectomy.
MATERIALS AND METHODS
In this correction coefficient-based descriptive study, sample size was estimated of 100 subjects based on confidence interval of 95% and the statistical power of 80% with supposition of correlation coefficient of r = 0.25 between body esteem and patients' mental health. Study population comprised all breast cancer patients referring to Seyed Al-Shohada hospital in Isfahan after mastectomy who were gradually selected and entered into the study. The inclusion criteria for the participants were the following: The participants should be among those who go to hospital for receiving health care or medical advice, at least 6 months should have been passed from their one-sided mastectomy, the participants should not have any other diagnosed disease, the patient should be able to respond to questions in the questionnaire, the patient should not be under chemotherapy, mastectomy should not be restorable, and all participants should be above 30.
The data collection tool was composed of body esteem and SCL25 questionnaires. Body esteem questionnaire was a part of physical disability body esteem questionnaire. Body esteem questionnaire was first adopted by Ghodousi et al. In their study, internal reliability was used to measure the reliability of the tool and Cronbach alpha was calculated as 0.80. This questionnaire has 13 general items with a five-point Likert scale ranging 1-5 points including absolutely agree = 1; agree = 2; no idea = 3; disagree = 4, and absolutely disagree = 5. It has four sub-scales including physical attraction (questions 1-9), feeling of being comfortable with the body (questions 3, 7, and 13), comparison of the body with a healthy body (questions 2, 5, 6, 10, and 12), and physical attraction from the patient's and others' viewpoints (questions 4, 8, and 11). Mean and standard deviation are separately calculated for each question and for all questions in the sub-scales. Appropriate body esteem is calculated based on the value of each question on body esteem, total score of body esteem, and mean total score of body esteem.
Total mean score ranges 13-65 points. The more the mean is closer to 65, the level of body esteem is higher. When it is lower and closer to 13, it shows lower body esteem. In this questionnaire, question 13 is inversely scored. The questions have been designed in such a way that single participants can also answer the questions.[12] The questionnaire of mental health, adapted to measure patient's mental health, was SCL-25, which is a brief form of SCL-90-R. SCL25-R contains nine dimensions of physical complaints, obsession and compulsion, irritability in personal interactions, depression, anxiety, phobic anxiety, psychosis, paranoid thoughts, aggression, and some extra questions. This scale includes 25 items with a five-point Likert scale of none = 0; little = 1; somehow = 2; much = 3; and severely = 4. The scores in mental health range from 0 to 100 in this questionnaire. Lower scores show higher mental health and the scores higher than 65 show possibility of a mental disorder.[13] In the present study, the reliability of the above questionnaire was measured with Cronbach alpha. The researcher, after referring to research environment, distributed the questionnaires among 30 patients. After collection of the questionnaires, Cronbach alpha for body esteem and mental health questionnaire were 0.85 and 0.92, respectively, through SPSS software version 16. After selection of the qualified subjects, the researcher introduced herself and explained the goal of the study to the subjects and after attaining their written consent and assuring them about the confidentiality of their information, the questionnaires were distributed among them. It should be noted that the researcher read the questions to the subjects and recorded their responses word for word.
The sampling was continued until the completion of the required number and lasted for 3 months. The data were analyzed through SPSS version 16. The tables were made by the use of descriptive statistical method. Inferential tests were used to analyze the data.
RESULTS
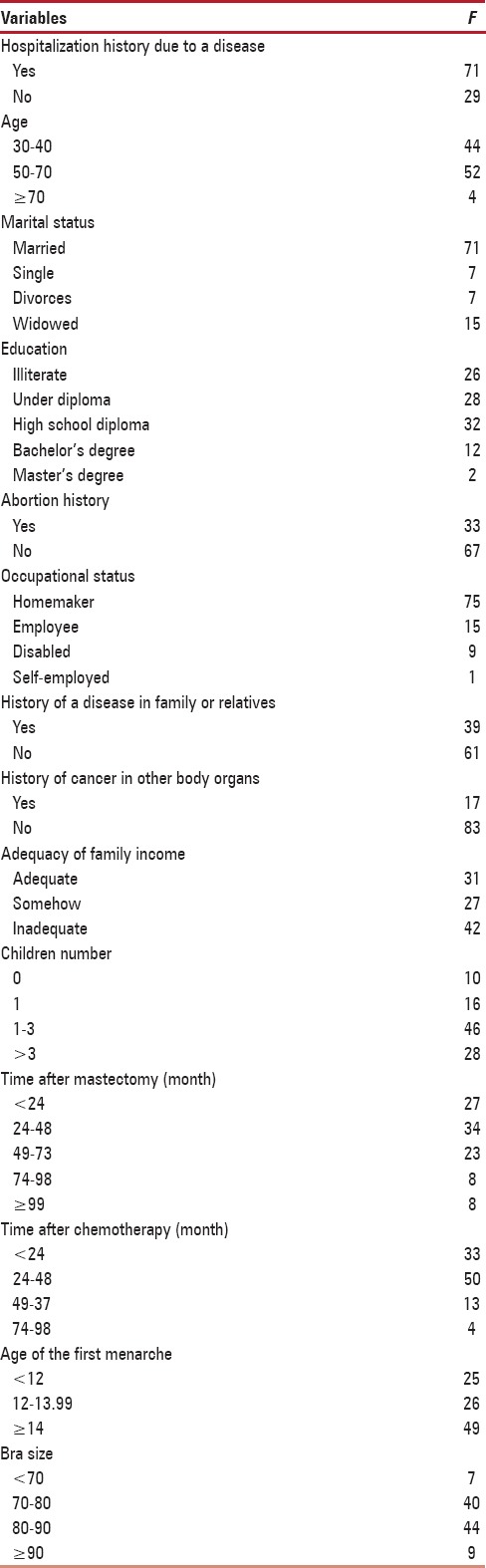
The obtained results showed a low score of body esteem (2.80) and its total mean (36.46) among the patients. The results showed that the highest mean score in sub-scales of body esteem was for physical attraction (65.2) and the lowest for comparison of the body with a healthy body (51.73). The highest and the lowest scores of body esteem were for items, “If someone tells me I am attractive, I doubt about him/her” and “I would look more attractive if I did not have such a disability” as 3.23 and 2.41, respectively [Table 1]. Total score of mental health (69) showed that the patients were likely to have mental disorders. With regard to nine dimensions of mental health, the highest mean score was for subjects' depression (3.05) [Table 2]. Spearman correlation coefficient showed a significant direct linear association among body esteem, hope, and mental health, and this association was stronger with body esteem and hope (Rs = 0.583, P < 0.001) [Table 3]. The findings also showed that the highest frequency was for the age group of 50-70 years (52%), 7% of the participants were single and 71% were married. Most of the participants (32%) had high school education, 33% had a history of abortion, and 17% had a history of cancer in other organs of their body. Subjects' other complementary data have been presented in Table 4.
Table 1.
Descriptive characteristics of body esteem sub-scales in patients
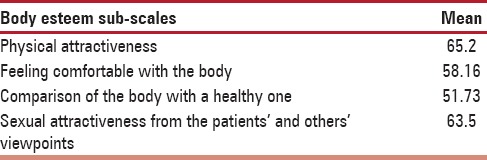
Table 2.
Mean and SD of mental health sub-scales in the subjects
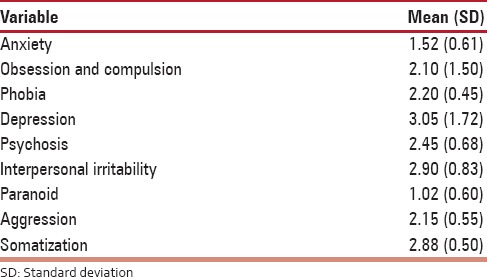
Table 3.
Association between mental health and body esteem in the subject
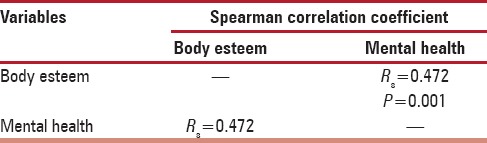
Table 4.
Frequency distribution of subjects' demographic characteristics
DISCUSSION
The results showed that the patients had low body esteem and their body esteem score was 2.80 (1.14). Although body esteem has a multi-dimensional structure, it is known by degrees of appearance, size, shape, and general appearance.[14] Body esteem changes personality domains, social situation, and success.[15] Our results are in line with those of Unukovych et al. They found that breast cancer and its treatments including mastectomy negatively affected body esteem.[16] Pinto believes that the patients after a mastectomy, when found their body abnormal and imperfect, wish they could exchange their body with a healthy one as chronic diseases manifestations and complications impair patients' comfort and peace and lead to their dissatisfaction with their body, and consequently influence their body esteem.[17] den Heijer et al. and Pinto et al. attained results consistent with the present study.[17,18] Meanwhile, our results are not in line with Ghodousi et al. on the association between body esteem and multiple sclerosis.[12] Based on the obtained total score of mental health (69) in the present study, the subjects were likely to have mental disorders. Most of the subjects showed the highest score for depression (1.63 ± 0.72) in the nine dimensions of mental health. Survival is longer in breast cancer, and consequently, the patients are influenced by cancer, its complications, and treatment outcomes for a longer time.[19] A stressful event can endanger various aspects of patients' personal health including physical, mental, and familial health as stressful treatments such as mastectomy cause high levels of stress, anxiety, and depression among the patients.[20] Kash et al., Fallbjork et al., and Isern and Tengrup obtained similar results.[21,22,23] Spearman correlation coefficient showed a significant direct linear association between body esteem and mental health, which is consistent with the findings of Fallbjork et al. and Kim et al.[21,22,23,24]
Physical identity, mental health, and probable success in various dimensions of life are among the factors, which are influenced by body esteem. It should be noted that the women with breast cancer, after mastectomy, lose a body part that is the symbol of their womanhood, and it impairs their body esteem, which results in their lowered self-confidence, loss of beauty, and consequently, anxiety and depression.[25]
With regard to the effect of mastectomy on body esteem and mental health and the association between above-mentioned variables, nurses can change public approach toward physically disabled people and play a pivotal role in positive body esteem among the patients through detection and referring these patients to counseling centers. They can also prevent the patients' mood disorders through detection of their psychological tensions.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
This study was derived from a research project, approved in vice-chancellery for research and technology in Shahrekord University of Medical Sciences as well as all authorities of Seyed Al-Shohada hospital in Isfahan and the patients who cooperated with us in this research.
REFERENCES
- 1.Prat A, Cheang MC, Martín M, Parker JS, Carrasco E, Caballero R, et al. Prognostic significance of progesterone receptor positive tumor cells within immune histochemically defined luminal a breast cancer. J Clin Oncol. 2013;31:203–9. doi: 10.1200/JCO.2012.43.4134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Esmaili R, Saiidi JA, Majd HA, Esmaieli M. A survey of the body image of mastectomies women referring to Imam Khomeini and Imam Hussein hospitals in Tehran, Iran. Indian J Psychol Med. 2010;32:34–7. doi: 10.4103/0253-7176.70528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Giardini A, Pisoni C, Giorgi I. ICF, quality of life, and depression in breast cancer: Perceived disability in disease-free women 6 months after mastectomy. Support Care Cancer. 2013;21:2949–53. doi: 10.1007/s00520-013-1794-7. [DOI] [PubMed] [Google Scholar]
- 4.Gopie JP, Mureau MA, Seynaeve C, Ter Kuile MM, Menke-Pluymers MB, Timman R, et al. Body image issues after bilateral prophylactic mastectomy with breast reconstruction in healthy women at risk for hereditary breast cancer. Fam Cancer. 2013;12:479–87. doi: 10.1007/s10689-012-9588-5. [DOI] [PubMed] [Google Scholar]
- 5.Ohaeri BM, Ofi AB, Campbell OB. Relationship of knowledge of psychosocial issues about cancer with psychic distress and adjustment among breast cancer clinic attendees in a Nigerian teaching hospital. Psychooncology. 2012;21:419–26. doi: 10.1002/pon.1914. [DOI] [PubMed] [Google Scholar]
- 6.Pujols Y, Seal BN, Meston CM. The association between sexual satisfaction and body image in women. J Sex Med. 2010;7(2 Pt 2):905–16. doi: 10.1111/j.1743-6109.2009.01604.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Seal BN, Bradford A, Meston CM. The association between body esteem and sexual desire among college women. Arch Sex Behav. 2009;38:866–72. doi: 10.1007/s10508-008-9467-1. [DOI] [PubMed] [Google Scholar]
- 8.Goldhirsch A, Winer EP, Coates AS, Gelber RD, Piccart-Gebhart M, Thürlimann B, et al. Personalizing the treatment of women with early breast cancer: Highlights of the St Gallen international expert consensus on the primary therapy of early breast cancer 2013. Ann Oncol. 2013;24:2206–23. doi: 10.1093/annonc/mdt303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dastan NB, Buzlu S. Depression and anxiety levels in early stage Turkish breast cancer patients and related factors. Asian Pac J Cancer Prev. 2011;12:137–41. [PubMed] [Google Scholar]
- 10.Giardini A, Pisoni C, Giorgi I, Borelli V, Scoccia E, Majani G. ICF, quality of life, and depression in breast cancer: Perceived disability in disease-free women 6 months after mastectomy. Support Care Cancer. 2013;21:2453–60. doi: 10.1007/s00520-013-1794-7. [DOI] [PubMed] [Google Scholar]
- 11.Henderson AK, Ellison CG. My body is a temple: Eating disturbances, religious involvement, and mental health among young adult women. J Relig Health. 2015;54:954–76. doi: 10.1007/s10943-014-9838-y. [DOI] [PubMed] [Google Scholar]
- 12.Ghodusi M, Heidari M. Evaluation body esteems and related factors in patients with Multiple Sclerosis. J Res Behave Sci. 2013;11:1–13. [Google Scholar]
- 13.Najarian B, Davoodi I. Making validation Scl25, short form Scl90. J Psychol. 2001;2:136–49. [Google Scholar]
- 14.Fitzsimmons-Craft EE, Harney MB, Koehler LG, Danzi LE, Riddell MK, Bardone-Cone AM. Explaining the relation between thin ideal internalization and body dissatisfaction among college women: The roles of social comparison and body surveillance. Body Image. 2012;9:43–9. doi: 10.1016/j.bodyim.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 15.Mak KK. Body esteem in Chinese adolescents: Effect of gender, age, and weight. J Health Psychol. 2012;17:3–16. doi: 10.1177/1359105312437264. [DOI] [PubMed] [Google Scholar]
- 16.Unukovych D, Sandelin K, Liljegren A, Arver B, Wickman M, Johansson H, et al. Contralateral prophylactic mastectomy in breast cancer patients with a family history: A prospective 2-years follow-up study of health related quality of life, sexuality and body image. Eur J Cancer. 2012;48:3150–6. doi: 10.1016/j.ejca.2012.04.023. [DOI] [PubMed] [Google Scholar]
- 17.Pinto BM, Trunzo JJ. Body esteem and mood among sedentary and active breast cancer survivors. Mayo Clin Proc. 2004;79:181–6. doi: 10.4065/79.2.181. [DOI] [PubMed] [Google Scholar]
- 18.den Heijer M, Seynaeve C, Timman R, Duivenvoorden HJ, Vanheusden K, Tilanus-Linthorst M, et al. Body image and psychological distress after prophylactic mastectomy and breast reconstruction in genetically predisposed women: A prospective long-term follow-up study. European Journal of Cancer. 2012;48:1263–8. doi: 10.1016/j.ejca.2011.10.020. [DOI] [PubMed] [Google Scholar]
- 19.Jacobsen PB, Jim HS. Consideration of quality of life in cancer survivorship research. Cancer Epidemiol Biomarkers Prev. 2011;20:2035–41. doi: 10.1158/1055-9965.EPI-11-0563. [DOI] [PubMed] [Google Scholar]
- 20.Nakatani Y, Iwamitsu Y, Kuranami M, Okazaki SH. Predictors of psychological distress in breast cancer patients after surgery. Kitasato Med J. 2013;43:49–56. [Google Scholar]
- 21.Fallbjork U, Rasmussen B, Karlsson S. Aspects of body image after mastectomy due to breast cancer - A two-year follow-up study. Eur J Oncol Nurs. 2012;14:1–6. doi: 10.1016/j.ejon.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 22.Kash KM, Holland JC, Halper MS, Miller DM. Psychological distress and surveillance behaviours of women with a family history of breast cancer. Indian J Psychol Med. 2013;84:24–30. doi: 10.1093/jnci/84.1.24. [DOI] [PubMed] [Google Scholar]
- 23.Isern AE, Tengrup I, Loman N, Olsson H, Ringberg A. Aesthetic outcome, patient satisfaction, and health-related quality of life in women at high risk undergoing prophylactic mastectomy and immediate breast reconstruction. J Plast Reconstr Aesthet Surg. 2008;61:1177–87. doi: 10.1016/j.bjps.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 24.Kim SH, Son BH, Hwang SY, Han W, Yang JH, Lee S, et al. Fatigue and depression in disease-free breast cancer survivors: Prevalence, correlates, and association with quality of life. J Pain Symptom Manage. 2008;35:644–55. doi: 10.1016/j.jpainsymman.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 25.Tel H, Dogan S. Fatigue, anxiety and depression in cancer patients. Neurol Psychiatry Brain Res. 2011;17:42–5. [Google Scholar]


