Abstract
Context:
There is paucity of scientific data from India on gender identity disorders (GIDs) or gender dysphoria (GD).
Aims:
To study the clinical, biochemical profile, personality characteristics and family support of GID subjects.
Settings and Design:
A retrospective and cross-sectional study at an endocrine referral center in Kolkata in Eastern India between 2010 and 2015.
Subjects and Methods:
Seventy-three GID subjects who presented to the center were included in the study. Clinical, biochemical profile, personality characteristics (cross-dressing), and family support were investigated. The protocol was presented to the Ethics Committee who felt that given the retrospective nature of the study, informed consent could be dispensed with. GD was diagnosed by Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition).
Statistical Analysis Used:
Unpaired t-test has been used to find the significance of study parameters between two groups of patients. Chi-square/Fisher Exact test has been used to find the significance of study parameters on categorical scale between two groups.
Results:
Out of the total 73 patients, 55 (75.34%) patients were male-to-female and remaining 18 (24.66%) were female-to-male. Around 11% of GD subjects practiced cross-dressing. In spite of median age of onset of GD was 9 years, the mean age of GD at presentation was quite late at 25.77 ± 6.25 years due to lack of social and informative support. It is difficult for transgender to express their sexual identity in family or in society as only 10.96% of our GD subjects had family support, leading to delayed presentation and delayed endocrine consultation. This delayed endocrine consultation have accounted for a significant proportion of GD subjects having unplanned and ill-timed castration (16.36%) or mastectomy (16.67%) even by nonmedically qualified person (66.7% of castrated subjects). All GD subjects had normal thyroid stimulating hormone, testosterone, estradiol, and karyotype concordant with their biological sex. No significant differences were demonstrated between any of the studied parameters namely age at presentation, onset-age of GD, hormone profile, family support, and cross-dressing preferences.
Conclusions:
Social taboo and lack of informative, family support leads to delayed medical consultation and have accounted for complexities in presentation indicating a huge need of awareness programs in our country. Social and informative support can be improved by awareness programs, which might lead to an early endocrine evaluation and proper treatment with improved outcomes.
Keywords: Cross-dressing, family support, female-to-male transsexuals, gender identity disorder, India, male-to-female transsexuals
INTRODUCTION
Gender identity is a person's intrinsic sense of self as male, female, or an alternate gender. Most persons have concordance between the natal gender and the gender identity; however, some have a disharmonious state between their natal gender and gender identity leading to a distress called gender dysphoria (GD). The last decade has witnessed a significant rise in gender variant persons looking for care at gender clinics across the world.[1] This surge in seeking assistance may be ascribed to multiple reasons being exposure to information about transgender available in the internet, more access to transgender characters in the social media and greater receptivity by the family members and peers with regard to one's gender identity crisis.[2]
SUBJECTS AND METHODS
This was a retrospective and cross-sectional study of 73 gender identity disorder (GID) subjects, who presented to a single endocrine referral center in Kolkata in Eastern India between 2010 and 2015. The protocol was presented to the Ethics Committee who felt that given the retrospective nature of the study, informed consent could be dispensed with. GD was diagnosed by Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition) (DSM-IV). Descriptive statistical analysis was carried out in this study. Results of continuous measurements were presented as mean ± standard deviation and results of categorical measurements were presented in number (%). Unpaired t-test has been used to find the significance of study parameters between three or more groups of patients. Chi-square/Fisher exact test has been used to find the significance of study parameters on categorical scale between two groups. Significance was assessed at the 5% level. The statistical software namely SAS (Statistical Analysis System) version 9.2 for windows, (SAS Institute Inc. Cary, NC, USA). was used for the analysis of the data and Microsoft Word version 2010 and Microsoft Excel version 2010 were used to generate graphs, tables.
RESULTS
Seventy-three gender identity patients as diagnosed by DSM-IV aged 13–42. The baseline demographic and descriptive characteristics of the gender variant subjects are outlined in Table 1. The mean age of the GID patients was found to be 25.77 ± 6.25 years, age range was 13–42 years. Out of the total 73 patients, 55 (75.34%) patients were male-to-female (MTF) and remaining 18 (24.66%) were female-to-male (FTM). The median age of onset of GD was 9 years, ranging from 7 to 11 years. All had normal karyotype according to their biological sex. There was no significant difference with regard to age of presentation, onset-age of GD, hormone profile, family support, cross-dressing preferences free thyroxine (FT4) levels, thyroid stimulating hormone (TSH) levels, and fasting plasma glucose between the FTM and MTF subjects [Table 2]. Table 3 demonstrates the testosterone and estradiol levels in the respective normal ranges of the FTM and MTF subjects.
Table 1.
Baseline characteristics of the study sample
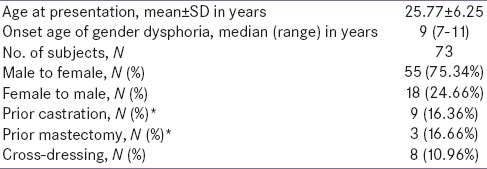
Table 2.
Demographic and basic descriptive characteristics of gender variant study population segregated by FTM and MTF cohorts
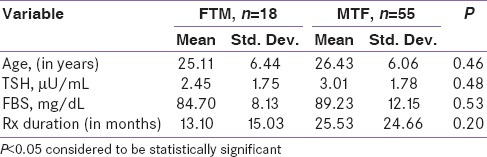
Table 3.
Gonadal hormone profile of the gender variant study population
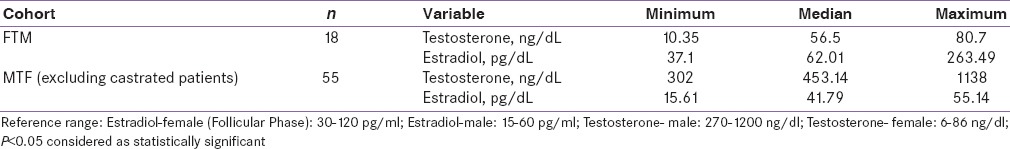
Table 4 shows that out of 18 subjects who chose to transform from FTM, only three (16.67%) had support from their family (first degree relatives), whereas 15 (83.33%) had faced resistance from their family members. Similarly, only five (9.26%) out of 54 subjects from the MTF cohort had support from their family and the remaining 49 (90.74%) subjects had opposition from their family. If we compare the family support between the two groups of GD subjects, there is no statistically significant difference in terms of support from their family members, P = 0.40.
Table 4.
Family support
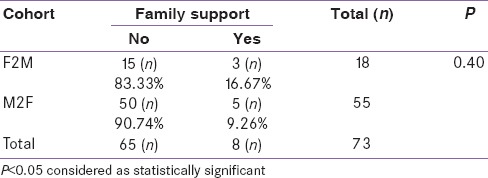
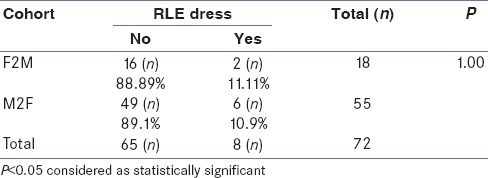
Table 5 presents that out of 18 subjects who chose to transform from FTM, only two (11.11%) had a cross-dressing preference, whereas 16 (88.89%) were not. Comparatively, only five (9.26%) out of 54 subjects from the MTF cohort used to cross-dress and the remaining 49 (90.74%) subjects were not. If we compare the dressing preference/pattern between the two groups of GID subjects, there is no statistically significant difference in terms of dressing preferences, P = 1.00. Nine (16.36%) out of 55 MTF patients presented to our endocrinology clinic with prior castration. Six (66.67%) out of nine castrated patients underwent castration by nonmedically qualified person. Similarly, three (16.67%) out of 18 FTM subjects also presented to the endocrinology center with prior mastectomy.
Table 5.
Cross-dressing preference
DISCUSSION
Gender variance is an umbrella term describing behaviors, interests, appearance, expression, or an identity of persons who do not conform to culturally defined norms expected of their natal gender.[3] Associated terms include gender nonconforming, gender creative, transgender, gender identity, etc., GID or GD is characterized by a strong and persistent identification with the opposite sex and discomfort with one's own sex.[4] Persons who experience persistent discomfort with their biologic sex or with the gender role of that sex (American Psychiatric Association [APA], 2000) and who display a strong and persistent cross-gender identification can be diagnosed with transsexualism (APA, 1980, 1987; World Health Organization, 1992) or GID(GID; APA, 1994, 2000).[5] In May 2013, the DSM-V replaced the term GID previously found in the (DSM-IV) with the term GD after much complex debate. Many view there placement as a paradigmatic shift toward depathologizing gender variant identity and behavior. The distinctive characteristic defining GD encompasses persistent discomfort with one's gender and a wish to get rid of their sexual characteristics and acquire sexual characteristics of the other gender.[6] Gender identity likely reflects a complex interplay of biological, environmental, and cultural factors.[7,8,9] Transgender is an adjective to describe individuals with an affirmed gender identity different than their physical sex characteristics. Transgender refers to identify people whose gender identity, expression, or behaviors cross or transcend culturally defined categories of gender.[8] FTM denotes to assigned female persons who identify oneself as male. MTF refers to assigned male persons who identify as female.[8] In recent times, India has also witnessed a surge in awareness, social and media activism in GD. However, there is paucity of scientific data from India on GIDs. We have tried to address this by tracing the characteristic features of GD at presentation in endocrine clinic.
Owing to paucity of data from Indian population, the profile and prevalence of gender variant behavior and GD, remains largely unknown. GD is rare, with an estimated worldwide lifetime prevalence of 1:12,900–1:35,000 for MTFs, and from 1:33,000 to 1:100,000 for FTMs[10,11] but much higher rates have been reported in various countries.[12] Few studies from abroad investigating gender variant behavior found that 2–4% of boys and 5–10% of girls behaved as the opposite sex from time-to-time.[13] Another study found that 22.8% of boys and 38.6% of girls exhibited 10 or more different gender atypical behaviors.[13] Thus some previous studies point toward a higher prevalence of FTMs than MTFs both in adult and child populations. However, we had contradictory results in our study subjects with MTF:FTM ratio of 3.05:1. Recently, Karla reported estimated population of 5–6 million eunuchs living in India. The eunuchs are nothing but MTF transsexuals.[14] This increased proportion of MTF transsexual in India represent the outlook of a male dominated society where the female counterpart (FTM) can hardly make their voice heard and present themselves for professional advice and management.
In our study, the mean age of presentation of GD patients was found to be 25.77 ± 6.25 years. This was an extreme delayed endocrine consultation considering the median age of onset of GD was 9 years, ranging from 7 to 11 years. On a cultural perspective India still continue to be very conservative, which means both denying own sexuality and also expressing sexual orientation. Wide spread prejudice means that it can often be difficult for Indian transgender to express their sexual identity in family or in society leading to delayed presentation.
The delay in endocrine consultation may have accounted for as significant proportion (16%) of our GD subjects having prior castration or mastectomy even by nonmedically qualified person. 16.67% of our MTF subjects presented with prior castration among which a two-third proportion of castration were being carried out by nonmedical persons. Our castration data corroborate with the findings of a recently published Indian review article.[14] The author reported eunuchs from India often presents to an endocrinologist with prior crude surgery which includes orchidectomy and partial or complete penectomy.[14] Few authors have identified several ground reasons for self-castration among transsexual woman.[15,16] The major barriers being the out-of-pocket cost for an elective orchiectomy, lack of access to a surgeon willing to perform such operations, waiting times for sex reassignment surgery, and under lying social, psychological and psychiatric conditions. These logical implications giving vent to frustration for self-castration may hold good for preferring castration by nonmedical persons in a developing country like India.[15,16] Richards et al., in their recent review on the impact of bilateral mastectomy in the life of FTMs had concluded bilateral mastectomy indispensable for FTMs to live safely and effectively in their reassigned sex.[17] They further went ahead advocating bilateral mastectomy as a prophylaxis against distress, distress buster and also indispensable for improving quality of life.[17] In our study, we found 16.67% of FTM subjects presented to the endocrinology clinic with prior mastectomy.
Indian transgenders face extreme lack of support (emotional and informational) from family and society. Confronted with their own sense of alienation and confusion, as well as the overwhelmingly negative messages in their home and society, most transgenders learn to suppress their orientation. In our study, only 10.96% of GD subjects (16.63% of the FTM and 9.26% of the MTF) had support from their family members. This may have also accounted for their late endocrine consultation. We had come across many transgenders who had left their family and their birth place in pursuit to establish themselves in the sex of their choice. Bonifacio et al., had mentioned in their paper about the gender variant youth facing a diverse issues that may their affect emotional and psychological well-being leading to posttraumatic stress disorder.[18] Ehrensaft also identified the gender variant youth experiencing variant levels of stigma, social ostracizing, and verbal and physical violence compromising their psychological well-being potentially leading to depression and/or anxiety.[19] A recent study by Roberts et al., found gender variance as a risk factor for going through physical, psychological and sexual abuse.[20]
Researches comparing clinical, biochemical profile and personality characteristics among GD subjects had generated mixed results, with dissimilar patterns for MTF and FTM transsexual subjects.[6] There is paucity of endocrine literature in general and specially from India. In our study, all GD subjects had normal karyotype according to their biological sex. There was no significant difference with regard to age of presentation, onset-age of GD, hormone profile, FT4 levels, TSH levels and fasting plasma glucose between the FTM and MTF subjects. The testosterone and estradiol levels of the FTM and MTF subjects were in the respective normal ranges concordant with their biological sex.
Miyajima et al., had conducted a study in Japan to identify differences in personality traits between MTF and FTM GID subjects. They concluded that high reward dependence and cooperativeness in the FTM and high self-transcendence in the MTF were characteristic of personality traits causing differences in interpersonal relationship and social functioning/adjustment between MTF and FTM cohorts.[21] We also studied and compared the cross-dressing style among the MTF and FTM subjects. 11.11% of the FTM subjects had a cross-dressing preference compared to 9.26% subjects of the MTF cohort with no significant difference between them. A statement from World Professional Association for Transgender Health urges cross-dressing to be considered “as dressing in conformity with core gender identity,” a psychological feature as for any other normal person.
CONCLUSION
We have tried to elaborate the characteristic features of 73 GD subjects at presentation to a tertiary endocrine clinic. Majority (75.34%) of GD subjects were MTF. Probably reflecting a male dominated society. Only 10.96% of our GD subjects had family support contributing to a delayed presentation at a mean age of 25 years in spite of the median age of onset of symptoms at 9 years. All subjects had normal TSH, testosterone, estradiol, and karyotype concordant with their biological sex. At presentation, 10.96% of GD subjects practiced cross-dressing. 16.36% of our MTF subjects had prior castration, 16.67% FTM subjects had prior mastectomy and many of these surgeries were unplanned, ill-timed and done by nonqualified persons. Social taboo and lack of informative, family support leads to delayed medical consultation and have accounted for complexities in presentation indicating a huge need of awareness programs in our country.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.de Vries AL, Cohen-Kettenis PT. Clinical management of gender dysphoria in children and adolescents: The Dutch approach. J Homosex. 2012;59:301–20. doi: 10.1080/00918369.2012.653300. [DOI] [PubMed] [Google Scholar]
- 2.Spack NP, Edwards-Leeper L, Feldman HA, Leibowitz S, Mandel F, Diamond DA, et al. Children and adolescents with gender identity disorder referred to a pediatric medical center. Pediatrics. 2012;129:418–25. doi: 10.1542/peds.2011-0907. [DOI] [PubMed] [Google Scholar]
- 3.Coleman EB, Bockting WO, Botzer M, Cohen-Kettenis P, DeCuypere G, Feldman J, et al. Standards of care for the health of transsexual, transgender and gender non-conforming people, version 6. Int J Transgend. 2001;17:366–433. [Google Scholar]
- 4.4th ed. Washington, DC: American Psychiatric Association; 1994. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- 5.5th ed. Washington, DC: American Psychiatric Association; 2013. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- 6.Hatami M, Ayvazi S. Investigating of personality characteristics (extroversion introversion) and early maladaptive schemas (EMS) in males and females with gender identity disorder (GID) Procedia Soc Behav Sci. 2013;84:1474–80. [Google Scholar]
- 7.Coleman EB, Bockting WO, Botzer M, Cohen-Kettenis P, DeCuypere G, Feldman J, et al. Standards of care for the health of transsexual, transgender and gender non-conforming people, version 7. Int J Transgend. 2011;13:165–232. [Google Scholar]
- 8.Hidalgo MA, Ehrensaft D, Tishelman AC, Clark L, Garofalo R, Rosenthal S, et al. The gender affirmative model: What we know and what we aim to learn. Hum Dev. 2013;56:285–90. [Google Scholar]
- 9.Rosenthal SM. Approach to the patient: Transgender youth: Endocrine considerations. J Clin Endocrinol Metab. 2014;99:4379–89. doi: 10.1210/jc.2014-1919. [DOI] [PubMed] [Google Scholar]
- 10.De Cuypere G, Van Hemelrijck M, Michel A, Carael B, Heylens G, Rubens R, et al. Prevalence and demography of transsexualism in Belgium. Eur Psychiatry. 2007;22:137–41. doi: 10.1016/j.eurpsy.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 11.Gómez-Gil E, Vidal-Hagemeijer A, Salamero M. MMPI-2 characteristics of transsexuals requesting sex reassignment: Comparison of patients in prehormonal and presurgical phases. JPers Assess. 2008;90:368–74. doi: 10.1080/00223890802108022. [DOI] [PubMed] [Google Scholar]
- 12.Zucker KJ, Lawrence AA. Epidemiology of gender identity disorder. Int J Transgend. 2009;11:8–18. [Google Scholar]
- 13.Sandberg DE, Meyer-Bahlburg HF, Ehrhardt AA, Yager TJ. The prevalence of gender-atypical behavior in elementary school children. J Am Acad Child Adolesc Psychiatry. 1993;32:306–14. doi: 10.1097/00004583-199303000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Kalra S. The eunuchs of India: An endocrine eye opener. Indian J Endocrinol Metab. 2012;16:377–80. doi: 10.4103/2230-8210.95676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McGovern SJ. Self-castration in a transsexual. J Accid Emerg Med. 1995;12:57–8. doi: 10.1136/emj.12.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.St Peter M, Trinidad A, IrwigMS Self-castration by a transsexual woman: Financial and psychological costs: A case report. J Sex Med. 2012;9:1216–9. doi: 10.1111/j.1743-6109.2011.02621.x. [DOI] [PubMed] [Google Scholar]
- 17.Richards C, Barrett J. The case for bilateral mastectomy and male chest contouring for the female-to-male transsexual. Ann R Coll Surg Engl. 2013;95:93–5. doi: 10.1308/003588413X13511609957290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bonifacio HJ, Rosenthal SM. Gender variance and dysphoria in children and adolescents. Pediatr Clin North Am. 2015;62:1001–16. doi: 10.1016/j.pcl.2015.04.013. [DOI] [PubMed] [Google Scholar]
- 19.Ehrensaft D. From gender identity disorder to gender identity creativity: True gender self child therapy. J Homosex. 2012;59:337–56. doi: 10.1080/00918369.2012.653303. [DOI] [PubMed] [Google Scholar]
- 20.Roberts AL, Rosario M, Corliss HL, Koenen KC, Austin SB. Childhood gender nonconformity: A risk indicator for childhood abuse and posttraumatic stress in youth. Pediatrics. 2012;129:410–7. doi: 10.1542/peds.2011-1804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miyajima E, Taira N, Koda M, Kondo T. Differences in personality traits between male-to-female and female-to-male gender identity disorder subjects. Psychiatry Res. 2014;220:496–9. doi: 10.1016/j.psychres.2014.07.069. [DOI] [PubMed] [Google Scholar]


