Abstract
Objectives
To quantify the risk of burn injury associated with home oxygen use and to examine the risk factors associated with the development of this injury.
Patients and Methods
We used a nested case-control and a retrospective cohort design to study enrollment and claims data from a national sample of Medicare beneficiaries 66 years and older with a diagnosis of chronic obstructive pulmonary disease (COPD) from January 1, 2001, through December 31, 2010. The primary outcome was burn injury in patients with COPD prescribed home oxygen.
Results
In the nested case-control method, patients with burn injury were twice (odds ratio, 2.43; 95% CI, 1.57–3.78) as likely to be prescribed oxygen in the preceding 90 days compared with those without burn injury. In the retrospective cohort study, the absolute risk of burn injury in patients prescribed oxygen therapy was 2.98 per 1000 patients compared with 1.69 per 1000 patients not prescribed oxygen during a 22-month period. The excess risk of a burn injury associated with oxygen was 0.704 per 1000 patients per year, and the number needed to harm was 1421. In multivariable analysis, factors associated with burn injury included male sex, low socioeconomic status, oxygen therapy use, and the presence of 3 or more comorbidities.
Conclusion
The benefits of oxygen therapy in patients with COPD outweigh the modest risk of burn injury associated with home oxygen use. However, with the increasing number of patients being prescribed oxygen, health care professionals must educate and counsel patients regarding the potential risk of burn injury.
Thirty-five years ago, 2 multicenter trials reported substantial improvements in survival and quality of life with continuous oxygen therapy in the treatment of severe hypoxemia associated with chronic obstructive pulmonary disease (COPD).1,2 Aside from smoking cessation, no other medical intervention therapy has improved survival for patients with COPD.3 As a result, oxygen therapy to treat hypoxemia associated with COPD has been widely adopted.4–8 Currently, oxygen is prescribed to an estimated 1 million Medicare beneficiaries at an annual cost of $2.9 billion.6
The risks of home oxygen therapy that have garnered the most consideration are hypercapnia and oxygen toxicity.9 Home oxygen is provided by 3 delivery systems: oxygen concentrator, compressed oxygen cylinder, and liquid oxygen. All can supply an oxygen concentration of 90% or more to the individual and enrich the local environment. Oxygen enrichment with a heat source or flame provides the needed elements to ignite a fire. The association between cigarette use and oxygen therapy has been described in case series from tertiary care burn centers, but quantitative risk estimates have not been reported.10–14 Physicians prescribing oxygen to patients with COPD struggle to balance the benefits (in the form of improved survival and quality of life) with the risk of fire hazard in patients who continue to smoke. In some countries, oxygen is not prescribed to current smokers, but in the United States there is no clear policy regarding the prescription of oxygen to an actively smoking individual. Moreover, the number of active smokers prescribed oxygen has been estimated to be 15% to 25%.15–17 To determine the scope of this issue, we examined the hazard of burn injury in patients with COPD receiving home oxygen and evaluated the factors associated with the risk of burn injury in a national sample of Medicare beneficiaries.
METHODS
Data Source
We used enrollment and claims data from a 5% national sample of Medicare beneficiaries from January 1, 2001, through December 31, 2010. More than 98% of adults in the United States 65 years or older are enrolled in Medicare, which comprises more than 45 million beneficiaries. In the past, the Centers for Medicare & Medicaid Services selected a random sample of 5% Medicare beneficiaries on the basis of the eighth and ninth digits (05, 20, 45, 70, and 95) of their health insurance claim number for research purposes because this sample is representative of the entire cohort.18,19
Data from multiple files were used for this study, including (1) Centers for Medicare & Medicaid Services entitlement information, (2) Medicare Provider Analysis and Review File, (3) hospital outpatient services, (4) 100% Physician/Supplier File (physician and other medical services), and (5) Durable Medical Equipment (DME) file.18,19 Demographic characteristics of patients were determined from enrollment files and hospital admission data (eg, diagnosis-related group from the Medicare Provider Analysis and Review File). The study was approved by the University of Texas Medical Branch Institutional Review Board, and written informed consent was not deemed necessary because of the nature of the study.
Study Cohort
We identified beneficiaries 66 years and older who were enrolled in Medicare Parts A and B for the entire year, were not enrolled in a health maintenance organization plan, and were not residents of a nursing facility. Patients with COPD were identified by one of the following: (1) 2 or more outpatient visits at least 30 days apart within 1 year noted by Evaluation and Management codes 99201 through 99205 or 99211 through 99215 with an encounter diagnosis of COPD on the basis of International Classification of Diseases, Ninth Revision (ICD-9) codes (491.X, 492.X, or 496.X), (2) an acute care hospitalization with COPD as the primary discharge diagnosis, and/or (3) an acute care hospitalization for respiratory failure (ICD-9 codes 518.81, 518.82, or 518.84) as the primary discharge diagnosis and COPD listed as the secondary diagnosis. Individuals with a burn injury were identified through an emergency department visit or hospital encounter with primary or secondary ICD-9 codes of 940.XX through 949.XX. Assessment of the risk of a burn injury in patients with COPD was performed using a nested case-control study and a retrospective cohort study.
Nested Case-Control Study
The nested case-control study allowed estimation of the risk of burn injury associated with oxygen use during a short-term period in a well-matched cohort. Index patients had an emergency department visit or hospitalization for a burn injury. Each index patient was matched with 3 controls by age ±5 years, sex, race, year of COPD diagnosis, region, socioeconomic status, and comorbidity count.20 The first recorded burn injury was defined as the index date for the cases and matched controls. We identified 685 patients with COPD who sustained a burn injury from January 1, 2001, through December 31, 2010, and matched this cohort to 2055 patients with COPD without a burn injury during this period. Oxygen therapy use was on the basis of Healthcare Common Procedure Coding System codes E1390, E1391, or E1392 from DME file claims submitted within 90 days of the index date. For patients who had a burn injury, we determined the site of injury21 and examined 30-day mortality.
Retrospective Cohort Study
This study design assessed the absolute risk of burn injury with oxygen use during a follow-up period. For each patient, we selected the first calendar year in which COPD was diagnosed in the study period. Exposure to oxygen was defined as a patient with COPD with claims for oxygen therapy in the first 2 months (January and February) of the calendar year who was followed up for 22 subsequent months for a burn injury. Oxygen therapy use was on the basis of Healthcare Common Procedure Coding System codes E1390, E1391, or E1392 from DME file claims submitted for the 2 consecutive months of January and February of a given calendar year.
Variables
Patient demographic characteristics were obtained from the denominator file and included the following: age (66–74, 75–84, or ≥85 years), sex, race (white or nonwhite), and 9 US geographic regions (New England, Middle Atlantic, East North Central, West North Central, South Atlantic, East South Central, West South Central, Mountain, and Pacific). Socioeconomic status was on the basis of whether the patient was eligible for state buy-in coverage provided by the Medicaid program for at least 1 month during the index year. Comorbidities were assessed with the number of comorbidities (0, 1, 2, or ≥3) using all Medicare inpatient and outpatient claims for the 365 days before the index date.
Statistical Analyses
For the nested case-control study, patient characteristics were expressed as mean ± SD for continuous variables and as percentages for categorical variables. Comparison of categorical variables was performed using the χ2 test. Conditional logistic regression was performed to examine the association between exposure to oxygen in the preceding 90 days and a burn injury.
For the retrospective cohort study, the risk of burn injury during a 22-month follow-up period was determined for patients prescribed oxygen and patients not prescribed oxygen using the failure rate from the product-limit estimation. Cox proportional hazards analysis was performed to estimate the risk of oxygen use on burn injury adjusted for age, sex, race, Medicaid eligibility, comorbidities, and year. In this analysis, patients were censored at death, change in oxygen use status, or the end of the 22-month follow-up. Analysis was performed with SAS statistical software, version 9.2 (SAS Institute Inc), and statistical significance was 2-sided with P<.05.
RESULTS
Case-Control Study
From 2001 through 2010, a total of 685 patients with COPD had an emergency department encounter or hospitalization for a burn injury. The index patients were well matched with 2055 patients with COPD and no burn injury (Table 1). Patients with a burn injury were more likely to have been prescribed oxygen therapy in the preceding 90 days compared with the controls (40.73% vs 25.06%; P<.001).
TABLE 1.
Baseline Characteristics of Cases With a Burn Injury and Matched Controls From a Sample of Patients With Chronic Obstructive Pulmonary Disease From 2001 Through 2010a
| Characteristic | Cases (n=685) | Controls (n=2055) | P value |
|---|---|---|---|
| Age, mean (SD), y | 75.26 (5.91) | 74.80 (6.24) | .09 |
|
| |||
| Age group, y | .73 | ||
| 66–74 | 348 (50.80) | 1079 (52.51) | |
| 75–84 | 281 (41.02) | 818 (39.81) | |
| ≥85 | 56 (8.18) | 158 (7.69) | |
|
| |||
| Sex | >.99 | ||
| Female | 337 (49.20) | 1011 (49.20) | |
| Male | 348 (50.80) | 1044 (50.80) | |
|
| |||
| Race | >.99 | ||
| White | 623 (90.95) | 1869 (90.95) | |
| Nonwhite | 62 (9.05) | 186 (9.05) | |
|
| |||
| Year of diagnosis | >.99 | ||
| 2001 | 26 (3.80) | 78 (3.80) | |
| 2002 | 45 (6.57) | 135 (6.57) | |
| 2003 | 54 (7.88) | 162 (7.88) | |
| 2004 | 91 (13.28) | 273 (13.28) | |
| 2005 | 83 (12.12) | 249 (12.12) | |
| 2006 | 79 (11.53) | 237 (11.53) | |
| 2007 | 68 (9.93) | 204 (9.93) | |
| 2008 | 64 (9.34) | 192 (9.34) | |
| 2009 | 66 (9.64) | 198 (9.64) | |
| 2010 | 109 (15.91) | 327 (15.91) | |
|
| |||
| Region | >.99 | ||
| New England | 36 (5.26) | 108 (5.26) | |
| Middle Atlantic | 82 (11.97) | 246 (11.97) | |
| East North Central | 121 (17.66) | 363 (17.66) | |
| West North Central | 52 (7.59) | 156 (7.59) | |
| South Atlantic | 141 (20.58) | 423 (20.58) | |
| East South Central | 72 (10.51) | 216 (10.51) | |
| West South Central | 77 (11.24) | 231 (11.24) | |
| Mountain | 29 (4.23) | 87 (4.23) | |
| Pacific | 71 (10.36) | 213 (10.36) | |
| Unknown | 4 (0.58) | 12 (0.58) | |
|
| |||
| No. of comorbidities | >.99 | ||
| 0 | 96 (14.01) | 288 (14.01) | |
| 1 | 115 (16.79) | 345 (16.79) | |
| 2 | 119 (17.37) | 357 (17.37) | |
| ≥3 | 355 (51.82) | 1065 (51.82) | |
|
| |||
| Low socioeconomic status | >.99 | ||
| No | 477 (69.64) | 1431 (69.64) | |
| Yes | 208 (30.36) | 624 (30.36) | |
|
| |||
| Oxygen therapy in previous 90 days | <.001 | ||
| Yes | 279 (40.73) | 515 (25.06) | |
| No | 406 (59.27) | 1540 (74.94) | |
Data are presented as No. (percentage) of study participants unless otherwise indicated.
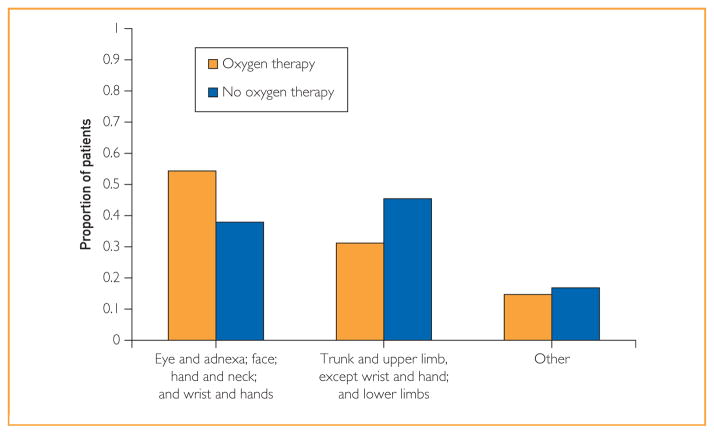
As shown in Figure 1, for patients with a burn injury who had been prescribed oxygen, the region most frequently involved was the face, head, and neck (54.25%) compared with burned patients not prescribed oxygen (37.83%). In a multivariable conditional logistic regression analysis, the odds of patients being prescribed oxygen in the preceding 90 days of burn injury were 2.43 (95% CI, 1.57–3.78) compared with those without a burn injury. The 30-day mortality rate was 4.82% for burned patients who had been prescribed oxygen vs 0.49% for burned patients not prescribed oxygen therapy (P<.001). In a logistic regression analysis, patients with COPD and a burn injury had an unadjusted odds of death within 30 days of 10.35 (95% CI, 5.07–21.12) compared with those without a burn injury.
FIGURE 1.
Distribution of burn injury sites in patients with chronic obstructive pulmonary disease by oxygen therapy use in the preceding 90 days, 2001–2010.
Retrospective Cohort Study
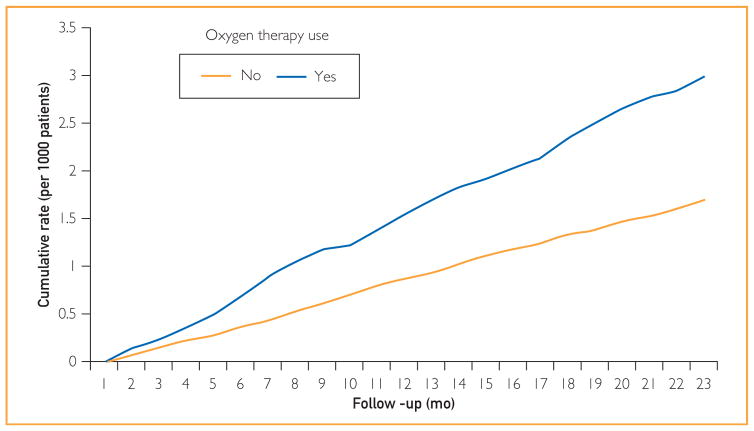
To estimate the absolute risk of burn injury in patients prescribed oxygen, we performed a retrospective cohort analysis study. Patients prescribed oxygen or not for the first 2 months of the calendar year were followed up for the subsequent 22 months to determine the occurrence of a burn injury. As shown in Figure 2, at the end of the 22-month follow-up, the risk of burn injury in patients prescribed oxygen therapy was 2.98 per 1000 patients compared with 1.69 per 1000 patients for those not prescribed oxygen in the first 2 months of the calendar year.
FIGURE 2.
Cumulative rate of burn injury during 22 months in patients with chronic obstructive pulmonary disease receiving oxygen therapy during first 2 calendar months in the cohort study. Yes indicates patients who were prescribed oxygen in January and February (n=97,372). No indicates patients who were not prescribed oxygen in January and February (n=254,884).
In a multivariable analysis (Table 2), the hazard ratio (HR) of a burn injury in patients with COPD prescribed oxygen was 1.68 (95% CI, 1.42–2.00). Other independent risk factors for burn injury included male sex (HR, 1.40; 95% CI, 1.19–1.66), low socioeconomic status (HR, 2.22; 95% CI, 1.84–2.69), and the presence of 3 or more comorbidities (HR, 1.34; 95% CI, 1.06–1.70).
TABLE 2.
Multivariable Analysis of Factors Associated With Hazard Ratio of Burn Injury in Patients With Chronic Obstructive Pulmonary Disease
| Variable | No. of patients (N=352,256) | Hazard Ratio of Burn Injury (95% CI) |
|---|---|---|
| Oxygen therapy | ||
| No | 254,884 | 1 [Reference] |
| Yes | 97,372 | 1.68 (1.42–2.00) |
|
| ||
| Low socioeconomic status | ||
| No | 292,369 | 1 [Reference] |
| Yes | 59,887 | 2.22 (1.84–2.69) |
|
| ||
| Region | ||
| New England | 18,366 | 1 [Reference] |
| East North Central | 60,958 | 1.12 (0.73–1.72) |
| East South Central | 29,081 | 1.19 (0.76–1.89) |
| Middle Atlantic | 50,944 | 1.00 (0.64–1.56) |
| Mountain | 17,005 | 0.98 (0.56–1.70) |
| Unknown | 2177 | 1.36 (0.41–4.53) |
| Pacific | 32,116 | 1.03 (0.65–1.64) |
| South Atlantic | 81,916 | 1.02 (0.67–1.55) |
| West South Central | 36,821 | 1.23 (0.79–192) |
| West North Central | 22,872 | 1.26 (0.77–2.05) |
|
| ||
| Age | 352,256 | 0.97 (0.96–0.99) |
|
| ||
| Sex | ||
| Female | 183,659 | 1 [Reference] |
| Male | 168,597 | 1.40 (1.19–1.66) |
|
| ||
| Race | ||
| White | 320,316 | 1 [Reference] |
| Nonwhite | 31,940 | 0.86 (0.65–1.14) |
|
| ||
| No. of comorbidities | ||
| 0 | 79,907 | 1 [Reference] |
| 1 | 91,647 | 1.02 (0.79–1.31) |
| 2 | 71,355 | 1.06 (0.81–1.38) |
| ≥3 | 109,347 | 1.34 (1.06–1.70) |
|
| ||
| Year of study | ||
| 2001 | 34,174 | 1 [Reference] |
| 2002 | 35,142 | 1.88 (0.58–1.32) |
| 2003 | 35,816 | 1.37 (0.95–1.97) |
| 2004 | 36,044 | 1.30 (0.90–1.88) |
| 2005 | 37,126 | 1.14 (0.78–1.66) |
| 2006 | 34,932 | 0.94 (0.63–1.40) |
| 2007 | 33,449 | 1.00 (0.68–1.49) |
| 2008 | 33,485 | 0.92 (0.61–1.39) |
| 2009 | 34,781 | 1.25 (0.85–1.84) |
| 2010 | 37,310 | 1.64 (1.15–2.35) |
DISCUSSION
Our findings indicate that patients with COPD prescribed oxygen therapy were more likely to sustain a burn injury compared with patients with COPD not prescribed home oxygen therapy. Furthermore, patients with COPD prescribed oxygen sustained a burn injury that frequently involved the face, neck, or hands. In addition to oxygen, the risk factors associated with development of a burn injury in patients with COPD included male sex, having 3 or more comorbidities, and low socioeconomic status. Moreover, patients who sustained a burn injury associated with home oxygen had a 10-fold greater mortality rate than patients with COPD and no burn injury.
Home oxygen is frequently prescribed to individuals with COPD and hypoxemia at rest because it has been reported to improve survival in patients with COPD and severe hypoxemia.1,2 A Cochrane review of long-term oxygen therapy in patients with COPD and severe hypoxemia (defined as PaO2 <55 mm Hg) found that 4.5 patients needed to be treated with long-term oxygen therapy to save 1 life during 5 years.22 Concerns have been raised about the expensive nature of home oxygen therapy and the benefits with oxygen therapy in patients with COPD and normal resting PaO2 experiencing desaturation during sleep or physical activity.23 Specifically, patients with COPD with a resting PaO2 of 56 to 65 mm Hg provided supplemental oxygen did not have improvements in survival compared with controls.24 Similarly, Chaouat et al25 reported no difference in survival between patients with COPD with a resting PaO2 of 56 to 69 mm Hg who received nocturnal oxygen and a well-matched control group. Medicare currently reimburses for supplement oxygen for patients with desaturation during sleep or physical activity. To further define the benefits of oxygen therapy in the latter 2 groups, a multicenter federally funded trial is under way.
Adverse effects related to home oxygen include mucosal irritation, carbon dioxide retention, retinopathy, pulmonary toxicity, and cutaneous burns.26 Single-center case series have described the occurrence of significant burn injuries associated with home oxygen therapy.27,28 The largest case series from a regional burn center in Pennsylvania described outcomes of 86 individuals hospitalized for burn injuries related to oxygen use during an 11-year period.29 The authors reported that 37% of burn injured patients required tracheal intubation with a median hospital stay of 7.5 days. Furthermore, the National Fire and Protection Agency reported that 1 of every 4 home fires involving medical oxygen that was reported to local fire departments resulted in death.10 The findings of our study obtained from a national database further highlight the risk associated with home oxygen therapy and burn injuries.
Physicians specializing in the care of burn injuries have recognized the association with long-term oxygen therapy in patients with COPD and exposure to lighted tobacco products.11–14 Other authors have reported that most such burn injuries were linked to lighted tobacco products.12 A report by the Centers for Disease Control and Prevention described a case series of 38 fatalities that occurred from 2000 to 2007 in 4 states in which 89% of the decedents were using long-term oxygen and smoking tobacco products at the outset of the fire.30 In the initial clinical trials that examined the effect of oxygen on survival, smoking cessation was encouraged for all participants, yet 38% to 43% continued to smoke.1,2,31 Prescribing oxygen to patients who continue to smoke is certainly controversial. This ethical dilemma was reviewed by Lacasse and colleagues,31 who suggested not prescribing oxygen to active smokers who fail to adhere to instructions and reevaluating patients discharged with a home oxygen prescription after hospitalization because a third of such patients no longer meet the requirement for home oxygen. Likewise, the Veterans Health Administration32 addressed the need for informed decision making in patients who continue to smoke while concurrently using oxygen and recommended using noncoercive measures to mitigate the danger. The dilemma is further highlighted by US and European agency recommendations regarding the prescription of home oxygen to active smokers, with most national agencies and respiratory societies requesting that health care professionals discourage smoking and recommend smoking cessation counseling while a few consider smoking an exclusion or absolute contraindication for oxygen therapy (Portugal and Slovakia).5
In our retrospective cohort study, the rate of burn injury in patients with COPD receiving oxygen therapy is 1.626 per 1000 patients per year compared with 0.922 per 1000 patients per year without oxygen. Thus, the excess rate of burn injury in patients receiving oxygen therapy is 0.704 per 1000 patients per year. In other words, one has to treat 1421 patients with oxygen therapy for 1 year to cause one burn injury. If we assume that all the excess risk of burns is concentrated in the patients who continue to smoke, and we estimate that the prevalence of smoking is 15% to 25%, then the excess risk of burn injury associated with oxygen therapy in smokers would be 0.106 to 0.176 per 1000 patients per year.
Our study has several limitations. First, we used data from fee-for-service Medicare beneficiaries, and our findings may not generalize to non-Medicare patients. In addition, these findings may not be generalized to Medicare beneficiaries enrolled in managed care plans or those without Medicare part B coverage. Second, oxygen therapy was on the basis of claims submitted under DME file use and may not represent the actual daily use of oxygen therapy. We were unable to establish smoking status, active or past, for individuals with burn injuries. We attempted to assess smoking status by claims submitted for smoking cessation, but the lack of reimbursement for tobacco cessation counseling before 2005 and the lack of physician use of this service limited our ability to accurately determine an individual’s smoking status. In addition, we were unable to obtain information on alcohol,33 narcotic, and/or sedative use, which is associated with increased risk for fire hazard.
CONCLUSION
In summary, the benefits of oxygen in patients with COPD outweigh the modest risks of burn injury. However, health care professionals should educate and counsel patients and family members of potential risk of burn injury and attempt to eliminate or mitigate this risk before prescribing home oxygen therapy.
Acknowledgments
We thank Sarah Toombs-Smith for her help with preparation of the manuscript. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
Grant Support: This work was supported by grants K05-CA134923 (J.S.G.) and 5P30AG024832 (J.S.G.) from the National Institutes of Health and by grants R01-HS020642 (Y.-F.K.) and R24HS022134 (J.S.G.) from the Agency for Healthcare Research and Quality.
Footnotes
Potential Competing Interests: Dr Sharma served on the advisory board of Sunovion Pharmaceuticals. The remaining authors have reported no potential conflicts of interest related to the content of this article.
References
- 1.Medical Research Council Working Party. Long-term home oxygen therapy in chronic hypoxic cor pulmonale complicating chronic bronchitis and emphysema. Lancet. 1981;1(8222):681–686. [PubMed] [Google Scholar]
- 2.Nocturnal Oxygen Therapy Trial Group. Continuous or nocturnal oxygen therapy in hypoxemic chronic obstructive lung disease: a clinical trial. Ann Intern Med. 1980;93(3):391–398. doi: 10.7326/0003-4819-93-3-391. [DOI] [PubMed] [Google Scholar]
- 3.Anthoninsen NR, Skeans MA, Wise RA, et al. The Lung Health Study Research Group. The effects of a smoking cessation intervention on 14.5-year mortality. Ann Intern Med. 2005;142(4):233–239. doi: 10.7326/0003-4819-142-4-200502150-00005. [DOI] [PubMed] [Google Scholar]
- 4.Vestbo J, Hurd SS, Agusti AG, et al. Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187(4):347–365. doi: 10.1164/rccm.201204-0596PP. [DOI] [PubMed] [Google Scholar]
- 5.Zielinski J. Indications for long term oxygen therapy: a reappraisal. Monaldi Arch Chest Dis. 1999;54(2):178–182. [PubMed] [Google Scholar]
- 6.Christopher KL, Porte P. Long term oxygen therapy. Chest. 2011;139(2):430–434. doi: 10.1378/chest.10-0242. [DOI] [PubMed] [Google Scholar]
- 7.Pelletier-Fleury N, Lanoe JL, Fleury B, Fardeau M. The cost of treating COPD patients with long-term oxygen therapy in a French population. Chest. 1996;110(2):411–416. doi: 10.1378/chest.110.2.411. [DOI] [PubMed] [Google Scholar]
- 8.Serginson JG, Yang IA, Armstrong JG, et al. Variability in the rate of prescription and cost of domiciliary oxygen therapy in Australia. Med J Aust. 2009;191(10):549–553. doi: 10.5694/j.1326-5377.2009.tb03308.x. [DOI] [PubMed] [Google Scholar]
- 9.Croxton TL, Bailey WC. Long-term oxygen treatment in chronic obstructive pulmonary disease: recommendations for future research: an NHLBI workshop report. Am J Resp Crit Care Med. 2006;174(4):373–378. doi: 10.1164/rccm.200507-1161WS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ahrens M National Fire Protection Association. [Accessed July 8, 2014];Fires and Burns Involving Home Medical Oxygen. www.nfpa.org/assets/files/pdf/os.oxygen.pdf.
- 11.Meuhlberg T, Smith MA, Wong L. Domiciliary oxygen and smoking: an explosive combination. Burns. 1998;24(7):658–660. doi: 10.1016/s0305-4179(98)00100-4. [DOI] [PubMed] [Google Scholar]
- 12.Robb BW, Hungness ES, Hershko DD, et al. Home oxygen therapy: adjunct or risk factor? J Burn Care Rehabil. 2003;24(6):403–406. doi: 10.1097/01.BCR.0000096275.27946.68. [DOI] [PubMed] [Google Scholar]
- 13.Edelman DA, Maleyko-Jacobs S, White MT, Lucas CE, Ledgerwood AM. Smoking and home oxygen therapy a preventable public health hazard. J Burn Care Res. 2008;29(1):119–122. doi: 10.1097/BCR.0b013e31815f5a3a. [DOI] [PubMed] [Google Scholar]
- 14.Chang TT, Lipinski CA, Sherman HF. A hazard of home oxygen therapy. J Burn Care Rehabil. 2001;22(1):71–74. doi: 10.1097/00004630-200101000-00015. [DOI] [PubMed] [Google Scholar]
- 15.Morrison D, Skwarski K, Mac Nee W. Review of prescription of domiciliary long term oxygen therapy in Scotland. Thorax. 1995;50(10):1103–1105. doi: 10.1136/thx.50.10.1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lacasse Y, Lecours R, Pelletier C, Bégin R, Maltais F. Randomised trial of ambulatory oxygen in oxygen-dependent COPD. Eur Respir J. 2005;25(6):1032–1038. doi: 10.1183/09031936.05.00113504. [DOI] [PubMed] [Google Scholar]
- 17.Ringbaek TJ, Lange P. The impact of the Danish Oxygen Registry on adherence to guidelines for long term oxygen therapy in COPD patients. Respir Med. 2006;100(2):218–225. doi: 10.1016/j.rmed.2005.04.023. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Medicare and Medicaid Services. [Accessed January 10, 2014];Medicare Program-General Information: Overview. 2010 Nov; http://www.cms.gov/MedicareGenInfo.
- 19.Research Data Assistance Center. [Accessed January 10, 2014];Medicare Data File Descriptions. 2010 Oct 1; http://www.resdac.umn.edu/Medicare/file_descriptions.asp.
- 20.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 21.King MS, Lipsky MS, Sharp L. Expert agreement in Current Procedural Terminology evaluation and management coding. Arch Intern Med. 2002;162(3):316–320. doi: 10.1001/archinte.162.3.316. [DOI] [PubMed] [Google Scholar]
- 22.Cranston JM, Crockett AJ, Moss JR, Alpers JH. Domiciliary oxygen for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2005;(4):CD001744. doi: 10.1002/14651858.CD001744.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stoller JK, Panos RJ, Krachman S, et al. Oxygen therapy for patients with COPD: current evidence and the long-term oxygen treatment trial. Chest. 2010;138(1):179–187. doi: 10.1378/chest.09-2555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gorecka D, Gorselak K, Sliwinski P, Tobiasz M, Zielinski J. Effect of long term oxygen therapy on survival in patients with chronic obstructive pulmonary disease with moderate hypoxaemia. Thorax. 1997;52(8):674–679. doi: 10.1136/thx.52.8.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chaouat A, Weitzenblum E, Kessler R, et al. A randomized trial of nocturnal oxygen therapy in chronic obstructive pulmonary disease patients. Eur Respir J. 1999;14(5):1002–1008. doi: 10.1183/09031936.99.14510029. [DOI] [PubMed] [Google Scholar]
- 26.Pierson DJ. Oxygen in respiratory care: a personal perspective from 40 years in the field. Respir Care. 2013;58(1):196–204. doi: 10.4187/respcare.02239. [DOI] [PubMed] [Google Scholar]
- 27.Vercruysse GA, Ingram WL. A rationale for significant cost savings in patients suffering home oxygen burns: despite many comorbid conditions, only modest care is necessary. J Burn Care Res. 2012;33(6):e268–e274. doi: 10.1097/BCR.0b013e3182504487. [DOI] [PubMed] [Google Scholar]
- 28.Al Kassis SA, Savetamal A, Assi R, et al. Characteristics of patients with injury secondary to smoking on home oxygen therapy transferred intubated to a burn center. J Am Coll Surg. 2014;218(6):1182–1186. doi: 10.1016/j.jamcollsurg.2013.12.055. [DOI] [PubMed] [Google Scholar]
- 29.Amani H, Lozano DD, Blome-Eberwein S. Brother, have you got a light? assessing the need for intubation in patients sustaining burn injury secondary to home oxygen therapy. J Burn Care Res. 2012;33(6):e280–e285. doi: 10.1097/BCR.0b013e31824d1b3c. [DOI] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention. Fatal fires associated with smoking during long term oxygen therapy - Maine, Massachusetts, New Hampshire, and Oklahoma, 2000–2007. MMWR Morb Mortal Wkly Rep. 2008;57(31):852–854. [PubMed] [Google Scholar]
- 31.Lacasse Y, LaForge J, Maltais F. Got a match? home oxygen therapy in current smokers. Thorax. 2006;61(5):374–375. doi: 10.1136/thx.2006.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Veterans Health Administration National Center for Ethics in Health Care. [Accessed July 8, 2014];Ethical considerations that arise when a home care patient on long term oxygen therapy continues to smoke. 2010 :1–15. www.ethics.va.gov/.../NEC_Report_20100301_Smoking_while_on_LTOT.
- 33.Bruck D, Ball M, Thomas IR. Fire fatality and alcohol intake: analysis of key factors. J Stud Alcohol Drugs. 2011;72(5):731–736. doi: 10.15288/jsad.2011.72.731. [DOI] [PubMed] [Google Scholar]