Abstract
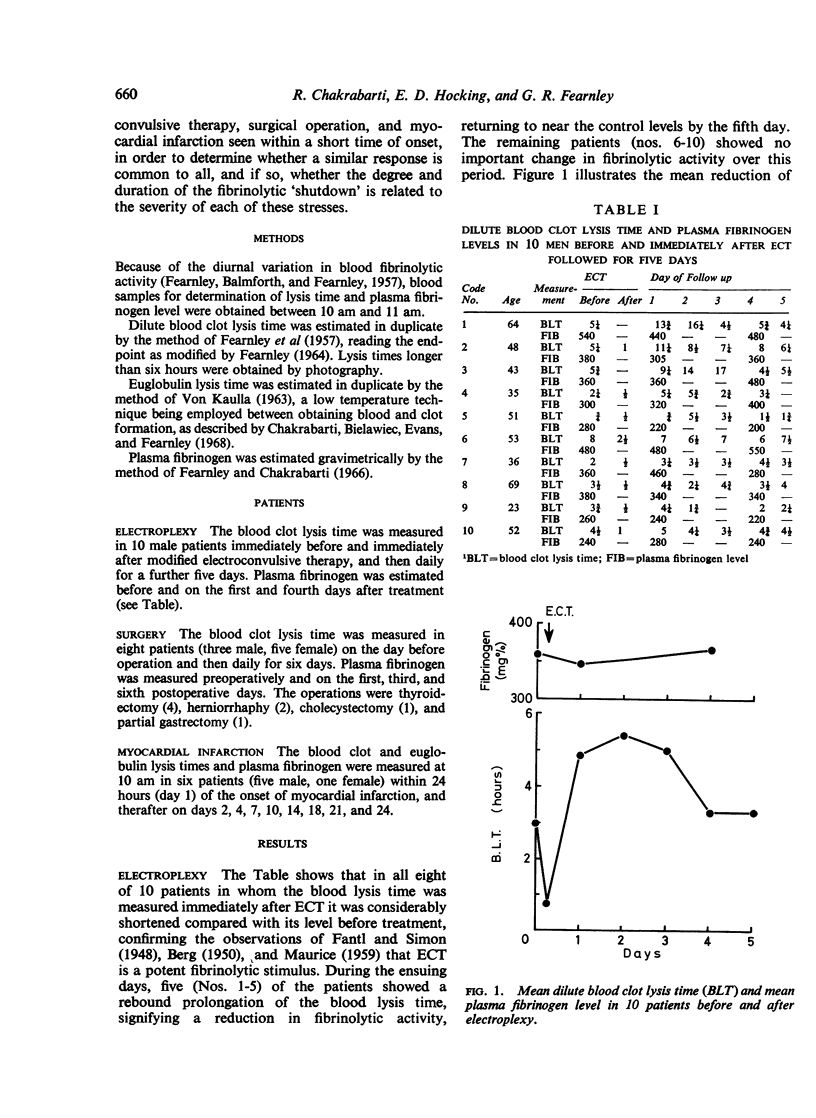
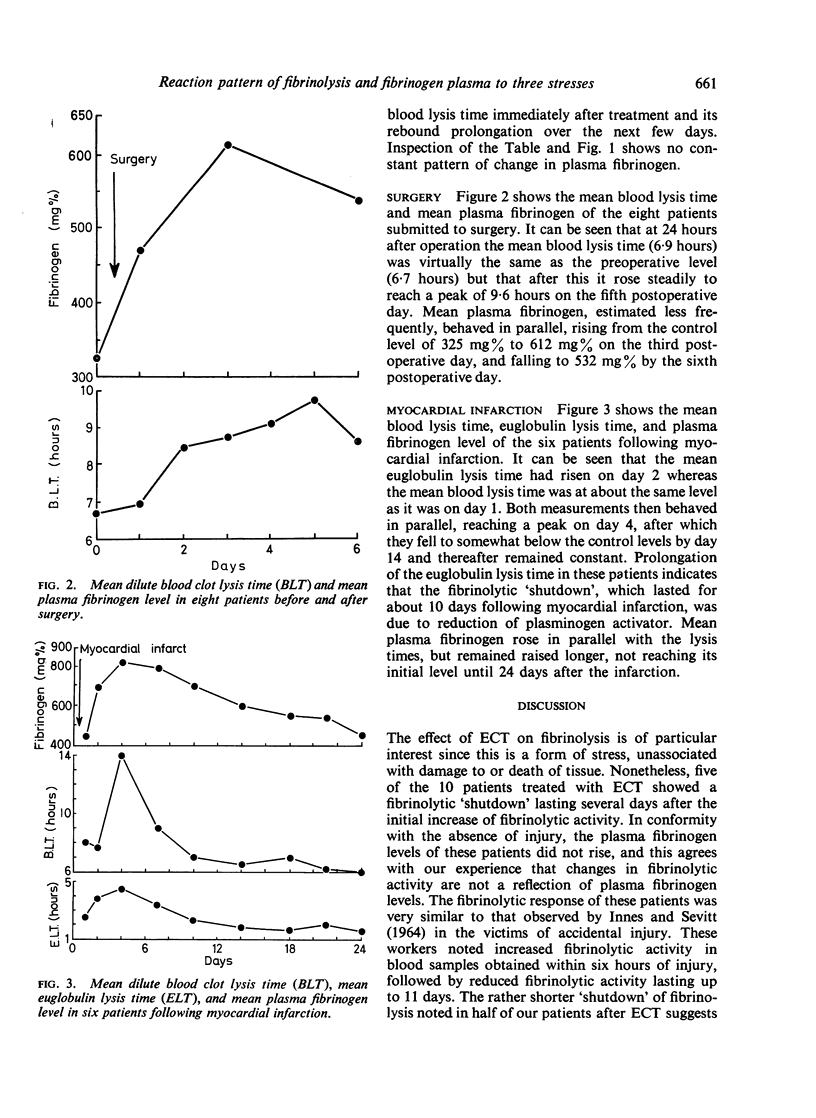
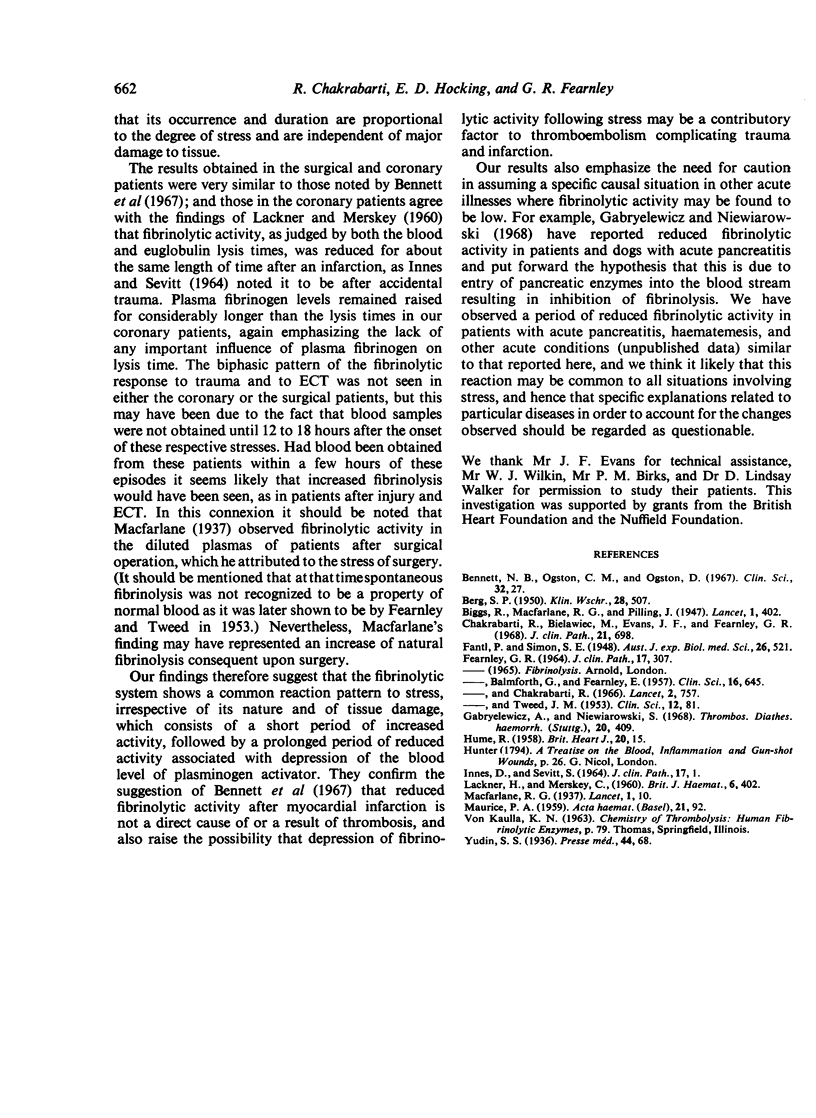
The effects of three types of stress—electroplexy, surgery, and myocardial infarction—on blood fibrinolytic activity and plasma fibrinogen levels were studied in 10, eight, and six patients respectively. The fibrinolytic response to electroplexy consisted of an initial short increase followed in half the patients by reduced fibrinolytic activity lasting two to four days. After surgery and myocardial infarction normal fibrinolytic activity was followed by a period of reduced activity; the timing of the measurements on these patients may have precluded recognition of an initial increase in fibrinolysis similar to that following electroplexy. The fibrinolytic `shutdown' which lasted for about 10 days in the coronary patients was evidently due to reduction of plasminogen activator, as judged by prolongation of the euglobulin lysis times as well as of the blood clot lysis times. Plasma fibrinogen levels rose in the surgical and coronary patients but not in the patients given electroplexy which indicates that fibrinolytic activity changes independently of plasma fibrinogen level. The results suggest that the fibrinolytic system exhibits a common reaction pattern to stress, irrespective of its nature and of tissue damage. They call for caution in assuming a specific causal association in acute diseases such as pancreatitis and haematemesis where similar fibrinolytic changes may be encountered.
Full text
PDF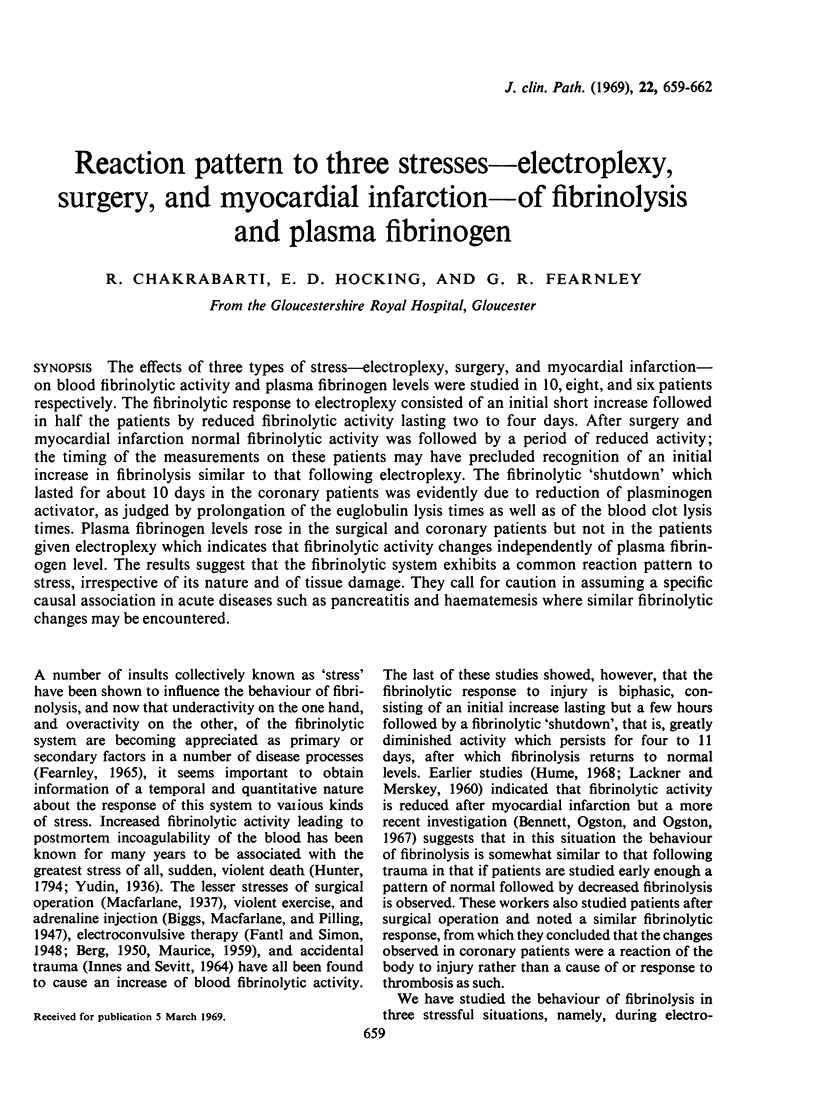
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BERG S. P. Elektroschock und Fibrinolyse. Klin Wochenschr. 1950 Aug 1;28(29-30):507–508. doi: 10.1007/BF01486303. [DOI] [PubMed] [Google Scholar]
- Bennett N. B., Ogston C. M., Ogston D. Studies on the blood fibrinolytic enzyme system following acute myocardial infarction. Clin Sci. 1967 Feb;32(1):27–37. [PubMed] [Google Scholar]
- Chakrabarti R., Bielawiec M., Evans J. F., Fearnley G. R. Methodological study and a recommended technique for determining the euglobulin lysis time. J Clin Pathol. 1968 Nov;21(6):698–701. doi: 10.1136/jcp.21.6.698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FEARNLEY G. R., BALMFORTH G., FEARNLEY E. Evidence of a diurnal fibrinolytic rhythm; with a simple method of measuring natural fibrinolysis. Clin Sci. 1957 Nov;16(4):645–650. [PubMed] [Google Scholar]
- FEARNLEY G. R. MEASUREMENT OF SPONTANEOUS FIBRINOLYTIC ACTIVITY. J Clin Pathol. 1964 May;17:307–309. doi: 10.1136/jcp.17.3.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fearnley G. R., Chakrabarti R. Fibrinolytic treatment of rheumatoid arthritis with phenformin plus ethyloestrenol. Lancet. 1966 Oct 8;2(7467):757–761. doi: 10.1016/s0140-6736(66)90360-6. [DOI] [PubMed] [Google Scholar]
- Gabryelewicz A., Niewiarowski S. Activation of blood clotting and inhibition of fibrinolysis in acute pancreatitis. Thromb Diath Haemorrh. 1968 Dec 31;20(3):409–414. [PubMed] [Google Scholar]
- HUME R. Fibrinolysis in myocardial infarction. Br Heart J. 1958 Jan;20(1):15–20. doi: 10.1136/hrt.20.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- INNES D., SEVITT S. COAGULATION AND FIBRINOLYSIS IN INJURED PATIENTS. J Clin Pathol. 1964 Jan;17:1–13. doi: 10.1136/jcp.17.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LACKNER H., MERSKEY C. Variation in fibrinolytic activity after acute myocardial infarction and after the administration of oral anticoagulant drugs and intravenous heparin. Br J Haematol. 1960 Oct;6:402–413. doi: 10.1111/j.1365-2141.1960.tb06259.x. [DOI] [PubMed] [Google Scholar]
- MAURICE P. A. Etude de deux variétés de fibrinolyse produites respectivement par injection d'un pyrogène et par électrochoc. Acta Haematol. 1959 Feb;21(2):92–101. doi: 10.1159/000205661. [DOI] [PubMed] [Google Scholar]



