Abstract
Background
Bariatric surgery, especially Roux-en-Y gastric bypass is an effective treatment for refractory morbid obesity, causing the loss of 75% of initial excess weight. After the surgery, however, weight regain can occur in 10-20% of cases. To help, endoscopic argon plasma coagulation (APC) is used to reduce the anastomotic diameter. Many patients who undergo this treatment, are not always familiar with this procedure and its respective precautions.
Aim
The aim of this study was to determine how well the candidate for APC understands the procedure and absorbs the information provided by the multidisciplinary team.
Method
We prepared a questionnaire with 12 true/false questions to evaluate the knowledge of the patients about the procedure they were to undergo. The questionnaire was administered by the surgeon during consultation in the preoperative period. The patients were invited to fill out the questionnaire.
Results
We found out that the majority learned about the procedure through the internet. They knew it was an outpatient treatment, where the anesthesia was similar to that for endoscopy, and that they would have to follow a liquid diet. But none of them knew that the purpose of this diet was to improve local wound healing.
Conclusion
Bariatric patients who have a second chance to resume weight loss, need continuous guidance. The internet should be used by the multidisciplinary team to promote awareness that APC will not be sufficient for weight loss and weight-loss maintenance in the long term. Furthermore, there is a need to clarify again the harm of drinking alcohol in the process of weight loss, making its curse widely known.
Keywords: Argon plasma coagulation, Bariatric surgery, Endoscopy, Weight gain
Abstract
Racional
A cirurgia bariátrica, em especial o bypass gástrico em Y-de-Roux é tratamento efetivo para a obesidade mórbida refratária, promovendo perda de 75% do excesso de peso inicial. Após o procedimento, no entanto, pode ocorrer reganho em 10-20% dos casos. Para auxiliar, há a fulguração com argônio endoscópico que objetiva a redução do diâmetro anastomótico. Muitos pacientes que se submetem a este tratamento, nem sempre conhecem o processo e seus respectivos cuidados.
Objetivo
Analisar o modo como o candidato ao procedimento de plasma endoscópico de argônio, entende o processo e absorve as informações transmitidas pela equipe multiprofissional.
Método
Foi elaborado um questionário com 12 questões do tipo Verdadeiro/Falso no intuito de avaliar o conhecimento do paciente acerca do método ao qual estava prestes a ser submetido. O questionário foi aplicado pelo médico cirurgião no momento de sua consulta no período pré-procedimento. Os pacientes foram convidados livremente a preencher o questionário.
Resultados
Verificou-se que a maioria conhecia o procedimento através da internet; sabia que era tratamento ambulatorial; que a anestesia era similar à da endoscopia; que necessitava de dieta líquida. Mas, nem todos sabiam que ela era para melhorar a cicatrização local.
Conclusão
Os pacientes bariátricos que possuem uma segunda chance para retomar o emagrecimento, precisam de orientações permanentes. A internet debe ser usada pela equipe multiprofissional para conscientização de que o PEA não será suficiente para a perda e manutenção de peso em longo prazo. Ainda há a necessidade de re-esclarecer o prejuízo da ingestão de álcool no processo de perda de peso, amplamente divulgando seu malefício.
INTRODUCTION
Weight regain after bariatric surgery, especially Roux-en-Y gastric bypass, shows a high prevalence and can occur 18-24 months after the surgical procedure. There are many possible causes, such as returning to bad eating habits as before the operation, excessive alcohol consumption, sedentarism and believing too much that only bariatric surgery will make up the whole weight loss and weight-loss maintenance process, and that the compromise of patients in their chronic treatment for obesity is safe.
Although having patients search for a multidisciplinary team regularly is the best way of controlling and treating weight regain, an innovative and non-invasive treatment known as endoscopic argon plasma coagulation (APC)2 has been utilized in Brazil since 2009 by the authors to help control it. APC is an outpatient procedure that is serial and performed by upper digestive endoscopy; it gradually reduces the diameter of the gastrojejunal anastomosis, increases gastric emptying time and causes early satiety, reducing food intake and thereby fostering weight loss.
However, patients do not always know and understand the directions of the multidisciplinary team for the procedure. The necessity to break the cycle of weight regain, which affects many, makes any information that gives hope for weight loss the best option for the moment. The tendency is that, after the procedure, doubts appear and need to be resolved, in the case they had not been understood at the first session of APC.
The objective of the present study was to analyze how well the candidate for the APC procedure understands the process and absorbs the information provided by the multidisciplinary team.
METHODS
A questionnaire was prepared with 12 true/false questions (Figure 1), for the purpose of evaluating the knowledge of the patient about the procedure they were to undergo. The questionnaire was administered by the surgeon during consultation in the preoperative period. The patients were invited to fill out the questionnaire and asked to sign an informed consent form. The study was approved by the Research Ethics Committee of Hospital Vita Batel, Curitiba, PR, Brazil.
FIGURE 1.
Questionnaire administered in this study of endoscopic argon plasma coagulation after bariatric surgery
| 1. I learned about endoscopic argon plasma coagulation through: |
| ( ) internet ( ) a friend who had it done ( ) medical recommendation ( ) my surgeon ( ) magazine ( ) TV ( ) others |
| which? ________________________________________________ |
| 2. The endoscopic argon plasma coagulation procedure guarantees bariatric patients that they will never regain weight. |
| ( ) true ( ) false |
| 3. The procedure commonly called endoscopic argon is thermal coagulation to narrow the food passageway from the stomach to the intestine and make the person feel satiated |
| ( ) true ( ) false |
| 4. How many sessions of endoscopic argon plasma coagulation may be needed so that the desire effect of satiety is achieved? |
| ( ) only 1 ( ) 2-3 ( ) 3-5 ( ) 5-7 |
| 5.Endoscopic argon plasma coagulation requires days of hospitalization, anesthesia and rest because its effects vary greatly from person to person. |
| ( ) true ( ) false |
| 6 The endoscopic argon plasma coagulation procedure is by the endoscopic route, is minimally invasive and, therefore, performed in an outpatient setting. It is an intervention that does not need hospitalization. |
| ( ) true ( ) false |
| 7. Argon is a chemical element that in contact with alcoholic beverages can be highly corrosive and cause ulcerations in the digestive tract. |
| ( ) true ( ) false |
| 8. The aim of the recommended diet after the procedure is only to help lose weight and stimulate the euphoria cause by the physiology of fasting. |
| ( ) true ( ) false |
| 9. The sedation utilized for the procedure called endoscopic argon plasma coagulation is generally the type used in gastric bypass surgery. |
| ( ) true ( ) false |
| 10. By narrowing the gastrojejunal anastomosis (junction between the new stomach and intestine) greatly, the endoscopic argon plasma coagulation procedure allows the patient to eat food that before was fattening for the surgery. |
| ( ) true ( ) false |
| 11. The endoscopic argon plasma coagulation procedure can be done in persons have had bariatric surgery or not. |
| ( ) true ( ) false |
| 12. Drinking alcoholic beverages after APC can be harmful to health. Use APC earlier in questionnaire and regularly? |
| ( ) true ( ) false |
Sixty-nine questionnaires were administered to patients of both sexes, candidates for the procedure to decrease weight regain by dilation of the gastrojejunal anastomosis or to complete the weight loss not achieved only with bariatric surgery. Of the patients who filled out the questionnaire of knowledge about the APC procedure, two turned in the questionnaire blank (2.89%). Another two participants (2.89%) filled out only the first page, leaving it incomplete. Incomplete and blank questionnaires were excluded from the sample, which then totaled 65 patients. Of these, only nine had undergone a previous psychological interview about APC (13.8%). This variable did not interfere with the results of the questionnaire. One of the participants who turned in a blank questionnaire and another responding only to the first page were excluded.
The data obtained were tabulated on a spreadsheet (Excel, version 2007) and the mean of the responses determined.
RESULTS
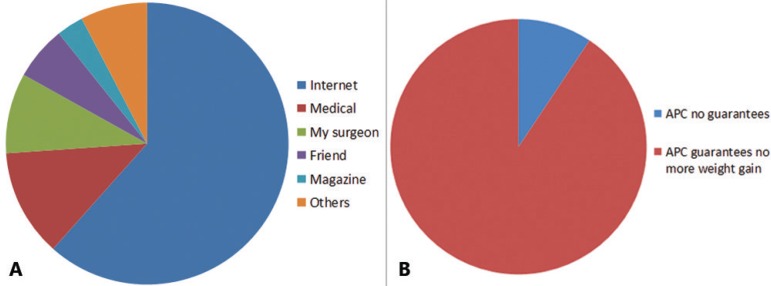
Of the total number of patients who filled out the questionnaire, 40 (61.5%) knew about the procedure through the internet, who considered the means of access and disclosure more effective, four (6.15%) through friends, and eight (12.3%) from medical recommendation, while six were informed directly by their surgeon (9.12%) and one through a magazine (1.5%). Other reasons were given by five persons (7.65) in seeking APC (Figure 2A).
Figure 2.
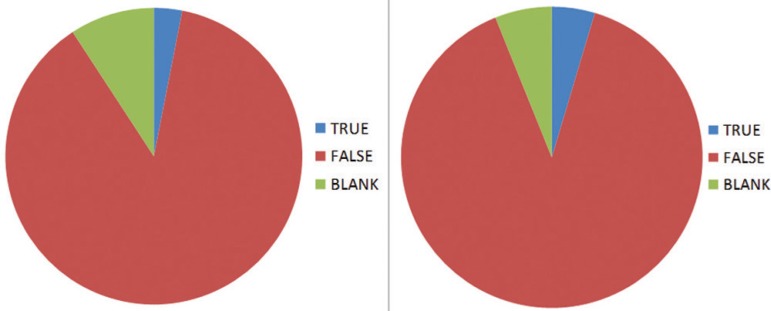
A) Means of communication through the patients learned of the APC procedure; B) guarantee of APC regarding future maintenance of weight loss
Of the group in general, 89.2% of the interviewees were aware that APC did not guarantee weight-loss maintenance, versus six (9.2%) who thought that it would (Figure 2B).
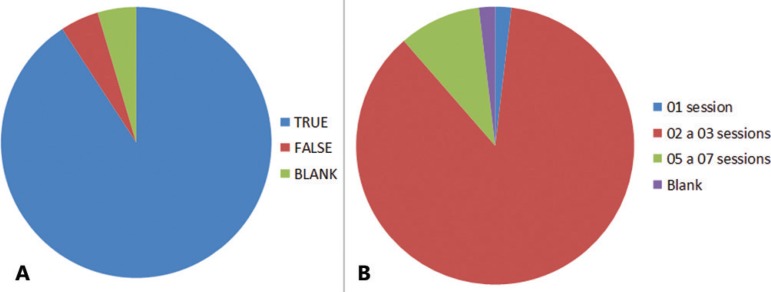
When asked what was the effective function of the procedure, 59 persons (90.7%) had a good comprehension of the procedure that it served to narrow the food passageway and to allow more time for gastric satiety, which can minimize food intake. However, three (4.16%) considered this information false and another three (4.16%) left the question blank (Figure 3A).
Figure 3.
A) Function of thermal coagulation to narrow the food passageway; B) number of APC sessions necessary for satisfactory results
With regard to the number of necessary sessions, the rate of doubts was high, where 69.2% of the interviewees believed that up to three sessions were needed, 1.5% (one patient) understood that only one session was needed, 7.6% (five) thought it was important to have five to seven sessions, and one person (1.5%) left the question blank (Figure 3B).
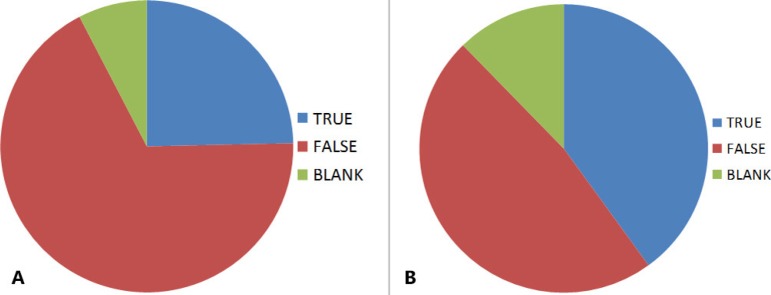
On the necessity of hospitalization, anesthesia and rest after the procedure, 16 patients (24.6%) considered it necessary to be hospitalized and to get rest besides anesthesia, 67.6% (44 persons) understood that this special care was not needed, and only five (7.6%) did not answer the question (Figure 4A).
Figure 4.
A) Care after APC: need for hospitalization, anesthesia and rest; B) knowledge of the effects of drinking alcohol after APC
When questioned if APC is an outpatient procedure, minimally invasive, 98.4% (64 patients) confirmed the information and only one (1.5%) did not give an answer.
A contentious issue was with the consumption of alcohol after the procedure, showing divided opinions: 40% of the interviewees believed that alcohol could have a negative effect on the stomach; 47.7% thought that alcohol did not cause any problem and 12.3% left the question blank (Figure 4B).
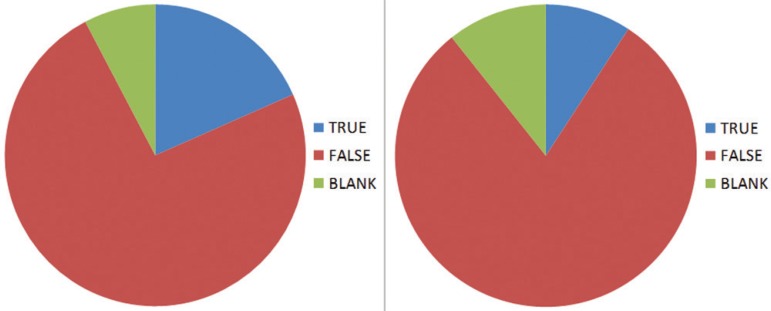
The restriction of food consistency after APC is very important and 73.8% of the interviewees had the idea that a liquid diet fostered wound healing and protection of the stomach, but still, a large percentage (18.4%) believed that the limitation of food consistency was to promote weight loss (Figure 5A).
Figure 5.
A) Objectives of the liquid diet in wound healing and protection of the stomach; B) anesthesia of APC was not the same as in the preceding operation
Of the interviewees, 80% knew that the anesthesia utilized for APC was not the same as for bariatric surgery and that only endoscopy was involved, facilitating recovery and return to work and daily activities; but six (9.2%) thought that the anesthesia was the same as in the previous operation and seven (10.7%) left the question blank (Figure 5B).
For 87.6% of the patients, eating anything would not be allowed and there would be a need for dietary restrictions similar as in bariatric surgery; but 3.07% (two persons) believed that they could eat all the food they wanted, and six (9.2%) did not know how to respond (Figure 6A).
Figure 6.
A) Unrestricted diet after APC; B) necessity of bariatric surgery prior to APC
To undergo APC, 89.2% understood that they needed to have had bariatric surgery, but three thought that prior bariatric surgery was not necessary and four left the question blank (Figure 6B).
A worrisome result was that 36.7% of the candidate patients for APC believe that it was not wrong to drink alcohol after the procedure, and only 50.7% were aware that the drinking alcohol beverages could hamper weight loss and cause discomfort. Furthermore, eight persons (12,3%) did not know how to answer this question.
DISCUSSION
Obesity is a chronic disease that requires continuous treatment to obtain satisfactory results. What was observed in this study was that many patients who sought various treatments were not always able to follow the directions they received from the multidisciplinary team, besides having some misconceptions about the treatments proposed and the limitations, be they dietetic or behavioral4.
The majority of those operated wanted to maintain their weight loss and slimmer body image, but they were not always prepared to follow the guidelines that chronic treatment requires10.
The use of the internet8, with the formation of obesity support groups, is becoming an effective means in spreading information on the subject, as confirmed in the present study, where 44,6% of the interviewees knew about APC through this form of communication.
With bariatric surgery, patients need to change their lifestyle to adapt to new conditions. With APC, which consists in an electrocoagulation technique without contact in which radiofrequency energy is applied to the tissue by means of the ionized argon gas, 87.6% understood its limitation and conceded that it would not be the absolute solution to avoid weight regain and that they would have to change their habits to obtain satisfactory results. According to Carolyn et al.3, during the use of calorie restricted diets, patients need to be careful in their choice of macronutrients - with priority for protein -, to diminish the risk of weight regain.
Among the many treatment options for weight loss, the patients understood that the APC procedure was not invasive and that it did not require hospitalization, that all would be discharged soon after the procedure, and that the objective was the narrowing of the food passageway.
The majority understood that the number of sessions would be two or three, where this would depend on the individual.
In relation to alcohol, it is worrisome that 47.6% considered such beverage was not harmful to the health of someone subjected to APC, and 40% of the patients only believed that alcohol could have a corrosive effect after the procedure. According to Yusef Kudsi et al.11, there is a high prevalence of alcoholism before the operation, and this could be the main reason for weight regain in those operated. Considered a calorie additive, alcohol requires continuous multidisciplinary follow-up9. Along this same line, 50.7% of the interviewees recognized that alcohol could have harmful effects on health, but still 36.9% did not consider this notion to be true. Ferguson et al.6, in studying lifestyle, found that those who drank alcoholic beverages and drugs before the bariatric procedure had a greater predisposition to maintain this habit and regain weight. In this study data prior to the operation were not analyzed.
Regarding a liquid diet, a high percentage of patients (18.4%) believed that the aim of this restriction in consistency was to promote weight loss, which was not true. The use of liquids immediately after APC is to facilitate wound healing in the stomach and, consequently, to elicit weight loss rebound, basically by loss of water and muscle mass, which is not physiologically healthy but needed at that moment. About 88% of the interviewees understood the necessity of restricting calories to promote weight loss as desired and changing eating habits as suggested for the postoperative period of bariatric surgery. It is known that afterwards patients may return to old eating habits, with soft foods in detriment of protein-rich foods. This occurs because of the difficulty of accepting meats, due to the lack of chewing and decrease in digestive enzymes. This dietary choice makes it difficult to lose weight and maintain weight loss in the long term1.
Himpens et al.7 demonstrated that weight regain occurs among gastric bypass patients and that the patients need alternative treatments to deal with returning morbidities. The majority of patients (89.2%) accepted that they needed to have had bariatric surgery before APC, and that only simple anesthesia as for endoscopy would be utilized.
Erick et al.5 examined the mechanisms of weight regain after loss and concluded that precautions need to be continuous since this is a chronic disease. Since there is a great abundance of information on obesity on the internet, much of without scientific merit, teams specialized in obesity need to have effective means of offering support to patients, with more in-depth information on the methods of treatment and their consequences and limitations. It should be especially clarified that the psychopathological disturbances in the preoperative period, or after weight regain and treatment with APC, will not be resolved with the procedure per se, and that they need to be handled and controlled with specific treatments.
Various correlation studies should be developed to better understand who are the operated patients who regain weight and what are their expectations of APC.
CONCLUSIONS
Bariatric patients that have a second chance to resume weight loss need continuous guidance. The internet should be used by the multidisciplinary team to promote awareness that APC alone will not be sufficient for weight loss and weight-loss maintenance in the long term. Furthermore, there is a need to reemphasize the harm of drinking alcohol in the process of weight loss, making its curse widely known.
Footnotes
Conflicts of interest: none
Financial source: none
REFERENCES
- 1.Apolzan JW, Carnell NS, Mattes RD, Campbell WW. Inadequate dietary protein increases hunger and desire to eat in younger and older men. J Nutr. 2007;137(6):1478–1482. doi: 10.1093/jn/137.6.1478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baretta GAP. Tratamento endoscópico do reganho de peso pós-bypass gástrico através da fulguração com argônio da anastomose gastrojejunal. Universidade Federal do Paraná; Curitiba: 2013. 78. [Google Scholar]
- 3.Walsh CO, Ebbeling CB, Swain JF, Markowitz RL, Feldman HA, Ludwig DS. Effects of diet composition on postprandial energy availability during weight loss maintenance. PLoS One. 2013;8(3): doi: 10.1371/journal.pone.0058172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dalle Grave R, Calugi S, El Ghoch M. Lifestyle modification in the management of obesity: achievements and challenges. Eat Weight Disord. 2013;18(4):339–349. doi: 10.1007/s40519-013-0049-4. [DOI] [PubMed] [Google Scholar]
- 5.Blomain ES, Dirhan DA, Valentino MA, Kim GW, Waldman SA. Mechanisms of Weight Regain following Weight Loss. SRN Obes. 2013;2013:210524–210524. doi: 10.1155/2013/210524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ferguson S, Al-Rehany L, Tang C, Gougeon L, Warwick K, Madill J. Self-reported causes of weight gain: among prebariatric surgery patients. Can J Diet Pract Res. 2013;74(4):189–192. doi: 10.3148/74.4.2013.189. [DOI] [PubMed] [Google Scholar]
- 7.Himpens J, Coromina L, Verbrugghe A, Cadière GB. Outcomes of revisional procedures for insufficient weight loss or weight regain after Roux-en-Y gastric bypass. Obes Surg. 2012;22(11):1746–1754. doi: 10.1007/s11695-012-0728-7. [DOI] [PubMed] [Google Scholar]
- 8.Mewton L, Smith J, Rossouw P, Andrews G. Current perspectives on Internet-delivered cognitive behavioral therapy for adults with anxiety and related disorders. Psychol Res Behav Manag. 2014;7:37–46. doi: 10.2147/PRBM.S40879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Odom J, Zalesin KC, Washington TL, Miller WW, Hakmeh B, Zaremba DL, Altattan M, Balasubramaniam M, Gibbs DS, Krause KR, Chengelis DL, Franklin BA, McCullough PA. Behavioral predictors of weight regain after bariatric surgery. Obes Surg. 2010;20(3):349–356. doi: 10.1007/s11695-009-9895-6. [DOI] [PubMed] [Google Scholar]
- 10.Sarwer DB, Wadden TA, Moore RH, Eisenberg MH, Raper SE, Williams NN. Changes in quality of life and body image after gastric bypass surgery. Surg Obes Relat Dis. 2010 Nov-Dec;6(6):608–614. doi: 10.1016/j.soard.2010.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kudsi OY, Huskey K, Grove S, Blackburn G, Jones DB, Wee CC. Prevalence of preoperative alcohol abuse among patients seeking weight-loss surgery. Surg Endosc. 2013;27(4):1093–1097. doi: 10.1007/s00464-012-2568-x. [DOI] [PMC free article] [PubMed] [Google Scholar]