Abstract
Objective:
We report our experience in diagnostic sensitivity of 3.0-T conventional MR vs 3.0-T MR arthrography of the hip for detection of acetabular labral tears and chondral defects in the same patient population.
Methods:
43 consecutive patients had both conventional hip MR and MR arthrography examinations performed. These examinations were reviewed retrospectively by independent reading of two musculoskeletal radiologists who read the MR and MR arthrogram examinations in a randomized fashion (i.e. MR and MR arthrogram examinations were read at separate sittings and in a randomized fashion so as not to bias reviewers). Scans were assessed for acetabular labral tears and chondral defects. All patients went on to arthroscopy.
Results:
Of these 43 patients, 40 had acetabular labral tears read by Reader 1 and 39 had acetabular labral tears read by Reader 2 on MR arthrogram, 39 had acetabular labral tears read by Reader 1 and 38 had acetabular labral tears read by Reader 2 on conventional MR examination. There were 42 labral tears in 43 patients at arthroscopy. There were four false-negative labral tears compared with arthroscopy on MR and three false negatives on MR arthrography for Reader 1 and five false negatives on MR and four false negatives on MR arthrography for Reader 2. Each reader had one false-positive labral tear compared with arthroscopy on both MR and MR arthrography. There were 32 acetabular chondral defects at arthroscopy. Reader 1 saw 21 acetabular chondral defects on conventional MR and 27 chondral defects at MR arthrography. Reader 2 saw 19 acetabular chondral defects at conventional MR and 25 acetabular chondral defects on MR arthrography. There were no false-positive readings of chondral defects compared with arthroscopy on MR and one false positive for Reader 1 and two false positives for Reader 2 on MR arthrography as compared with arthroscopy. On conventional MR examination, sensitivities and specificities as compared with arthroscopy were as follows: Reader 1 acetabular labral tear (90% sensitivity, 0% specificity) and Reader 2 acetabular labral tear (88% sensitivity, 0% sensitivity). On MR arthrogram, sensitivities and specificities as compared with arthroscopy for Reader 1 were 93%, 0% and for Reader 2 were 90%, 0%, respectively. Sensitivities and specificities for detection of acetabular chondral defects as compared with arthroscopy were Reader 1 conventional MR (65% sensitivity, 100% specificity), Reader 1 MR arthrography (81% sensitivity, 91% specificity), Reader 2 conventional MR (59% sensitivity, 100% specificity) and Reader 2 MR arthrography (71% sensitivity, 82% specificity).
Conclusion:
In this series, 3.0-T MR demonstrated sensitivity for detection of acetabular labral tears that rivals the sensitivity of 3.0-T MR arthrography of the hip. In this series, 3.0-T MR arthrography was more sensitive than conventional 3.0-T MR for detection of acetabular chondral defects.
Advances in knowledge:
3.0-T MR and MR arthrography are near equivalent in the diagnosis of acetabular labral tears. This information is useful for pre-operative planning.
MR arthrography has been reported to be more sensitive and specific for detection of acetabular labral tears in the hip than conventional MRI.1–10 MR arthrography has also been reported to be superior in detection of acetabular cartilage defects as compared with conventional MRI.11 To our knowledge 3.0-T MR vs 3.0-T MR arthrography sensitivity for detection of acetabular labral tears and chondral defects has not been specifically assessed.
To our knowledge, Petersilge et al1 first reported the utility of hip MR arthrography in the diagnosis of acetabular labral tears. Toomayan et al2 compared MR arthrography of the hip with conventional MRI of the hip in different patient populations. He found MR arthrography with a small field of view to be substantially more sensitive for detection of acetabular labral tears than conventional MRI. Sutter et al11 found 1.5 T MR arthrography to be superior to conventional MRI for detecting labral tears and acetabular cartilage defects.
Patients with acetabular labral tears present with symptoms of persistent pain, clicking, locking and decreased range of motion. With the availability of hip arthroscopy, labral tears can more easily be addressed with minimally invasive surgery. Accurate pre-operative identification of labral tears is needed.2 Based on previous studies demonstrating the accuracy of MR arthrography in detection of acetabular labral tears, surgeons often request MR arthrography of the hip to characterize labral tears prior to surgery.1–10 The purpose of this study is to assess 3.0-T MR vs MR arthrography diagnostic performance in detection of acetabular labral tears and chondral defects in the same patient population using arthroscopy as a reference standard.
METHODS AND MATERIALS
43 consecutive conventional hip MR and MR arthrography examinations performed between January 2013 and July 2013 on patients with hip pain who went on to arthroscopy were read retrospectively and independently by two musculoskeletal radiologists each with over 10 years' experience in reading musculoskeletal examinations. All patients were referred from one orthopaedic group. The three members of this orthopaedic group all had over 5 years' experience in performing hip arthroscopy. The age range of the 43 patients was 14–57 years (mean, 34 years). 28 patients were males and 15 patients were females. All patients had arthroscopy performed within 53 days of the MR examination (range 2–53 days, mean time between MR examination and arthroscopy was 18 days). Prospective MR and MR arthrogram reports were provided to the orthopaedic surgeons. The patients selected for arthroscopy had abnormal clinical examinations. Institutional Review Board approval was obtained for this retrospective review and correlation with surgical records.
All patients underwent MRI of the hip coronal, sagittal and axial planes on a 3-T GE Signa scanner (GE Healthcare, Milwaukee, WI). Coronal and sagittal fast spin echo T1 weighted [550/10 ms, repetition time (TR)/echo time (TE), number of excitations (NEX) of 3], coronal and sagittal fast spin echo fat-saturated T2 weighted (4100/55 ms, TR/TE, NEX of 3) and fast spin echo fat-saturated T2 weighted axial (3900/55 ms, TR/TE, NEX of 4) sequences with a field of view of 16 cm on all images were used. Slice thickness was 4 mm with a 10% interslice gap on all sequences. The echo train length was ten on all T2 weighted and three on the T1 weighted sequences. The bandwidth was 31.25 kHz on all sequences. The imaging time for the coronal and sagittal T2 weighted sequences was 3 min 51 s. The imaging time for the T2 weighted axial sequences was 4 min 18 s while the imaging time for the T1 weighted sequences was 3 min 16 s. The matrix for all T2 weighted sequences was 320 × 320, and the matrix for all T1 weighted sequences was 320 × 256. A USA Instruments (USA Instruments Inc., Aurora, OH) Torso PA 8 channel coil was used.
All 43 patients also had MR arthrography performed immediately following the conventional MR examination. We routinely perform pre- and post-arthrogram images in our institution. MR arthrography was performed with approximately 15 cc of a dilute MAGNEVIST®/saline mixture (Berlex Laboratories Inc., Wayne, NJ) with a concentration of 0.15 cc of MAGNEVIST per 20 cc of normal saline. A 22-gauge needle was placed in the hip joint via an anterior approach with the assistance of fluoroscopy. One of three musculoskeletal radiologists performed the injection. After injection of this mixture into the hip joint, the hip was exercised and T1 (TR 625 ms/TE 12 ms) fat-saturated coronal, sagittal and axial images were obtained. T1 (TR 625/TE 12) fat-saturated oblique coronal images were performed prior to MR arthrography for direct comparison with images after MR arthrography. The imaging time for each of the T1 weighted sequences was 2 min 36 s. All MR arthrography images were performed with a 16-cm field of view and a 4-mm slice thickness (with a 10% interslice gap). All other MR parameters (i.e. matrix and bandwidth) were the same as those for the conventional MR examinations.12
The hip arthroscopies were performed with the use of a fibre-optic device. The arthroscope was placed in the hip to assess the joint. During the arthroscope, it was determined whether there were labral tears. The tears found were either debrided or repaired depending on the type of tear. Definitions used in the arthroscopy reports were as follows. Recess was defined as a naturally occurring cleft or opening that is not pathologic or indicative of trauma. Tear was defined as a pathologic detachment of a structure from its natural origin or separation within the structure itself.12
All 43 patients had their MR examinations retrospectively reviewed by independent reading of two musculoskeletal radiologists. The readers were blinded to the results of arthroscopy at the time of review. Retrospective MR readings were then correlated with results in those patients who underwent arthroscopy (n = 43). The surgeons were aware of prospective MR interpretations prior to the patients undergoing arthroscopy. The conventional MR examinations and MR arthrograms were reviewed in a random order so as not to bias the reviewers. The MR arthrograms were reviewed along with T2 weighted fat-saturated MR sequences in all three planes. Reviewers were blinded to names of the patients, prospective MR reports and arthroscopy results.
MR criteria used for diagnosis of labral tear were a detached labrum, a partial or full thickness cleft of increased T2 weighted signal intensity in the labrum or distortion of the labrum from the normal triangular morphologic configuration resulting in an enlarged, small or irregular shape or detachment. These are the criteria as set forth by Ziegert et al.13
The images were assessed for the presence or absence of acetabular labral tears. The acetabular labral tears were not graded: i.e. on retrospective review images were not graded for high or low grade, large or small or detached or non-detached labral tears but rather simply whether such lesions were present or not. On retrospective review, positive findings were described when the observer could definitively diagnose a labral tear based on the images provided. On completion of the retrospective review, the discordant MR and MR arthrography readings were analysed.
Acetabular chondral defects were identified on the MR images on the basis of morphologic and signal changes in a defined cartilage surface that suggested either focal thinning or discontinuity of the cartilage or a lack of definable hyaline cartilage on the surface being evaluated.14 Chondral defects were not graded: i.e. on retrospective review images were not graded for high or low grade chondral defects.
Statistical analysis
The sensitivity and specificity of MR and MR arthrograms for detection of acetabular labral tears and acetabular chondral defects as compared with arthroscopy were calculated. The true and false positives and negatives as compared with arthroscopy were calculated for both MR and MR arthrography.
Interreader agreement was tested by using Cohen's kappa coefficient. The κ values of ≤0 indicate poor agreement, 0.01–0.20 indicate slight agreement, 0.21–0.40 indicate fair agreement, 0.41–0.60 indicate moderate agreement, 0.61–0.80 indicate substantial agreement and 0.81–1.00 indicate almost perfect agreement. All analyses were performed by using a program provided by Google Docs (Google Inc., Mountain View, CA, https://docs.google.com).
p-values for sensitivity for labral tears and chondral defects for Reader 1 and 2 compared with arthroscopy were calculated. The comparison of sensitivities was performed using the McNemar test.
RESULTS
Of these 43 patients, 40 had acetabular labral tears read by Reader 1 and 39 had acetabular labral tears read by Reader 2 on MR arthrogram, 39 had acetabular labral tears read by Reader 1 and 38 had acetabular labral tears read by Reader 2 on conventional MR examination. There were 42 labral tears in 43 patients at arthroscopy (Figures 1–5) (Table 1).
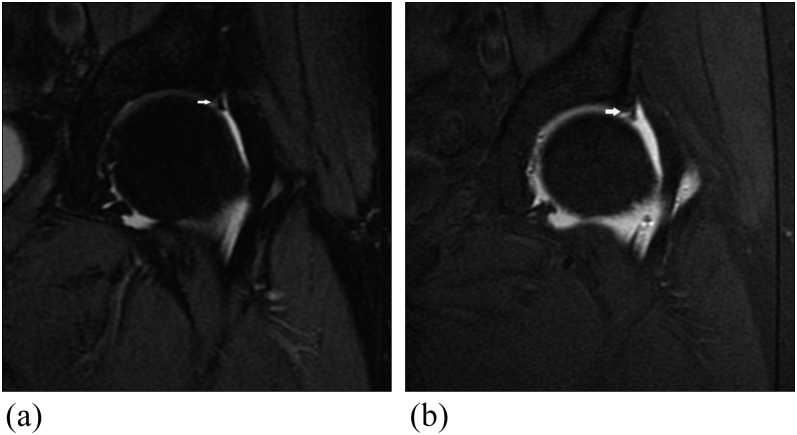
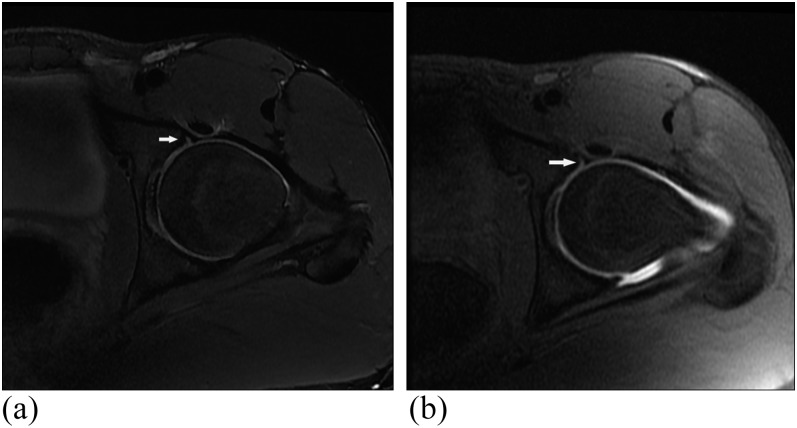
Figure 1.
30-year-old male with hip pain. (a) T2 weighted coronal MR image [3250/55 ms, repetition time (TR)/echo time (TE)] shows acetabular labral tear (arrow). (b) T1 weighted fat-saturated coronal MR arthrogram image (677/12 ms, TR/TE) shows acetabular labral tear (arrow). This was confirmed arthroscopically.
Figure 5.
41-year-old male with hip pain. (a) T2 weighted sagittal MR image [3850/55 ms, repetition time (TR)/echo time (TE)] was read as intact acetabular labrum by both readers (arrow). (b) T1 weighted fat-saturated sagittal MR arthrogram image (677/12 ms, TR/TE) shows acetabular labral tear (arrow). An acetabular labral tear was confirmed on arthroscopy.
Table 1.
MR and MR arthography acetabular labral tears compared with arthroscopy
| Labral tear | Labral tears | True positive | True negative | False positive | False negative | Sensitivity compared with arthroscopy (%) | Specificity compared with arthroscopy (%) |
|---|---|---|---|---|---|---|---|
| Tear on arthroscopy | 42 | 42 | 1 | 0 | 0 | 100 | 100 |
| Tear on 3.0-T MR Reader 1 | 39 | 38 | 0 | 1 | 4 | 90 | 0 |
| Tear on 3.0-T MR Reader 2 | 38 | 37 | 0 | 1 | 5 | 88 | 0 |
| Tear on 3.0-T MR arthrogram Reader 1 | 40 | 39 | 0 | 1 | 3 | 93 | 0 |
| Tear on 3.0-T MR arthrogram Reader 2 | 39 | 38 | 0 | 1 | 4 | 90 | 0 |
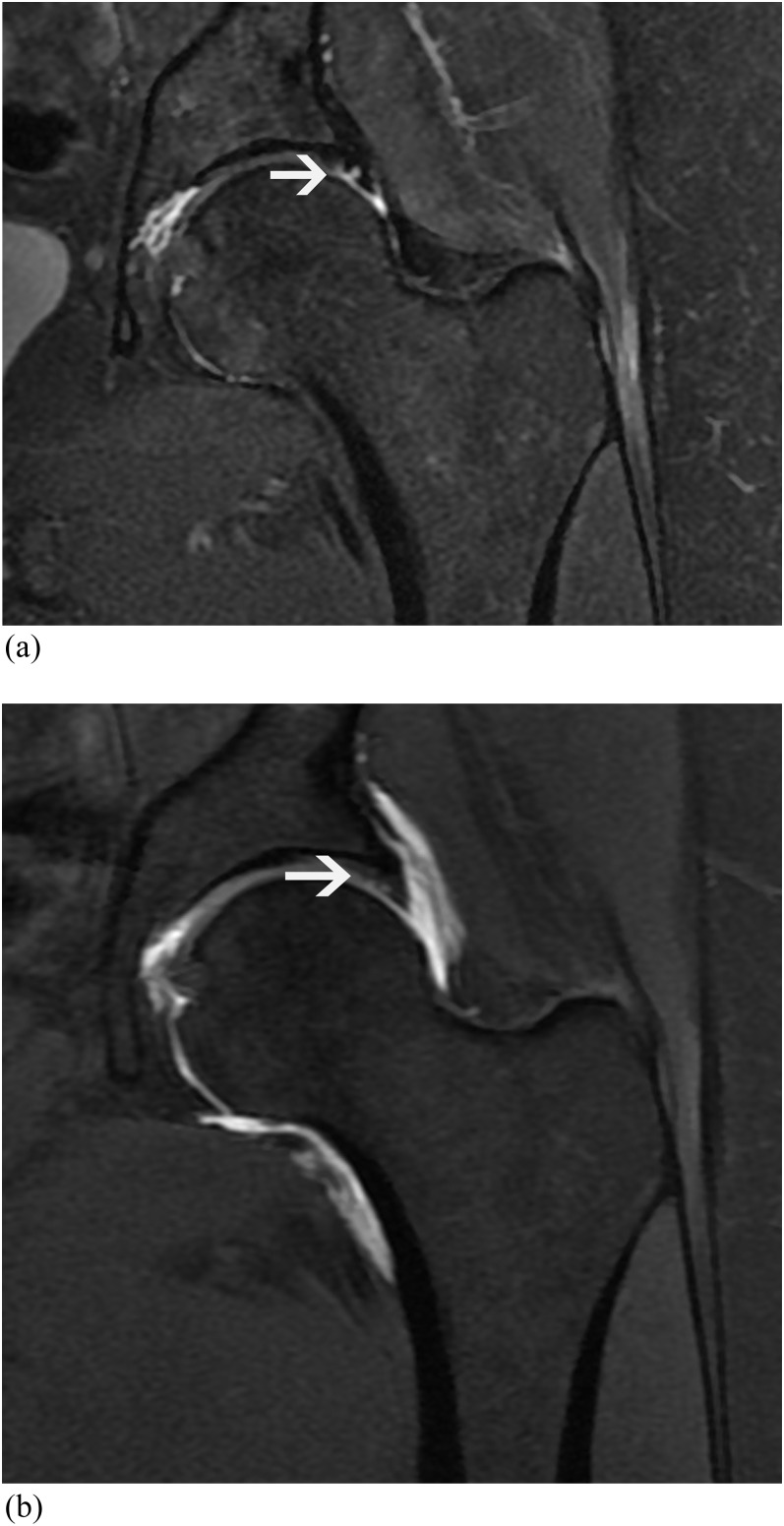
Figure 4.
46-year-old male with hip pain. (a) T2 weighted coronal MR image [3850/55 ms, repetition time (TR)/echo time (TE)] shows acetabular labral tear (arrow). (b) T1 weighted fat-saturated coronal MR arthrogram image (677/12 ms, TR/TE). Acetabular labral tear is less well seen on arthrogram images than on conventional MR images (arrow). Both readers described this as an acetabular labral tear on both MR and MR arthrography. An acetabular labral tear was confirmed on arthroscopy.
There were four false-negative labral tears compared with arthroscopy on MR and three false negatives on MR arthrography for Reader 1 and five false negatives on MR and four false negatives on MR arthrography for Reader 2 (Figure 2). Each reader had one false-positive labral tear compared with arthroscopy on both MR and MR arthrography (Figure 3) (Table 1). The patient with additional findings on MR arthrography as compared with conventional MR examination had arthroscopic correlation that confirmed MR arthrography findings.
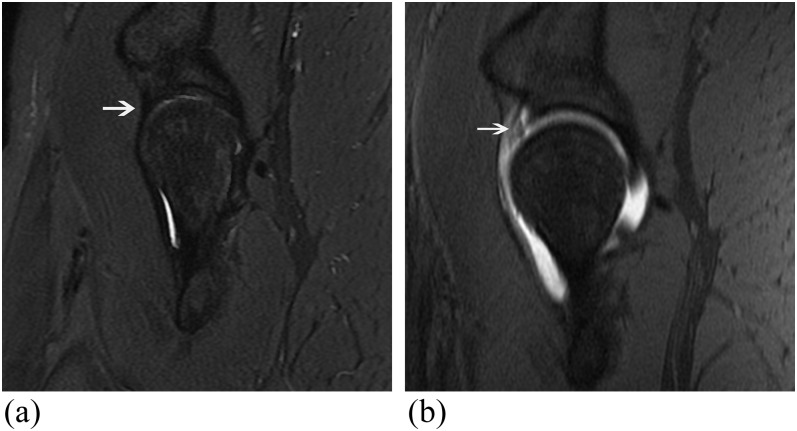
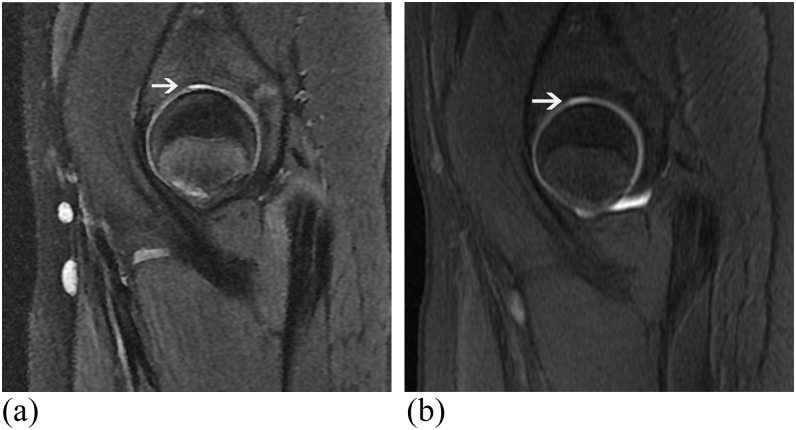
Figure 2.
24-year-old male with hip pain. (a) T2 weighted coronal MR image [3850/55 ms, repetition time (TR)/echo time (TE)] shows acetabular labrum read as normal by both readers (arrow). A tear of the lateral aspect of the acetabular labrum was seen at arthroscopy. No tear was seen on further retrospective review. (b) T1 weighted fat-saturated axial MR arthrogram image (677/12 ms, TR/TE) shows acetabular labrum read as normal by both readers (arrow). A tear of the lateral aspect of the acetabular labrum was seen at arthroscopy. No tear was seen on further retrospective review.
Figure 3.
38 year-old male with hip pain. (a) T2 weighted axial MR image [3850/55 ms, repetition time (TR)/echo time (TE)] shows findings described as torn acetabular labrum by both readers (arrow). (b) T1 weighted fat-saturated axial MR arthrogram image (677/12 ms, TR/TE) shows findings described as torn acetabular labrum by both readers (arrow). No tear was found at arthroscopy.
On conventional MR examination, sensitivities and specificities as compared with arthroscopy were as follows: Reader 1 acetabular labral tear (90% sensitivity, 0% specificity) and Reader 2 acetabular labral tear (88% sensitivity, 0% specificity). On MR arthrogram, sensitivities and specificities as compared with arthroscopy for Reader 1 were 93%, 0% and for Reader 2 were 90%, 0%, respectively (Table 1).
There were 32 acetabular chondral defects at arthroscopy. Reader 1 saw 21 acetabular chondral defects on conventional MR and 27 chondral defects at MR arthrography. Reader 2 saw 19 acetabular chondral defects at conventional MR and 25 acetabular chondral defects on MR arthrography. There were no false-positive readings of chondral defects compared with arthroscopy on MR and one false positive for Reader 1 and two false positives for Reader 2 on MR arthrography as compared with arthroscopy (Figures 6–8) (Table 2).
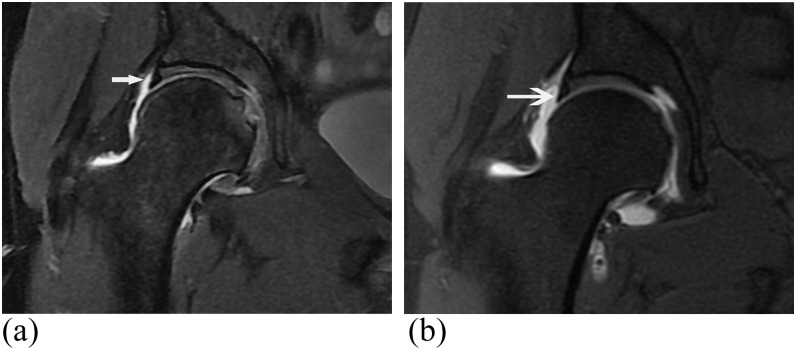
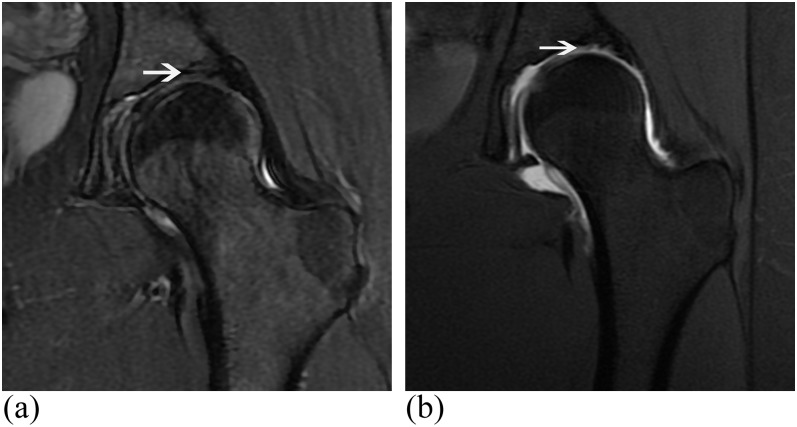
Figure 6.
27-year-old male with hip pain. (a) T2 weighted sagittal MR image [3850/55 ms, repetition time (TR)/echo time (TE)] was read as acetabular chondral defect (arrow). (b) T1 weighted fat-saturated sagittal MR arthrogram image (677/12 ms, TR/TE) was read as acetabular chondral defect (arrow). This was confirmed on arthroscopy.
Figure 8.
16-year-old male with hip pain. (a) T2 weighted sagittal MR image [3850/55 ms, repetition time (TR)/echo time (TE)] shows findings described as normal appearing acetabular articular cartilage by both readers (arrow). (b) T1 weighted fat-saturated sagittal MR arthrogram image (677/12 ms, TR/TE) shows findings described as an acetabular chondral defect by both readers (arrow). No chondral defect was found at arthroscopy. This was a false positive as compared with arthroscopy for the MR arthrogram.
Table 2.
MR and MR arthrography detection of acetabular chondral defects compared with arthroscopy
| Acetabular chondral defect | Acetabular chondral defects | True positive | True negative | False positive | False negative | Sensitivity compared with arthroscopy (%) | Specificity compared with arthroscopy (%) |
|---|---|---|---|---|---|---|---|
| Defect on arthroscopy | 32 | 32 | 11 | 0 | 0 | 100 | 100 |
| Defect on 3.0-T MR Reader 1 | 21 | 21 | 11 | 0 | 11 | 65 | 100 |
| Defect on 3.0-T MR Reader 2 | 19 | 19 | 11 | 0 | 13 | 59 | 100 |
| Defect on 3.0-T MR arthrogram Reader 1 | 27 | 26 | 10 | 1 | 6 | 81 | 91 |
| Defect on 3.0-T MR arthrogram Reader 2 | 25 | 23 | 9 | 2 | 9 | 71 | 82 |
Sensitivities and specificities for detection of acetabular chondral defects as compared with arthroscopy were Reader 1 conventional MR (65% sensitivity, 100% specificity), Reader 1 MR arthrography (sensitivity 81%, specificity 91%), Reader 2 conventional MR (59% sensitivity, 100% specificity) and Reader 2 MR arthrography (71% sensitivity, 82% specificity) (Table 2).
Kappa values comparing agreement of Readers 1 and 2 were as follows: labral tear on MR (κ = 0.876), labral tear on MR arthrography (κ = 0.845), chondral defect on MR (κ = 0.907) and chondral defect on MR arthrography (κ = 0.806). Kappa values indicated almost perfect agreement between readers for labral tears on MR and MR arthrography and for chondral defects on MR. There was substantial agreement between readers for chondral defects on MR arthrography.
p-values for sensitivity for labral tears and chondral defects for Reader 1 and 2 compared with arthroscopy were as follows: sensitivity for labral tears Reader 1 p-value = 1, sensitivity for labral tears Reader 2 p-value = 1, sensitivity for chondral defects Reader 1 p-value = 0.125 and sensitivity for chondral defects Reader 2 p-value = 0.063. The differences in sensitivity were not statistically significant. There were not enough negative cases for adequate p-value testing for specificity.
DISCUSSION
There is a high prevalence of positive findings on conventional hip MR and MR arthrography examination in patients with hip pain. Labral tears are secondary to traumatic injury or degeneration of the labrum. They are most commonly seen in patients aged 20–50 years of age. Most labral tears are located anterior superiorly or posterior superiorly.1,2
Patients with labral tears present with hip pain, decreased range of motion, snapping or clicking and locking. Labral tears are associated with acetabular dysplasia, femoral acetabular impingement, legg calve perthes, slipped capital femoral epiphysis and degenerative hip disease.1,2,4
Previous studies have indicated that MR arthrography provides superior accuracy in the detection of acetabular labral tears as compared with conventional MRI.1–10 With MR arthrogram, intra-articular contrast extends into the labral tear allowing separation of the torn labrum from the acetabular articular cartilage. Czerny et al5 demonstrated a sensitivity of 91% and a specificity of 71% in detection of acetabular labral tears by MR arthrography as compared with surgery.
The results of this study compare favourably with previously performed studies in assessment of sensitivity for detection of acetabular labral tears by both MR and MR arthrogram. Toomayan et al2 compared MR arthrography with conventional MR in two different populations. They found conventional MR sensitivity for detection of acetabular labral tears to be 25% as compared with arthroscopy while MR arthrogram sensitivity was 92% compared with arthroscopy. This study was limited in that some patients had open field of view imaging to include both hips, the patients who had MR arthrograms were not the same patients who had conventional MR examinations, and the study was not performed on 3.0-T MR systems.
Sutter et al11 compared conventional MR vs MR arthrography at 1.5 T. They found MR arthrography to be superior to conventional MRI for detecting labral tears and acetabular cartilage defects. In the present study, MR and MR arthrography had similar accuracy for detection of acetabular labral tears but there was increased accuracy in detection of chondral defects with the use of MR arthrography. In the present study, 3.0-T MRI was used as compared with 1.5 T MRI. 3.0-T MRI allows for higher resolution imaging than 1.5 T MRI. Labral tears may be more easily seen on conventional 3.0-T imaging owing to the higher resolution as compared with 1.5 T MRI. Chondral defects may be very difficult to visualize at any resolution unless intra-articular contrast extends into the chondral defect. In Sutter's study, there was a time delay between MR and MR arthrograms of as much as 3.5 months. This time delay allows for the possibility of more advanced lesions or new lesions being present on the images performed at a later time. In the present study, the MR and MR arthrograms were performed on the same day.
Ziegert et al13 retrospectively analysed MR arthrograms of the hip for detection of acetabular labral tears compared with arthroscopy. In this study of 189 patients, MR arthrography was 97% sensitive as compared with arthroscopy. Conventional MRI was not assessed in this study.
In the present study, conventional 3.0-T MR examination was near equivalent to 3.0-T MR arthrography for detection of acetabular labral tears. In only one patient did MR arthrography allow for detection of an acetabular labral tear not seen on conventional MR examination (Figure 5). Intra-articular contrast extension into an area of labral tear can allow for accurate diagnosis of a labral tear. In this study, small field of view 3.0-T conventional MRI provided high-resolution images that allowed the diagnosis of an acetabular labral tear in all but one patient.
In this study, acetabular chondral defects were difficult to visualize on both 3.0-T conventional MR and MR arthrography examinations. Acetabular chondral defects can be very difficult to visualize owing to the narrow thickness of the cartilage. In this study, intra-articular contrast did allow for more sensitive detection of acetabular chondral defects. This most likely is owing to the need for intra-articular-injected contrast to fill in the areas of chondral defect in order to see the defect in some cases (Figure 7). The high signal of the contrast on T1 fat-saturated images highlights the areas of chondral defect. However, in many cases the chondral defects could not be visualized despite the intra-articular injection of contrast.
Figure 7.
34-year-old male with hip pain. (a) T2 weighted coronal MR image [3850/55 ms, repetition time (TR)/echo time (TE)] shows normal appearing acetabular articular cartilage (arrow). (b) T1 weighted fat-saturated coronal MR arthrogram image (677/12 ms, TR/TE) shows an acetabular chondral defect (arrow). This was confirmed on arthroscopy.
In this study, there was a high prevalence of positive findings on both MR and MR arthrography. This is partly owing to a selection bias owing to a high threshold for the surgeon to perform hip surgery. Another selection bias is that all but four patients who went on to arthroscopy had at least one abnormal finding on MR arthrography. Therefore, some potential false-negative MR arthrograms were not assessed.
CONCLUSIONS
In this series 3.0-T MR demonstrated sensitivity for detection of acetabular labral tears as compared with arthroscopy that rivals the sensitivity of 3.0-T MR arthrography of the hip. 3.0-T conventional MR of the hip may be sufficient for pre-operative planning of acetabular labral repair. There was increased sensitivity and specificity for detection of chondral defects in the acetabulum at 3.0-T MR arthrogram imaging as compared with conventional 3.0-T MRI.
Acknowledgments
ACKNOWLEDGMENTS
I would like to acknowledge Dr Lawrence Yao for help with statistical analysis.
REFERENCES
- 1.Petersilge CA, Haque MA, Petersilge WJ, Lewin JS, Lieberman JM, Buly R. Acetabular labral tears: evaluation with MR arthrography. Radiology 1996; 200: 231–5. doi: 10.1148/radiology.200.1.8657917 [DOI] [PubMed] [Google Scholar]
- 2.Toomayan GA, Holman WR, Major NM, Kozlowicz SM, Vail TP. Sensitivity of MR arthrography in the evaluation of acetabular labral tears. AJR Am J Roentgenol 2006; 186: 449–53. doi: 10.2214/AJR.04.1809 [DOI] [PubMed] [Google Scholar]
- 3.Hodler J, Yu JS, Goodwin D, Haghighi P, Trudell D, Resnick D. MR arthrography of the hip: improved imaging of the acetabular lagrum with histologic correlation in cadavers. AJR Am J Roentgenol 1995; 165: 887–91. doi: 10.2214/ajr.165.4.7676987 [DOI] [PubMed] [Google Scholar]
- 4.Petersilge CA. From the RSNA Refresher Courses. Radiological Society of North America. Chronic adult hip pain: MR arthrography of the hip. Radiographics 2000; 20: S43–52. doi: 10.1148/radiographics.20.suppl_1.g00oc12s43 [DOI] [PubMed] [Google Scholar]
- 5.Czerny C, Hoffman S, Newhold A, Tschauner C, Engel A, Recht MP, et al. Lesions of the acetabular labrum: accuracy of MR imaging and MR arthrography in detection and staging. Radiology 1996; 200: 225–30. doi: 10.1148/radiology.200.1.8657916 [DOI] [PubMed] [Google Scholar]
- 6.Studler U, Kalberer F, Leunig M, Zanetti M, Hodler J, Dora C. MR arthrography of the hip: differentiation between an anterior sublabral recess as a normal variant and a labral tear. Radiology 2008; 249: 947–54. doi: 10.1148/radiol.2492080137 [DOI] [PubMed] [Google Scholar]
- 7.Blankenbaker DG, Tuite MJ. Acetabular Labrum. Magn Reson Imaging Clin N Am 2013; 21: 21–33. doi: 10.1016/j.mric.2012.09.006 [DOI] [PubMed] [Google Scholar]
- 8.Thomas JD, Li Z, Agur AM, Robinson P. Imaging of the acetabular labrum. Semin Musculoskelet Radiol 2013; 17: 248–57. doi: 10.1055/s-0033-1348091 [DOI] [PubMed] [Google Scholar]
- 9.Chan YS, Lien LC, Hsu HL, Wan YL, Lee MS, Hsu KY, et al. Evaluating hip labral tears using magnetic resonance arthrography: a prospective study comparing hip arthroscopy and magnetic resonance arthrography diagnosis. Arthroscopy 2005; 21: 1250. [DOI] [PubMed] [Google Scholar]
- 10.Petersilge CA. MR arthrography for evaluation of the acetabular labrum. Skeletal Radiol 2001; 30: 423–30. doi: 10.1007/s0025610300423 [DOI] [PubMed] [Google Scholar]
- 11.Sutter R, Zubler V, Hoffmann A, Saupe NM, Dora C, Kalberer F, et al. Hip MRI: how useful is intraarticular contrast material for evaluating surgically proven lesions of the labrum and articular cartilage? AJR Am J Roentgenol 2014; 202: 160–9. doi: 10.2214/AJR.12.10266 [DOI] [PubMed] [Google Scholar]
- 12.Magee T. 3-T MRI of the shoulder: is MR arthrography necessary? AJR Am J Roentgenol 2009; 192: 86–92. doi: 10.2214/ajr.192.5_supplement.0a86 [DOI] [PubMed] [Google Scholar]
- 13.Ziegert AJ, Blankenbaker DG, De Smet AA, Keene JS, Shinki K, Fine J. Comparison of standard hip MR arthrographic imaging planes and sequences for detection of arthroscopically proven labral tear. AJR Am J Roentgenol 2009; 192: 1397–400. doi: 10.2214/AJR.08.1609 [DOI] [PubMed] [Google Scholar]
- 14.Sonin AH, Pensy RA, Mulligan ME, Hatem S. Grading articular cartilage of the knee using fast spin-echo proton density-weighted MR imaging without fat supression. AJR Am J Roentgenol 2002; 179: 1159–66. doi: 10.2214/ajr.179.5.1791159 [DOI] [PubMed] [Google Scholar]