Abstract
This prospective, longitudinal study examined the transactional relations among perceived maternal parenting stress, maternal insensitivity, and child behavior across toddlerhood through age 6 within families of a child born preterm. A sample of 173 mother-child dyads were followed from just before the infant was discharged from the neonatal intensive care unit to 6 years of age, with observational measurements of maternal insensitivity and child noncompliance (24 and 36 months), maternal self-reports of perceived parenting stress (24 months, 36 months, 6 years), and maternal reports of child externalizing behavior at 6 years. Results indicated that maternal insensitivity at 36 months significantly mediated the relation between parenting stress at 24 months and externalizing behaviors at 6 years. Parenting stress was also directly associated with child noncompliance at 36 months and with child externalizing behavior at 6 years. Neonatal risk was associated with increased maternal insensitivity at 24 months, but also decreased parenting stress at 24 months. No significant “child effects” from child behavior to either maternal insensitivity or parenting stress were found. Parenting stress appears to play a critical role for children born preterm, and it is associated with children’s behavior both directly and through its influence on parenting. The role of neonatal risk needs continued investigation, as families traditionally considered to be at lower risk may still face significant challenges.
Keywords: prematurity, parenting stress, behavior problems, transactional, parent-child interactions
Each year, 11.39% of children are born preterm in the United States (Martin, Hamilton, Osterman, Curtin & Matthews, 2015), and these children face elevated risk of developing behavior problems, attention problems, and cognitive and learning difficulties (Bhutta, Cleves, Casey, Cradock, & Anand, 2002; Gray, Indurkhya, & McCormick, 2004). In addition to the risks experienced by their children, many parents of children born preterm experience high levels of stress and symptomatology (Feldman-Reichman, Miller, Gordon, & Hendricks-Munoz, 2000), and early parent-child interactions may be strained (Forcada-Guex, Pierrehumbert, Borghini, Moessinger, 2006). Given the large number of infants born preterm, in concert with the improving preterm survival rates (Matthews & MacDorman, 2012), greater attention should be given to bidirectional, transactional processes occurring in these families over the course of childhood (Sameroff, 2009), including understanding how neonatal risk affects mothers and how parents and children are mutually influential. The present study examined transactional processes linking parenting stress, mother-child interactions, and the development of children’s challenging behaviors from infancy through age 6 in the context of premature birth.
Prematurity as a Context for Parenting
Prematurity represents a significant challenge to children and families. Infants born preterm are at risk for less optimal cognitive development and attention deficits and behavior problems compared to their term peers (e.g., Bhutta et al., 2002; Gray et al., 2004). Historically, research on prematurity has compared children born preterm and term, finding that children born earlier present with more risks, as do their families (Bhutta et al., 2002). Traditionally, infants born in the late preterm period were thought to be at relatively low developmental risk, with little focus on them past infancy, but emerging research indicates that infants born late preterm are also at elevated risk for neurodevelopmental, learning, behavioral, and attentional problems (Shah, Robbins, Coelho, & Poehlmann, 2013; Woythaler, McCormick, & Smith, 2011).
Families of infants born preterm are also at risk. Parenting stress is elevated in mothers of high-risk infants within the first year of life compared to term infants (Brummelte, Grunau, Synnes, Whitfield, & Petrie-Thomas, 2011; Singer et al., 1999). Perceived parenting stress reflects the degree to which parents experience the demands of daily parenting tasks as stressful (Deater-Deckard, 2006), and has been shown to affect parenting behaviors (Crnic & Low, 2002) and child behavior (Crnic, Gaze, & Hoffman, 2005).
However, there is some inconsistency in the literature focusing on parenting stress in families of infants born preterm (Gray, Edwards, O’Callaghan, & Cuskelly, 2012), particularly as children grow older (Treyvaud et al., 2011; Brummelte et al., 2011). Little work has compared levels of parenting stress within preterm samples past infancy, although Singer and colleagues (1999) found that mothers of high-risk, very low birthweight children reported higher levels of perceived stress in comparison to mothers of low-risk, very low birthweight children. Similar to term samples, elevated parenting stress and distress adversely affect early maternal sensitivity and parent-child relationships for children born preterm (Muller-Nix et al., 2004), and parenting stress is influenced by children’s behavior (Benzies, Harrison, & Magill-Evans, 2004). Theories examining the mechanisms for how parenting stress affects children’s behavior suggest both a possible direct path as well as a possible mediated path, wherein parenting stress affects the quality of parenting interactions, which subsequently affect child adjustment (Deater-Deckard, 2006). However, such models have rarely been tested in families of children born preterm.
Prematurity and Mother-Child Interactions
Parent-child interactions can be challenging in the context of prematurity. During play interactions, premature infants exhibit less emotional positivity, cooperation, and responsiveness than term infants, and their mothers engage in more intrusive and less sensitive behaviors (Forcada-Guex et al., 2006). A comparison of children born very preterm, moderately preterm, and term indicated that mothers of infants born very preterm showed more intrusiveness and difficulty scaffolding as well as less sensitivity (Clark, Woodward, Horwood, & Moor, 2008).
Differences in parent-child interaction quality have implications for children’s social emotional development (Clark et al., 2008; Landry, Smith, Swank, Assel, & Vellet, 2001). Whereas responsive and supportive interactions are associated with better language, cognitive, and social development (Tamis-LeMonda, Shannon, Cabrera, & Lamb, 2004), Landry et al. (2001) found that consistent maternal responsivity across time was particularly important for cognitive and social development in children born preterm. Maternal sensitivity has also been associated with children’s early regulatory abilities in preterm populations (Clark et al., 2008).
Transactional Developmental Models
Research with high risk children and families has turned from understanding reciprocal relations between parent and child functioning at one point in time to examining how parents and children influence each other across time (Pardini, 2008). These transactional models of development suggest that both parents and children are actively engaged in interactions and can mutually affect one another’s behavior over time (Sameroff, 2009). Support for transactional models has often focused on the connection between maternal depression and children’s behavior problems, with studies finding bidirectional effects from preschool through adolescence (Gross, Shaw, Burwell, & Nagin, 2009; Harvey & Metcalfe, 2012). Transactional relations between parenting stress and child behavior have also been examined (e.g., Neece, Green, & Baker, 2012). A recent study by Yates and colleagues (2010) tested potential transactional relations among contextual strain (stressful life events, relationship tension, and social support), parenting quality, and child dysregulation. They found direct associations between contextual strain and later child behavior, but the effect was not reciprocal nor mediated through parenting.
However, when transactional relations have been further investigated, the evidence to support child-effects on parenting and symptomatology is more limited (Yates et al., 2010). Children’s behavior may only influence parental symptomatology at certain points in development (Harvey & Metcalfe, 2012), for only one gender (Yates et al., 2010), or child-effects may not be found at all (Hanington, Ramchandani, & Stein, 2010). There are strong theoretical foundations for examining the impact of the child on parent behavior, but child effects may be curbed by other factors, such as financial or work stress, and difficult to capture.
In families of children born preterm, understanding the mechanisms of effects is vital in order to separate the influence of neonatal risk from other factors. While there is evidence that intrusive parenting is related to more negative outcomes for children (Landry et al, 2001), parenting stress is related to more negative parenting (Crnic & Low, 2002) as well as worsening externalizing behavior (Crnic & Low, 2002), longitudinal examinations of these mediated paths are rarely conducted in a preterm population. Given that these children are at risk for elevated behavior problems (particularly those born in the late preterm period), in the present study we examined a transactional mediation model focusing on the development of behavior problems from 24 months through age 6.
Child Externalizing Behavior Problems
Children born preterm experience more behavioral difficulties than term infants, including greater internalizing, externalizing, and attentional difficulties (Bhutta et al., 2002; Gray et al, 2004). These differences have been found in comparisons of children born late preterm and term (Woythaler et al., 2011), although evidence also suggests higher levels of externalizing behavior for infants born in the late versus very preterm period (Shah et al., 2013).
Yet little is known about whether early noncompliance in toddlers born preterm has implications for the development of subsequent externalizing problems. Noncompliance and opposition to parental requests are dysregulated behaviors that may lead to significant externalizing behavior problems if such dysregulation and accompanying negative affect escalate over time (Kochanska & Aksan, 1995). While studies examining trajectories of children’s externalizing behaviors have predominantly focused on school-age children, opposition and defiance in toddlers has been often been characterized as more developmentally appropriate and less concerning (Campbell, Shaw, & Gilliom, 2000). However, evidence suggests that oppositional and impulsive behaviors seen during toddlerhood can set children on a path that may lead to later externalizing and conduct problems (Campbell, 2006). Yet trajectories from noncompliance to externalizing behavior are largely unexamined in the preterm population. While internalizing problems are also elevated in preterm populations (Bhutta et al., 2002), internalizing disorders are historically not linked to noncompliance and oppositional behavior, and thus, beyond the focus of this study.
Parenting quality also has implications for how children behave in relationships, such as how well children respond to parental requests (Kochanska & Aksan, 1995). Oppositional behaviors in infancy and early childhood are likely related to both temperament and caregiving (Campbell, 2006), and sensitive and proactive parenting can change a child’s behavioral trajectory (Denham et al., 2000). In previous research with infants born preterm, (Poehlmann et al., 2012) toddlers who experienced elevated neonatal medical risks and increasing maternal depressive symptoms over time exhibited the most observed opposition to maternal requests.
Current Study
The current study examined the transactional relations among perceived maternal parenting stress, maternal insensitivity during play, and child behavior in children born preterm between 24 months and 6 years of age. We hypothesized that earlier parenting stress would be associated with later child behavior problems, whereas early child noncompliance would simultaneously contribute to later parenting stress. A specific mediated path was hypothesized from parenting stress to maternal insensitivity to child behavior problems. Higher neonatal risk was hypothesized to be associated with greater initial parenting stress and levels of insensitivity.
Method
Participants
A total of 181 infant-mother dyads were recruited from three Neonatal Intensive Care Units (NICU) in Southcentral and Southeastern Wisconsin between 2002–2005. A research nurse from each hospital invited families to participate if they met the following criteria: (a) Infants were born at ≤37 weeks gestation or weighed <2500grams at birth; (b) infants had no known congenital malformations, prenatal drug exposures or significant neurological findings during the NICU stay (e.g., Down syndrome, periventricular leukomalacia, grade IV intraventricular hemorrhage) so the study could focus on risk instead of more known developmental trajectories, (c) mothers were at least 17 years of age; (d) mothers could read English; and (e) mothers self-identified as the infant’s primary caregiver. If a child was part of a multiple birth, one child was randomly selected to participate in the study. As the hospital would not allow us to be the “first contact” for families and they gave us only information about families who signed consent forms, 181 (97%) participated in data collection. Data from 173 families were utilized in this study. Data from 8 of the original 181 families were removed because we later discovered from our review of infant medical records that a grade IV intraventricular hemorrhage had occurred prior to the infants’ NICU discharge (3), the child was later diagnosed with cerebral palsy (1), or the child was born after 36 weeks gestation, despite having low birth weight (4).
Participant family characteristics paralleled the population of Wisconsin during the data collection period. Infants were stratified by gestational age: very preterm < 32 weeks (n=82, 47.4%), moderate preterm between 32 and 33 6/7 weeks (n=43, 24.9%), and late preterm between 34 and 36 weeks (n=48, 27.7%) (See Table 1).
Table 1.
Sample Demographic and Neonatal Characteristics at NICU Discharge (N=173)
| Variable | Range or Frequency (and %) | M | SD |
|---|---|---|---|
| Maternal Age | 17–42 | 29.54 | 6.26 |
| Maternal Education (years) | 8–21 | 14.25 | 2.69 |
| Family Income per Year ($) | 0–210,000 | 57,390 | 42252.29 |
| Gender of Child | |||
| Male | 92 (53.2%) | ||
| Female | 81 (46.8%) | ||
| Child ABIQ score at age 3 | 61–133 | 98.71 | 13.63 |
| Verbal Knowledge Subtest | 1–17 | 9.76 | 2.54 |
| Nonverbal Fluid Reasoning Subtest | 3–17 | 9.81 | 2.81 |
| Infant Race | |||
| African American | 24 (13.9%) | ||
| Asian | 1 (0.6%) | ||
| Caucasian | 114 (65.9%) | ||
| Latino | 3 (1.7%) | ||
| Middle Eastern | 2 (1.2%) | ||
| Multiracial | 29 (16.7%) | ||
| Marital Status | |||
| Married or cohabitating | 140 (80.9%) | ||
| Not married or cohabitating | 33 (19.1%) | ||
| Infant Gestational Age (in weeks) | 23.71–36 | 31.34 | 3.03 |
| Infant Birth Weight | 490–3328 | 1712.46 | 577.23 |
| Extremely Low (<1,000 g) | 28 (16.2%) | ||
| Very Low (<1,500 g) | 37 (21.4%) | ||
| Low (<2,500 g) | 95 (54.9%) | ||
| Normal (≥2,500 g) | 13 (7.5%) | ||
| Days Hospitalized | 2–136 | 33.27 | 27.92 |
| Multiple Birth | 33 (19.1%) | ||
| Medical Concerns | |||
| Apnea | 119 (68.8%) | ||
| Respiratory Distress Syndrome | 91 (52.6%) | ||
| Chronic Lung Disease | 17 (9.8%) | ||
| Gastroesophageal Reflux | 16 (9.2%) | ||
| Retinopathy of Prematurity | 2 (1.1%) | ||
| Sepsis and Other Infections | 22 (12.7%) | ||
| Health of Child between Discharge and age 3 | |||
| Times Reported Sick | 0–36 | 11.69 | 7.90 |
| Number of Hospital Visits | 0–9 | 0.58 | 1.28 |
Overall, 32.4% of the sample received early intervention services between birth to three years old, including 23.2% receiving physical therapy, 15.5% receiving occupational therapy, and 19% receiving speech therapy. 15.2% received one type of intervention, 6.0% received two types of interventions, and 11.3% received three or more interventions. The intervention data was parent-reported and only reflects our knowledge of early intervention while they were enrolled in the study. Length of time in therapy was not consistently reported.
Attrition
The current study included data from the NICU Discharge, 16 month, 24 month, 36 month, and 6 year assessments. One hundred seventy-three mother-child dyads participated at hospital discharge, 147 at 24 months, 138 at 36 months, and 109 participated at 6 years. Sixty percent of the original families participated at the 6-year assessment. Families lost to attrition did not differ from families who remained in the study on birthweight, gestational age, neonatal health, child gender, paternal age, family income, number of children in the family, and maternal race. However, families were more likely to be lost to attrition when the mother was younger, single and had completed fewer years of education, and when the father had completed fewer years of education. In addition, infants lost to attrition were less likely to be Caucasian.
Procedure
Families were enrolled in the study through three hospitals following IRB approval. An IRB-approved brochure was distributed to families in each NICU, a research nurse described the study to eligible families, and interested mothers signed consent forms. A researcher met with the mother in the NICU just prior to infant’s discharge, and mothers completed questionnaires. Nurses completed a history of hospitalization via review of the infant’s medical records shortly after NICU discharge. At 16, 24, and 36 months’ postterm (age corrected for prematurity), families visited the laboratory playroom. Mothers completed questionnaires while a research assistant administered a standardized developmental assessment to the child. At 24 and 36 months, mothers and children were videotaped playing together and completing a clean-up task. Each of the laboratory visits lasted approximately 1.5 to 2 hours. Mothers were paid $65 for the 16-month visit, $80 for the 24-month visit, $85 for the 36-month visit, and children were given an appropriate book or toy at each visit. At 6 years, mothers completed a 20–25 minute phone interview and a number of self-report questionnaires that were returned in a self-addressed, stamped envelope. Mothers were sent a $15 gift card for participation.
Measures
Infant prematurity, neonatal risk, and health
The hospitalization form completed by nurses was used to create a neonatal health risk index, drawing on previous indices for infants born preterm (Littman & Parmelee, 1978; Scott, Bauer, Kraemer, & Tyson, 1997). Infant birthweight and gestational age were standardized using z-scores and then reverse-coded so that higher scores reflected more prematurity and lower birthweight. Next, 10 dichotomized neonatal medical complications (1=present, 0 =absent) were summed and standardized: apnea, respiratory distress, chronic lung disease, gastroesophageal reflux, multiple birth, supplementary oxygen at NICU discharge, apnea monitor at NICU discharge, 5-min Apgar score <6, ventilation during NICU stay, and NICU stay of >30 days. This risk index was averaged with the reversed-coded gestational age and birthweight. The resulting index (M=.001, SD=2.67) had a Cronbach’s α=.89, with higher scores reflecting more neonatal risk, and was normally distributed.
Between departure from the NICU and 36 months, parent-reported health variables were collected, including number of times the child was sick and the number of hospital visits (See Table 1). Due to significant skew, number of hospitalized visits was dichotomized (0=no hospital visits; 66.9% of sample, 1=1 or more hospital visits).
Maternal parenting stress
Daily maternal parenting stress (or parenting hassles) was assessed at 24 months, 36 months, and 6 years using the Parenting Daily Hassles (PDH) scale (Crnic & Greenberg, 1990). The PDH is a self-report questionnaire consisting of 20 parenting tasks that can by trying or challenging. Examples of items include cleaning up messes, difficulty getting privacy, and having to change plans because of an unplanned child need. Mothers report both how often the hassle occurs and the perceived intensity of that hassle on a 5-point scale. The perceived intensity score reflects appraised stressfulness by the parent, whereas frequency reflects only the presence of stressors. Prior research has indicated that cognitive appraisal of significant events as stressful best predicts the stressor’s impact (Lazarus, DeLongis, Folkman, & Gruen, 1985). Thus, the perceived intensity summary scale was used at all time-points. The PDH had high internal consistency (Cronbach α=.86–.87) across time points, and was normally distributed. While parenting daily hassles were correlated with maternal depression (r =.28, p =.001) at 24 months, the PDH is a distinct variable.
Insensitive/intrusive parenting
At 24 and 36 months postterm, infant-mother play interactions took place in the laboratory playroom with a standard set of age-appropriate toys. Interactions were videotaped and later coded using the Parent Child Early Relational Assessment (PCERA; Clark, 2010). The PCERA is designed to assess the frequency, duration, and intensity of affect and behavioral characteristics of parents and infants that occur during 5 minutes of face-to-face interactions. In the 15 minute free-play interaction, the middle interaction period from 5–10 minutes was coded. On the basis of the 5 minute observation, each variable is coded on a scale ranging from 1 (negative relational quality) to 5 (positive relational quality). Previous studies of the PCERA have reported an acceptable range of internal consistency (r=.75–.96) and factorial validity (Clark, 1999). In this study, the established 8-item subscale (Clark, 1999) of Parental Insensitivity, Intrusiveness, and Inconsistency was used (Cronbach’s α= .78 at 24 months; α= .71 at 36 months), including parental rigidity, insensitivity, inconsistency, intrusiveness, anxiety, physical contact, structure, reading cues and verbalizing. Lower scores indicate more insensitive and intrusive behavior. The scale was normally distributed. Ten percent of the sample was independently coded by four trained research assistants at each timepoint, with regular checks for reliability throughout the coding period. Percent agreement is the standard used in the PCERA. Interrater percent agreement ranged from .83 to .97 across codes and timepoints, with a mean of .88. Kappas ranged from .58 to 1.0 (mean of .71 across timepoints).
Toddler noncompliance
The child’s noncompliance with maternal requests was assessed at 24 and 36 months through a toy cleanup task that followed an unstructured 15-minute play session. At the end, children were given a large plastic bin and mothers were instructed to have the child pick up the toys. The cleanup session ended when the toys were picked up or after 5 minutes, whichever came first. The cleanup session was videotaped and coded using a continuous approach to coding, with 30-second intervals (up to 10), based on Kochanska and Aksan (1995). The following mutually exclusive codes were applied: (1) committed compliance, where the child followed the mother’s request without reminders or coercion while exhibiting positive affect; (2) situational compliance, where although the child generally followed the mother’s request, he or she did so without positive affect, enthusiasm, or sense of cooperation; (3) passive noncompliance, where although the child did not pick up the toys, he or she did not become involved in overt conflict with mother; (4) refusal negotiation, where the child did not pick up the toys, the mother attempted to coerce the child, and the child negotiated or refused; and (5) defiance, where the child did not pick up the toys and that angry interactions ensued. If more than one behavior was shown in a 30 second interval, the least productive mutually exclusive code was used. On average, the 24 month clean-up task lasted about 4 minutes (M=8.72 interval blocks, SD=1.85, Range=3–10), whereas the average 36 month task lasted 3 minutes, 30 seconds (M=8.10, SD=2.29, Range=3–10).
Following Kochanska (2002), we calculated the proportion of time children spent in noncompliance (proportion of passive noncompliance, refusal negotiation, and defiance intervals combined). Situational and committed compliance codes were not used in this paper because of low variability: situational compliance is common and developmentally appropriate for toddlers, whereas committed compliance had low occurrence at 24 months (56% of children showed no committed compliance). Across the intervals coded, 93% of children had one or more intervals in which they exhibited some form of noncompliance with maternal requests at 24 months, while 78% of children had one or more intervals at 36 months, and the overall noncompliance code was normally distributed. Videotapes were coded by trained students. Exact percent agreement across independently coded tapes ranged from .76 to .80, and agreement within 1 point ranged from .94 to .98 for both time points. Kappa’s ranged from .65 to .80, with a mean of .70. Raters of noncompliance were independent of and blind to the ratings of maternal insensitivity.
Child externalizing behavior
Mothers completed the Preschool Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2000) at 16 months and the School-Age Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2001) at 6 years. The CBCL is a widely-used, standardized behavior-rating scale that is completed by an adult with whom the child lives. The preschool form lists 99 problem behaviors, whereas the school-age form lists 113 problem behaviors. Mothers rate each behavior on a scale of 0 (not true), 1 (somewhat or sometimes true), or 2 (very true or often true) in reference to the last 6 months. Responses on the Externalizing Problem Scale were summed to create a total score, which was normally distributed. The raw Externalizing scale at 16 months was used as an auxiliary control variable (M=11.04, SD=6.63, Range=0–29), whereas the raw Externalizing scale at 6 years was used as a study variable (M=6.45, SD=5.79, Range=0–26; Cronbach’s α=.87). Although the CBCL was collected at 16 months corrected age, the average chronological age of children at the time was 18.1 months (Range=16.4–21.5 months). For a clinical interpretation, T scores greater than 63 are considered clinically significant, whereas T scores between 60–63 are considered in the borderline range. At 6 years, 21% of the sample had borderline or clinically significant externalizing behaviors (M=50.06, SD=9.90), while only 6% did at 16 months (M=50.18, SD=9.93).
Maternal socioeconomic status (SES)
Mothers completed a demographic questionnaire while their infants were in the NICU, including data regarding years of education and family income. Family income was initially skewed due to one family reporting an income of $500,000, so it was top-coded to the next highest family with a reported family income of $210,000. A maternal SES index was then created by standardizing and averaging maternal education and family income (α=.74) (Davis-Kean, 2005)
Cognitive development
Children’s cognitive skills were estimated at 36 months using the Abbreviated Battery IQ scale (ABIQ) from the Stanford-Binet Intelligence Scales, 5th edition (Roid, 2003). The ABIQ comprises the sum of Nonverbal Fluid Reasoning and Verbal Knowledge subtests (α=.62), scores are based upon postterm age (i.e. adjusted for prematurity). The ABIQ scale has an alpha of .90 (Roid, 2003).
Data Analytic Plan
Analyses examined the transactional nature of parenting stress, maternal insensitivity, and children’s behavior, in addition to addressing the early influence of neonatal risk. Analyses were conducted using path model analysis in structural equation modeling with 95% confidence intervals constructed with bootstrapping in MPlus Version 6.12 12 (Muthén & Muthén, 2010). Analyses utilized a three-tiered autoregressive path model with cross-lagged associations among parenting stress, maternal insensitivity, and children’s noncompliance and behavior problems. To assess the role of neonatal risk, parenting stress, maternal insensitivity, and noncompliant behavior at 24 months were all simultaneously regressed on neonatal risk.
In the model, parenting stress at age 6 years was simultaneously regressed on itself at 36 months, and parenting stress at 36 months was regressed on itself at 24 months to measure construct stability. Simultaneously, maternal insensitivity at 36 months was regressed onto itself at 24 months. Maternal report of externalizing behavior at 6 years was regressed on observed noncompliance at 36 months, which was simultaneously regressed on noncompliance at 24 months. Additionally, cross-lagged paths were simultaneously estimated from 24 month parenting stress to maternal insensitivity and noncompliance at 36 months, from 24 month maternal insensitivity to parenting stress and noncompliance at 36 months, and from 24 month noncompliance to parenting stress and maternal insensitivity at 36 months. Similarly, cross-lagged paths were estimated from parenting stress and maternal insensitivity at 36 months to 6 year externalizing behaviors, and from maternal insensitivity and noncompliance at 36 months to 6 year parenting stress. The cross-lagged paths examine direction of effect at each time period.
Mediation analysis was conducted using MODEL INDIRECT in Mplus with 95% confidence intervals constructed by bias-corrected bootstrapping (1000 samples) to provide a more accurate estimation of standard errors (MacKinnon, 2008). Overall estimation for adequate model fit was determined according to values of Root Mean Square Error of Approximation (RMSEA<.05), Standardized Root Mean Square Residual (SRMR < .05), Comparative Fit Index (CFI>.95), and a non-significant chi square statistic.
To provide a more accurate estimation of parameters and reduce bias while accounting for missing data, analyses were conducted using full information maximum likelihood estimation with auxiliary variables. Auxiliary variables are correlated to missingness and/or recapture lost information and can improve power (Enders, 2010). In an analysis, the auxiliary variables are correlated with all of the other variables in the study to accurately account for their effect. Based on the theory and the attrition data, the variables SES, cognitive level, use of early intervention (0=no, 1=yes), number of times sick between discharge and age 3, hospitalization between discharge and age 3 (0=no, 1=yes) and maternal-reported externalizing behavior at 16 months were used as auxiliary variables. Auxiliary variables do not change the degrees of freedom in a model nor do they affect chi-square or RMSEA fit statistics. However, auxiliary variables can inflate the CFI statistic, so a modified CFI calculated by using a baseline model that estimates auxiliary variables correlations and constraints was reported in analyses (Enders, 2010).
Results
Descriptive Statistics and Correlations
Descriptive statistics are presented in Table 2, and correlations among the variables are presented in Table 3. Mothers reported similar levels of perceived parenting stress across time, and there were moderate to high correlations across time points, indicating high rank-order stability. Maternal insensitivity also maintained relatively similar levels and showed a small correlation between 24 and 36 months.
Table 2.
Descriptive Statistics
| Variable | M | SD | Range |
|---|---|---|---|
| Parenting Stress (24m) | 20.31 | 11.28 | 0–54 |
| Parenting Stress (36m) | 21.95 | 11.31 | 0–53 |
| Parenting Stress (6yr) | 21.19 | 11.52 | 0–54 |
| Maternal Insensitivity (24m) | 31.52 | 4.06 | 18–40 |
| Maternal Insensitivity (36m) | 32.99 | 3.34 | 23–39 |
| Noncompliance (24m) | .52 | .29 | 0–1 |
| Noncompliance (36m) | .34 | .29 | 0–1 |
| Externalizing Behavior (6yr) | 6.45 | 5.79 | 0–26 |
| Neonatal Risk | .00 | 2.67 | −4.08–6.56 |
| SES | −.02 | .87 | −1.73–2.30 |
| Externalizing Behavior (16m) | 11.04 | 6.62 | 0–29 |
Note: Neonatal Risk and SES are based on variables that have been standardized and averaged. The individual variables that comprise these composites are listed in Table 1.
Table 3.
Correlation Table of Study Variables
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | 13. | 14. | 15. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Neonatal Risk | -- | ||||||||||||||
| 2. Parenting Stress (24m) | −.19* | -- | |||||||||||||
| 3. Parenting Stress (36m) | −.16† | .61** | -- | ||||||||||||
| 4. Parenting Stress (6yr) | −.14 | .49** | .53** | -- | |||||||||||
| 5. Mat. Insensitivity(24m) | −.23* | .08 | −.00 | .17 | -- | ||||||||||
| 6. Mat. Insensitivity(36m) | .06 | −.15 | −.19* | −.03 | .27* | -- | |||||||||
| 7. Noncompliance (24m) | .10 | −.16† | −.06 | −.15 | −.09 | −.05 | -- | ||||||||
| 8. Noncompliance (36m) | .07 | .16 | .03 | .10 | −.08 | −.11 | .27* | -- | |||||||
| 9. Externalizing Beh. (16m) | −.15† | .22* | .41* | .32* | −.05 | .01 | −.12 | −.12 | -- | ||||||
| 10. Externalizing Beh. (6yr) | .01 | .34* | .30* | .29* | −.18† | −.25* | .05 | .23* | .42** | -- | |||||
| 11. SES | −.10 | −.04 | −.05 | .02 | .42** | .32** | −.01 | −.05 | −.10 | −.33* | -- | ||||
| 12. Cognitive Level (36m) | −.02 | −.04 | −.00 | .04 | .33** | .23* | −.10 | −.17* | −.01 | −.15 | .35** | -- | |||
| 13. Gender | −.06 | .07 | .03 | .03 | −.01 | −.03 | .20* | .09 | −.10 | .15 | .08 | −.12 | -- | ||
| 14. Intervention | .32** | −.04 | −.07 | −.24* | −.02 | .13 | −.01 | .08 | −.11 | −.09 | .11 | −.08 | −.03 | -- | |
| 15. Times Sick | −.06 | .20* | .27* | .23* | .07 | −.07 | .09 | .18 | .15 | .30* | .07 | −.02 | .25* | .11 | -- |
| 16. Hospitalization | .20* | −.23* | −.06 | −.10 | −.16 | −.06 | .14 | .17 | −.17† | −.02 | −.06 | −.06 | .11 | .22* | .38** |
Note. Gender was coded such that 0=girl, 1=boy. Intervention was coded so that 0=no early intervention, 1=early intervention. Hospitalization was coded such that 0=no hospitalizations, 1=1 or more hospitalizations. In the PCERA, lower scores on insensitivity indicate more insensitivity and intrusiveness, whereas higher scores indicate more sensitivity and less intrusiveness.
p<.08,
p<.05,
p<.001.
Noncompliance decreased from 24 to 36 months, t(134)=6.04, p<.001, Cohen’s d=.62. Observed noncompliant behavior at 36 months showed a small but significant correlation with mother-reported externalizing behavior at 6 years, signifying some association, but also suggesting some differences in construct. Length of clean-up task was examined as a potential covariate, but was only associated with increased oppositional compliance (r=.38, p<.001, r=.42, p<.001, at 24 and 36 months respectively), as would be expected, and no other study variables, so it was not included in the model.
Correlations were found between parenting stress and later maternal insensitivity, as well as between parenting stress and children’s behavior. Correlations were also found between maternal insensitivity at 36 months and externalizing behavior problems at 6 years.
Neonatal risk related to increased maternal insensitivity and decreased parenting stress at 24 months. Preliminary analyses also used ANOVAs to test the associations between neonatal risk and study variables using the three categories of prematurity (very, moderate, and late). However, findings were similar in the dichotomized and continuous approaches, so the broader continuous neonatal risk variable was used in analyses. SES and cognitive level were associated with maternal insensitivity and child behavior, supporting their use as auxiliary variables. Early intervention and hospitalization were associated with greater prematurity and fewer parenting hassles, while number of time sick was associated with greater parenting hassles. There were no differences in prediction between the ABIQ scale score and the two subtest scores for Verbal Knowledge and Nonverbal Reasoning, so the ABIQ score was used for parsimony. Boys exhibited more noncompliance than girls at 24 months and thus, gender was used as covariate to noncompliance in the final model. There was no evidence of gender moderating these processes.
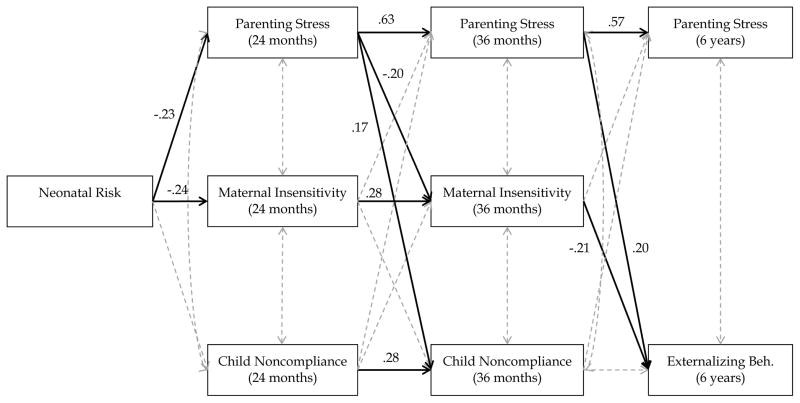
Overall Model
The fit indices for the overall model indicated good fit, X2(18)= 20.93, p=.283, CFI=.980, RMSEA=.020, SRMR=.035 (Figure 1). Using R2, the final model predicted 39.2% and 31.9% of the variance of parenting stress at 36 and 6 years, respectively. It predicted 10.5% of the variance of maternal insensitivity at 36 months, 10.0% of the variance of noncompliance at 36 months, 15.4% of the variance of externalizing behavior at 6 years.
Figure 1.
Final transactional model of child and parent behavior. Numbers indicate significant standardized path coefficients at p<.05. Dotted lines were not significant. In this model, SES cognitive level, use of early intervention, number of times sick, hospitalization, and CBCL at 16 months are accounted for as auxiliary variables, and gender is covaried with noncompliance. In the PCERA, lower scores on insensitivity indicate more insensitivity and intrusiveness, whereas higher scores indicate more sensitivity and less intrusiveness.
SES was associated with maternal insensitivity at 24 and 36 months (B=.39, p<.001, and B=.24, p=.001, respectively), and externalizing behavior at 6 years (B=−.23, p=.040). Cognitive level was associated with 24-month maternal insensitivity (B=.32, p<.001), coded so that lower scores indicated more insensitive and intrusive behavior. Externalizing behavior at 16 months was associated with greater externalizing behavior at 6 years (B=.37, p<.001), and more parenting stress at 36 months (B=.41, p<.001). Use of early intervention was associated with less intrusive behavior at 24 and 36 months (B=.33, p<.001, B=.23, p=.005, respectively) and less oppositional behavior at 36 months (B=−.20, p=.016). Hospitalization was associated with less parenting stress at 24 months (B=−.20, p=.033).
Stability over time
The model indicated large regression coefficients for parenting stress from 24 months to 6 years, suggesting strong stability (See Table 4 for parameter estimates). Between 24 and 36 months, maternal insensitivity and noncompliance each showed small but significant regressions coefficients with themselves, suggesting these constructs maintain some stability, but also continue to change during toddlerhood. Although correlated and significant prior to bootstrapping, observed noncompliance at 36 months was not significantly associated with externalizing behavior at 6 years after using bias-corrected bootstrapping.
Table 4.
Parameter Estimates for Autoregressive and Crossover Paths
| Parameter | B | p | 95% Confidence Interval |
|---|---|---|---|
| Construct Stability | |||
| Parenting Stress (24m) → Parenting Stress (36m) | .63 | <.001 | [.48, .76] |
| Parenting Stress (36m) → Parenting Stress (6yr) | .57 | <.001 | [.36, .83] |
| Maternal Insensitivity (24m) → Maternal Insensitivity (36m) | .28 | .002 | [.09 .38] |
| Noncompliance (24m) → Noncompliance (36m) | .28 | .003 | [.10, .46] |
| Noncompliance (36m) → Externalizing Beh. (6yr) | .20 | .108 | [−.89, 8.78] |
| Associations with Neonatal Risk | |||
| Neonatal Risk → Parenting Stress (24m) | −.23 | .006 | [−1.71, −.31] |
| Neonatal Risk → Maternal Insensitivity (24m) | −.24 | .007 | [−1.67 −.29] |
| Neonatal Risk → Noncompliance (24m) | .13 | .127 | [−.01, .03] |
| Crossover Paths | |||
| Parenting Stress (24m) → Maternal Insensitivity (36m) | −.20 | .032 | [−.11, −.01] |
| Parenting Stress (24m) → Noncompliance (36m) | .17 | .047 | [.00, .01] |
| Maternal Insensitivity (24m) → Parenting Stress (36m) | −.07 | .386 | [−.58, .24] |
| Maternal Insensitivity (24m) → Noncompliance (36m) | −.08 | .367 | [−.02, .01] |
| Noncompliance (24m) → Parenting Stress (36m) | .01 | .927 | [−5.24, 5.54] |
| Noncompliance (24m) → Maternal Insensitivity (36m) | −.05 | .592 | [−2.76, 1.62] |
| Parenting Stress (36m) → Externalizing Beh. (6yr) | .20 | .042 | [.01, .19] |
| Maternal Insensitivity (36m) → Parenting Stress (6yr) | .10 | .325 | [−.40, 1.04] |
| Maternal Insensitivity (36m) → Externalizing Beh. (6yr) | −.21 | .019 | [−.68, −.05] |
| Noncompliance (36m) → Parenting Stress (6yr) | .08 | .397 | [−4.44, 9.89] |
Note. B=standardized path coefficients. Bolded numbers indicate significant findings at p<.05. In the PCERA, lower scores on insensitivity indicate more insensitivity and intrusiveness, whereas higher scores indicate more sensitivity and less intrusiveness.
Transactional relations
Higher parenting stress at 24 months was related to more observed maternal insensitivity at 36 months, supporting the hypothesis that parental stress is associated with later parenting (Figure 1, Table 4). Furthermore, greater 24-month parenting stress was associated with more 36-month child noncompliance, and greater 36-month parenting stress related to more 6-year child externalizing problems, supporting a “parent-effects” model. Maternal insensitivity at 36 months was associated with more externalizing behavior at 6 years. Neither noncompliance nor insensitivity related to later parenting stress, contrary to hypotheses.
Associations with neonatal risk
Neonatal risk was associated with less maternal sensitivity at 24 months (Figure 1, Table 4). Greater neonatal risk was also associated with lower 24-month parenting stress, contrary to hypotheses. To further probe, gestational age was examined separately from neonatal risk factors, but the results did not change, so we used the more comprehensive neonatal risk index in the final model. Given that multiple births can be associated with more stress in parents (Lutz et al., 2012), the model was also tested using only singleton families, and there were no significant differences in relations between neonatal risk and parenting stress (B=−.23, p=.004 in full sample, B=−.24, p=.005 in singleton sample). Neonatal risk was not associated with 24-month child noncompliance.
Tests of mediation
Given the results of the autoregressive analyses, the following mediations were tested. First, as hypothesized, the effect of parenting stress at 24 months on externalizing behavior at 6 years, as mediated by maternal insensitivity at 36 months, was significant, 95% CI [.001, .060]. More 24-month parenting stress was associated with greater 36-month maternal insensitivity, which was then associated with more 6-year externalizing behavior. Second, the effect of neonatal risk on maternal insensitivity at 36 months, as mediated by 24-month parenting stress, was significant, 95% CI [.002, .143], suggesting that higher neonatal risk related to less parenting stress, which was associated with less insensitive and intrusive parenting. Third, the effect of neonatal risk on 36-month child noncompliance, as mediated by 24-month parenting stress, was not significant, 95% CI [−.010, .000]. No mediations tested the effect of children’s behavior on mothers, given the nonsignificant path coefficients.
Discussion
This prospective longitudinal study examined the transactional relations among parenting stress, maternal insensitivity, and the development of behavior problems in children born preterm at age 6. Parenting stress has long been implicated as an important determinant of parenting and child behavior, although investigations using transactional developmental models are more recent (Neece et al., 2012; Yates et al., 2010) and have rarely been investigated in children born preterm. Our findings strongly supported a parent-effects model, wherein maternal insensitivity mediated the relation between early parenting stress and children’s externalizing behavior. Parenting stress also directly predicted children’s later behavior problems. However, our study found limited evidence for child effects, aside from effects of neonatal health.
In our sample, greater parenting stress when children were 24 months was associated with increased maternal insensitivity at 36 months, which was then associated with higher levels of externalizing behavior when the child was 6 years old. This mediated path existed over the course of four years, as shown using multiple methodologies, suggesting an important developmental process in high risk children. Infants born preterm often exhibit neurodevelopmental immaturities that result in less responsive interactions with their parents, with mothers of infants born preterm engaging in more intrusive and less sensitive behaviors compared to mothers of term infants (Forcada-Guex et al., 2006). Such intrusiveness and insensitivity to the child’s cues may have problematic implications for the development of children’s challenging behaviors, particularly in the context of elevated parenting stress.
Parenting stress has been hypothesized to affect children either indirectly (through parental negativity) or more directly by influencing child behavior (Deater-Deckard, 2006). Our study found support for both hypotheses; greater parenting stress was both directly and indirectly associated with increased externalizing problems in 6-year-olds born preterm, and higher parenting stress was also associated with more child noncompliance at 36 months. In contrast to the majority of transactional findings focusing on more clinically-based measures of distress (Gross et al., 2009), our measure of perceived parenting stress focused on parenting daily hassles that all parents experience to some degree, experiences that may be salient to many families.
Contrary to hypotheses, child behavior was not associated with either later maternal insensitivity or parenting stress. Although some prior research has found child behavior to be important influence on perceived stress (Williford, Calkins, & Keane, 2007), other studies have not found bidirectional relations with parenting stress (Yates et al., 2010) when testing transactional models. In the present study, parenting stress remained relatively stable, with strong correlations at each time point, which makes finding cross-over relations more difficult (Rogosa, 1980). Child behavior may be differentially influential on stress across time, such as in adolescence when the child tests boundaries, or may be mediated or moderated by unexamined variables, such as support or coping. Additionally, some noncompliance and opposition to parental requests during toddlerhood is normative, as children begin to exert their independence and individuality (Campbell et al., 2000). Parents may consider their children’s behavior to be less stressful if it is perceived to be developmentally appropriate.
Further, prior studies finding support for child-effects on parenting stress often utilized parent reports of behavior problems (Neece et al., 2012), whereas our study analyzed observed noncompliant behavior in addition to reports of behavior problems. We did not find a significant relation between observed noncompliance at 36 months and parent-report of externalizing behavior at 6 years in the full multivariate model, although correlations were significant. Parent reports and observational assessments of behavior often show only modest relations (Hinshaw, Han, Erhardt, & Huber, 1992). While both parent-report and observed methods are useful in capturing a range of child behaviors, they may measure somewhat distinct constructs, and perhaps it is the perception of problematic child behavior that covaries with parenting stress. Further exploration of methodology involved in capturing oppositional behavior is needed.
Although parenting stress was not associated with earlier noncompliance, it was related to infants’ early neonatal characteristics. Greater neonatal risk was associated with less parenting stress at 24 months, contrary to hypotheses. While prior evidence suggests that mothers of infants born preterm experience higher levels of stress and depression that mothers of term infants (Brummelte et al., 2011), these between-subjects comparison focus less on degree of prematurity. Children who scored lower on the neonatal risk index were most often born in the late preterm period. General assumptions are that these children will fare better than their higher-risk counterparts on major morbidities, but recent studies have actually found that infants born in the late preterm period may be at greater risk for parent-reported behavioral difficulties compared to infants born at earlier gestational ages (Gray et al., 2004; Shah et al., 2013).
Explanations for why parents of infants born in the late preterm period report greater behavior problems and parenting stress are understudied, but a few potential explanations exist. Infants born very preterm may have greater access to early intervention services, which can be an important positive predictor of outcomes for children (Hill, Brooks-Gunn, & Waldfogel, 2003) and could reduce parental stress. The correlations in our study among early intervention, neonatal risk, and parenting stress support such an interpretation. Additionally, parents of infants born very preterm may have different expectations of their children than parents of infants born later. Parents of infants born very preterm are more often told to expect difficulties by the medical team, and thus they may perceive certain hassles as part of the child’s medical profile, rather than as an unexpected or stressful hassle. Parents of children born late preterm, who may expect more normative development, may perceive the child’s daily behaviors as stressful.
The study has both theoretical and practical implications. When applying transactional models to high risk populations, it is important to examine both parent- and child-effects at multiple points in time and on different sets of behaviors. In the present study, we did not find child-effects when examining longitudinal relations between child noncompliance and insensitive parenting or parenting stress. However, the child’s initial neonatal risk level was significantly associated with both insensitive parenting and parenting stress during the toddler period. Moreover, our findings suggest the importance of studying and providing parenting support to all families of infants born preterm, not just the families of the most medically fragile infants. Infants born preterm are at risk for developing behavior problems, and parenting stress and insensitive parenting are family processes implicated in the development of such problems. Interventions that seek to increase the sensitive responsiveness of parents and decrease perceived parenting stress may be particularly important for this population.
There are a few limitations in this study that should be considered. The six-year data collection was a telephone contact, and no observational data were collected. Mothers reported parenting stress across time and children’s externalizing behavior, which involves shared method variance. However, the distance between measurements (3–4 years) should lessen the potential effect of the shared method, and the relation of parenting stress to observed child behavior adds to the validity of findings across domains. Our study focused on infants born preterm and their mothers, but did not include infants with significant neonatal neurological complications (e.g. Grade IV hemorrhages, PVL) and thus, the results are not generalizable to those infants, low-risk term infants, or to fathers. Further, the sample size may not be large enough to detect more nuanced findings. The ethnic representation in the sample may mask significant racial and socioeconomic disparities in preterm births (Martin et al., 2015). There was significant attrition in the sample between the initial NICU visit and the 6 year follow-up, which may have impacted findings. Given that attrition differentially affected single, younger mothers with fewer years of education, and with non-Caucasian infants, full information maximum likelihood was conducted with auxiliary variables, including SES, was used to minimize the effects of attrition (Enders, 2010). However, the attrition may still influence the generalizability of the findings. Finally, this report did not include children’s internalizing behavior problems.
Families of children born preterm face multiple challenges, and much is still unknown about the lifecourse development for these children and their parents. Our findings suggest that parenting stress plays a critical role, affecting children’s behavior both directly and through its influence on parenting. Yet, the mechanisms through which neonatal risk affects families need continued investigation, as infants born preterm and their parents are at risk for challenges in social-emotional development, particularly those born in the late preterm period. Children’s behavior did not relate to later parenting stress, although further studies should look into issues of developmental timing and measurement in preterm samples. Through understanding complex family processes, strategies for early identification and intervention may be best developed.
Acknowledgments
Funding: This work was supported by grants for the National Institutes of Health (grant numbers R01 HD44163, T32 HD07489, and P30 HD03352) and the University of Wisconsin.
Special thanks to the children and families who generously gave of their time to participate in this study and the numerous students who assisted with data collection and coding.
References
- Achenbach TM, Rescorla LA. ASEBA Preschool Forms & Profiles: An Integrated System of Multi-informant Assessment. Burlington, VT: ASEBA; 2000. [Google Scholar]
- Achenbach TM, Rescorla LA. ASEBA School Age Forms and Profiles. Burlington, VT: ASEBA; 2001. [Google Scholar]
- Benzies KM, Harrison MJ, Magill-Evans J. Parenting stress, marital quality, and child behavior problems at age 7 years. Public Health Nursing. 2004;21(2):111–121. doi: 10.1111/j.0737-1209.2004.021204.x. [DOI] [PubMed] [Google Scholar]
- Bhutta AT, Cleves MA, Casey PH, Cradock MM, Anand K. Cognitive and behavioral outcomes of school-aged children who were born preterm. Journal of the American Medical Association. 2002;288(6):728–737. doi: 10.1001/jama.288.6.728. [DOI] [PubMed] [Google Scholar]
- Brummelte S, Grunau RE, Synnes AR, Whitfield MF, Petrie-Thomas J. Declining cognitive development from 8 to 18 months in preterm children predicts persisting higher parenting stress. Early Human Development. 2011;87(4):273–280. doi: 10.1016/j.earlhumdev.2011.01.030. [DOI] [PubMed] [Google Scholar]
- Campbell SB, Shaw DS, Gilliom M. Early externalizing behavior problems: Toddlers and preschoolers at risk for later adjustment. Development and Psychopathology. 2000;12:467–488. doi: 10.1017/s0954579400003114. [DOI] [PubMed] [Google Scholar]
- Campbell SB. Behavior problems in preschool children: A review of recent research. Journal of Child Psychology and Psychiatry. 2006;36(1):113–149. doi: 10.1111/j.1469-7610.1995.tb01657.x. [DOI] [PubMed] [Google Scholar]
- Clark CA, Woodward LJ, Horwood LJ, Moor S. Development of emotional and behavioral regulation in children born extremely preterm and very preterm: Biological and social influences. Child Development. 2008;79(5):1444–1462. doi: 10.1111/j.1467-8624.2008.01198.x. [DOI] [PubMed] [Google Scholar]
- Clark R. The parent-child early relational assessment: A factorial validity study. Educational and Psychological Measurement. 1999;59(5):821–846. [Google Scholar]
- Clark R. The Parent-Child Early Relational Assessment (Instrument and Manual) Madison, WI: Department of Psychiatry, University of Wisconsin School of Medicine and Public Health; 2010. [Google Scholar]
- Crnic KA, Gaze C, Hoffman C. Cumulative parenting stress across the preschool period: relations to maternal parenting and child behaviour at age 5. Infant and Child Development. 2005;14(2):117–132. doi: 10.1002/icd.384. [DOI] [Google Scholar]
- Crnic KA, Greenberg MT. Minor parenting stresses with young children. Child Development. 1990;61:1628–1637. doi: 10.1111/j.1467-8624.1990.tb02889.x. [DOI] [PubMed] [Google Scholar]
- Crnic K, Low C. Everyday stresses and parenting. 2. Vol. 5. Mahwah, NJ, US: Lawrence Erlbaum Associates, Publishers; 2002. pp. 243–267. [Google Scholar]
- Davis-Kean PE. The influence of parent education and family income on child achievement: the indirect role of parental expectations and the home environment. Journal of Family Psychology. 2005;19:294–304. doi: 10.1037/0893-3200.19.2.294. [DOI] [PubMed] [Google Scholar]
- Deater-Deckard K. Parenting stress and child adjustment: Some old hypotheses and new questions. Clinical Psychology: Science and Practice. 2006;5(3):314–332. doi: 10.1111/j.1468-2850.1998.tb00152.x. [DOI] [Google Scholar]
- Denham SA, Workman E, Cole PM, Weissbrod C, Kendziora KT, Zahn-Waxler C. Prediction of externalizing behavior problems from early to middle childhood: The role of parental socialization and emotion expression. Development and Psychopathology. 2000;12:23–45. doi: 10.1017/s0954579400001024. [DOI] [PubMed] [Google Scholar]
- Enders CK. Applied missing data analysis. New York: Guilford Press; 2010. [Google Scholar]
- Feldman-Reichman SR, Miller AC, Gordon RM, Hendricks-Munoz KD. Stress appraisal and coping in mothers of NICU infants. Children’s Health Care. 2000;29(4):279–293. doi: 10.1207/S15326888CHC2904_4. [DOI] [Google Scholar]
- Forcada-Guex M, Pierrehumbert B, Borghini A, Moessinger A, Muller-Nix C. Early dyadic patterns of mother–infant interactions and outcomes of prematurity at 18 months. Pediatrics. 2006;118(1):107–114. doi: 10.1542/peds.2005-1145. [DOI] [PubMed] [Google Scholar]
- Gray PH, Edwards DM, O’Callaghan MJ, Cuskelly M. Parenting stress in mothers of preterm infants during early infancy. Early Human Development. 2012;88(1):45–49. doi: 10.1016/j.earlhumdev.2011.06.014. [DOI] [PubMed] [Google Scholar]
- Gray RF, Indurkhya A, McCormick MC. Prevalence, stability, and predictors of clinically significant behavior problems in low birth weight children at 3, 5, and 8 years of age. Pediatrics. 2004;114(3):736–743. doi: 10.1542/peds.2003-1150-L. [DOI] [PubMed] [Google Scholar]
- Gross HE, Shaw DS, Burwell RA, Nagin DS. Transactional processes in child disruptive behavior and maternal depression: A longitudinal study from early childhood to adolescence. Development and Psychopathology. 2009;21(1):139–156. doi: 10.1017/S0954579409000091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanington L, Ramchandani P, Stein A. Parental depression and child temperament: Assessing child to parent effects in a longitudinal population study. Infant Behavior and Development. 2010;33(1):88–95. doi: 10.1016/j.infbeh.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey EA, Metcalfe LA. The interplay among preschool child and family factors and the development of ODD symptoms. Journal of Clinical Child & Adolescent Psychology. 2012:1–13. doi: 10.1080/15374416.2012.673161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill JL, Brooks-Gunn J, Waldfogel J. Sustained effects of high participation in an early intervention for low-birth-weight premature infants. Developmental Psychology. 2003;39(4):730–744. doi: 10.1037/0012-1649.39.4.730. [DOI] [PubMed] [Google Scholar]
- Hinshaw SP, Han SS, Erhardt D, Huber A. Internalizing and externalizing behavior problems in preschool children: Correspondence among parent and teacher ratings and behavior observations. Journal of Clinical Child Psychology. 1992;21(2):143–150. doi: 10.1207/s15374424jccp2102_6. [DOI] [Google Scholar]
- Kochanska G. Committed compliance, moral self, and internalization: A mediational model. Developmental Psychology. 2002;38(3):339–351. doi: 10.1037/0012-1649.38.3.339. [DOI] [PubMed] [Google Scholar]
- Kochanska G, Aksan N. Mother-child mutually positive affect, the quality of child compliance to requests and prohibitions, and maternal control as correlates of early internalization. Child Development. 1995;66:236–254. doi: 10.1111/j.1467-8624.1995.tb00868. [DOI] [Google Scholar]
- Landry SH, Smith KE, Swank PR, Assel MA, Vellet S. Does early responsive parenting have a special importance for children’s development or is consistency across early childhood necessary? Developmental Psychology. 2001;37(3):387–403. doi: 10.1037//0012-1649.37.3.387. [DOI] [PubMed] [Google Scholar]
- Lazarus RS, DeLongis A, Folkman S, Gruen R. Stress and adaptational outcomes: The problem of confounded measures. American Psychologist. 1985;40:770–779. [PubMed] [Google Scholar]
- Littman B, Parmelee A. Medical correlates of infant development. Pediatrics. 1978;61(3):470–474. doi: 10.1542/peds.61.3.470. [DOI] [PubMed] [Google Scholar]
- Lutz KF, Burnson C, Hane A, Samuelson A, Maleck S, Poehlmann J. Parenting stress, social support, and mother-child interactions in families of multiple and singleton preterm toddlers. Family Relations. 2012;61:642–656. doi: 10.1111/j.1741-3729.2012.00726.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP. Introduction to statistical mediation analysis. Hillsdale, NJ: Lawrence Erlbaum Associates; 2008. [Google Scholar]
- Martin JA, Hamilton BE, Osterman MJK, Curtin SC, Mathews MS. Births: Final data for 2013. National Vital Statistics Reports. 2015;64(1):1–65. [PubMed] [Google Scholar]
- Matthews TJ, MacDorman M. Infant mortality statistics from the 2008 period linked birth/infant death data set. National Vital Statistics Reports. 2012;60(5):1–28. [PubMed] [Google Scholar]
- Muller-Nix C, Forcada-Guex M, Pierrehumbert B, Jaunin L, Borghini A, Ansermet F. Prematurity, maternal stress and mother–child interactions. Early Human Development. 2004;79(2):145–158. doi: 10.1016/j.earlhumdev.2004.05.002. doi:10.1016.j.earlhumdev.2004.05.002. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 6. Los Angeles: Muthen; 2010. [Google Scholar]
- Neece CL, Green SA, Baker BL. Parenting stress and child behavior problems: A transactional relationship across time. American Journal on Intellectual and Developmental Disabilities. 2012;117(1):48–66. doi: 10.1352/1944-7558-117.1.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pardini DA. Novel insights into longstanding theories of bidirectional parent–child influences: Introduction to the special section. Journal of Abnormal Child Psychology. 2008;36(5):627–631. doi: 10.1007/s10802-008-9231-y. [DOI] [PubMed] [Google Scholar]
- Poehlmann J, Schwichtenberg AM, Hahn E, Miller K, Dilworth-Bart J, Kaplan D, Maleck S. Compliance, opposition, and behavior problems in toddlers born preterm or low birthweight. Infant Mental Health Journal. 2012;33(1):34–44. doi: 10.1002/imhj.20335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogosa D. A critique of cross-lagged correlation. Psychological Bulletin. 1980;88(2):245–258. [Google Scholar]
- Roid G. Stanford-Binet Intelligence Scales. 5. Itasca, IL: Riverside; 2003. [Google Scholar]
- Sameroff A. The transactional model of development: How children and contexts shape each other. Washington, D.C: American Psychological Association; 2009. [Google Scholar]
- Scott DT, Bauer CR, Kraemer HC, Tyson J. The neonatal health index. In: Gross RT, Spiker D, Haynes CW, editors. Helping low birthweight premature babies. Stanford, CA: Stanford University Press; 1997. pp. 341–357. [Google Scholar]
- Shah PE, Robbins N, Coelho RB, Poehlmann J. The paradox of prematurity. Infant Behavior and Development. 2013;36(1):50–62. doi: 10.1016/j.infbeh.2012.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer LT, Salvator A, Guo S, Collin M, Lilien L, Baley J. Maternal psychological distress and parenting stress after the birth of a very low-birth-weight infant. Journal of the American Medical Association. 1999;281(9):799–805. doi: 10.1001/jama.281.9.799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamis-LeMonda CS, Shannon JD, Cabrera NJ, Lamb ME. Fathers and mothers at play with their 2- and 3-year-olds: Contributions to language and cognitive development. Child Development. 2004;75(6):1806–1820. doi: 10.1111/j.1467-8624.2004.00818.x. [DOI] [PubMed] [Google Scholar]
- Treyvaud K, Doyle LW, Lee KJ, Roberts G, Cheong JL, Inder TE, Anderson PJ. Family functioning, burden and parenting stress 2 years after very preterm birth. Early Human Development. 2011;87(6):427–431. doi: 10.1093/jpepsy/jss042. [DOI] [PubMed] [Google Scholar]
- Williford AP, Calkins SD, Keane SP. Predicting change in parenting stress across early childhood: Child and maternal factors. Journal of Abnormal Child Psychology. 2007;35(2):251–263. doi: 10.1007/s10802-006-9082-3. [DOI] [PubMed] [Google Scholar]
- Woythaler MA, McCormick MC, Smith VC. Late preterm infants have worse 24-month neurodevelopmental outcomes than term infants. Pediatrics. 2011;127(3):622–e29. doi: 10.1542/peds.2009-3598. [DOI] [PubMed] [Google Scholar]
- Yates TM, Obradović J, Egeland B. Transactional relations across contextual strain, parenting quality, and early childhood regulation and adaptation in a high-risk sample. Development and Psychopathology. 2010;22(03):539–555. doi: 10.1017/S095457941000026X. [DOI] [PubMed] [Google Scholar]