Abstract
Context:
Type 2 diabetes mellitus (T2DM) in young adults is increasing in India. Data on the prevalence of cardiovascular (CV) risk factors and complications associated with young-onset T2DM (YOD) at the time of diagnosis of diabetes are limited. This data can aid in aggressive diabetes management, CV risk reduction, and prevention of complications.
Aim:
To determine the prevalence of CV risk factors, micro and macrovascular complications in patients with newly diagnosed YOD. To assess the percentage of patients who require statin therapy based on current American Diabetes Association (ADA) guidelines.
Settings and Design:
This was a retrospective cross-sectional study of 1500 patients with newly detected YOD across seven centers from 2013 to 2015.
Designs and Methods:
Patients were evaluated for complications of diabetes and CV risk factors such as body mass index (BMI), hypertension, dyslipidemia, and smoking.
Statistical Analysis:
Measurements have been presented as mean ± standard deviation; results on categorical measurements have been presented in percentages.
Results:
The mean age, glycated hemoglobin and BMI were 34.7 ± 4.2 years, 9.9 ± 2.4%, and 26.8 ± 4.7 kg/m2. Hypertension, dyslipidemia, BMI >23 kg/m2, and smoking were presented in 27.6%, 62.4%, 84.2%, and 24%. Diabetic retinopathy, neuropathy, and nephropathy were seen in 5.1%, 13.2%, and 0.9%. Ischemic heart disease, peripheral vascular disease, and stroke were presented in 0.7%, 2%, and 0.1%. As per current guidelines, 95.33% needed statin therapy.
Conclusion:
This study demonstrates that patients with YOD have micro and macrovascular complications at diagnosis. Nearly, every patient required a statin to reduce CV risk. This highlights the importance of screening patients with YOD for CV risk factors and complications of diabetes at the time of diagnosis.
Keywords: Cardiovascular risk, complications, dyslipidemia, neuropathy, retinopathy, type 2 diabetes, young onset diabetes
INTRODUCTION
The prevalence of type 2 diabetes mellitus (T2DM) in India is increasing exponentially.[1] There has also been an increase in the number of young adults with T2DM.[1] Patients diagnosed to have T2DM under the age of 40 years are designated to have Young onset Diabetes (YOD).[2]
In Asian Indians, diagnosis of diabetes occurs at younger ages and lower body mass index (BMI).[3] Patients with YOD often have inadequate glycemic control and multiple cardiovascular (CV) risk factors. This contributes to an increase in micro and macrovascular complications over time.[2,4,5,6,7]
The extent of complications and presence of CV risk factors at the time of diagnosis of T2DM in India has been reported in several studies.[8,9,10,11] Data on patients with YOD are limited. Identification of CV risk factors, complications, and initiation of multifactorial risk reduction is pivotal to diabetes care in this vulnerable population.
The aim of this study was to determine the prevalence of CV risk factors, micro, and macrovascular complications, and assess the need for statin therapy in patients with newly diagnosed YOD in India.
DESIGNS AND METHODS
This is a retrospective analysis of patients with newly diagnosed YOD attending the outpatient departments of seven specialized diabetes clinics across India between 2013 and 2015. The study population comprised 1500 patients with newly diagnosed YOD. The diagnosis of diabetes was based on the ADA criteria.[12] Newly diagnosed diabetes was defined by an arbitrary cut-off point as a known duration of diabetes <3 months. Patients with type 1 diabetes, gestational diabetes mellitus those confirmed or suspected to have latent autoimmune diabetes in adults were excluded. Standard protocols were uniformly followed across all the study centers for patient evaluation and data entry.
Each patient underwent a thorough history and physical examination. History of hypertension, dyslipidemia, smoking, micro and macrovascular complications of diabetes was recorded. Patients were screened for the presence of CV risk factors such as BMI, hypertension, dyslipidemia (low-density lipoprotein [LDL] >100 mg/dl) along with the micro and macrovascular complications of diabetes.
Definitions
Body mass index
Lower BMI cut-offs as per Indian guidelines[13] were used to diagnose overweight and obese patients. BMI definitions were as follows:
<18.5 kg/m2: Underweight
18.5–22.9 kg/m2: Normal BMI
23–24.9 kg/m2: Overweight
>25 kg/m2: Obese.
Hypertension
The blood pressure (BP) was measured in the sitting position, after 15 min of rest in a quiet room. Those with a BP >140/90 mmHg were diagnosed to have hypertension. This was confirmed at three follow-up BP recordings before the diagnosis was made.[14]
Dyslipidemia
The diagnosis of dyslipidemia was made in all patients who had an LDL cholesterol >100 mg/dl in a fasting lipid profile.[15]
Retinopathy
The diagnosis of retinopathy was made by a retinal specialist on a dilated pupil using direct ophthalmoscopy using the early treatment diabetic retinopathy study grading system.[16]
Nephropathy
The diagnosis of nephropathy was based on the 24 h urine protein estimation or the albumin creatinine ratio (i.e., urinary albumin excretion of ≥300 μg/mg of creatinine).[17]
Neuropathy
The diagnosis of neuropathy was based on symptoms and on clinical examination using a 128 Hz tuning fork, a Semmes Weinstein 10 g monofilament and a biothesiometer. Vibratory perception threshold (VPT) of the great toes was measured in a standardized manner by a single observer and neuropathy was diagnosed if the mean VPT was ≥20 V.[18]
Ischemic heart disease (IHD) was diagnosed based on a treadmill test or coronary angiogram in patients who had an abnormal baseline resting electrocardiogram or a history of physician treated IHD.
Peripheral vascular disease (PVD) was diagnosed clinically based on the history of claudication or the absence of palpable pulsations of the dorsalis pedis and or the posterior tibial artery during the foot examination. This was confirmed by an ankle-brachial index value ≤0.9 or >1.3 or on Doppler duplex imaging.[11]
Cerebrovascular accident (CVA) was diagnosed based on history, clinical examination or history of physician treated CVA/previous computed tomography/magnetic resonance imaging records.
Statistical analysis
The statistical analysis was carried out using Microsoft Excel and results on continuous measurements have been presented as mean ± standard deviation and results on categorical measurements have been presented in percentages (%).
RESULTS
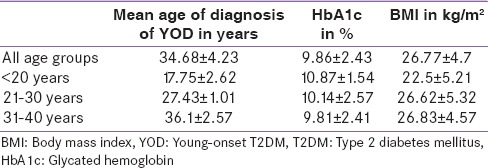
Of the 1500 patients, 74% were men. The mean age was 34.68 ± 4.23 years and 84% of the patients were aged between 31 and 40 years. The mean glycated hemoglobin (HbA1c) at the time of diagnosis was 9.86 ± 2.43% and the mean BMI was 26.77 ± 4.7 kg/m2. The mean age, HbA1c, BMI in the study population and across each decade are shown in Table 1.
Table 1.
Mean age, HbA1c, and BMI
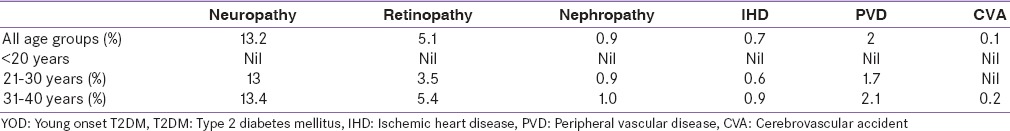
Diabetic neuropathy, retinopathy, and nephropathy were seen in 13.2%, 5.1%, and 0.9% of the patients, respectively. Mild to moderate nonproliferative diabetic retinopathy (NPDR) was present in 4.5% of the patients and 0.5% had severe NPDR. 0.7% had associated maculopathy. None of the patients had proliferative retinopathy, vitreous hemorrhage, or retinal detachment. Macrovascular complications such as IHD, PVD, and CVA were presented in 0.67%, 2%, and 0.1%, respectively. This distribution across each decade is tabulated in Table 2.
Table 2.
Micro and macrovascular complications in patients with YOD
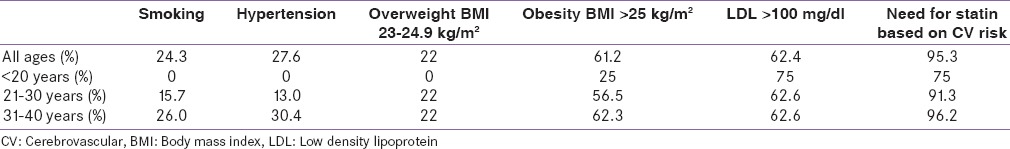
Data on the CV risk factors such as smoking, hypertension, dyslipidemia, and BMI >23 kg/m2 across each decade are tabulated in Table 3. The presence of CV risk factors and the application of current guidelines[15] called for statin initiation in 95.33% of patients.
Table 3.
CV risk factors across each decade
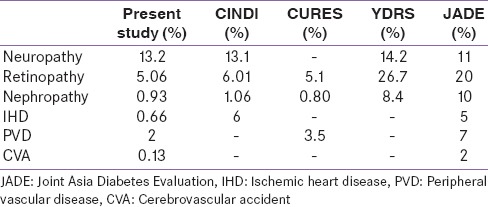
The micro and macrovascular complications observed in this study and the prevalence rates in CINDI, CURES, YDRS, and Joint Asia Diabetes Evaluation (JADE) are depicted in Table 4.
Table 4.
Micro and macrovascular complications at the time of diagnosis of type 2 diabetes
DISCUSSION
Type 2 diabetes is a major cause for morbidity and death. The global prevalence is on the rise and only one out of every two individuals with diabetes is aware that they have diabetes. The recent Indian study shows that 50% of the population is aware of a condition called diabetes.[19] Patients remain undiagnosed as they are asymptomatic for long periods of time. Diagnosis of diabetes is important as it is a major public health problem and adequate control of hyperglycemic and CV risk factors can prevent long-term complications.[20,21,22,23] Macro and microvascular complications may be present at the time of diagnosis of diabetes due to the insidious nature of the disease. Screening for complications at the time of diagnosis of diabetes is crucial. If present, the progression of these complications can be slowed by aggressive control of hypertension, dyslipidemia, glycemic control, use of angiotensin converting enzyme inhibitors, or angiotensin receptor blockers.[24,25,26]
Asian Indians are known to develop T2DM at a younger age and at a lower BMI.[3] Data from CINDI indicates that 46%, i.e., almost half of the patients with type 2 diabetes are diagnosed under the age of 40 years in India.[8] Estimates of prevalence across Asia from the JADE Program report that 20%, i.e. nearly one in every five clinic patients have YOD.[2]
A younger age of onset implies that patients will need to bear the burden of diabetes for a longer period of time. This in addition to suboptimal control of hyperglycemia and CV risk factors puts them at a greater risk for the development of complications.[2,4,5] A recent study from clinic population shows that patients with type 2 diabetes with regular follow-up was associated with significantly lower glycemic burden and lower incidence of retinopathy and nephropathy.[27]
The extent of complications and presence of CV risk factors at the time of diagnosis of type 2 Diabetes in India has been reported in several studies such as CURES, YDRS, and CINDI. A subgroup analysis of the complications across each decade in patients with YOD is limited. This prevalence of neuropathy, retinopathy, and nephropathy at the time of diagnosis is similar to the observations in CINDI, YDRS, and CURES.[8,9,10,28] The JADE cohort included all patients with newly diagnosed and known YOD, irrespective of the duration of diabetes. Higher prevalence rates of micro and macrovascular complications have been reported in JADE.[2] This only further reiterates the value of screening for complications at the time of diagnosis of diabetes even in young patients, as recognition and aggressive treatment of complications and their risk factors can delay progression of these complications.
This study also demonstrates that CV risk factors are highly prevalent even in young patients with type 2 diabetes. One in every four patients was a smoker, one in three had hypertension, two out of three had dyslipidemia, and four out of five patients had a BMI >23 kg/m2. An increase in the CV risk factors was observed as the age advanced across each decade. Dyslipidemia was present even in patients <20 years and the prevalence of all the CV risk factors was much higher beyond the age of 20. The prevalence rates between the third and fourth decade were very similar. The rise in CV risk at an early age highlights the importance of screening for risk factors in all young adults. Similar observations have been reported in JADE.[2]
In this study, 62% of patients with YOD had dyslipidemia, i.e., an LDL >100 mg/dl. On applying the current guidelines to clinical practice, the percentage of patients requiring CV risk reduction with statin, increases from 62% to 95.33%. This implies that nearly all patients, even those under the age of 40 years in India, are at a high risk of CV events and require lipid lowering therapy in the form of statins to ameliorate that risk.
This study demonstrates that there is a large group of patients with YOD at risk for CV events. This study underlines the importance of screening all patients with type 2 diabetes for CV risk factors and complications of diabetes at the time of diagnosis.
The Asian Indian phenotype supplemented by an imperfect lifestyle increased the burden of YOD. Identification and optimal treatment of all CV risk factors in addition to glycemic control in this vulnerable population are important in improving the quality and quantity of life.
The strengths of the study lie in the multi centric design and thorough evaluation for diabetes complications. Limitations include male preponderance among the participants that could have resulted in the high proportion of subjects reporting smoking. Furthermore, as the study population comprised patients attending private diabetes clinics, the middle, and upper socioeconomic classes are likely to be overrepresented.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
Authors sincerely acknowledge the contributions of Dr. V Mohan, Dr. Ranjit Unnikrishnan, Dr. Sanjay Reddy, Dr. Sarita Bajaj, Dr. Jalal Ahmed and Dr. Jayanth Panda.
REFERENCES
- 1.Anjana RM, Pradeepa R, Deepa M, Datta M, Sudha V, Unnikrishnan R, et al. Prevalence of diabetes and prediabetes (impaired fasting glucose and/or impaired glucose tolerance) in urban and rural India: Phase I results of the Indian Council of Medical Research-India Diabetes (ICMR-INDIAB) study. Diabetologia. 2011;54:3022–7. doi: 10.1007/s00125-011-2291-5. [DOI] [PubMed] [Google Scholar]
- 2.Yeung RO, Zhang Y, Luk A, Yang W, Sobrepena L, Yoon KH, et al. Metabolic profiles and treatment gaps in young-onset type 2 diabetes in Asia (the JADE program): A cross-sectional study of a prospective cohort. Lancet Diabetes Endocrinol. 2014;2:935–43. doi: 10.1016/S2213-8587(14)70137-8. [DOI] [PubMed] [Google Scholar]
- 3.Raji A, Seely EW, Arky RA, Simonson DC. Body fat distribution and insulin resistance in healthy Asian Indians and Caucasians. J Clin Endocrinol Metab. 2001;86:5366–71. doi: 10.1210/jcem.86.11.7992. [DOI] [PubMed] [Google Scholar]
- 4.Song SH, Gray TA. Early intensive cardiovascular risk management in young people with type 2 diabetes. Diabetes Res Clin Pract. 2011;92:e70–2. doi: 10.1016/j.diabres.2011.02.027. [DOI] [PubMed] [Google Scholar]
- 5.Chuang LM, Soegondo S, Soewondo P, Young-Seol K, Mohamed M, Dalisay E, et al. Comparisons of the outcomes on control, type of management and complications status in early onset and late onset type 2 diabetes in Asia. Diabetes Res Clin Pract. 2006;71:146–55. doi: 10.1016/j.diabres.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 6.Constantino MI, Molyneaux L, Limacher-Gisler F, Al-Saeed A, Luo C, Wu T, et al. Long-term complications and mortality in young-onset diabetes: Type 2 diabetes is more hazardous and lethal than type 1 diabetes. Diabetes Care. 2013;36:3863–9. doi: 10.2337/dc12-2455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ramachandran A, Ma RC, Snehalatha C. Diabetes in Asia. Lancet. 2010;375:408–18. doi: 10.1016/S0140-6736(09)60937-5. [DOI] [PubMed] [Google Scholar]
- 8.Sosale A, Prasanna Kumar KM, Sadikot SM, Nigam A, Bajaj S, Zargar AH, et al. Chronic complications in newly diagnosed patients with type 2 diabetes mellitus in India. Indian J Endocrinol Metab. 2014;18:355–60. doi: 10.4103/2230-8210.131184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rema M, Premkumar S, Anitha B, Deepa R, Pradeepa R, Mohan V. Prevalence of diabetic retinopathy in urban India: The Chennai urban, rural epidemiology study (CURES) eye study, I. Invest Ophthalmol Vis Sci. 2005;46:2328–33. doi: 10.1167/iovs.05-0019. [DOI] [PubMed] [Google Scholar]
- 10.Unnikrishnan RI, Rema M, Pradeepa R, Deepa M, Shanthirani CS, Deepa R, et al. Prevalence and risk factors of diabetic nephropathy in an urban South Indian population: The Chennai urban, rural epidemiology study (CURES 45) Diabetes Care. 2007;30:2019–24. doi: 10.2337/dc06-2554. [DOI] [PubMed] [Google Scholar]
- 11.Premalatha G, Shanthirani S, Deepa R, Markovitz J, Mohan V. Prevalence and risk factors of peripheral vascular disease in a selected South Indian population: The Chennai urban population study. Diabetes Care. 2000;23:1295–300. doi: 10.2337/diacare.23.9.1295. [DOI] [PubMed] [Google Scholar]
- 12.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(Suppl 1):S62–9. doi: 10.2337/dc10-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization. The Asia Pacific Perspective. Redefining Obesity and its Treatment. Published by Health Commission Australia Pty Limited on behalf of the Steering Committee: World Health Organization, International Association for the study of Obesity and International Obesity Task Force. 2000 [Google Scholar]
- 14.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: The JNC 7 report. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 15.American Diabetes Association Standards of Medical Care. (8) Cardiovascular disease and risk management. Diabetes Care. 2015;38:S49. doi: 10.2337/dc15-S011. [DOI] [PubMed] [Google Scholar]
- 16.Grading diabetic retinopathy from stereoscopic color fundus photographs – An extension of the modified airlie house classification. ETDRS report number 10. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology. 1991;98(5 Suppl):786–806. [PubMed] [Google Scholar]
- 17.Pradeepa R, Anjana RM, Unnikrishnan R, Ganesan A, Mohan V, Rema M. Risk factors for microvascular complications of diabetes among South Indian subjects with type 2 diabetes – The Chennai urban rural epidemiology study (CURES) eye study-5. Diabetes Technol Ther. 2010;12:755–61. doi: 10.1089/dia.2010.0069. [DOI] [PubMed] [Google Scholar]
- 18.Pradeepa R, Rema M, Vignesh J, Deepa M, Deepa R, Mohan V. Prevalence and risk factors for diabetic neuropathy in an urban South Indian population: The Chennai urban, rural epidemiology study (CURES-55) Diabet Med. 2008;25:407–12. doi: 10.1111/j.1464-5491.2008.02397.x. [DOI] [PubMed] [Google Scholar]
- 19.Deepa M, Bhansali A, Anjana RM, Pradeepa R, Joshi SR, Joshi PP, et al. Knowledge and awareness of diabetes in urban and rural India: The Indian Council of Medical Research India Diabetes study (Phase I): Indian Council of Medical Research India Diabetes 4. Indian J Endocrinol Metab. 2014;18:379–85. doi: 10.4103/2230-8210.131191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Intensive blood. glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352:837–53. [PubMed] [Google Scholar]
- 21.UK Prospective Diabetes Study. XII: Differences between Asian, Afro-Caribbean and white Caucasian type 2 diabetic patients at diagnosis of diabetes. UK Prospective Diabetes Study Group. Diabet Med. 1994;11:670–7. [PubMed] [Google Scholar]
- 22.Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. UK Prospective Diabetes Study Group. BMJ. 1998;317:703–13. [PMC free article] [PubMed] [Google Scholar]
- 23.Sosale B, Reddy Y, Nagbhushana MV, Sosale A, Jude EB. Peripheral arterial disease in patients with type 2 diabetes mellitus in South India: The urban vs. rural divide. J Acad Med Sci. 2012;2:105–9. [Google Scholar]
- 24.Lewis EJ, Hunsicker LG, Clarke WR, Berl T, Pohl MA, Lewis JB, et al. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med. 2001;345:851–60. doi: 10.1056/NEJMoa011303. [DOI] [PubMed] [Google Scholar]
- 25.Brenner BM, Cooper ME, de Zeeuw D, Keane WF, Mitch WE, Parving HH, et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. NEngl J Med. 2001;345:861–9. doi: 10.1056/NEJMoa011161. [DOI] [PubMed] [Google Scholar]
- 26.Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, et al. National Kidney Foundation practice guidelines for chronic kidney disease: Evaluation, classification, and stratification. Ann Intern Med. 2003;139:137–47. doi: 10.7326/0003-4819-139-2-200307150-00013. [DOI] [PubMed] [Google Scholar]
- 27.Anjana RM, Shanthirani CS, Unnikrishnan R, Mugilan P, Amutha A, Nair HD, et al. Regularity of follow-up, glycemic burden, and risk of microvascular complications in patients with type 2 diabetes: A 9-year follow-up study. Acta Diabetol. 2015;52:601–9. doi: 10.1007/s00592-014-0701-0. [DOI] [PubMed] [Google Scholar]
- 28.Amutha A, Datta M, Unnikrishnan R, Anjana RM, Mohan V. Clinical profile and complications of childhood-and adolescent-onset type 2 diabetes seen at a diabetes center in south India. Diabetes Technol Ther. 2012;14:497–504. doi: 10.1089/dia.2011.0283. [DOI] [PubMed] [Google Scholar]


