Abstract
Objectives
Despite a national crisis of increased prevalence of obesity and type 2 diabetes mellitus in adolescents, especially among Hispanics, there is a paucity of data on health indicators among farmworker adolescents and their peers. The main aim of this study was to estimate the prevalence of cardiovascular disease risk factors in a population of Hispanic adolescent students in south Texas. The study also aimed to compare the prevalence of these risk factors between students enrolled in the Migrant Education Program (MEP) and other students, and between boys and girls.
Methods
In partnership with the Weslaco (Texas) Independent School District and the Migrant Education Department, a cohort study was conducted from 2007 to 2010 to estimate the prevalence of overall obesity (body mass index ≥85th percentile for age and sex), abdominal obesity (waist circumference ≥75th percentile for age, sex, and ethnicity), acanthosis nigricans (AN), and high blood pressure (HBP; ≥90th percentile for age, height, and sex or systolic/diastolic BP ≥120/80 mm Hg) among MEP students compared with other students from two south Texas high schools. Multilevel logistic regression was used to assess the relation between sex and our main outcomes of interest while accounting for within-school nesting of participants.
Results
Among 628 sampled students, 508 (80.9%) completed the consent procedure and participated in the study. Of these, 257 were MEP students and 251 were non-MEP peers. Approximately 96.7% of participants were Hispanic and 50.0% were boys. Analyses of data across the years comparing MEP students and non-MEP students show an average prevalence of 44.8% versus 47.7% for overall obesity, 43.2% versus 43.7% for abdominal obesity, 24.7% versus 24.7% for AN, and 29.2% versus 32.8% for HBP. Across recruitment and follow-up years, the prevalence of overall obesity, abdominal obesity, and HBP was 1.3 to 1.5, 1.2 to 1.8, and 2.9 to 4.6 times higher in boys than in girls, respectively. In contrast, the prevalence of AN varied little by sex.
Conclusions
The high prevalence of cardiovascular risk factors in both groups suggests a compelling need for comprehensive, culturally targeted interventions to prevent future cardiovascular diseases in these high-risk Hispanic adolescents, especially among boys. There were not, however, substantial differences between MEP students and other students. These findings also support the feasibility of conducting future epidemiologic studies among adolescent farmworkers and their families, as well as culturally appropriate school or community-based interventions.
Keywords: cardiovascular disease, adolescents, blood pressure, obesity, acanthosis nigricans, farmworker, HispanicsA
Although there are no precise estimates, there are at least 1 million farmworkers in the United States.1 More than three-fourths of farmworkers self-identify as being Latino/Hispanic and farmworker families earn between $17,500 and $19,500/year on average.2 The uninsured rate of children of farmworkers is three times that of other children and nearly twice that of those categorized at or near the federal poverty level.1 Mobility also creates problems for the migrant farmworker adolescent population, socially, educationally, and physically, as they migrate with their families for farm work.3 Taken together, these data paint a picture of an at-risk Hispanic adolescent population with limited access to health care.
It is also important to consider whether there are differences in health between farmworkers and other Hispanic residents, such as has been reported in adults in the California Agricultural Workers Health Study and the Binational Health Study.4 In extensive reviews of the health of farmworkers in the United States, Villarejo1,4 noted the lack of nationwide data on obesity, hypertension, cholesterol, and other chronic disease indicators among the farmworker population, with an even greater gap in information on farmworker youth.
Despite these issues and a national crisis of increased prevalence of obesity and type 2 diabetes mellitus in adolescents, especially among Hispanics, studies focusing on the overall health status and risks of adolescent farmworkers are sparse and limited in scope.5,6 To begin to address this research gap, the present study was conducted to estimate the prevalence of overall obesity, abdominal obesity, acanthosis nigricans (AN), and high blood pressure (HBP) in a population of predominantly Hispanic adolescent students attending high schools in Weslaco, Texas, along the border of Texas and Mexico. The prevalence of these cardiovascular risk factors also was compared between students in the Migrant Education Program (MEP) students and other students and between boys and girls. This project was approved by the Committee for the Protection of Human Subjects at the University of Texas Health Science Center at Houston (protocol no. HSC-SPH-07-0284) and the institutional review board at Texas A&M University (protocol no. 2010-0878).
Methods
The study design was a prospective cohort study following participants for up to 3 years. Study participants were identified from a listing of 9th-grade MEP students in two high schools. An equal number of randomly selected non-MEP 9th-grade students were recruited from the same high schools. The cohort had a dynamic aspect that allowed the entry of new 9th-grade students in the second year and the exit of students each year. Each year (2007–2010) during winter, study participants underwent a minimum clinical examination consisting of measured height and weight, waist circumference, screening for AN, and BP. A survey also obtained information on demographic characteristics and work history. This article focuses on the prevalence of cardiovascular disease risk factors by MEP status and sex at baseline and each year of follow-up.
Sample Size and Study Population
All MEP students in the two high schools were identified and an approximately equal number of non-MEP students were sampled at random. With a fixed sample size of approximately 250 MEP students and 250 non-MEP students, an odds ratio close to 2.0 (comparing MEP students and non-MEP students) could be detected with 80% power for each of the outcome conditions of interest (obesity, AN, and HBP, based on estimates from the literature), even when the more strict Bonferroni-adjusted alpha level of 0.01 was enforced.7 To qualify for MEP, a student had to have migrated or had at least one parent who migrated (temporarily moved from the Weslaco Independent School District to a different school district or administrative area in the United States) within the previous 3 years to work in agriculture or fishing as a principal means of employment.3,8
Data Collection, Survey Development, and Staff Training
Student and parental informed consent were required before participating in the study. Because farmworkers in south Texas usually migrate in mid-to late spring, and return home in early-to middle autumn, study data were collected from January to March of each year, after an intensive training and institutional review board certification of bilingual interviewers.
Each year at baseline and for up to 3 additional years, study participants completed a three-step process. First, the participant completed a short self-administered questionnaire that included items pertaining to demographics and health risk behaviors. Next, an interviewer administered a more complex set of questions pertaining to medical and work history. Finally, the participant underwent the minimum clinical examination. Clinical results for students with elevated measurements for BP or who had a positive AN screening were mailed to the parents and were referred to community healthcare providers for follow-up.
Variable Definitions
Our main outcomes of interest were overall obesity, abdominal obesity, AN on the neck, and HBP. Overall obesity was defined as body mass index (BMI) at or above the 85th percentile for age and sex.9 BMI was calculated as the weight in kilograms divided by the square of height in meters. Height was assessed to the nearest 0.1 cm using a Shorr Board stadiometer (Shorr Productions, Olney, MD), and weight was measured to the nearest 0.1 kg using a portable Tanita BWB-800S (Tanita Corporation, Arlington, IL) digital scale. Abdominal obesity was defined as waist circumference at or above the 75th percentile for age, sex, and ethnicity.10 AN was defined as a visual discoloration and/or thickening of the skin on the back of the neck. AN can be a marker for high blood insulin levels and insulin resistance; assessment methods were based on standards used for the Texas state-wide school-based screening program.11,12 HBP was defined as at or above the 90th percentile for age, height, and sex or ≥120/80 mm Hg.13 The screening was based on a single occasion, but three consecutive measurements were taken and the second and third were averaged to obtain the analyzed values for systolic and diastolic BP. All of the measurements were taken with the Omron HEM-907XL (Omron Healthcare, Lake Forest, IL), an automated machine. Measurement was taken using the right arm, after sitting quietly for 5 minutes with back support, feet on the floor, and arm supported, with antecubital fossa at heart level.13 Readings were entered into a Web-based program to obtain the age, height, and sex-based percentile for each student.
Data Management and Statistical Analysis
Data were entered via Web Forms into a Microsoft SQL relational database (Microsoft, Redmond, WA), and the data were password protected to ensure access to approved staff only. All numeric or coded data were double entered to minimize data entry errors. Initially, data were edited manually and then computer edited for out-of-range and contradictory values.
Continuous variables were converted into discrete variables using established cutpoints as defined in the definition of the variables above. The prevalence for each outcome variable (overall obesity, abdominal obesity, AN, and HBP) was calculated.
Multilevel logistic regression was used to assess the relation between sex and each of our main outcomes of interest. The multilevel nature of this approach allowed us to account for the nesting of participants within each schoolB. The resulting models estimated the average (marginal) prevalence of each outcome in the whole population and used the latter to calculate marginal crude prevalence ratios. Although odds ratios are commonly used in similar studies, the prevalence ratio avoids the overestimation of the effect of the exposure associated with the use of odds ratios when the frequency of the outcome is high, as it was for each outcome in our study. Standard errors of the prevalence ratio were estimated using the delta method. All of the analyses were conducted using STATA/SE version 13.1 (StataCorp LP, College Station, TX).
Results
Response Rates
Among 9th-grade students, 181 MEP students and 196 non-MEP students in year 1 and an additional 116 MEP students and 135 non-MEP students in year 2 were asked to complete a baseline assessment. Among these 628 sampled students, 508 (257 MEP and 251 non-MEP) participated (80.9%) after completing consent procedures. At baseline (across years 1 and 2), the response was 86.5% among MEP students and 75.8% among non-MEP students. Response rates in the follow-up assessments were >90% in both groups across all years. The denominator for these proportions was the number of participants from the original cohort who were still eligible (ie, attending school at one of the two high school campuses). A substantial number of participants were ineligible because they were no longer attending school. Of those enrolled in year 1 (n = 275), the proportion still eligible at the final (third) year of follow-up was 49.1%. Of those enrolled in year 2 (n = 233), the proportion still eligible at the final (second) year of follow-up was 75.3%. The available sample size by survey year, regardless of year of enrollment, was as follows: baseline (n = 257 MEP, n = 251 non-MEP), first year of follow-up (n = 209 MEP, n = 220 non-MEP), second year of follow-up (n = 165 MEP, n = 181 non-MEP), and third year of follow-up (n = 65 MEP, n = 65 non-MEP).
A separate pilot study focusing on MEP students examined the impact of this loss to follow-up and found that indicators of obesity and HBP were higher at baseline among the loss to follow-up group but not significantly different than study completers. The prevalence of AN was significantly higher at baseline among the loss to follow up group, however (manuscript in preparation).
The participants at baseline were 50.0% boys and had a median age of 15.0 years. A total of 96.7% self-identified as being Hispanic, Latino, or Mexican American; 92.2% were born in the United States, and 78.8% used solely English to complete the survey.
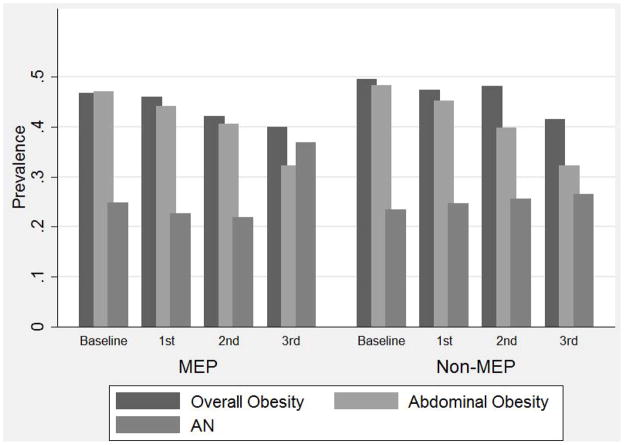
Prevalence of Overall Obesity, Abdominal Obesity, and AN
The average prevalence across the years of the study for overall obesity was 44.8% for MEP students and 47.7% for non-MEP students; for abdominal obesity, the prevalence was 43.2% and 43.7% for MEP students and non-MEP students, respectively. The average prevalence of AN across the study years was 24.7% in MEP students and 24.7% in non-MEP students. Figure 1 displays the prevalence of these outcomes by MEP status at baseline and each year of follow-up. The differences in proportions between MEP students and non-MEP students were not statistically significant (α > 0.05) each year for any of these endpoints.
Fig. 1.
Chronic disease risk factors by Migrant Education Program status, Weslaco, Texas high schools, 2007–2010.
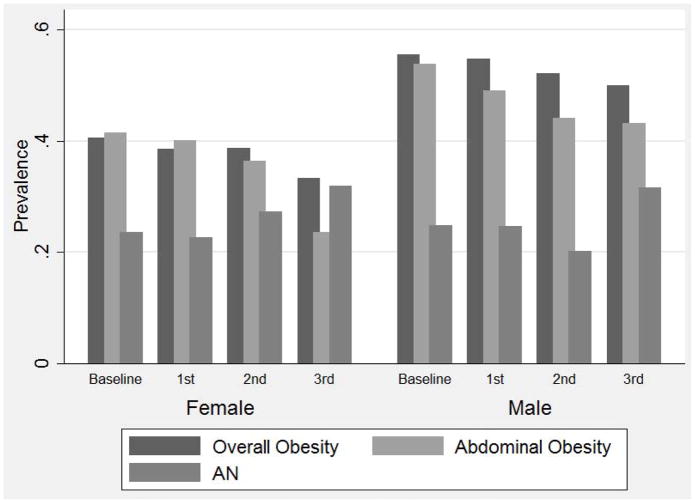
The prevalence of each of these outcomes by sex was examined next. The average prevalence across study years for overall obesity was 54.0% in boys compared with 38.7% in girls, was 49.1% in boys versus 38.0% in girls for abdominal obesity, and was 24.2% in boys versus 25.1% in girls for AN. Figure 2 shows the prevalence of these study outcomes at baseline and each year of follow-up for male and female students. From the multilevel analysis, the prevalence of overall obesity in boys was 1.3 to 1.5 times higher as in girls each year, was 1.2 to 1.8 times higher for abdominal obesity, and was approximately the same for AN in boys as compared with girls (Table).
Fig. 2.
Chronic disease risk factors by sex, Weslaco, Texas high schools, 2007–2010.
Table.
Prevalence ratios (95% CIs) for boys versus girls for study outcomes by study year, Weslaco, Texas high schools, 2007–2010
| Follow-up year | Overall obesity | Abdominal obesity | Positive screen for AN | HBP |
|---|---|---|---|---|
| Baseline | 1.4 (1.1–1.6) | 1.3 (1.1–1.6) | 1.0 (0.8–1.4) | 2.9 (2.1–4.2) |
| Year 1 | 1.4 (1.2–1.7) | 1.2 (1.0–1.5) | 1.1 (0.8–1.5) | 4.6 (3.0–7.0) |
| Year 2 | 1.3 (1.1–1.7) | 1.2 (0.9–1.6) | 0.7 (0.5–1.1) | 4.3 (2.7–6.8) |
| Year 3 | 1.5 (1.0–2.3) | 1.8 (1.1–3.0) | 1.0 (0.6–1.6) | 4.2 (2.1–8.4) |
AN, acanthosis nigricans; CIs, confidence intervals; HBP, high blood pressure.
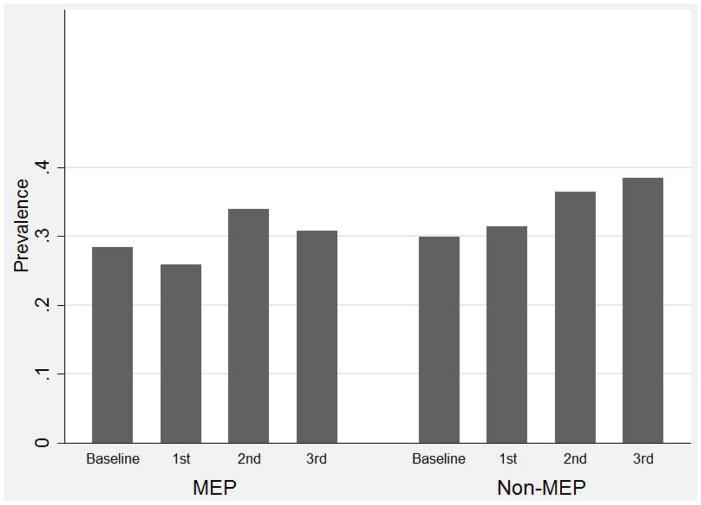
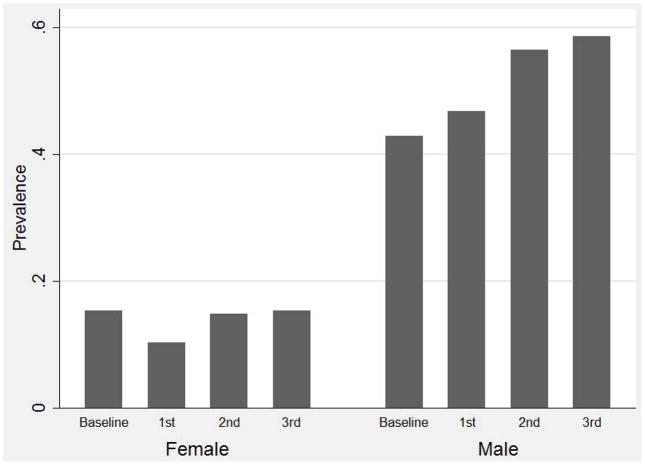
HBP
The average prevalence of HBP across the years of the study was 29.2% for MEP students and 32.8% for non-MEP students. Figure 3 shows the prevalence of HBP at baseline and each year of follow-up for MEP students and non-MEP students (not statistically significant for any year). The average prevalence of HBP across study years comparing male with female students was striking: 48.7% in boys versus 13.7% in girls. Figure 4 displays the prevalence of HBP for male and female students at baseline and each year of follow-up. From the multilevel analysis, the prevalence of HBP was 2.9 to 4.6 times higher in male students compared with female students (Table).
Fig. 3.
High blood pressure by Migrant Education Program status, Weslaco, Texas high schools, 2007–2010.
Fig. 4.
High blood pressure by sex, Weslaco, Texas high schools, 2007–2010.
Discussion
Studying a population of high school students in south Texas helps fill a research gap by estimating the prevalence of overall obesity, abdominal obesity, AN, and HBP in a predominantly Hispanic adolescent population, including members of migrant farmworker families. The strengths of this study also included using migrant education as an enumeration infrastructure enhancing the opportunity to conduct epidemiologic cohort studies in a hard-to-reach agricultural population. Furthermore, a comparison of outcomes in MEP students to other students was able to be included. Our response rates for those enrolled in school each year and eligible for the study were excellent, reaching >95% in the final year of follow-up; however, there was the expected attrition over time from graduation, dropouts, and moves.
The limitations of this study included the constraint on the sample size that was adequate to detect increases in the health outcomes between migrant and other students. A larger sample size would allow more powerful analyses on various subgroups and the ability to detect interactions. Also, because blood samples were not drawn, the study did not include lipid or blood glucose measures that would be important to include in future studies.
The results are alarming in terms of the high prevalence of cardiovascular disease risk factors among these high school students and concern for the possible adverse future course of these risk factors. Overall, >40% of students had overall or abdominal obesity, approximately 25% screened positive for AN, and approximately one-third had HBP readings. Although younger, southwest Texas school children in grades 3, 5, 7, and 9 were reported to be obese (22%), positive for AN (23%), and have elevated BP (>90th percentile, 21%).14 Similarly, Urrutia-Rojas et al15 reported that among among 1066 Hispanic students 10 to 12 years old, the prevalence of obesity was 31.9%, the prevalence of AN was 17%, and elevated BP at the 95% cutoff was 23.6%. The reported prevalence in these studies is somewhat lower than that in our study, presumably because of the younger age and/or different cutoff criteria used for BP.
One of the unexpected findings of this study was the high prevalence of HBP readings among boys and the nearly fourfold higher prevalence among male students compared with female students (approximately 49% of boys and 14% of girls). A differential between male and female students, although of lower magnitude, also has been reported in a national sample of US adolescents 12 to 19 years of age using National Health and Nutrition Examination Survey (NHANES) data from 2005–2010. Based on the average of three BP readings (an average of two used in this study), 22.3% of boys and 9.7% of girls had BPs at or exceeding the 90th percentile for age, height, and sex.16 Using NHANES data among children and adolescents 8 to 17 years of age from 1988 to 2008, Rosner et al17 reported the prevalence of elevated systolic BP or diastolic BP (>90th percentile or 120/80) to be 19.2% for boys and 12.6% for girls. As can be seen, direct comparisons of our study results with the literature are challenging because each study covered different time periods, different demographic profiles, different averaging and cutoffs for elevated BP, and they may have used different types of BP monitoring devices. It also is important to note that elevated BP readings are not synonymous with hypertension because elevated readings on at least three different occasions are recommended for a diagnosis.13
To put our findings into context, it is important to note the national trends in the prevalence of obesity and HBP. The prevalence of obesity has more than tripled in adolescents in the United States in the past 30 years; a trend analysis indicated a significant increase in obesity for male patients only in the past 12 years,18 suggesting a partial explanation for the associated BP differential we detected in boys. One systematic review concluded that child and adolescent obesity was related to greater arterial stiffness.19 The American Medical Association has adopted a policy to recognize obesity as a disease.20 The levels of BP also have been increasing in children and adolescents and are higher in minority youth17,21; however, the increasing trend was not reported in other studies.22 Rosner et al17 attributed the increase in BP in children from 1988–1994 to 1999–2008 using NHANES data to the concomitant increase in obesity, waist circumference, and sodium intake during the same period.
National screening recommendations for AN and BP also are important to consider when informing future research or prevention and control recommendations among understudied populations, such as the population of Hispanic adolescents in our study. There is no accepted recommendation for AN screening nationally. The Centers for Disease Control and Prevention recommends focusing on primary prevention23 and the American Diabetes Association recommended screening school-age children 10 years old and older for AN if they have a BMI >85th percentile with other risk factors.24,25 Harrell et al26 suggested that because of the association between overweight and elevated BP and lipid levels, overweight or obese adolescents should be screened for elevated BP and lipids. In contrast to the recommendations for routine screening of BP in children and adolescents by the American Academy of Pediatrics, the Community Preventive Services Task Force released a statement indicating insufficient evidence to either support or refute this recommendation for the prevention of cardiovascular disease in adulthood.27 The task force’s concerns focused on the diagnostic accuracy of routine screening in the clinical setting and on the lack of evidence as to whether screening results accurately predicted children at increased risk for adult hypertension and cardiovascular disease.28 Although the present study cannot inform this recommendation directly, it is important to measure and document suspected and known risk factors for developing cardiovascular disease in adulthood among understudied populations.
Conclusions
This study demonstrated a high prevalence of overall and abdominal obesity, AN, and HBP among Hispanic high school students in south Texas. The excesses were noted particularly among male students. The evidence is compelling for a need to intervene at individual, family, school, and community levels. Because these risk factors are highly correlated, interventions on any of these factors may affect the overall risk profile.
Overall, these findings support the feasibility of conducting future epidemiologic studies among adolescent farmworkers and their families, as well as school-or community-based interventions that are culturally appropriate. There also is a strong need for longitudinal studies on children, including an adequate sample of Hispanic children, with and without cardiovascular risk factors into adulthood to better describe the significance of these indicators as predictors of future chronic disease.
Key Points.
This study demonstrated a high prevalence of overall obesity, abdominal obesity, acanthosis nigricans, and high blood pressure readings among Hispanic high school students in south Texas.
Although no significant differences were detected between students from migrant farmworker families and other students, there was a sex differential, most notably for elevated blood pressure among male students.
The findings support the feasibility of conducting future epidemiologic studies among adolescent farmworkers and their families, as well as school or community-based interventions that are culturally appropriate.
Acknowledgments
This research was supported by Cooperative Agreement No. U50 OH07541 to the Southwest Center for Agricultural Health, Injury Prevention, and Education at the University of Texas Health Science Center at Tyler from the Centers for Disease Control and Prevention (CDC)/National Institute for Occupational Safety and Health (NIOSH), and Grant No. 5T42OH008421 to the Southwest Center for Occupational and Environmental Health, a NIOSH Education and Research Center, from NIOSH/CDC.
S.P.C. has received funding/compensation from a CDC/NIOSH grant from the University of Texas Health Science Center, Tyler, Agricultural Health Center and the Southwest Center for Occupational and Environmental Health. She is a member of the NIOSH Board of Scientific CounselorsA. E.M.S. has received compensation from an institutional grant to the University of Texas Health Science Center at Houston School of Public Health, San Antonio Regional Campus. D.J.D. has received compensation from an institutional grant from the National Institutes of Health. C.J.C. has received funding/compensation from a grant to the University of Texas Health Science Center, Tyler. J.L. has ongoing grants with CDC/NIOSH and past institutional grants from the Association of Occupational and Environmental Clinics and the US Department of Labor, Solicitor’s Office. L.E.B. has no financial relationships to disclose and no conflicts of interest to report.
The authors thank the students who participated in the study, their teachers, and Weslaco ISDC staff. We thank Superintendent Richard Rivera, Principal Sue Peterson, Principal Isidoro Nieto, Linda Taormina (Migrant Education Program), Nurse Nora Trevino, Lety Martinez and the SHAC, Dr. Raymond Villarreal, Mary Mendoza, Sylvia Cavazos, all of the members of the Migrant Education Program staff, Yolanda Morado from the Starr County AgriLIfe Extension Service, Ricardo Reyna of People First of Texas, and former students Drs Christina Socias and Julie St. John for their support of this project.
Footnotes
Confirm whether board membership occurred.
The SMJ permits only 5 key words. Pls eliminate 2 from this list.
Is “within each school” correct? (Previously “within school”)
Define ISD.
Its contents are solely the responsibility of the authors and do not necessarily represent the official views of CDC/NIOSH or the National Institutes of Health.
References
- 1.Villarejo D. [Accessed July 24, 2015];Health-related inequities among hired farm workers and the resurgence of labor-intensive agriculture. http://kresge.org/library/health-related-inequities-among-hired-farm-workers-and-resurgence-labor-intensive-agricult-0. Published 2012.
- 2.Farmworker Justice. [Accessed July 21, 2015];Selected statistics on farmworkers. http://www.farmworkerjustice.org/sites/default/files/NAWS%20data%20factsht%201-13-15FINAL.pdf.
- 3.US Department of Education, Office of the Under Secretary. The same high standards for migrant students: holding Title 1 schools accountable. Volume II: measurement of migrant student educational achievement: final report. [Accessed July 24, 2015]; http://www.ed.gov/offices/OUS/PES/esed/title1-accountable/vol-ii.pdf. Published 2002.
- 4.Villarejo D. The health of U.S. hired farm workers. Annu Rev Public Health. 2003;24:175–193. doi: 10.1146/annurev.publhealth.24.100901.140901. [DOI] [PubMed] [Google Scholar]
- 5.Borre K, Ertle L, Graff M. Working to eat: vulnerability, food insecurity, and obesity among migrant and seasonal farmworker families. Am J Ind Med. 2010;53:443–462. doi: 10.1002/ajim.20836. [DOI] [PubMed] [Google Scholar]
- 6.Kilanowski JF, Moore LC. Food security and dietary intake in midwest migrant farmworker children. J Pediatr Nurs. 2010;25:360–366. doi: 10.1016/j.pedn.2009.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schlesselman JJ. Sample size requirements in cohort and case-control studies of disease. Am J Epidemiol. 1974;99:381–384. doi: 10.1093/oxfordjournals.aje.a121625. [DOI] [PubMed] [Google Scholar]
- 8.Texas Education Agency. [Accessed August 18, 2013];Education of migratory children. http://www.tea.state.tx.us/index4.aspx?id=4863&menu_id=798. Published 2012.
- 9.Barlow SE Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 10.Fernández JR, Redden DT, Pietrobelli A, et al. Waist circumference percentiles in nationally representative samples of African-American, European-American, and Mexican-American children and adolescents. J Pediatr. 2004;145:439–444. doi: 10.1016/j.jpeds.2004.06.044. [DOI] [PubMed] [Google Scholar]
- 11.King-Tryce K, Garza L, Ozias JM. Acanthosis nigricans and insulin resistance. Dis Prev News. 2002;62:1–4. [Google Scholar]
- 12.University of Texas-Pan Am Border Health Office. [Accessed August 19, 2015];The Texas Risk Assessment for Type 2 Diabetes in Children program: A Report to the Governor and the 82nd Legislature of the State of Texas. https://rfes.utpa.edu/resources/TRAT2DC_Legislative_Report_2011.pdf. Published 2011.
- 13.National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114(2 Suppl 4th Report):555–576. [PubMed] [Google Scholar]
- 14.Otto DE, Wang X, Tijerina SL, et al. A comparison of blood pressure, body mass index, and acanthosis nigricans in school-age children. J Sch Nurs. 2010;26:223–229. doi: 10.1177/1059840510365154. [DOI] [PubMed] [Google Scholar]
- 15.Urrutia-Rojas X, Egbuchunam CU, Bae S, et al. High blood pressure in school children: prevalence and risk factors. BMC Pediatr. 2006;6:32. doi: 10.1186/1471-2431-6-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shay CM, Ning H, Daniels SR, et al. Status of cardiovascular health in US adolescents: prevalence estimates from the National Health and Nutrition Examination Surveys (NHANES) 2005–2010. Circulation. 2013;127:1369–1376. doi: 10.1161/CIRCULATIONAHA.113.001559. [DOI] [PubMed] [Google Scholar]
- 17.Rosner B, Cook NR, Daniels S, et al. Childhood blood pressure trends and risk factors for high blood pressure: the NHANES experience 1988–2008. Hypertension. 2013;62:247–254. doi: 10.1161/HYPERTENSIONAHA.111.00831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ogden CL, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012;307:483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cote AT, Phillips AA, Harris KC, et al. Obesity and arterial stiffness in children: systematic review and meta-analysis. Arterioscler Thromb Vasc Biol. 2015;35:1038–1044. doi: 10.1161/ATVBAHA.114.305062. [DOI] [PubMed] [Google Scholar]
- 20.American Medical Association. [Accessed July 24, 2015];Obesity as a disease. http://www.ama-assn.org/ama/pub/news/news/2013/2013-06-18-new-ama-policies-annual-meeting.page. Published 2013.
- 21.Din-Dzietham R, Liu Y, Bielo MV, et al. High blood pressure trends in children and adolescents in national surveys, 1963 to 2002. Circulation. 2007;116:1488–1496. doi: 10.1161/CIRCULATIONAHA.106.683243. [DOI] [PubMed] [Google Scholar]
- 22.Freedman DS, Goodman A, Contreras OA, et al. Secular trends in BMI and blood pressure among children and adolescents: the Bogalusa Heart Study. Pediatrics. 2012;130:e159–e166. doi: 10.1542/peds.2011-3302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention. [Accessed July 24, 2015];National diabetes fact sheet. http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf. Published 2011.
- 24.American Diabetes Association. Standards of medical care in diabetes (position statement) Diabetes Care. 2006;29(Suppl 1):S4–S42. [PubMed] [Google Scholar]
- 25.Abraham C, Rozmus CL. Is acanthosis nigricans a reliable indicator for risk of type 2 diabetes in obese children and adolescents? A systematic review. J Sch Nurs. 2012;28:195–205. doi: 10.1177/1059840511430952. [DOI] [PubMed] [Google Scholar]
- 26.Harrell JS, Jessup A, Greene N. Changing our future: obesity and the metabolic syndrome in children and adolescents. J Cardiovasc Nurs. 2006;21:322–330. doi: 10.1097/00005082-200607000-00014. [DOI] [PubMed] [Google Scholar]
- 27.Moyer VA US Preventive Services Task Force. Screening for primary hypertension in children and adolescents: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2013;159:613–619. doi: 10.7326/0003-4819-159-9-201311050-00725. [DOI] [PubMed] [Google Scholar]
- 28.US Preventive Services Task Force. [Accessed August 19, 2015];Blood pressure in children and adolescents (hypertension): screening. http://www.uspreventiveservicestaskforce.org/uspstf/uspshypechld.htm.