Abstract
Incidence of abdominal pregnancy is accounting for 1.4% of all ectopic pregnancies. This is a rare case report of a 35-year-old multigravida who was presented to our hospital at 24 weeks of gestation with advanced live intraabdominal pregnancy diagnosed by ultrasound. The patient was followed up till 28 weeks in hospital for medicolegal viability in Egypt. Midline laparotomy was done, a live baby was delivered, and hysterectomy was done for attached placenta. Mother was discharged in good health, and baby was admitted in neonatal intensive care unit with no congenital anomalies and died after three weeks of sepsis. The management of advanced abdominal pregnancy remains controversial. Diagnosis and management of advanced abdominal pregnancy is still a challenge to today’s medical world. But high index of suspicion aided with imaging studies can help in timely diagnosis, thereby preventing the associated life-threatening complications.
Keywords: abdominal pregnancy, ectopic pregnancy, ultrasound, hysterectomy, preterm, laparotomy
Introduction
Primary abdominal pregnancy results from implantation in peritoneal cavity, exclusive of tubal, ovarian, or intraligamentary implantation.1 It can also occur as a secondary abdominal pregnancy due to secondary implantation from an aborted tubal pregnancy, ruptured cornual pregnancy, or as a result of intraabdominal fertilization.2,3 The estimated incidence of abdominal pregnancy is 1 in 10,000 live births and 1.4% of all ectopic pregnancies.4,5 Advanced abdominal pregnancy refers to a pregnancy that continues beyond 20 weeks with a fetus living.6 Despite the availability of medical health facilities worldwide, the cases of advanced abdominal pregnancy associated with high fetomaternal morbidity and mortality are still encountered. Estimated maternal mortality rate is 5 per 1000 cases, about seven to eight times the mortality rate of ectopic pregnancies in general.4 The most important causes of maternal death are hemorrhagic shock, coagulopathy, and infection.7 The survival of infants after 30 weeks is 63%8 with 20–40%8,9 incidence of birth defects due to compression by the absence of amniotic fluid buffer. Limb deficiencies and central nervous system anomalies are the most common malformations, while facial or cranial asymmetries and joint abnormalities are the most common deformations. The management of advanced abdominal pregnancy remains controversial.
Case Report
A 35-year-old multigravida, G3P2, NVD, was presented to the emergency department of our hospital at 24 weeks of gestation with complains of abdominal pain. She underwent abdominal ultrasound examination in private clinic where abdominal pregnancy was not suspected except late at 24 weeks due to inexperience in ultrasound. The patient did not receive regular antenatal checkup because she was in a remote area from medical facilities. She was vitally stable on admission with no vaginal bleeding and no signs of acute abdomen. On clinical examination of the abdomen, fetal parts were palpable superficially and fetal heart rate was 140/minute and regular. A repeat abdominal ultrasound examination was done in our hospital that showed an empty uterus with a single live fetus seen outside uterine cavity with no amniotic fluid in the amniotic sac surrounding it (Fig. 1). Placenta was attached to the fundus of the uterus with marked increase in vascularity. The patient’s hemoglobin count was 10 g/dL with normal liver and kidney function tests. Level of alpha-fetoprotein was elevated. The decision according to our department protocol was to follow up till the age of medical legal viability in Egypt—~28 weeks of gestation in the hospital with interference in case of any emergency because of already late presentation approaching viability. The patient underwent exploratory laparotomy under general anesthesia through lower midline incision (Fig. 2–6). The fetus was intraperitoneal with omentum covering an amniotic sac. The membranes were thick and were ruptured. Liquor was drained out. A live baby girl was extracted as breech with some toes gangrenous by omental bands around them that were excised. The cord was doubly clamped, cut, and tied close to its placental attachment. Birth weight was 1.5 kg. The fetus was vigorous with normal Apgar score at five minutes with no congenital anomalies. Placenta was left undisturbed that was attached to the fundus of the uterus. Severe bleeding occurred on trial of removal with no plane of separation, so subtotal hysterectomy without bilateral salpingo-oophorectomy was done. Abdomen was closed in layers. Two units of blood transfusion and two units of plasma were given intraoperatively with two units of blood postoperatively.
Figure 1.
Ultrasound 2D showing empty uterus with placenta attached to fundus with blood supply from uterus and fetal head in abdomen (A), whole fetus seen intraabdominal not surrounded by uterine wall and anhydraminos (B), and maternal liver seen beside fetal liver characteristic of extra uterine location of fetus (C).
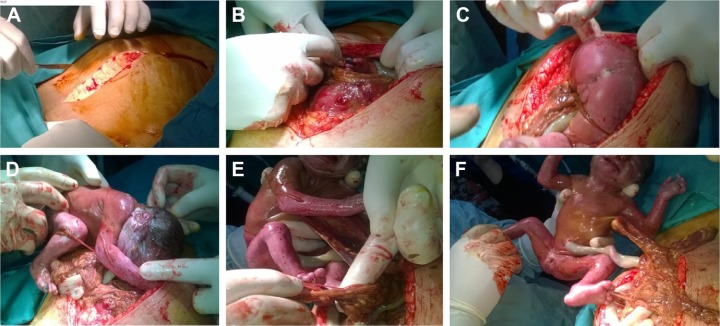
Figure 2.
Steps of the operation. Midline laparotomy (A), entering abdominal cavity with fetal leg seen with gangrenous toe in the peritoneal cavity outside the uterus (B), extraction of the fetus by breech extraction (C), complete delivery of fetus with omental bands around fetal legs and body (D), omental bands around fetal toes with resulting gangrene with amniotic membrane covering the fetus with no liquor in peritoneal cavity (E), and vigorous female baby with amniotic membrane around the fetus with omental bands attached (F).
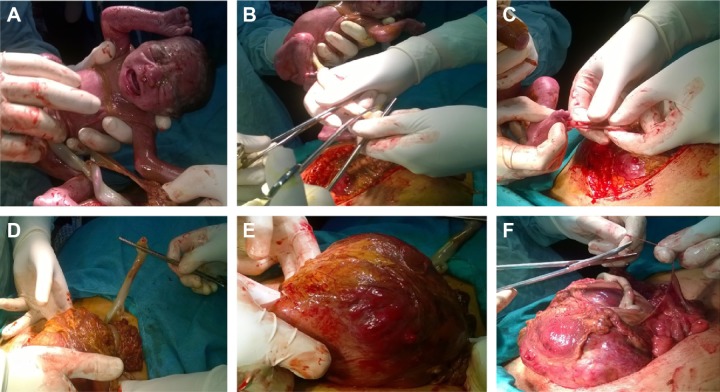
Figure 3.
Continuation of the steps. Normal fetus (A), clamping and cutting of cord (B), disentanglement and removal of omental bands from toes of the baby (C), delivering the uterus outside the abdomen (D), placenta attached to the fundus of the uterus (E), and dissection of the colon from the uterus (F).
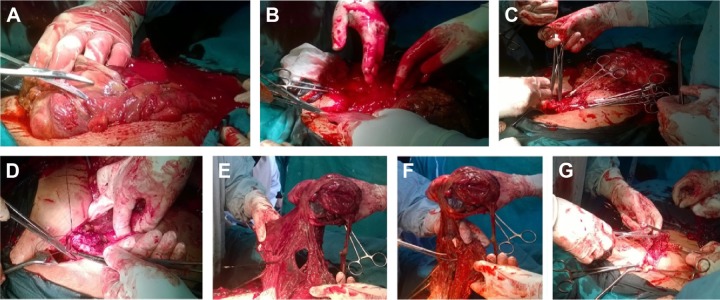
Figure 4.
Steps of hysterectomy. Dissection of the colon (A), placenta separation occurred spontaneously with severe bleeding and morbid attachment (B), delayed ligation technique (C), suturing the stump and the pedicles (D), omental adhesions to the uterine specimen (E), clamping and excision of the omental adhesions (F), ligating the omentum after excision (G).
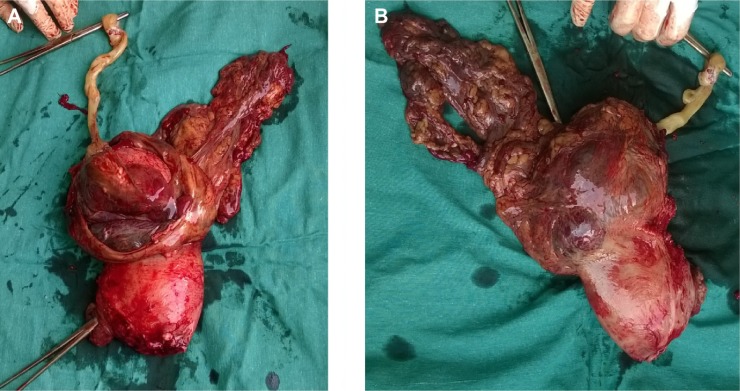
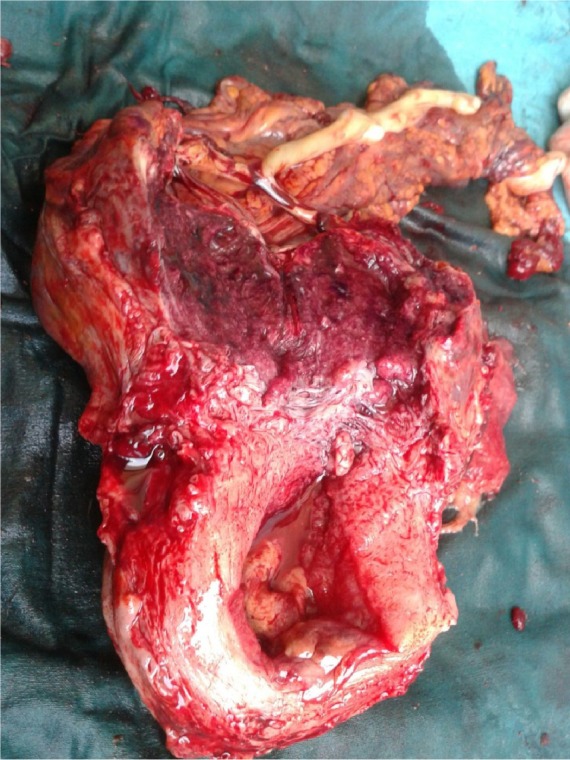
Figure 5.
Hysterectomy specimen with artery forceps in the cervix showing thinning out of myometrium near fundus with the suspicion of early ruptured cornual pregnancy with attachment of the placenta to the fundus with omental adhesions.
Figure 6.
Cut section in the hysterectomy specimen with empty cavity and placenta attached to the fundus with no plane of separation.
The patient remained hemodynamically stable. Her postoperative period was uneventful. Mother was discharged in good health. Vascular surgeon recommended waiting for spontaneous amputation of the toes. The baby was admitted in neonatal intensive care unit with hyaline membrane disease that was treated and died after three weeks of sepsis, although antibiotics were given to the baby. Cut section of hysterectomy specimen revealed thinning near the fundus that might be the site of early rupture of cornual pregnancy that progressed to secondary abdominal pregnancy, and histopathology revealed placental attached to fundus with empty cavity. Cornual pregnancy was suspected, as was missed in early ultrasound scan because it is nearly intrauterine.
Discussion
Diagnosis and management of advanced abdominal pregnancy is still a challenge. But high index of suspicion aided with imaging studies can help in timely diagnosis of this rare obstetrical occurrence preventing life-threatening complications. The patient may present with vaginal bleeding, persistent abdominal pain, or painful fetal movements. On examination, abnormal presentation, easily palpable fetal parts, uneffaced and displaced cervix or palpation of abdominal mass separate from uterus.10 High index of suspicion is the first step in the diagnosis. Increased levels of maternal serum alpha-fetoprotein add to the suspicion.6 Ultrasonography and magnetic resonance imaging are diagnostic modalities that are used for the confirmation of abdominal pregnancy.10 Ultrasound showed empty uterus, absence of amniotic fluid, absence of myometrium between bladder and gestation, and abnormal lie with fetal parts close to abdominal wall.6,10,11 But sonographic diagnosis is missed in half of the cases.6 Despite all, the diagnosis in most of the cases is made at the time of surgery only. If the fetus is mature, immediate laparotomy is the definitive management, but if fetus is immature and mother is in good health, one can opt for conservative management with strict surveillance giving mother’s safety the primary importance. After delivering baby, the management of placenta is also controversial due to diffuse and unidentifiable blood supply of abnormally implanted placenta. Life-threatening hemorrhage during laparotomy is the main concern. If one cannot identify and ligate the vascular supply of placenta, it is preferable to leave it as such for natural regression,7 which can be monitored by β-hCG levels and ultrasonography—this process takes several months. Methotrexate administration can lead to massive necrosis and subsequent infection.7 Angiographic embolization can be used to block placental vessels.12
Conclusion
Obstetricians and radiologists should improve their skills to diagnose these cases in time, so that they do not reach advanced stage where management itself becomes difficult. In any case, a high index of suspicion is crucial, and this should be triggered by any of the following clues: bleeding or nonlabor abdominal pain during the third trimester, maternal declaration of the cessation of fetal movements, perception on the part of the mother or the physician that something is not right, abnormal fetal lie, displaced cervix or abdominal mass palpated apart from the fetus, unusual echographic appearance of the placenta, failed induction and ultrasound with empty cavity, fetus away from uterus, fetus not surrounded by myometrium, and anhydraminos with the exclusion of cornual pregnancy in early pregnancy.
Acknowledgments
The cooperation of EL-Shatby Maternity University Hospital residents who participated in appointing the patient and following up is acknowledged. The commitment and compliance of the patient who reported the required data and attended for the regular follow-up are also appreciated.
Footnotes
ACADEMIC EDITOR: Nicole Powell-Dunford, Editor in Chief
PEER REVIEW: Three peer reviewers contributed to the peer review report. Reviewers’ reports totaled 499 words, excluding any confidential comments to the academic editor.
FUNDING: Authors disclose no external funding sources.
COMPETING INTERESTS: Authors disclose no potential conflicts of interest.
Paper subject to independent expert blind peer review. All editorial decisions made by independent academic editor. Upon submission manuscript was subject to anti-plagiarism scanning. Prior to publication all authors have given signed confirmation of agreement to article publication and compliance with all applicable ethical and legal requirements, including the accuracy of author and contributor information, disclosure of competing interests and funding sources, compliance with ethical requirements relating to human and animal study participants, and compliance with any copyright requirements of third parties. This journal is a member of the Committee on Publication Ethics (COPE).
Author Contributions
Conceived the concepts: ESEB, MA, ASEA. Wrote the first draft of the manuscript: ASEA. Contributed to the writing of the manuscript: ASEA, AEH. Agree with manuscript results and conclusions: ESEB, MA, ASEA. Jointly developed the structure and arguments for the paper: ESEB, ASEA. Made critical revisions and approved final version: ESEB, MA, ASEA. All authors reviewed and approved of the final manuscript.
Ethical Approval
Written informed consent was obtained from the patient for publication of this case report and the accompanying images.
REFERENCES
- 1.Cunningam L. William’s Obstetrics. 23rd ed. 2010. Ectopic pregnancy, Chapter 10; p. 249. [Google Scholar]
- 2.Elagwany AS, Elgamal HH, Abdeldayem TM. Ruptured ectopic pregnancy in non-communicating right rudimentary horn: a case report. Apollo Med. 2013 doi: 10.1016/j.apme.2013.10.002. [DOI] [Google Scholar]
- 3.Awad EE, El-agwany AS, El-habashy AM, et al. Lower uterine segment pregnancy (Cesarean Scar Pregnancy and early placenta accreta): a rising complication from cesarean section with possible and similar early ultrasound diagnoses and management. The Egyptian Journal of Radiology and Nuclear Medicine. 2015;46:977–980. [Google Scholar]
- 4.Atrash HK, Friede A, Hogue CJR. Abdominal pregnancy in United States: frequency and maternal mortality. Obstet Gynecol. 1987;63(3):333–337. [PubMed] [Google Scholar]
- 5.Bouyer J, Coste J, Fernandez H, et al. Sites of ectopic pregnancy: a 10 year population based study of 1800 cases. Hum Reprod. 2002;17:3224–3230. doi: 10.1093/humrep/17.12.3224. [DOI] [PubMed] [Google Scholar]
- 6.Worley KC, Hnat MD, Cunningham FG. Advanced extra-uterine pregnancy: diagnostic and therapeutic challenges. Am J Obstet Gynecol. 2008;198(3):297.e1–297e7. doi: 10.1016/j.ajog.2007.09.044. [DOI] [PubMed] [Google Scholar]
- 7.Berek JS. Early pregnancy loss and ectopic pregnancy, Chapter 20. Berek and Novak’s Gynecology. (15th ed) 2012;644:628. [Google Scholar]
- 8.Stevens CA. Malformations and deformations in abdominal pregnancy. Am J Med Genet. 1993;47(8):1189–1195. doi: 10.1002/ajmg.1320470812. [DOI] [PubMed] [Google Scholar]
- 9.Rahman MS, Al-Suleiman SA, Rahman J, et al. Advanced abdominal pregnancy–observations in 10 cases. Obstet Gynecol. 1982;59:366–372. [PubMed] [Google Scholar]
- 10.Isah AY, Ahmed Y, Newbode EL, et al. Abdominal pregnancy with a full term live fetus: case report. Ann Afr Med. 2008;4(7):198–199. doi: 10.4103/1596-3519.55653. [DOI] [PubMed] [Google Scholar]
- 11.Bertrand G, Le Ray C, Simard-Emond L, et al. Imaging in the management of abdominal pregnancy: a case report and review of literature. J Obstet Gynaecol Can. 2009;31(1):57–62. doi: 10.1016/s1701-2163(16)34055-5. [DOI] [PubMed] [Google Scholar]
- 12.Cardosi RJ, Nackley AC, Londono J, et al. Embolisation for advanced abdominal pregnancy with a retained placenta. A case report. Reprod Med. 2002;47(10):861–863. [PubMed] [Google Scholar]