Abstract
Background
The more effective treatment for severe obesity is bariatric surgery. Gastric bypass is a surgical technique used worldwide; however, as well as other techniques; it has postoperative risks, including nutrient deficiency.
Aim
To determine the amounts of dietary iron, calcium, vitamin D and vitamin B12 ingested by patients of a public hospital one year after gastric bypass, and compare with the recommendations of the Recommended Dietary Allowances.
Methods
This was a transverse descriptive study and the sample consisted of 36 women, with at least one year of gastric bypass. Data collected included sociodemographic, anthropometric and diet variables. Dietetic information was collected through a validated food frequency questionnaire. Ingestion of iron, calcium, vitamin D and vitamina B12 was evaluated in comparison with the Recommended Dietary Allowances, as well as correlation of micronutrient ingestion with time of surgery.
Results
There was inadequate consumption of iron, calcium and vitamin D. The vitamin B12 intake was considered adequate. There was statistically significant positive correlation between the time of surgery and the ingestion of iron, vitamin B12 and vitamin D.
Conclusion
The intake of iron, calcium and vitamin D of women one year after gastric bypass was inadequate, emphasizing the importance of multiprofessional monitoring postoperatively to prevent nutrient deficiencies.
Keywords: Gastric bypass, Diet, Micronutrients
Abstract
Racional
O tratamento considerado mais eficiente para o grau severo da obesidade é a cirurgia bariátrica. O bypass gástrico é a técnica cirúrgica mais utilizada no mundo; porém, assim como as outras técnicas, oferece riscos no pós-operatório, incluindo a deficiência de nutrientes.
Objetivo
Determinar as quantidades de ferro, cálcio, vitamina D e vitamina B12 dietéticas ingeridas por pacientes atendidos em um hospital público após um ano de bypass gástrico, e comparar com as recomendações da Recommended Dietary Allowances.
Métodos
Estudo transversal descritivo com amostra composta por 36 mulheres com mais de um ano de bypass gástrico. Foram coletados dados sociodemográficos, antropométricos e alimentares. Estes últimos foram realizados por meio de Questionário de Frequência Alimentar validado. Foi feita comparação da ingestão de ferro, cálcio, vitamina D e vitamina B12 com as Recommended Dietary Allowances, assim como a correlação do tempo de pós-operatório com o consumo desses micronutrientes.
Resultados
Houve inadequação no consumo de ferro, cálcio e vitamina D. A ingestão de vitamina B12 mostrou-se adequada. Foi encontrada correlação positiva estatisticamente significativa entre o tempo de operação e o consumo de ferro, vitamina B12 e vitamina D.
Conclusão
A ingestão de ferro, cálcio e vitamina D de mulheres um ano após o bypass gástrico foi inadequada, enfatizando a importância do acompanhamento multiprofissional no pós-operatório para prevenção de carências de nutrientes.
INTRODUCTION
Obesity is a chronic disease that occurs through excessive accumulation of adipose tissue that may or may not be associated with other diseases, such as hypertension, type 2 diabetes mellitus, obstructive sleep apnea, dyslipidemia28. The frequency of obesity has been increasing in Brazil over the past decades. Currently, 17,4% of the adult Brazilian population have some degree of this disease and the Federal District has a frequency of 14%7.
With the epidemic of obesity, different treatments have emerged, which have been perfected over time. Among them, bariatric surgery has proven to be more effective in the long term for morbid obesity5,8. The gastric bypass or Fobi-Capella tecnique is the most common surgical technique performed in Brazil and worldwide. That is because it presents a low morbidity and mortality, leads to adequate weight loss and resolution of comorbidities without major nutritional compromise or gastrointestinal symptoms5. This technique consists of the formation of a proximal gastric pouch of 30-60 ml, associated with intestinal bypass of 100-150 cm excluding the duodenum from the food transit. Regarding postoperative complications, the patient may develop, in the long term, deficiencies of some macro and micronutrients and may also have episodes of vomiting, diarrhea and dumping syndrome in the immediate postoperative period.
Pre and postoperative monitoring, by a multidisciplinary team, are necessary so as to avoid nutritional deficiencies, including in the late postoperative period5.
In general, in mixed procedures like gastric bypass, there is a significant decrease in food intake over time, which can lead to nutrient deficiency, if the diet is not adequate8. Not only the reduction of food intake is responsible for the risk of deficiencies, but food intolerances may also occur. Thus, the decline in consumption of major food sources may lead to lack of nutrients. In the bypass surgery, in which occurs the exclusion of duodenal transit, nutrients absorbed in this specific intestinal portion, such as iron, calcium, vitamin D and vitamin B12, have their absorption reduced5. Over the years, the body stores of micro-nutrients are depleted leading to these deficiencies; therefore, it becomes necessary to have periodic monitoring after the operation, through physical and biochemical exams5. It is noteworthy that possible preoperative deficiencies should also be investigated in order to be corrected beforehand. This ensures that deficiencies developed before the surgery are not confused with post-operative complications5.
Food intake can be evaluated by means of a few methods such as the dietary 24-hour recall, the three-day food record and the Food Frequency Questionnaire20. However, it is known that any assessment method has limitations in use and therefore is not able to quantify the precise dietary intake20. The Food Frequency Questionnaire is a dietary survey commonly used in the assessment of micronutrient intake and its relationship with the emergence of non-communicable chronic diseases, since it is able to evaluate a relatively long period of time9. There are flaws inherent to this instrument, for example, the bias of memory which can affect the accuracy of the information collected10.
Recommendations for intake of macro and micronutrients currently most used are the Recommended Dietary Allowances (RDA), drawn from the evaluation of the average consumption of the healthy American population increased by two standard deviations, covering the needs 97-98% of Americans14. However, as previously mentioned, the recommendations apply only to healthy groups. For patients undergoing bariatric surgery, there are studies claiming that micronutrient intake according to the RDA is not enough to meet the needs of these individuals5. However, there are no specific recommendations for this type of population.
Nutrient supplementation after surgery for obesity is required in all surgery tecniques5. In 2008, the American Association of Endocrinologists, the Obesity Society and the American Society for Metabolic and Bariatric Surgery developed guidelines for clinical practice for the perioperative period on nutrition, metabolic and nonsurgical support of bariatric patients. These guidelines were updated in 2013, containing 74 recommendations for patients in the preoperative and postoperative periods of bariatric surgery1. In cases of gastric bypass, there must be special care with respect to possible deficiencies of iron, calcium, vitamin D, vitamin B1, vitamin B12 and folato5.
The present study aimed to determine the amounts of iron, calcium, vitamin D and vitamin B12 ingested by women attending a public hospital, one year after gastric bypass, and compare with the recommendations of RDA14.
METHODS
The project was presented and approved by the Ethics Committee on Human Research of the State Department of Health of the Federal District of Brazil. All patients who agreed to participate read and signed the consent form.
This is a descriptive cross-sectional study conducted in an outpatient nutrition high complexity assistance unit of patients with morbid obesity in a regional hospital. Patients over 12 months of surgery, who had postoperative nutritional appointment scheduled at the clinic in the period from February to July 2013, were invited to participate in the study.
During the nutritional appointment, the nutritionist responsible for the study applied a questionnaire to collect sociodemographic, anthropometric and food consumption data. The questionnaire presented data on gender, age, education and occupation. Weight and height were measured to calculate BMI and percent loss of excess weight (%LEW). Weight was measured on a digital scale with a maximum capacity of 300 kg. The height was obtained by Sanny stadiometer Personal Caprice®. BMI was calculated using the formula: weight/height². The %LEW was obtained from the formula: weight loss after surgery/overweight x 100. Excess weight was calculated by subtracting the weight at the start of preoperative monitoring from ideal weight, established by Metropolitan Life Table18.
To assess the intake of iron, calcium, vitamin B12 and vitamin D, a quantitative Food Frequency Questionnaire was assigned. It is a validated form, proposed by Furlan-Viebig12. The dietary survey in question was validated for quantification of food intake and assessment of micronutrient intake in the development of chronic diseases.
Calculations of micronutrient intake were conducted based on the Brazilian Food Composition Table29, Table for Evaluation of Food Consumption in Domestic Measures22 and Table Food Composition - Support for Nutritional Decision21. The average consumption was found for each individual micronutrient compared with the RDA (1989)14.
The patients were questioned about any complications or gastrointestinal discomfort after eating any food. The question was asked in an open manner so that the patient could report potential difficulties in the consumption of certain foods. These data are listed for further analysis.
To evaluate the distribution of the sample and compare the averages of the data collected, the t-student test was used in Graphpad Instat version 3.0 software. To test associations between the operating time and the consumption of micronutrients, the Pearson correlation was used, considering the significance level below 0.05 (p).
RESULTS
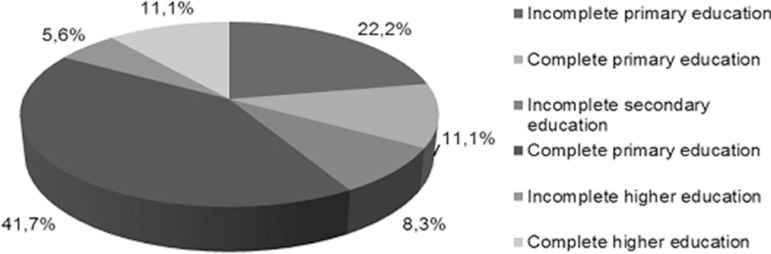
The sample consisted of 36 women. The mean age was 42.8±9.8 years. Regarding education, 41.2% reported having completed high school (Figure 1).
Figure 1.
Distribution of women undergoing gastric bypass according to level of education.
The mean period of operation was 20.1± 3.7 months (14-24); the mean BMI 30.0±5.5 kg/m² and the average PEP of 60.9%±23.2% (from 18.4 to 108.4%).
With respect to dietary micronutrients, the entire sample had inadequate intake of iron, calcium and vitamin D in comparison with the RDA14. On the other hand, vitamin B12 reached 104.2% of the intake adequacy with respect to the same reference values (Table 1).
TABLE 1.
Micronutrient dietary intake adequacy of women undergoing gastric bypass
| Adequacy | |||
|---|---|---|---|
| Iron | 5,5 mg | 18 mg | 30,5% |
| Calcium | 590,3 mg | 1000 mg | 59,0% |
| Vitamin B12 | 2,5 µg | 2,4µg | 104,2% |
| Vitamin D | 0,5 µg | 15 µg | 3,3% |
RDA: Recommended Dietary Allowance. IOM, 19898.
Regarding the time of operation and the consumption of micronutrients, there was a positive correlation between the first parameter and the consumption of vitamin D (r=0.6352, p<0.0001), vitamin B12 (r=0.3586, p= 0.0317) and iron (r=0.3955, p=0.0170). There was no statistically significant correlation between the time of operation and calcium intake (r=-0.1868, p=0.2754).
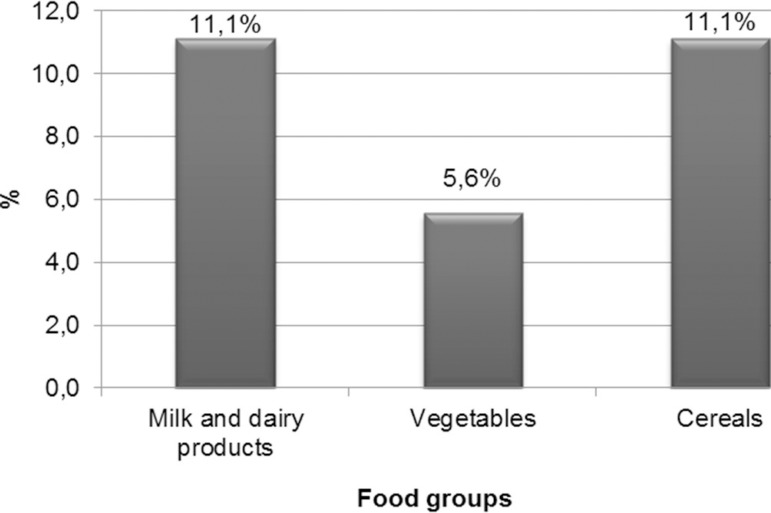
Regarding the dietary data, 27.8% reported some food intolerance. The most reported were milk or dairy products and cereals, with 40% of complaints each. Other foods mentioned were vegetables, with 11.1% of intolerance (Figure 2).
Figure 2.
Prevalence of food intolerance according to food groups in women one year after gastric bypass
DISCUSSION
The profile of patients who undergo bariatric surgery is essentially of women13. This predominance, as found in this study, also occurs throughout the hospital. Although the initial objective of the research was not to assess dietary intake in women, due to the great demand for women's operations during the period of data collection, the sample consisted of only female.
Gastric bypass can be considered successful when, among other factors, the patient reaches %EWL of at least 50%30. The patients in this study achieved an average of 60.9±23.2% of EWL and 27.8% (n=10) did not reach 50%. In general, this sample achieved sufficient weight loss considering the time of operation.
Regarding micronutrients analyzed, the amount of iron ingested through diet alone was far below the recommendations (RDA14) in this period. This may be due to low consumption of its food sources, led by slow digestion inherent to these foods. The iron-rich foods are also rich in protein and fiber, nutrients that take time to digest and slow gastric emptying, which may cause satiety. With the reduction of stomach volume due to the surgical technique, this feeling tends to exacerbate. The decrease in the production of gastric juice (especially hydrochloric acid, essential in optimizing the bioavailability of iron, reducing it from ferrous to ferric form) and the characteristic intestinal bypass in this surgical technique, which isolates the duodenum and early jejunum - absorption sites of this nutrient - are other factors that can contribute to the development of iron deficiency4.
Recent studies showed, similarly, inadequacy in dietary iron intake in patients over one year of surgery. However, the adequacy value of this paper (30.5%) was lower than indicated by these other authors. Moizé et al.19 found inadequacy of 48-79%; Prevedello et al.23 of 71.7%; and Silva et al.27 88.2%. This disparity between these results may be due to differences in the instruments used to collect food intake data. Moizé et al.19 used food diaries of three days, while the last two authors used a 24-hour recall. It is known that inadequate consumption of iron-rich foods in the long run can result in the development of iron deficiency anemia, which manifests through fatigue, irritability, weakness, brittle nails and may lead to more serious consequences if not treated16.
Dietary calcium in the sample also did not meet recommendations, supplying only 59% of daily needs according to RDA. In the same postoperative period, Prevedello et al.23 found 41.7% adequacy, Silva et al.27 and 47.3% Moizé et al.19 85%. The results brought by the cited studies suggest insufficient calcium intake of these patients, although the differences in the results may be due to the different methodologies used. Insufficient dietary calcium intake in this study can be explained by the discomfort that some patients reported during the study after ingestion of milk and its derivatives, since this food group was the cause of most food intolerances. According to Martinez et al.17, lactose intolerance may be responsible for symptoms such as bloating, intestinal cramps, flatulence and diarrhea. It is stated further that these symptoms may occur after gastric bypass or worsen, if there is a low tolerance preoperatively17. Calcium deficiency is multifactorial and can occur by low intake of food sources and also by excluding its site of absorption (duodenum and proximal jejunum) after the operation16. Osteoporosis and secondary hyperparathyroidism are examples of bone disease that may occur after bariatric surgery16. Common manifestations are: brittle teeth, back pain and seizures.
Vitamin D is directly involved in the absorption and metabolism of calcium. Deficiency of this vitamin can occur after bariatric surgery, as the site of absorption (duodenum and proximal jejunum) is excluded from food transit due to the intestinal bypass performed. In addition, the dietary sources of vitamin D are usually not consumed in sufficient amount to supply the metabolic needs even in the preoperative period. The Consumer Expenditure Survey showed that the average intake of Brazilian adults is 3.5 mg for men and 2.9 mg among women15. These numbers are considerably distant from the recommendation, of 15 ug for the adult population14. In the postoperative period of obesity surgery, this deficit in intake remains. Prevedello et al.23 found a 30% adequacy. The results of this study show even greater deficit, as the ingestion comprises only 3.3% of daily needs. Bordallo et al.4 state steatorrhea as a factor that may also contribute to vitamin D deficiency, since the gastric bypass promotes poor absorption of fats and hence can affect the absorption of fat-soluble vitamins.
Vitamin B12 presented different results from other micronutrients in this study, being the only one ingested sufficiently to meet the daily needs (104.2% of RDA14). Blake et al.3 and Prevedello et al.23 showed similar results, in that their samples had more than 100% adequacy of consumption in relation to the recommendations (125% and 158.3% suitability, respectively). In this case, the first study used a food frequency questionnaire to quantify food consumption, while the second one used a 24-hour recall. The vitamin B12 deficiency can occur due to several factors. Initially, the low consumption of its sources can cause it. Among patients in the postoperative period, the reduction of consumption is common, since studies show that red meat is commonly not tolerated25,26. However, a key factor in reducing the absorption is decreased production of intrinsic factor, by the stomach, that by connecting with vitamin B12 allows its absorption by the distal portion of the ileus25. Therefore, despite the intake being sufficient, the absorption of the micronutrient in question is probably very weak and may lead to the development of nutritional deficiencies. Pernicious anemia is a consequence of the deficiency of this vitamin, which usually manifests with the same symptoms of iron deficiency anemia.
The different dietary surveys used by the authors of the studies made it difficult to compare the results and impossible to correct the data analysis of this study. It is known that there is an instrument that accurately quantifies the food intake of a population. The Food Frequency Questionnaire is flawed because it depends on the patient's memory and demands much time for answering11. Nevertheless, its use is recommended in the assessment of micronutrient intake allowing investigation of nutritional needs11.
The positive and statistically significant correlation between time after surgery and the intake of iron, vitamin B12 and vitamin D suggests adapting of the eating habits over time. Basfi-fer et al.2 also found that dietary iron intake increased between the 6th and 12th month postoperatively. On the other hand Rebolledo et al.24 brought this same result, but between the 12th and 18th month. Prevedello et al.23 found in his study that dietary intake of iron, vitamin B12 and vitamin D increased from the 6th to the 30th month, but no statistical analyzes were performed to verify the significance of these data.
Patients undergoing bariatric surgery can develop intolerances to certain types of food26. Schweiger et al.26 and Salgado et al.25 found red meat as the main culprit for food intolerances. In the present study, the findings presented differences from study previously cited, since milk and derivatives and cereals were the most commonly cited food groups to cause food intolerances by patients in the sample. Since this is a subjective evaluation and can depend on how it is questioned, the differences in the results of studies can be justified.
There are no recommendations for intake of specific micronutrients for patients undergoing bariatric surgery; therefore, values used as reference recommendations were the same directed at the healthy population. The anatomical and physiological changes associated with gastric bypass disabsorptive processes lead to increasing nutritional needs. Thus, the risk of nutrient deficiencies increase as well as the importance of nutritional monitoring in the postoperative period.
Because of the multiple factors that may cause deficiencies of the micronutrients studied, supplementation is necessary for prevention and/or treatment6. The exclusive use of multivitamins in patients undergoing gastric bypass has not proven sufficient, being necessary to continuously monitor the consumption and the possible lack of each micronutrient and use specific supplementation, as needed individually6.
The adjustment in dietary intake of micronutrients may occur over time after surgery for obesity. Possibly this is due to adaptation to the dietary habits of the patient in the long term. An important aspect that needs to be investigated is nutrient deficiency prior to operation. Possible deficiencies that may be identified must be treated so that no aggravation occurs postoperatively.
The multidisciplinary monitoring of bariatric patients preoperatively and postoperatively is important and should be encouraged. Special attention is needed to the late postoperative period, since it is common that patients do not give continuity to this monitoring, thus compromising treatment success.
CONCLUSION
The dietary ingestion of the population studied was not sufficient to meet its nutritional needs, since it was found inadequate as to the intake of iron, calcium and vitamin D. Therefore, nutrient supplementation in the postoperative period is important to prevent the onset of nutritional deficiencies. Vitamin B12 presented different results from other nutrients analyzed, reaching nutritional recommendations over a year after surgery.
Footnotes
Conflicts of interest: none
Financial source: none
REFERENCES
- 1.AACE/TOS/ASMBS Bariatric Surgery Clinical Practice Guidelines. Endocr Pract. 2013;19(2) [Google Scholar]
- 2.Basfi-fer K, Rojas P, Carrasco F, Valencia A, Inostroza J, Codoceo J, Pizarro F, Olivares M, Papapietro K, Csendes A, Rojas J, Adjemian D, Calderón E, Ruz M. Evolución de la ingesta y del estado nutricional de zinc, hierro y cobre en mujeres sometidas a cirugía bariátrica hasta el segundo año postoperatorio. Nutr Hosp. 2012;27(5):1527–1535. doi: 10.3305/nh.2012.27.5.5913. [DOI] [PubMed] [Google Scholar]
- 3.Blake M, Fazio V, O'Brien P. Assessment of nutrient intake in association with weight loss after gastric restrictive procedures for morbid obesity. Aust N Z J Surg. 1991;61(3):195–199. doi: 10.1111/j.1445-2197.1991.tb07591.x. [DOI] [PubMed] [Google Scholar]
- 4.Bordalo LA, Mourão DM, Bressan J. Deficiências nutricionais após cirurgia bariátrica: por que ocorrem? Acta MedPort. 2011;24(S4):1021–1028. [PubMed] [Google Scholar]
- 5.Bordalo LA, Teixeira TFS, Bressan J, Mourão DM. Cirurgia bariátrica: como e por que suplementar. Rev. Assoc. Med. Bras. 2011;57(1):113–120. doi: 10.1590/s0104-42302011000100025. [DOI] [PubMed] [Google Scholar]
- 6.Bordalo LA, Teixeira TFS, Bressan J, Mourão DM. Cirurgia bariátrica: como e por que suplementar. Rev. Assoc. Med. Bras. 2011;57(1):113–120. doi: 10.1590/s0104-42302011000100025. [DOI] [PubMed] [Google Scholar]
- 7.Brasil; Ministério da Saúde; Secretaria de Vigilância em Saúde; Secretaria de Gestão Estratégica e Participativa. Vigitel Brasil 2011: vigilância de fatores de risco e proteção para doenças crônicas por inquérito telefônico / Ministério da Saúde, Secretaria de Vigilância em Saúde, Secretaria de Gestão Estratégica e Participativa. Brasília: Ministério da Saúde; 2012. [Google Scholar]
- 8.Camberos-Solis R, Jimenez-Cruz A, Bacardí-Gascón M, Culebras JM. Efectividad y seguridad a largo plazo del bypass gástrico en "Y" de Roux y de la banda gástrica: revisión sistemática. Nutr. Hosp. 2010;25(6) [PubMed] [Google Scholar]
- 9.Crispim SP, Ribeiro RCL, Panato E, Silva MMS, Rosado LEFP, Rosado GP. Validade relativa de um questionário de frequência alimentar para utilização em adultos. Rev Nutr. 2009;22(1):81–95. [Google Scholar]
- 10.Crispim SP, Franceschini SCC, Priore SE, Fisberg RM. Validação de inquéritos dietéticos: uma revisão. Nutrire Rev Soc Bras Aliment Nutr. 2003;26(10):27–41. [Google Scholar]
- 11.Duarte ACG. Avaliação nutricional: aspectos clínicos e laboratoriais. São Paulo: Atheneu; 2007. [Google Scholar]
- 12.Furlan-Viebig R, Pastor-Valero M. Desenvolvimento de um questionário de frequencia alimentar para o estudo de dietas e doenças não transmissíveis. Rev SaúdePública. 2004;38(4):581–584. doi: 10.1590/s0034-89102004000400016. [DOI] [PubMed] [Google Scholar]
- 13.Garrido J, Arthur B. Cirurgia da obesidade. São Paulo: Editora Atheneu; 2006. [Google Scholar]
- 14.Institute of Medicine, Food and Nutrition Board . Dietary Reference Intakes: RDA and AI for Vitamins and Elementes. 1989. Disponível em: http://fnic.nal.usda.gov/dietary-guidance/dietary-reference-intakes/dri-tables. [Google Scholar]
- 15.Instituto Brasileiro de Geografia e Estatística. Pesquisa de Orçamento Familiares 2008-2009: Tabela de Composição Nutricional dos Alimentos Consumidos no Brasil. Ministério do Planejamento, Orçamento e Gestão; Rio de Janeiro: 2011. [Google Scholar]
- 16.John S, Hoegerl C. Nutritional deficiencies after gastric bypass surgery. JAOA. 2009;109(11):601–604. [PubMed] [Google Scholar]
- 17.Martínez RD, Méndez LFP. Intolerancia a la lactosa. Rev. esp. enferm. dig. 2006;98(2):143–143. doi: 10.4321/s1130-01082006000200009. [DOI] [PubMed] [Google Scholar]
- 18.Metropolitan Life Insurance Company . Metropolitan Height And Weight Tables For Men And Women On Metric Basis. 1999. [Google Scholar]
- 19.Moizé V, Andreu A, Flores L, Torres F, Ibarzabal A, Delgado S, Lacy A, Rodriguez L, Vidal J. Long-term dietary intake and nutritional deficiencies following sleeve gastrectomy or Roux-En-Y gastric bypass in a mediterranean population. J. Acad. Nutr Diet. 2013;113(3):400–410. doi: 10.1016/j.jand.2012.11.013. [DOI] [PubMed] [Google Scholar]
- 20.Molag ML, Vries JH, Ocke MC, Dagnelie PC, van den Brandt PA, Jansen MC, et al. Design characteristics of food frequency questionnaires in relation to their validity. Am J Epidemiol. 2007;166(12):1468–1478. doi: 10.1093/aje/kwm236. [DOI] [PubMed] [Google Scholar]
- 21.Phillipi ST. Tabela de Composição de Alimentos - Suporte para Decisão Nutricional. 4. Ed. Manole; 2013. [Google Scholar]
- 22.Pinheiro ABV. Tabela para Avaliação de Consumo Alimentar em Medidas Caseiras. 5. Ed. Rubio; Rio de Janeiro: 2004. [Google Scholar]
- 23.Prevedello CF, Colpo E, Mayer ET, Copetti H. Análise quantitativa e qualitativa da dieta de pacientes no pré e pós-operatório de cirurgia bariátrica. Rev. Bras. Nutr Clin. 2009;24(3):159–165. [Google Scholar]
- 24.Rebolledo A, Basfi-fer K, Rojas P, Codoceo J, Inostroza J, Carrasco F, Ruz M. Evolución y calidad de la alimentación de mujeres con obesidad severa y mórbida sometidas a bypass gástrico. Archivos Latinoamericanos de Nutrición. 2009;50(1):7–13. [PubMed] [Google Scholar]
- 25.Salgado W Jr, Modotti C, Nonino CB, Ceneviva R. Anemia andirondeficiencybeforeandafterbariatricsurgery. SurgObesRelatDis; Jun 15, 2013. [Google Scholar]
- 26.Schweiger C, Weiss R, Keidar A. Effect of different bariatric operations on food tolerance and quality of eating. Obes Surg. 2010;20(10):1393–1399. doi: 10.1007/s11695-010-0233-9. [DOI] [PubMed] [Google Scholar]
- 27.Silva SA, Burgos MGPA, Santos EMC, Batista JEM, Bion FM. Consumo alimentar de obeso sem período pré e pós-operatórios de cirurgia bariátrica. A. Fac. Med. Univ. Fed Pernamb. 2005;50(1):15–18. [Google Scholar]
- 28.Sociedade Brasileira de Cirurgia Bariátrica . Consenso Brasileiro Multissocietário em Cirurgia da Obesidade. São Paulo: 2006. [Google Scholar]
- 29.Tabela brasileira de composição de alimentos / NEPA - UNICAMP- 4 ed rev e ampl. Campinas: NEPA - UNICAMP; 2011. [Google Scholar]
- 30.Valezi AC, Mali JJ, Menezes MA, Brito EM, Souza JCL. Weight loss eight years after gastric bypass. Rev. Col. Bras Cir. 2011;38(4):232–236. doi: 10.1590/s0100-69912011000400006. [DOI] [PubMed] [Google Scholar]